Abstract
Purpose
Donor site pain affects 32–43 % of patients after anterior cruciate ligament surgery when the autograft is freshly harvested bone-patellar tendon-bone tissue. Our aim was to compare functional and morphological differences between donor sites with and without serum albumin-coated bone allograft filling.
Methods
After harvesting and implanting the graft, the tibia site was filled with either fresh autologous cancellous bone enhanced with albumin-coated allograft or autologous bone alone. The patella site was filled either with albumin-coated allograft or with blood clot. Knee function was evaluated by the VISA, Lysholm and IKDC scores and a visual analog scale of pain during standing, kneeling and crouching after six weeks and six months. Computed tomography was performed at six months for morphological evaluation.
Results
At six weeks, both groups were still recovering from surgery and the overall knee function was still impaired but the functional scores were significantly higher in the Bone-Albumin group. The pain with crouching and kneeling was also lower as compared to controls. At six months, the knee function scores were close to normal, with a slight decrease in the controls. Pain at kneeling was still prominent in the controls, but significantly lower in the Bone-Albumin group. Computed tomography showed significantly smaller bone defects and higher bone density in the Bone-Albumin group.
Conclusions
Results from the present study indicate that donor site pain, a disturbing long-term side effect of bone-patellar tendon-bone surgery, is significantly reduced if bone buildup in the patella and the tibia is augmented by serum albumin-coated bone allografts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cruciate ligament (ACL) reconstruction is one of the most common knee interventions, and multiple studies have been conducted to investigate grafting techniques. So far, most data suggest that graft type has limited influence on clinical outcome, and bone-patellar tendon-bone (BTB) or hamstring tendon can provide stable knee function [1–4]. As a result, both methods are treatment strategies on the clinical palette, differing in their indications [5, 6].
Donor site pain, however, remains a problematic side effect after BTB reconstruction, affecting 32–43 % of the patients [7–9]. The reason behind this phenomenon is the slow or inadequate bone buildup in the tibial and patellar harvest sites. Autologous bone tissue is the best material for bone replacement therapies because it is osteoconductive, osteoinductive and contains osteogenic cells. However, its available volume in this specific indication is low, thus creating the need for other suitable substitute materials. Allogenic bone substitutes are generally used because they are completely biocompatible materials with good osteoconductive properties. The osteoinductivity of these bone substitutes is less favourable, therefore proteins, growth factors, or even stem cells can be used to augment this feature [10]. Although these complex, fully loaded implants can achieve very good bone remodeling in experimental studies, their clinical usefulness is rather limited especially in less serious indications such as BTB surgery [11, 12], creating a pressing clinical need for a bone substitute with improved efficacy and minimal cost and complexity.
In our previous experiments, we showed that bone allografts with a lyophilized serum albumin coating (Bone-Albumin) led to improved allograft properties. Mesenchymal stem cells attach and proliferate on the albumin-coated surface rapidly and by activating stem cells; Bone-Albumin induces faster ossification and reduces healing time in different animal models [13–15]. This was also supported by a first-in-human study, where not only good clinical outcomes were achieved, but implanted allografts also showed intensive osteoblast function even after one year [16].
In the present study, we used Bone-Albumin chips to reduce the size of the bone defects after harvesting patellar tendon grafts, and compared the functional and morphologic differences between donor sites. We hypothesized that donor site morbidity with Bone-Albumin would be less prominent, thereby eliminating a major side effect of BTB reconstruction and improving overall clinical outcome.
