Summary
Introduction
ACL reconstruction with quadruple hamstring graft (HT) as well as bone-patellar tendon-bone autograft (PT) is a frequent procedure in athletes after ACL rupture. Both techniques are reported to provide for satisfying results but only few articles compare both techniques.
Material and methods
Prospective evaluation was performed on 96 patients with isolated ACL rupture undergoing reconstruction with a HT or PT autograft by a single surgeon at our institution. Long time follow-up after five years included the IKDC and KOOS evaluation form as well as clinical assessment (ROM, Lachmann testing, KT-2000).
Results
Comparing both methods revealed no significant differences regarding IKDC and KOOS. The KT-2000 arthrometer testing showed a slightly increased mean laxity in the HT group. There were no differences regarding harvest side symptoms comparing HT and PT as well as one and two incision technique. Kneeling pain was significantly less common after HT autograft.
Summary
HT as well as PT autograft achieve equally good clinical results in athletes at five year follow-up with no significant difference regarding knee stability. Although no difference concerning the harvest site was identified, HT seems to be favorable for patients who work in a kneeling position.
Zusammenfassung
Hintergrund
Semitendinosus- und Gracilissehne (STG) als auch die Patellarsehne (BTB) sind gängige Transplantate zur Rekonstruktion des vorderen Kreuzbandes. Die Ergebnisse beider Techniken sind jeweils zufriedenstellend, jedoch gibt es nur wenige Arbeiten, die die Ergebnisse beider Methoden bei Leistungssportlern miteinander vergleichen.
Material und Methoden
96 Patienten mit isolierter vorderer Kreuzbandruptur wurden prospektiv randomisiert und in die Studie eingeschlossen. Die operative Versorgung der inkludierten Patienten mit STG- oder BTB-Transplantat erfolgte an einem Zentrum durch einen einzigen Operateur. Langzeituntersuchungen nach mindestens fünf Jahren schlossen den IKDC- und KOOS-Fragebogen sowie klinische Ergebnisse (ROM, Lachmann Test, KT-2000) ein.
Ergebnisse
Der Vergleich beider Methoden ergab keine signifikanten Unterschiede hinsichtlich KOOS und IKDC. Der instrumentelle Kniestabilitätstest KT-2000 ergab eine leichte erhöhte Laxizität bei Patienten der STG-Gruppe. Es gab keine signifikanten Unterschiede hinsichtlich Entnahmemorbidität im Vergleich, sowie im Vergleich zwischen der Singel- und Doppel-Inzisionstechnik. Schmerzen beim Knien traten signifikant seltener nach STG-Transplantat auf.
Zusammenfassung
Sowohl das STG- als auch BTB-Transplantat liefern vergleichbar gute klinische Ergebnisse in einem sportlich hoch aktiven Kollektiv mit einem Langzeit-Follow-up von zumindest fünf Jahren. Dabei ergab sich kein signifikanter Unterschied hinsichtlich Kniegelenks-Stabilität. Obwohl auch kein signifikanter Unterschied hinsichtlich Entnahmemorbidität vorliegt, scheint das STG Transplantat für Patienten in knienden Berufen vorteilhaft zu sein.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the high frequency of anterior cruciate ligament reconstructions, there are notable differences in the surgeons’ preference regarding the choice of the ligament graft [1, 2]. Common procedures include bone-patellar tendon-bone autografts, four strand semitendinosus and gracilis hamstring autografts, quadrizeps tendon autografts with or without bone plug, and allografts from a variety of sources [1, 3–9].
The two standard methods for anterior cruciate ligament (ACL) reconstructions are the bone-patellar tendon-bone autografts, and the semitendinosus and gracilis tendon autografts fixed with interference screws, posts, buttons or staples [1, 10–12]. Several studies have reported on good and reproducible results with these two techniques, but there are obvious problems with both methods regarding donor-site-morbidity and kneeling discomfort [13–17].
