Abstract
Purpose
To determine whether the use of plasma rich in growth factors accelerates healing of the donor site in bone-tendon-bone anterior cruciate ligament (ACL) reconstruction (patellar graft). The use of the patellar graft presents post-operative problems such as anterior knee pain, which limits its use and leads to preference being taken for alternative grafts.
Methods
A double-blind, randomized, clinical trial was performed comparing two groups of patients who underwent ACL reconstruction using patellar tendon graft and comparing the use of plasma rich in growth factors at the donor site after graft harvest in terms of local regeneration by ultrasound assessment.
Results
The plasma rich in growth factors group shows earlier donor site regeneration in comparison with the control group (2 months earlier), with significant differences in the first 4 months of the follow-up.
Conclusion
The application of plasma rich in growth factors shows accelerated tissue regeneration processes with respect to the control group. This fact, together with the previously published with similar conclusions, can create a knowledge basis in order to set out new recovery guidelines following ACL reconstruction.
Level of evidence
Therapeutic study, Level I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee injuries account for a significant group of sports pathologies. One of the utmost importance and severity is anterior cruciate ligament (ACL) rupture, which accounts for up to 50 % of these injuries [19]. In the United States alone, it is estimated that 50,000 patients undergo surgery every year due to this lesion [17]. ACL rupture renders the athlete incapable of playing soccer due to the instability that this rupture entails. Thus, soccer players who suffer from ACL injuries frequently undergo surgery with the notion of an earlier return to play [17].
The bone-patellar tendon-bone ligament (patellar graft) is a widely used autograft for this type of surgery [37]. Donor site complications include anterior knee pain, with figures that vary from 4–60 % [8]. The central third of the patellar ligament, with tibial and patellar bone blocks, is employed as an ACL and recognized by the popular nomenclature “patellar graft” or “bone-tendon-bone” (BTB).
BTB-ACL reconstruction is associated with anterior knee pain in 4 % to 60 % of the patients; this could be improved by adhering to contemporary recovery precepts, thereby reducing post-operative anterior knee pain at the harvest site. There is an existent relationship between donor site defect healing time and anterior knee pain, leading to a rise in the use of alternatives in previous years due to donor site pain after patellar tendon graft harvest. The empty space or gap that is left after graft harvest has been defined as the cause of persistent discomfort and pain at the donor site for several months [46]. However, the usefulness of BTB graft for anterior cruciate ligament injuries has previously been studied [45].
In order to accelerate the healing process, autologous plasma rich in growth factors (PRGF®) allows for a new possibility in the preventive treatment of these complications. PRGF are biologically enhanced peptides, which have been shown to accelerate tissue repair [41, 43]. Studies such as those carried out by Orrego et al. [39], Radice et al. [40] or a previous work by our research group [44] have observed accelerated ligamentous tissue maturation when compared to a control group.
Surgeries that have included the application of PRGF have shown accelerated tissue maturation processes [15, 39, 40, 42, 44]. Orrego et al., Radice et al. and Seijas et al. showed these accelerated processes in ACL reconstruction [39, 40, 44], whereas Sanchez et al. [42] did the same with Achilles tendon and athletes. Anoka et al. [6] reviewed the use of growth factors and observed an augmented healing process in medial collateral ligament of the knee.
The persistent donor site gap after harvesting a central third patellar tendon autograft appears to be correlated with anterior knee pain, suggesting that if PRGF can in fact accelerate the maturation process, one could achieve tissue less susceptible to morbidity, and by doing so, one could appreciate improved outcomes for the B-PT-B ACL reconstruction technique [46].
Shelbourne et al. [46] discussed the donor site defect, reporting discomfort and pain at the anterior knee. Following the abovementioned studies [39, 40, 44], the hypothesis of the present study is that the application of PRGF accelerates donor site maturation in BTB-ACL reconstruction, measured with ultrasound.
Materials and methods
A prospective, randomized, double-blinded, clinical trial with two groups of patients was performed, comparing the treatment group (PRGF®) with the control group. Forty-three patients undergoing anterior cruciate ligament reconstruction (following the BTB technique) were included in the trial.