Materials and methods
Study protocol and patients
Between 2013 and 2014, male and female patients undergoing ACL reconstruction were asked to participate in our prospective, randomized study. Clinical evaluation of patients at follow-up and morphologic measurements were performed by blinded experimenters. Thirty-nine patients between the age of 18 and 50 were enrolled with the inclusion criteria of high level sports activity prior to injury. Exclusion criteria were associated collateral ligament damage, immune-rheumatologic pathologies, chondropathies higher than grade II (Outerbridge), pre-existing anterior knee pain and previous surgery on the same knee. ACL reconstruction was performed with BTB autografts. All patients received detailed information about the risks and benefits of the procedure prior to granting informed consent and undergoing surgery. Patients were randomly assigned into two groups: 19 patients (2 female / 17 male) in the control group (ACL reconstruction with BTB), and 20 patients (2 female / 18 male) in the Bone-Albumin treated group (ACL reconstruction with BTB plus serum albumin coated allograft implanted into the donor-sites). All patients underwent the same rehabilitation protocol. The study was performed under the approval of the local ethical committee (ALLO-2013-02). Patients were blinded towards the treatment group throughout the study.
Bone-Albumin - serum albumin coated bone chips
Bone pieces were harvested from cadavers or femoral heads harvested at primary hip replacement surgery under the operational license of West-Hungarian Tissue Bank and processed immediately to produce autolysed, antigen extracted allogenic bone according to Urist’s method. The preservation method was freeze-drying under aseptic conditions followed by EtOH sterilisation. After freeze-drying, the bone grafts were submerged in sterile 10 % human serum albumin solution for one minute under aseptic conditions (low-salt-content Biotest human albumin infusion, Biotest Pharma GmbH, Dreieich, Germany) and a second freeze-drying was performed with the same parameters to obtain Bone-Albumin.
Surgical protocol
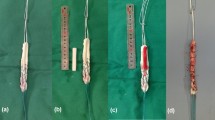
Patients enrolled in the control group were treated according to our routine clinical protocol. BTB autografts were used to reconstruct the ACL. Briefly, the middle third of the patellar tendon was harvested with approximately 10x10x20 mm bone blocks from the patella and tibia. From median arthrotomy, the remains of the ACL was removed. Next, the tibial bone tunnel was prepared to be 9–10 mm in diameter, while the femoral tunnel was 10–11 mm in diameter and placed on the medial surface of the lateral femoral condyle. The tibial part of the BTB autograft was fixed in the femoral tunnel with an interference screw. After tensioning the graft, the patellar bone block was stabilized in the tibial tunnel with two titanium K-wires. Autologous cancellous bone was used to repair the tibial donor site, while the patellar donor site was filled with blood clot. In the treatment group Bone-Albumin mixed with autologous cancellous bone was used to fill the tibial donor site, while only Bone-Albumin was used to fill the patellar defect. At the tibial site, Bone-Albumin and autologous bone was manually mixed in equal volumes and used for filling in the defect. Approximately 3 cm3 allograft chips were required to adequately fill either donor site (Figs. 1 and 2).
Patella donor site filling techniques. Panels a, b, and c show the control technique in an intra-operative picture and one week post-operative axial and 3D CT images. Panels d, e, and f show the Bone-Albumin filling technique. Note that Bone-Albumin filling was complete in each case intra-operatively, however, small bone graft fragments were visible in the early post-op CT in the pre-patellar soft tissue space
Patient follow up
Patients underwent physical examination and VISA (Victorian Institute of Sport Assessment), Lysholm, IKDC (International Knee Documentation Committee) and VAS (visual analog scale) subjective questionnaires. Scores were collected on the post-operative sixth week and sixth month. The VISA score is designed specifically to quantify knee function in subjects with patellar tendinopathy regarding different activities involving knee movement. The score range is 0 to 100. Visual analog scale (VAS) ranging from 0 (no pain) to 10 (maximum pain) evaluates the average knee pain during normal daily activities. Patients were asked to point at the value corresponding to their pain on the numeric scale during kneeling, squatting or standing. Activity level was recorded with the use of International Knee Documentation Committee (IKDC) and Lysholm scores post-operatively.
Computed tomography
Computed tomography (CT) of the knee was also performed after the sixth month with a Phillips Brilliance 64 machine. Axial slices were obtained with 120 Kv and 300 mA (slice thickness: 0.9 mm, increment 0.45 mm, collimation 64 × 0.625 mm, pitch 0.579, rotation time 0.75 s). Remaining bone defect volume was measured with interpolated images on axial slices. The density (HU) of the regenerating defect was measured in a 20-mm2 circular region of interest placed approximately 2 mm below the cortex level. In a separate group of patients CT was performed at one week after surgery in order to illustrate the early positioning of the bone fillers (n = 2 per treatment group). 3D images were reconstructed with Philips Extended Brilliance Workspace software (v3.5.0.2254).