The purpose of this study was to compare the 5-year outcome of ACL reconstructions with bone-patellar tendon-bone autografts (PT) and 4-strand semitendinosus and gracilis hamstring (HT) autografts. We analyzed the clinical outcome and long-term morbidity of the patients undergoing all operative procedures by a single surgeon. Our hypothesis was that the use of HT grafts in ACL reconstruction would cause less donor-site-morbidity in terms of anterior knee pain, whereas PT grafts were expected to achieve a better knee stability. In addition the harvesting of the mid-third of the patellar tendon was compared using either a single skin incision or a double skin incision technique.
Material and methods
This prospective, comparative study (level II study) was performed at Vienna General Hospital, Medical University of Vienna between 2004 and 2008. The criteria for inclusion in this study were patients following anterior cruciate ligament reconstructions by a single surgeon. All of these patients wished to return to sports involving pivoting, cutting or sidestepping, or those with repeated episodes of instability, despite non-operative treatment involving physiotherapy [18]. Their dataset was examined for completeness and accuracy. Collected data included variables such as age, sex, mechanism of injury, type of implant (patellar tendon or hamstring tendon graft), operative techniques, intra- and postoperative complications, postoperative rehabilitation as well as clinical follow-up examination of at least five years.
Patients with incomplete dataset, patients aged younger than 15 (or with an epiphysis of the knee not closed so far), or older than 45 years of age as well as patients who had undergone previous surgery of the ipsilateral or contralateral ACL were excluded from this study. Exclusion criteria also contained patients with instability of the medial or lateral collateral ligament, patients with increased cartilage damage (Outerbridge grade III or IV) as well as patients with a rupture of their graft (ACL re-rupture).
In a five year period 96 patients (28 females/ 68 males) with an average age of 28.8 (15–45) years at the time of surgery met criteria for inclusion and were enrolled in this study. 56 patients (11/45 f/m, average age: 28.4) underwent ACL reconstruction by a patellar tendon graft and were entered into the PT group, whereas 40 patients (17/23 f/m, average age: 29.2) were treated by a hamstring tendon graft and included into the HT group. The patients were randomly assigned to one of the two study groups. Both groups were compared in terms of sex, time of surgery, injury of the medial or lateral meniscus and cartilage defect (grade I or II). Further, patients who had undergone patellar tendon graft reconstruction were additionally separated into groups, relating to the graft harvesting method (single (PT1) vs. two-incision (PT2) graft technique, see also “surgical techniques” below). We had 26 patients who were included into the PT1 and 30 patients who were entered into the PT2 group.
All of the included patients demonstrated (at least) Lachman grade II and positive pivot shift tests on clinical and radiographic (x-ray and MRI) examination, preoperatively. Surgical treatment performed within 12 days after injury were considered acute and when performed after 12 weeks as delayed. Patients were not submitted to operation between 12 days and 12 weeks after the injury because of increased risk of arthrofibrosis [19, 20]. Physical therapy with intensive training of the quadriceps muscle was applied to all patients that were operated in a delayed manner. All patients agreed to participate in a research program and the study was approved by the Institutional Review Board.
Surgical technique and graft harvesting procedures
All procedures were performed by one surgeon in the arthroscopic transtibial technique. In the PT group the interference screw fixation for both proximal and distal were used [21]. In the HT group the graft was fixed with an interference screw in the tibia and with the Transfix femoral drill guide System (Arthrex, Naples, FL) in proximal graft fixation. Referring to the graft harvesting procedures, the PT group was divided in two sub-groups.
In PT-1 group, the one-incision graft harvesting technique was applied by a vertical incision from the inferior pole of patella to the tibial tubercle. The paratendon was identified and dissected carefully. After harvesting the autograft the paratendon was exactly adapted with sutures.
In PT-2 group, the subcutaneous two-incision graft harvesting technique, the mid-third of the patellar tendon was harvested through two vertical incisions, one over the apex of the patella and the other over the tibial tubercle. The graft was retrieved subcutaneously under the paratendon with the aim of protecting the infrapatellar branches of the saphenous nerve leaving the major part of the paratendon intact. In both groups the tendon defects were left open and no bone grafting of the defects in the inferior pole of patella or the tibial tubercle were implemented.