All patients included had suffered an acute injury of the ACL and presented with rotational instability of the knee, both symptomatically and upon physical examination, with normal joint mobility and without bone oedema. The proposed treatment for all patients was reconstructive surgery scheduled 6 weeks post-injury.
Patients were treated in 2009 with a follow-up period of 2 years. Inclusion criteria were age between 18- and 65-year old; ACL complete rupture; oral and written comprehension of Spanish in order to complete the questionnaires; first surgical procedure in the evaluated knee as well as understanding and accepting their enrolment in the present study signing an informed consent. Exclusion criteria were partial ACL rupture; revision surgery (graft rupture); concomitant diseases (infections, oncological, collagen, soft tissue or haematological); inability to undergo an MRI (either personal or medical reasons); unwilling to complete the protocol follow-up and subjects that during the study suffered from new knee injuries.
After selection and enrolment, all subjects were automatically randomized into group A or B using the function RANDOM from Microsoft Excel, (Microsoft Office 2007).
Once assigned to a group, the only difference in the treatment between patients was at the end of surgery, when growth factors were either applied or not, in accordance with their randomly assigned group. The rest of the treatment including surgery, follow-up, control periods and additional tests was synonymous for all patients included in the trial.
The patellar tendons were examined by ultrasonography before and after the ACL surgery by the same examiner (MR). The study was performed with the equipment “ACUSON Antares (Siemens, Erlangen, Germany)” with a multifrequency linear probe, between 7.27 and 11.43 MHz.
Both tendons were examined before surgery to rule out injuries in the patellar tendon and again at 4, 8, 16, 24, 36, 48 and 96 weeks after surgery, measuring the same parameters each time; vascularization of the tendon and the state of repair at the tendon graft harvest site.
The Öhberg scale was used to assess vascularization, in which the level 0 was considered as the non-existence of vessels, level 1 the presence of one or more vessels, level 2 as two or more vessels, level 3 as three or more and level 4 as four or more vessels [38], using Doppler ultrasound.
Due to the lack of validated scales regarding donor site or tendinous tissue, a new scale was created for the present study using ultrasonography (the Rius classification). To achieve this, a previous validation was performed with 10 cases being evaluated by two independent radiologists (ultrasound specialized) at the same timings as in the present work (4, 8, 16, 24, 36, 48 weeks), finding absolute coincidence in 57 out of 60 performed studies (95 %).
The repair process at the donor site was evaluated with stages A to D, where A represented the absence of repair, B a start in the repair process with less than 50 % scar tissue, C advanced repair process with more than 50 % repaired tissue and stage D when complete repair was observed. The presence of a greater number of echoes within the donor site gap indicates a more advanced state of repair.
All patients included in this trial underwent an ACL reconstruction with autologous patellar graft performed by the same surgical team. They all followed the same rehabilitation programme and underwent the same follow-up with the same surgeon.
At the end of the surgery, plasma rich in growth factors (PRGF®) (technique described by Anitua et al. [5]) was injected at the donor site for patients enrolled in group A. After skin closure, the graft harvest gap was located by palpation and 1 cc of PRGF® was injected into the patellar bone gap. The same procedure was performed in the tibial bone gap, and finally from the centre of the harvest gap, 1 cc was injected with the needle directed cranially and 1 cc caudally in the tendinous area, under the paratenon, which had previously been sutured. Patients in group B did not receive the injection of PRGF® at the end of the surgery.
Patients involved in the present clinical trial signed an informed consent in order to participate and were aware that they would randomly enter either the PRGF group or the control group. To avoid bias from patients, 20 cc of preanaesthetic peripheral blood was extracted from all patients. Once anesthetized and shortly before the end of surgery, a member of the team consulted the group to which the patient had been assigned, previously randomized using an Excel program. Ultrasound assessments were performed by a blinded consultant, unaware of which group patients belonged to.
Given that patients were under anaesthesia at the time of PRGF application, there was no way of them knowing the group to which they had been randomized.