Statistical analysis
All of the values are reported as the means ± SEM. The statistical analysis was performed using Student’s t test using GraphPad Prism software, and p values < 0.05 were considered significant. According to the power analysis performed with BioMath software (http://biomath.info), sufficient effect sizes can be detected with a sample size of n = 16 using 90 % power and 95 % significance.
Results
The average age in the control group was 30.3 ± 1.7 and 26.7 ± 1.9 in the Bone-Albumin group. In the control group ten professional athletes, seven recreational athletes (performing sport activities at least twice a week) and two persons with sedentary lifestyles were included. In the Bone-Albumin group 11 professional athletes, seven recreational athletes and two persons with sedentary lifestyles were included. Patients received treatment 24 ± ten weeks and 14 ± five weeks after the injury in the control and Bone-Albumin groups, respectively.
At the examination date six weeks post-operatively, both treatment groups were still under recovery from the operation itself, and overall knee function was compromised as evidenced by the IKDC and VISA scores, less so in the Lysholm activity scale (Fig. 3). However, both the IKDC and VISA scores were significantly lower in the control than in the Bone-Albumin group (Fig. 3). Pain at the donor site was significantly lower in the treatment group both at kneeling and crouching, while standing pain was negligible in both groups (Fig. 3).
Functional knee scores. Panel a shows IKDC, panel b shows VISA and panel c shows Lysholm activity score results at six weeks and six months post operatively, each with a potential maximum value of 100. Panel d shows Knee pain at six weeks and six months after BTB surgery. Visual analog scale of knee pain on a 0–10 scale in standing, kneeling and crouching positions. * p < 0.05 between the two treatment groups
At six months, when the tendon is considered healed and the patients generally return to their previous sport activity levels, the knee functional scores were close to normal (IKDC control: 85 ± 2 vs treated: 91 ± 2, Lysholm control: 96 ± 1 vs. treated: 97 ± 1, VISA control: 94 ± 1 vs. treated: 96 ± 2) with a slight but statistically significant advantage for Bone-Albumin in the IKDC score (Fig. 3). At this time point, donor site pain generally starts to take precedence over other symptoms. Indeed, although standing and crouching pain subsided in both groups, kneeling pain was prominent in the controls but significantly lower in the treatment group (VAS control: 3.70 ± 0.33 vs. treated: 1.30 ± 0.34, p < 0.01) (Fig. 3).
Bone density and the remaining bone defect were measured with computed tomography. In the patella, defects filled with Bone-Albumin had significantly smaller bone void and higher density values than the controls, which were filled with blood clot only (Fig. 4). The tibia was either filled with the available autograft only or autograft mixed with Bone-Albumin. Since the volume of the available autograft bone was variable, the completeness of the filling was scored by the operator on a scale of unfilled, moderately, well, or completely filled defects. At six-month follow-up, the completeness of the filling was not correlated with the bone density in the control group (Table 1). In the treatment group, the level was always ‘complete’, because Bone-Albumin filling was used to top up the defects. After six months, no significant bone void was detected in either groups at the tibia site, but Bone-Albumin augmentation of the autograft resulted in a significantly denser new bone than that filled with autograft only (605 ± 41 vs. 407 ± 48 HU, p < 0.05, respectively) (Fig. 5).