In the HT group graft harvesting was performed through a 3 cm oblique incision over the pes anserinus. After identifying the gracilis and semitendinosus tendons the vinculae had been cut and afterwards the hamstring tendons were harvested with a closed tendon stripper and prepared as a quadruple-strand graft.
Follow-up protocol
Clinical evaluation of knee function and stability was assessed by an independent examiner after surgery. The minimum follow-up time was at least 5 years. Patients underwent routine clinical examination as well as completing the International Knee Documentation Committee (IKDC) and the Knee Injury and Osteoarthritis Outcome Score (KOOS) evaluation forms [22, 23].
The IKDC includes Demographic Form, a Current Health Assessment Form, a Subjective Knee Evaluation Form, a Knee History Form, a Surgical Documentation Form and a Knee Examination Form. Each parameter is qualified as A “normal”, B “nearly normal”, C “abnormal” or D “severely abnormal”. We only used the Knee Examination Form. This form is designed to compare the reconstructed knee to a normal contra lateral knee.
The KOOS is a self-administered instrument designed specifically for evaluation of patients with knee injury. It has been tested and shown to be valid, reliable, and responsive to changes. It consists 5 subscales: pain, symptoms, function in activities of daily living (ADL), sport and recreation function and knee-related quality of life (QOL). A score of 100 indicates no symptoms and a score of 0 indicates extreme symptoms.
Anterior-posterior knee stability was determined subjectively by performing the Lachman Test as well as objectively by using the KT-2000 arthrometer. Range of motion was assessed using a goniometer.
Referring to harvest site symptoms patients were asked to note tenderness, irritation of the nerve or numbness at the autograft harvest site and grade these symptoms as A (none), B (mild), C (moderate) or D (severe). In addition, kneeling pain was reported if it was present after patients kneeled on a carpeted floor. The severity was recorded in A to D, like the harvest site symptoms.
In addition, minor associated injuries of the knee were also analyzed to determine its influence on the clinical outcome. Minor associated injuries included meniscal tears or ruptures as well as cartilage lesions (Outerbridge I and II).
Rehabilitation
Both groups of patients were treated by a similar rehabilitation program. Immediately after surgery closed kinetic chain muscle rehabilitation program was arranged focusing on achieving full extension 2 weeks after surgery. In the PT group cycling was commenced after 6 weeks, running after 8 weeks and competitive sports were allowed after 4 months. In the HT group cycling was started after 6 weeks, running after 3 months and competitive sports were permitted after 6 months.
Statistical analysis
For statistical analysis, preoperative variables as well as clinical results after surgery were compared between the two study groups. For comparison of quantitative data Fisher exact test was perfomed; for comparison of categorical data we used Student t test and Mann-Whitney-U test. Statistical significance was defined as p < 0.05.
Results
We finally included 96 patients to compare the outcome of ACL reconstruction by PT (n = 56, 58 %) or HT (n = 40, 42 %) autograft. Within the PT group, one-incision graft harvesting technique (n = 26, 27 %) and two-incision graft harvesting technique (n = 30, 31 %) were separately analyzed.
Time of surgery and associated injuries of the knee
31 patients (32 %) were treated within 12 days after injury, whereas 65 patients (68 %) underwent ACL reconstruction after a period of 12 weeks. The ratio “acute treatment” to “delayed treatment” was distributed similarly in both study groups. Statistical analysis revealed that the time of surgery related to the time of injury had no significant influence on the outcome in both groups (p > 0.05).
Minor associated injuries of the knee were noted in 57 (59 %) patients whereas 39 (41 %) patients had no further injuries. Isolated meniscal tears were found in 32 patients (33 %), isolated cartilage lesions were seen in 14 patients (15 %) and a combination of both injuries in 11 patients (11 %). Statistical analysis showed that the presence of minor associated injuries had no significant influence in both groups. The mean time follow-up between both groups – PT (5.2 years) and HT (5.4 years) – also showed no significant difference (p > 0.05).
Outcome of IKDC score
Referring to the overall outcome of the IKDC score 88 % of patients (n = 84) reported normal (grade A) or nearly normal (grade B) knee function. In summary, 44 patients (46 %) were graded as A, 40 patients (42 %) were graded as B, nine patients (9 %) had the grade C (abnormal) and three patients (3 %) had the grade D (severely abnormal).