Furthermore, the patient group that received PRGF did not notice any differences with the control group given that the puncture signs remained mixed with those belonging to the surgery itself. Questionnaires were filled out by the patient and collected by a third party impartial to the study, thus guaranteeing the definition of the present clinical trial, randomized and double-blinded.
This trial was set out as a clinical trial and approved by the Ethics Committee at Hospital Quirón Barcelona. The ethical number of the present clinical trial was CEIC 09-45, following the guidelines of Royal Decree RD 223/2004 from the Ministry of Health, Social Services and Equality.
Statistical analysis
A sample size determination of 40 patients (20 per group) was estimated to detect with a 70 % power as significant an odds ratio of 3.5, using χ2 test with a 5 % statistical significance. Data were collected from an extra 10 % (four patients), leaving 23 and 21 patients after randomization. However, three patients were lost during follow-up, with the final groups consisting of 22 and 19 patients, respectively. Taking into consideration that a possible loss would occur during the follow-up, an extra 10 % (four patients) was added to the estimated sample size. As expected, one patient was lost during the follow-up. Therefore, the final sample size included in the present study was of 43 subjects.
The development of the association between tendon maturity and treatment during the follow-up was evaluated by estimating adjusted odds ratios using an ordinal logistic regression with the GEE method.
The ultrasound measurements were performed by the same physician and are the result of three measurements that were sequentially carried out the same day and repeated at each study period (4, 8, 16, 24, 36, 48 and 96 weeks) after surgery.
The time required for each individual to reach complete ultrasound tendon maturity was analysed, that is, when they reached maturity categorized as stage “D”. The existence of a link between PRGF and the time elapsed was investigated. Identifying the exact moment that maturity takes place can be challenging, and to that end, time interval between the last visit (at which point maturity had not yet completed) and the first visit (that presented complete maturity) was studied. To analyse differences between treatments, log-rank test was used.
Results
Forty-three patients were included in the study. Group A (with PRGF®) n = 23 and Group B (control without PRGF®) n = 20. One patient was excluded from the study for failing to meet the follow-up criteria due to a change of residence.
The distribution of patients in both groups was randomly executed, showing no significant differences between age, sex, occupation, education, smoking habits or sport activity level.
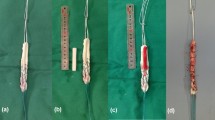
Data obtained by ultrasound on the degree of maturity at the donor site were presented in Table 1 and Fig. 1.
Individuals with PRGF were more associated with higher scores of maturity than individuals without PRGF in the fourth month of the follow-up (p = 0.0037). No differences at the other follow-up times were found. The speed at which maturity takes place is accelerated by the use of PRGF.
With reference to the Ohberg scale assessment, only a few cases of vascular increase were detected by Doppler ultrasound. The only month that had some variability in the Ohberg variable was month two; however, no statistically significant association was found (n.s.).
Discussion
The most important finding of the present study was the accelerated maturation process at the patella donor site in ACL reconstruction (bone-patellar tendon-bone graft) using PRGF.
Employing ultrasonography (US) for evaluation of the patellar tendon has been described in different works for determining tendon defects [22] and concluded that these exams present comparable results with MRI. Therefore, US was the chosen imaging method in the present study due its simplicity, accessibility and patients’ acceptance.
Complete maturity of the patellar tendon defect (grade D of the Rius classification) begins in the fourth month (33 % of patients), over 90 % of cases at 9 months and 100 % at 1 year of the follow-up, as can be observed in the present study from a global perspective (both groups). As previous studies have pointed out, regarding the use of ultrasound over the patellar area in this type of surgery, there are several different degrees of maturity and/or healing around a year after surgery [11].
Several authors have studied patellar tendon healing times; MRI studies claimed that the defect closed between 8 months and 2 years post-operatively [9, 12, 36]. On the other hand, the histological study carried out by Nixon et al. [36] reported the presence of scar tissue indistinguishable from normal tissue at 2 years after surgery. Along the same lines, Adriani et al. [1] noted that surgical closure of the patellar paratenon defect generated an ultrasonographic image identical to normal tendon a year after surgery.