Morphometric measurements of the patellar site. Panel a shows remaining bone void, while panel b shows density of the newly formed bone at six months post-operatively. Panels c-f show representative CT images from the patella. Panel c shows 3D reconstruction and panel d shows an axial slice of the control group. Panel e shows 3D reconstruction and panel f shows an axial slice of the Bone-Albumin treated group. There is a significantly lower remaining defect size with a significantly denser remodeled bone in the Bone-Albumin group, indicating a nearly complete tissue healing. * p < 0.05 between the two treatment groups
Density measurements of the tibial donor site. Panel a shows the density of autologous bone filling compared to Bone-Albumin + autologous bone. Significantly higher density is observed in the Bone-Albumin group. Panel b and c show axial CT slices of the tibial donor site filled with autologous bone and Bone-Albumin + autologous bone, respectively (regions of interest are circled with dashed lines). * p < 0.05 between the two treatment groups
Discussion
Pain and disability associated with the donor site can be so severe that it seriously limits the application of bone autografting, especially in cases where the indication is not life-threatening [7]. BTB is a well-known and widely used technique for ACL reconstruction and, despite the good overall clinical outcome, donor site pain is limiting its use. The key factor in donor site morbidity is not functional loss, since much of the bone stock is rebuilt in a longer period of time, but rather the slow or inadequate bone buildup underneath. The low amount of autologous cancellous bone usually available during BTB reconstruction can be enough to partly fill the tibial defects but not both patella and tibia. Moreover, in the present study the amount of leftover cancellous bone was sufficient only in 58 % of the cases (11 complete or substantial filling from 19 cases) to fill one defect, while the other was left open, which is clearly suboptimal. Persistent pain at the donor site is probably related to continuous disturbance of the periosteum caused by slow tissue remodeling. Thus, tissue-engineering strategies in ACL surgery must address the problem of pain and healing time rather than bone strength or bone volume, as these are considered adequately healed even if left untreated. In the present study, donor site pain was significantly less already after six weeks post-operatively if Bone-Albumin was used to fill the bone defects. In addition, Bone-Albumin filling resulted in better bone morphology, since after six months smaller remaining bone defect was seen at the patellar site and denser new bone was observed at the patellar and tibial harvesting sites.
Several techniques were investigated that aimed to improve donor site healing in BTB surgery. In a prospective randomized study from Cervellin it was described that platelet rich plasma (PRP) filling of both sites was significantly better at 12 month post-op [17]. A similar study has recently reported faster recovery of the donor site with plasma rich in growth factors, another blood-serum-based therapeutic approach [18]. These observations confirm the findings from our present study, since all three interventions achieved better healing with a serum-based technology. However, it seems from the results that Bone-Albumin achieved an even better and earlier bone remodeling than PRP or PRGF, which provide only osteoinduction, but no osteoconduction.
One very important question about bone tissue substitutes is whether they induce ectopic bone formation. Bone morphogenetic proteins (BMP), for example, are available in recombinant form, but recent literature data show ectopic bone formation as a potential side effect of the treatment, which dampened enthusiasm among clinicians [19, 20]. It is important to note that the dosage of BMP has not been well studied, though allogeneic bone substitutes may contain these proteins at physiological levels. Although in the present study we didn’t use specific growth factors, the fact that albumin induces stem cell proliferation on the surface of the grafts raises the question of ectopic bone formation. After filling the donor sites with Bone-Albumin, CT scans were taken on the first post-operative week to visualize the defects. These scans showed the defects to be completely filled, and some stray graft fragments were also visible in the surrounding connective tissue. On the CT scans taken at six months, we observed no ectopic bone deposition in any of the cases, meaning that the dislocated allograft fragments had been completely resorbed and bone formation was induced only within the bone defect site boundaries.
Interestingly, the addition of Bone-Albumin to the autologous cancellous bone resulted in denser new bone buildup at the tibial site. Since density is correlated with the mineralization status, it is possible that Bone-Albumin augmented autografts resulted in faster ossification compared to autografts alone. This suggests the active role of serum albumin in bone remodeling, however, it is confined to the physiological bone shape as uncontrolled or sustained bone growth was not observed throughout the study.
Even though serum albumin is a well-described protein, only a limited number of scientific studies investigate its effects on bone formation. One series of studies showed that albumin production is increased locally after bone trauma [21]. Moreover, it has been shown that albumin enhances osteoblast proliferation [22]. In addition, albumin was shown to increase stem cell adhesion to various biomaterial surfaces, creating a convenient milieu for further cell function [23–25]. These studies further suggest that locally increased albumin concentration may assist the endogenous progenitor population. Since albumin dissolves easily, stem cell recruitment ceases quite quickly. However, this time seems long enough to increase the number of active cells in the injury site, resulting in faster ossification.