Comparing PT grafts and HT grafts as well as PT-1 and PT-2 incision techniques, there were no statistically significant differences between the study groups (p > 0.05); see Table 1.
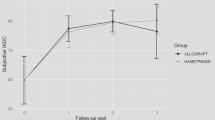
The KOOS results
With regards to the outcome of the KOOS there were no significant differences between patients with PT and HT grafts as well as between patients with one-incision or two-incision techniques. Referring to the subscale of sports and recreation patients with HT grafts had slightly better results compared to those with PT grafts. In addition the one-incision technique had a slight superior outcome compared to two-incision technique regarding the subscale of quality of life. The detailed results of the KOOS are presented in Table 2.
Knee stability and range of motion
Referring to anteriorposterior knee stability, we had a negative Lachman test in 86 % (n = 83) without any significant differences between PT and HT grafts (p > 0.05). The KT-2000 arthrometer also presented similar results between the operated and the contralateral limb with a mean of 1.4 mm in the PT and 2.1 mm in the HT group (p = 0.079).
Range of motion (ROM)
Range of motion (ROM) revealed full extension and flexion more than 130° in 93 % (n = 89) of the patients, whereas 7 % (n = 7) had a slight deficit (< 10°) in extension.
Harvest site symptoms and kneeling pain
With regards to harvest site symptoms, there was no significant difference comparing the PT and the HT group (p > 0.05). In the HT group 19 patients (19 %) were graded A (none), 12 patients (12 %) were graded B (mild), 8 patients (8 %) were graded C (moderate) and 3 patients (3 %) were graded D (severe). In the PT group 18 patients (19 %) were graded A, 14 patients (15 %) were graded B, 19 patients (19 %) were graded C and 5 patients (5 %) were graded D. Comparing the PT1 and PT2 group there was also no significant difference (PT 1/PT 2: A 9/9, B 6/8 C 14/5, D 3/2) in the outcome. Within the HT group (n = 40) irritations of the saphenous nerve were found in 21 patients (53 %).
Relating to kneeling pain, patients within the PT group had a significantly higher incidence of kneeling pain than patients in the HT group (p < 0.0001; see Table 3). Comparing patients within the PT1 group and PT2 group no significant difference was found (see also Table 3).
Discussion
In this study the two most frequently used ACL reconstruction techniques were compared prospectively. Doing so, PT as well HT autografts achieved equally good clinical results in terms of IKDC score identifying 92 % after BT as normal or nearly normal, respectively 80 % in the HT group.
Especially knee stability was satisfactory at follow-up, with negative Lachmann test in 86 % of all patients. Eriksson et al. report a positive Lachmann Test (≥ 3 mm) in 52 % at follow-up after 2.75 yrs (BT and HT). But this finding alone might not fully reflect the patient’s post-reconstruction satisfaction of 89.5 % reporting normal or nearly normal knee function [11]. This is similar to our overall satisfaction of 88 % after more than five years follow-up. Further, KT-2000 testing revealed no significant differences between the groups in our collective. This is in contrast to findings by Corry et al. reporting a significant side-to-side difference between the groups (1.1 vs 1.7 mm) [5]. But as IKDC and Lysholm scores are comparable within their collective, KT-1000 results in their opinion might not be directely linked to clinical outcome [5].
Donor-side morbidity, e.g. saphenous nerve irritation is reported to be a frequent complication after HT harvest, but are thereby not ultimately affecting activities of daily life [24]. In our collective HT was harvested using an oblique incision. Of note, oblique incision is reported to have the least incidence of nerve injury besides the highest subjective postoperative satisfaction in comparison to vertical and transverse incision [24]. Within their study Sabat et al the rate of numbness is reported to be as high as 37.8 % after 6 months compared to 55 % in our collective. Pinczewski et al report kneeling problem after HT grafts with an incidence of 27 % [25]. A more medial approach for HT harvest might reduce the incidence of injuring the infrapatellar branch and reduce the incidence of subsequent kneeling pain [15].