Both the ultrasound study by Adriani et al. and the MRI study by Nixon report a thickening of the tendon that was normalizing as the year progressed, monitoring with a series of images at 3, 6, 9 and 12 months [1, 36]. Other authors, such as Meisterling et al. and Karns et al., reported in their studies slightly extended periods, 2.5 and 4 years, respectively, to achieve complete closure of the defect [21, 35]. In contrast, Lidén et al. evidenced a visible defect at 10 years with MRI, with thickening of the patellar tissue [30].
Different animal studies both in goats and dogs showed a structurally different tissue from normal, but the lack of intraoperative closure of the paratenon could be an influence for the persistence of the tendon defects [26, 29]. CT and MRI studies with a 2-year follow-up evidenced donor site defects [23–25].
In this line, Liu et al. [31] published patellar defects that persisted after 14 years. Other authors concluded that although the defects could persist for long periods, these were also reduced with time [10, 24].
Seriated examinations were performed at 4, 8, 12, 24, 48 and 96 weeks in our series, evaluating at which point the donor site defect closed.
PRGF has been proposed as a tendon repair technique due to its numerous bioactive molecules involved in the ligament and tendon repair process [42].
Almeida et al. [13] studied the use of PRGF in patellar tendon healing following ACL reconstruction and observed a positive effect after 6 months and a decrease in donor site pain, measured with MRI instead of US as in the present study.
Culture studies with the use of PRGF have shown a cellular increase in tendon tissues and especially an increase in collagen levels [4, 14, 20]. Animal studies have demonstrated an increase in cell density, neovascularization and resistance force between 30 and 65 % according to studies [2, 3, 7] with an improvement within biomechanical properties in the medial collateral ligament in its early stages [18, 47]. The study by Xie et al. [48] performed with dogs suggested a role of PRGF in promoting synthesis of extracellular matrix after ACL reconstruction. Along the same lines, the study by Fernandez-Sarmiento et al. [15] showed histological changes at eight weeks, consistent with an accelerated early healing process in repaired Achilles tendons in sheep after surgical disruption and repair treated with PRGF.
Studies by Kondo et al. [27] also demonstrated that the application of growth factors in ACL elongations achieved improved tension compared with patients where growth factors were not applied.
Other studies have shown growth factors to be useful in achieving early mobility and earlier return to sports in Achilles tendons and rotator cuff repair [28, 42]. Meanwhile, Foster et al. [16] published their series on medial collateral ligament injuries in soccer players with 27 % reductions to recovery times.
The study group by Lyras et al. [32–34] has published several works on donor site in which they evidence that studies in rabbits using PRGF enable faster tendon tissue regeneration in patellar tendon defects.
In the present study, it was observed with US that the group to which PRGF had been applied advanced towards stages of repair or maturity at a faster rate than the control group. This increased speed can be observed at the fourth month with complete maturity, being statistically significant (52 vs. 10 %, p = 0.0037).
This difference decreases in the following months with no significant differences. It is therefore evident that the use of PRGF accelerates the process of maturity substantiated by ultrasonographic studies.
No degrees of hypervascularization of the patellar tendon during its different stages of regeneration were observed with the Doppler ultrasound evaluations in the present study, except for some rare isolated case of grades 1 and 2 at some points of the follow-up, for which reason Doppler ultrasound assessment could be considered as useless for diagnosis or evaluation of the regenerated patellar donor site. Other more precise techniques, such as angiography, would probably show the condition of hypervascularity caused by tissue maturation.
As the study of Shelbourne et al. [46] confirmed, there is a clear relationship between the patellar defect and discomfort and pain at the anterior knee. The present study aimed to evaluate whether there were differences within healing time with PRGF, which could lead to less discomfort and pain. A major problem regarding ACL reconstruction with patellar graft is this anterior knee pain; therefore, a faster healing time could allow a quick return to the preinjury level of function.