In conclusion, results from the present study showed that kneeling pain, a most disturbing long-term side effect of BTB harvesting in a young and active patient population, is significantly less if the bone buildup in the patella is augmented by serum albumin-coated bone allografts. The bone substitution technique resulted in faster and more complete ossification, producing superior clinical outcome without ectopic bone deposition compared to standard surgical protocol. Since Bone-Albumin proved its safety and efficacy in the present study, the grafting technique could be extended to other clinical situations, where a fully rebuilding bone tissue is the ultimate goal.
References
Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE Jr (2004) Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. Am J Sports Med 32(8):1986–1995
Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M (2005) A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med 33(9):1337–1345. doi:10.1177/0363546504274145
Holm I, Oiestad BE, Risberg MA, Aune AK (2010) No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med 38(3):448–454. doi:10.1177/0363546509350301
Meuffels DE, Poldervaart MT, Diercks RL, Fievez AW, Patt TW, Hart CP, Hammacher ER, Meer F, Goedhart EA, Lenssen AF, Muller-Ploeger SB, Pols MA, Saris DB (2012) Guideline on anterior cruciate ligament injury. Acta Orthop 83(4):379–386. doi:10.3109/17453674.2012.704563
Kim SJ, Lee SK, Choi CH, Kim SH, Jung M (2014) Graft selection in anterior cruciate ligament reconstruction for smoking patients. Am J Sports Med 42(1):166–172. doi:10.1177/0363546513505191
Reinhardt KR, Hetsroni I, Marx RG (2010) Graft selection for anterior cruciate ligament reconstruction: a level I systematic review comparing failure rates and functional outcomes. Orthop Clin North Am 41(2):249–262. doi:10.1016/j.ocl.2009.12.009
Kraeutler MJ, Bravman JT, McCarty EC (2013) Bone-patellar tendon-bone autograft versus allograft in outcomes of anterior cruciate ligament reconstruction: a meta-analysis of 5182 patients. Am J Sports Med 41(10):2439–2448. doi:10.1177/0363546513484127
Feller JA, Webster KE (2003) A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med 31(4):564–573
Beynnon BD, Johnson RJ, Fleming BC, Kannus P, Kaplan M, Samani J, Renstrom P (2002) Anterior cruciate ligament replacement: comparison of bone-patellar tendon-bone grafts with two-strand hamstring grafts. A prospective, randomized study. J Bone Joint Surg Am 84-A(9):1503–1513
Holzmann P, Niculescu-Morzsa E, Zwickl H, Halbwirth F, Pichler M, Matzner M, Gottsauner-Wolf F, Nehrer S (2010) Investigation of bone allografts representing different steps of the bone bank procedure using the CAM-model. Altex 27(2):97–103
Leitgeb J, Kottstorfer J, Schuster R, Kovar FM, Platzer P, Aldrian S (2014) Primary anterior cruciate ligament reconstruction in athletes: a 5-year follow up comparing patellar tendon versus hamstring tendon autograft. Wien Klin Wochenschr 126(13–14):397–402. doi:10.1007/s00508-014-0550-4
Kartus J, Movin T, Karlsson J (2001) Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy 17(9):971–980. doi:10.1053/jars.2001.28979
Skaliczki G, Schandl K, Weszl M, Major T, Kovacs M, Skaliczki J, Szendroi M, Dobo-Nagy C, Lacza Z (2013) Serum albumin enhances bone healing in a nonunion femoral defect model in rats: a computer tomography micromorphometry study. Int Orthop 37(4):741–745. doi:10.1007/s00264-012-1770-8