Harvest of the BTB tendon can also cause significant donor-side morbidity. Injury to the infrapatellar branches of the saphenous nerve (IPSN) may thereby also result in neurinomas and problems when knee walking [1, 3, 26, 27]. This is reported to be as frequent up to 80 % after BTB using the one-incision technique [28]. This finding might be attributable to the harvesting technique, suggesting superior results for the two-incision technique, where the graft is harvested subcutaneously [14–16]. In our collective, no difference between the one and two incision technique was detected (70 %-PT1 vs. 82 % PT2). In an effort to reduce IPSN irritations a rather parapatellar incision for the PT graft was used in our collective. According to Wagner et al this might reduce the incidence of knee walking pain [29]. Despite the prospective study design and comparable parameters we could not detect any major advantages. Donor site morbitiy is comparable between groups and is thereby in accordance to recent literature [11, 30, 31]. The strengths of this study is the high comparability between groups as all operations were done by one experienced surgeon. Furthermore, in both techniques the grafts were continuously fixed in the same manner (see operative technique). Moreover, the time to follow-up of 5.3 years is longer than many other large trials [5, 30–34].
Conclusion
We therefore conclude that both methods are of equal strength, while preferring HT reconstruction in patients with kneeling jobs (paving) as those trend towards less pain during knee walking.
Conflict of interest
We hereby certify that there are no actual or potential conflicts of interest for the authors of the present paper. There are no undisclosed financial or personal relationships with other people or organizations that could inappropriately influence our work.
References
Ejerhed L, Kartus J, Sernert N, Köhler K, Karlsson J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction? A prospective randomized study with a two-year follow-up. Am J Sports Med. 2003;31(1):19–25.
Jansson KA, Linko E, Sandelin J, Harilainen A. A prospective randomized study of patellar versus hamstring tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(1):8–12.
Aglietti P, Buzzi R, Zaccherotti G, De Biase P. Patellar tendon versus doubled semitendinosus and gracilis tendons for anterior cruciate ligament reconstruction. Am J Sports Med. 1994;22(2):211–7.
Clancy WG Jr, Nelson DA, Reider B, Narechania RG. Anterior cruciate ligament reconstruction using one-third of the patellar ligament, augmented by extra-articular tendon transfers. J Bone Joint Surg Am. 1982;64(3):352–9.
Corry IS, Webb JM, Clingeleffer AJ, Pinczewski LA. Arthroscopic reconstruction of the anterior cruciate ligament. A comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med. 1999;27(4):444–54.
Fu FH, Bennett CH, Lattermann C, Ma CB. Current trends in anterior cruciate ligament reconstruction. Part I: Biology and biomechanics of reconstruction. Am J Sports Med. 1999;27(6):821–30 (Review).
Indelicato PA, Linton RC, Huegel M. The results of fresh-frozen patellar tendon allografts for chronic anterior cruciate ligament deficiency of the knee. Am J Sports Med. 1992;20(2):118–21.
Jackson DW, Heinrich JT, Simon TM. Biologic and synthetic implants to replace the anterior cruciate ligament. Arthroscopy. 1994;10(4):442–52.
Kim DW, Kim JO, You JD, Kim SJ, Kim HK. Arthroscopic anterior cruciate ligament reconstruction with quadriceps tendon composite autograft. Arthroscopy. 2001;17(5):546–50.
Asik M, Sen C, Tuncay I, Erdil M, Avci C, Taser OF. The mid- to long-term results of the anterior cruciate ligament reconstruction with hamstring tendons using Transfix technique. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):965–72.
Eriksson K, Anderberg P, Hamberg P, Löfgren AC, Bredenberg M, Westman I, Wredmark T. A comparison of quadruple semitendinosus and patellar tendon grafts in reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2001;83(3):348–54.
Fu FH, Bennett CH, Ma CB, Menetrey J, Lattermann C. Current trends in anterior cruciate ligament reconstruction. Part II. Operative procedures and clinical correlations. Am J Sports Med. 2000;28(1):124–30 (Review).
Jones KG. Reconstruction of the anterior cruciate ligament using the central one-third of the patellar ligament. J Bone Joint Surg Am. 1970;52(4):838–9.