Some limitations must be taken into consideration when reviewing the current manuscript. Ours is a single-centre study with a limited number of patients. Furthermore, evaluation was performed with a non-validated ultrasonographic evaluation scale; however, no other evaluating scales are currently available. In addition, the use of magnetic resonance imaging could have increased the knowledge of tissue and bone regeneration; however, the economic restrictions for this test made it impossible to include it in the study design. Although ultrasound adds the limitation of being examiner-dependent, a recognized and expert physician trained for over 20 years in muscular ultrasonography was asked to perform the tendinous ultrasonography. Nevertheless, there is a comprehensible technical bias that could have been reduced with the participation of two or more ultrasound experts. Unfortunately, due to structural and economic reasons, this was not possible in the present study. Further multi-centre clinical trials should be carried out in order to draw clearer conclusions.
Conclusion
In conclusion, the present study shows that the use of PRGF accelerated the maturation process at the donor site. If a reduction in discomfort within the anterior knee in early stages is proven, as previous studies regarding the application of PRGF in ACL graft have observed, one of the most frequent complications could be better controlled. The present study does not aim to evaluate an improvement in functionality of the applied graft, as PRGF was not injected into the graft, and thus, there is no reason why time of return to play should vary. The use of PRGF has been proven to accelerate the process of tissue regeneration. Considering the current results combined with those from previous studies where PRGF was applied, future studies could benefit from the demonstrated accelerated maturation times, thus providing shorter rehabilitation periods and an earlier return to play.
References
Adriani E, Mariani PP, Maresca G, Santori N (1995) Healing of the patellar tendon after harvesting of its mid-third for anterior cruciate ligament reconstruction and evolution of the unclosed donor site defect. Knee Surg Sports Traumatol Arthrosc 3(3):138–143
Anderson K, Seneviratne AM, Izawa K, Atkinson BL, Potter HG, Rodeo SA (2001) Augmentation of tendon healing in an intraarticular bone tunnel with use of a bone growth factor. Am J Sports Med 29:689–698
Anitua E, Sanchez M, Nurden AT, Zalduendo M, de la Fuente M, Orive G et al (2006) Autologous fibrin matrices: a potential source of biological mediators that modulate tendon cell activities. J Biomed Mater Res A 77(2):285–293
Anitua E, Andía I, Sanchez M, Azofra J, del Mar Zalduendo M, de la Fuente M et al (2005) Autologous preparations rich in growth factors promote proliferation and induce VEGF and HGF production by human tendon cells in culture. J Orthop Res 23(2):281–286
Anitua E (1999) Plasma rich in growth factors: preliminary results of use in the preparation of sites for implants. Int J Oral Maxillofac Implants 14:529–535
Anoka N, Nyland J, McGinnis M, Lee D, Doral MN, Caborn DN (2012) Consideration of growth factors and bio-scaffolds for treatment of combined grade II MCL and ACL injury. Knee Surg Sports Traumatol Arthrosc 20(5):878–888
Aspenberg P, Virchenko O (2004) Platelet concentrate injection improves Achilles tendon repair in rats. Acta Orthop Scand 75:93–99
Beaufils P, Gaudot F, Drain O, Boisrenoult P, Pujol N (2011) Mini-invasive technique for bone patellar tendon bone harvesting: its superiority in reducing anterior knee pain following ACL reconstruction. Curr Rev Musculoskelet Med 4(2):45–51
Berg EE (1992) Intrinsic healing of a patellar tendon donor site defect after anterior cruciate ligament reconstruction. Clin Orthop Relat Res 278:160–163
Bernicker JP, Haddad JL, Lintner DM, DiLiberti TC, Bocell JR (1998) Patellar tendon defect during the first year after anterior cruciate ligament reconstruction: appearance on serial magnetic resonance imaging. Arthroscopy 14(8):804–809