Horvathy DB, Vacz G, Szabo T, Szigyarto IC, Toro I, Vamos B, Hornyak I, Renner K, Klara T, Szabo BT, Dobo-Nagy C, Doros A, Lacza Z (2015) Serum albumin coating of demineralized bone matrix results in stronger new bone formation. J Biomed Mater Res B Appl Biomater. doi:10.1002/jbm.b.33359
Weszl M, Skaliczki G, Cselenyak A, Kiss L, Major T, Schandl K, Bognar E, Stadler G, Peterbauer A, Csonge L, Lacza Z (2012) Freeze-dried human serum albumin improves the adherence and proliferation of mesenchymal stem cells on mineralized human bone allografts. J Orthop Res 30(3):489–496
Klara T, Csonge L, Janositz G, Csernatony Z, Lacza Z (2014) Albumin-coated structural lyophilized bone allografts: a clinical report of 10 cases. Cell Tissue Bank 15(1):89–97. doi:10.1007/s10561-013-9379-8
Cervellin M, de Girolamo L, Bait C, Denti M, Volpi P (2012) Autologous platelet-rich plasma gel to reduce donor-site morbidity after patellar tendon graft harvesting for anterior cruciate ligament reconstruction: a randomized, controlled clinical study. Knee Surg Sports Traumatol Arthrosc 20(1):114–120. doi:10.1007/s00167-011-1570-5
Seijas R, Rius M, Ares O, Garcia-Balletbo M, Serra I, Cugat R (2015) Healing of donor site in bone-tendon-bone ACL reconstruction accelerated with plasma rich in growth factors: a randomized clinical trial. Knee Surg Sports Traumatol Arthrosc 23(4):991–997. doi:10.1007/s00167-013-2787-2
Even J, Eskander M, Kang J (2012) Bone morphogenetic protein in spine surgery: current and future uses. J Am Acad Orthop Surg 20(9):547–552. doi:10.5435/JAAOS-20-09-547
Fu R, Selph S, McDonagh M, Peterson K, Tiwari A, Chou R, Helfand M (2013) Effectiveness and harms of recombinant human bone morphogenetic protein-2 in spine fusion: a systematic review and meta-analysis. Ann Intern Med 158(12):890–902. doi:10.7326/0003-4819-158-12-201306180-00006
Yamaguchi M, Igarashi A, Misawa H, Tsurusaki Y (2003) Enhancement of albumin expression in bone tissues with healing rat fractures. J Cell Biochem 89(2):356–363. doi:10.1002/jcb.10510
Ishida K, Yamaguchi M (2004) Role of albumin in osteoblastic cells: enhancement of cell proliferation and suppression of alkaline phosphatase activity. Int J Mol Med 14(6):1077–1081
Liu X, Zhou X, Li S, Lai R, Zhou Z, Zhang Y, Zhou L (2014) Effects of titania nanotubes with or without bovine serum albumin loaded on human gingival fibroblasts. Int J Nanomedicine 9:1185–1198. doi:10.2147/IJN.S55514
Bernards MT, Qin C, Jiang S (2008) MC3T3-E1 cell adhesion to hydroxyapatite with adsorbed bone sialoprotein, bone osteopontin, and bovine serum albumin. Colloids Surf B: Biointerfaces 64(2):236–247. doi:10.1016/j.colsurfb.2008.01.025
Horvathy DB, Vacz G, Cselenyak A, Weszl M, Kiss L, Lacza Z (2013) Albumin-coated bioactive suture for cell transplantation. Surg Innov 20(3):249–255. doi:10.1177/1553350612451353
Acknowledgments
This study was supported by a research sponsorship grant of OrthoSera GmbH to Semmelweis University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
ZL declares conflict of interest as the funder and CEO of the start-up company OrthoSera GmbH, which holds a patent for Bone-Albumin.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards (ALLO-2013-02).
Rights and permissions
About this article
Cite this article
Schandl, K., Horváthy, D.B., Doros, A. et al. Bone-Albumin filling decreases donor site morbidity and enhances bone formation after anterior cruciate ligament reconstruction with bone-patellar tendon-bone autografts. International Orthopaedics (SICOT) 40, 2097–2104 (2016). https://doi.org/10.1007/s00264-016-3246-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3246-8