Kartus J, Ejerhed L, Eriksson BI, Karlsson J. The localization of the infrapatellar nerves in the anterior knee region with special emphasis on central third patellar tendon harvest: a dissection study on cadaver and amputated specimens. Arthroscopy. 1999;15(6):577–86.
Kartus J, Ejerhed L, Sernert N, Brandsson S, Karlsson J. Comparison of traditional and subcutaneous patellar tendon harvest. A prospective study of donor site-related problems after anterior cruciate ligament reconstruction using different graft harvesting techniques. Am J Sports Med. 2000;28(3):328–35.
Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy. 2001;17(9):971–80 (Review).
Portland GH, Martin D, Keene G, Menz T. Injury to the infrapatellar branch of the saphenous nerve in anterior cruciate ligament reconstruction: comparison of horizontal versus vertical harvest site incisions. Arthroscopy. 2005;21(3):281–5.
Shelbourne KD, Gray T. Anterior cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation. A two- to nine-year followup. Am J Sports Med. 1997;25(6):786–95.
Berbig R, Rillmann P. Timing of the surgery of rupture of the anterior cruciate ligament. Effects of acute or delayed surgery on arthrofibrosis rate and work disability Unfallchirurg. 2000;103(9):726–30.
Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med. 1991;19(4):332–6.
Matthews LS, Soffer SR. Pitfalls in the use of interference screws for anterior cruciate ligament reconstruction: brief report. Arthroscopy. 1989;5(3):225–6.
Hefti F, Müller W, Jakob RP, Stäubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3–4):226–34.
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS) – Development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96.
Sabat D, Kumar V. Nerve injury during hamstring graft harvest: a prospective comparative study of three different incisions. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2089–95.
Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564–74.
Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR Jr. Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31(1):2–11.
Yasuda K, Tsujino J, Ohkoshi Y, Tanabe Y, Kaneda K. Graft site morbidity with autogenous semitendinosus and gracilis tendons. Am J Sports Med. 1995;23(6):706–14.
Maletis GB, Cameron SL, Tengan JJ, Burchette RJ. A prospective randomized study of anterior cruciate ligament reconstruction: a comparison of patellar tendon and quadruple-strand semitendinosus/gracilis tendons fixed with bioabsorbable interference screws. Am J Sports Med. 2007;35(3):384–94.
Wagner M, Kääb ML, Schallock J, Haas NP, Weiler A. Hamstring tendon versus patellar tendon anterior cruciate ligament reconstruction using biodegradable interference fit fixation: a prospective matched-group analysis. Am J Sports Med. 2005;33(9):1327–36.
Kraeutler MJ, Bravman JT, McCarty EC. Bone-patellar tendon-bone autograft versus allograft in outcomes of anterior cruciate ligament reconstruction: a meta-analysis of 5182 patients. Am J Sports Med. 2013;41(10):2439–48.
Ahn JH, Kim JG, Wang JH, Jung CH, Lim HC. Long-term results of anterior cruciate ligament reconstruction using bone-patellar tendon-bone: an analysis of the factors affecting the development of osteoarthritis. Arthroscopy. 2012;28(8):1114–23.
Mulford JS, Hutchinson SE, Hang JR. Outcomes for primary anterior cruciate reconstruction with the quadriceps autograft: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2013;21(8):1882–8.
Tibor LM, Long JL, Schilling PL, Lilly RJ, Carpenter JE, Miller BS. Clinical outcomes after anterior cruciate ligament reconstruction: a meta-analysis of autograft versus allograft tissue. Sports Health. 2010;2(1):56–72.
Marx RG, Hetsroni I. Surgical technique: medial collateral ligament reconstruction using Achilles allograft for combined knee ligament injury. Clin Orthop Relat Res. 2012;470(3):798–805.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leitgeb, J., Koettsdorfer, J., Schuster, R. et al. Primary anterior cruciate ligament reconstruction in athletes: a 5-year follow up comparing patellar tendon versus hamstring tendon autograft. Wien Klin Wochenschr 126, 397–402 (2014). https://doi.org/10.1007/s00508-014-0550-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-014-0550-4