Brandsson S, Faxen E, Eriksson BI, Kälebo P, Swärd L, Lundin O, Karlsson J (1998) Closing patellar tendon defects after anterior cruciate ligament reconstruction: absence of any benefit. Knee Surg Sports Traumatol Arthrosc 6(2):82–87
Coupens SD, Yates CK, Sheldon C, Ward C (1992) Magnetic resonance imaging evaluation of the patellar tendon after use of its central one-third for anterior cruciate ligament reconstruction. Am J Sports Med 20(3):332–335
De Almeida AM, Demange MK, Sobrado MF, Rodrigues MB, Pedrinelli A, Hernandez AJ (2012) Patellar tendon healing with platelet-rich plasma: a prospective randomized controlled trial. Am J Sports Med 40(6):1282–1288
De Mos M, van der Windt A, Jahr H et al (2008) Can platelet-rich plasma enhance tendon repair? A cell culture study. Am J Sports Med 36:1171–1178
Fernandez-Sarmiento JA, Dominguez JM, Granados MM, Morgaz J, Navarrete J, Carrillo JM et al (2013) Histological study of the influence of plasma rich in growth factors (ORGF) on the healing of divided Achilles tendons in sheep. J Bone Joint Surg Am 95(3):246–255
Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA (2009) Platelet-rich plasma. From basic science to clinical applications. Am J Sports Med 37:2259–2272
Franck CB, Jackson DW (1997) The science of reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am 79(10):1556–1576
Hildebrand KA, Woo SL-Y, Smith DW et al (1998) The effects of platelet-derived growth factor-BB on healing of the rabbit medial collateral ligament. Am J Sports Med 26:549–554
Insall JN, Scott WN (2004) Surgery of the knee, 3rd ed. Churchill Livingstone, Philadelphia, 600–650
Kajikawa Y, Morihara T, Sakamoto H et al (2008) Platelet-rich plasma enhances the initial mobilization of circulation-derived cells for tendon healing. J Cell Physiol 215:837–845
Karns DJ, Heidt RS Jr, Holladay BR, Colosimo AJ (1994) Case report: revision anterior cruciate ligament reconstruction. Arthroscopy 10(2):148–157
Kartus J, Ejerhed L, Sernert N, Brandsson S, Karlsson J (2000) Comparison of traditional and subcutaneous patellar tendon harvest. A prospective study of donor site-related problems after anterior cruciate ligament reconstruction using different graft harvesting techniques. Am J Sports Med 28:328–335
Kartus J, Movin T, Papadogiannakis N, Christensen LR, Lindahl S, Karlsson J (2000) A radiographic and histologic evaluation of the patellar tendon after harvesting its central third. Am J Sports Med 28(2):218–226
Kartus J, Lindahl S, Stener S, Eriksson BI, Karlsson J (1999) Magnetic resonance imaging of the patellar tendon after harvesting its central third: a comparison between traditional and subcutaneous harvesting techniques. Arthroscopy 15:587–593
Kartus J, Stener S, Lindahl S, Engström B, Eriksson BI, Karlsson J (1997) Factors affecting donor-site morbidity after anterior cruciate ligament reconstruction using bone-patellar tendon-bone autografts. Knee Surg Sports Traumatol Arthrosc 5:222–228
Kohn D, Sander-Beuermann A (1994) Donor-site morbidity after harvest of a bone-tendon-bone patellar tendon autograft. Knee Surg Sports Traumatol Arthrosc 2(4):219–223
Kondo E, Yasuda K, Yamanaka M, Minami A, Tohyama H (2005) Effects of administration of exogenous growth factors on biomechanical properties of the elongation-type anterior cruciate ligament injury with partial laceration. Am J Sports Med 33:188–196
Kovacevic D, Rodeo SA (2008) Biological augmentation of rotator cuff tendon repair. Clin Orthop 466:622–633
LaPrade RF, Hamilton CD, Montgomery RD, Wentorf F, Hawkins HD (1997) The reharvested central third of the patellar tendon. A histologic and biomechanical analysis. Am J Sports Med 25(6):779–785
Lidén M, Ejerhed L, Sernert N, Bovaller A, Karlsson J, Kartus J (2006) The course of the patellar tendon after reharvesting its central third for ACL revision surgery: a long-term clinical and radiographic study. Knee Surg Sports Traumatol Arthrosc 14(11):1130–1138
Liu SH, Hang DW, Gentili A, Finerman GA (1996) MRI and morphology of the insertion of the patellar tendon after graft harvesting. J Bone Joint Surg Br 78(5):823–826
Lyras DN, Kazakos K, Verettas D, Chronopoulos E, Folaranmi S, Agrogiannis G (2010) Effect of combined administration of transforming growth factor-b1 and insulin-like growth factor I on the mechanical properties of a patellar tendon defect model in rabbits. Acta Orthop Belg 76(3):380–386
Lyras DN, Kazakos K, Verettas D, Polychronidis A, Tryfonidis M, Botaitis S et al (2009) The influence of platelet-rich plasma on angiogenesis during the early phase of tendon healing. Foot Ankle Int 30(11):1101–1106
Lyras DN, Kazakos K, Verettas D, Botaitis S, Agrogiannis G, Kokka A et al (2009) The effect of platelet-rich plasma gel in the early phase of patellar tendon healing. Arch Orthop Trauma Surg 129(11):1577–1582
Meisterling RC, Wadsworth T, Ardill R, Griffiths H, Lane-Larsen CL (1993) Morphologic changes in the human patellar tendon after bone-tendon-bone anterior cruciate ligament reconstruction. Clin Orthop Relat Res 289:208–212
Nixon RG, SeGall GK, Sax SL, Cain TE, Tullos HS (1995) Reconstitution of the patellar tendon donor site after graft harvest. Clin Orthop Relat Res 317:162–171
Noyes FR, Butler DL, Grood ES (1984) Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am 66(3):344–352
Ohberg L, Alfredson H (2002) Ultrasound guided sclerosis of neovessels in painful chronic Achilles tendinosis: pilot study of a new treatment. Br J Sports Med 36(3):173–177
Orrego M, Larrain C, Rosales J, Valenzuela L, Matas J, Durruty J et al (2008) Effects of platelet concentrate and a bone plug on the healing of hamstring tendons in a bone tunnel. Arthroscopy 24(12):1373–1380
Radice F, Yanez R, Gutierrez V, Rosales J, Pinedo M, Coda S (2010) Comparison of magnetic resonance imaging findings in anterior cruciate ligament grafts with and without autologous platelet-derived growth factors. Arthroscopy 26(1):50–57
Sanchez M, Anitua E, Cugat R, Azofra J, Guadilla J, Seijas R et al (2009) Nonunions treated with autologous preparation rich in growth factors. J Orthop Trauma 23(1):52–59
Sánchez M, Anitua E, Azofra J, Andía I, Padilla S, Mujika I (2007) Comparison of surgically repaired Achilles tendon tears using platelet-rich fibrin matrices. Am J Sports Med 35(2):245–251
Sanchez-Gonzalez DJ, Mendez-Bolaina E, Trejo-Bahena NI (2012) Platelet-rich plasma peptides: key for regeneration. Int J Pept 2012:532519
Seijas R, Ares O, Catala J, Alvarez-Diaz P, Cusco X, Cugat R (2013) Magnetic Resonance imaging evaluation of patellar tendon graft remodeling after anterior cruciate ligament reconstruction with or without platelet-rich plasma. J Orthop Surg (Hong Kong) 21(1):10–14
Seijas R, Cugat R (2010) Anterior cruciate ligament graft: bone-tendon-bone. Tech Knee Surg 9(4):209–215
Shelbourne KD, Trumper RV (1997) Preventing anterior knee pain after anterior cruciate ligament reconstruction. Am J Sports Med 25(1):41–47
Weiler A, Peters G, Mäurer J, Unterhauser FN, Südkamp NP (2001) Biomechanical properties and vascularity of an anterior cruciate ligament graft can be predicted by contrast-enhanced magnetic resonance imaging. A two-year study in sheep. Am J Sports Med 29:751–761
Xie X, Wu H, Zhao S, Xie G, Huangfu X, Zhao J (2013) The effect of platelet-rich plasma on patterns of gene expression in a dog model of anterior cruciate ligament reconstruction. J Surg Res 180(1):80–88
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seijas, R., Rius, M., Ares, O. et al. Healing of donor site in bone-tendon-bone ACL reconstruction accelerated with plasma rich in growth factors: a randomized clinical trial. Knee Surg Sports Traumatol Arthrosc 23, 991–997 (2015). https://doi.org/10.1007/s00167-013-2787-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2787-2