Abstract
Purpose
High tibial osteotomy (HTO) is a commonly used treatment to correct varus malalignment of the knee. The purpose of this study was, first, to determine, whether HTO allows return to pre-operative work, depending on the amount of work load. Second, the restoration of sports ability and a difference in sports activities pre- to postoperative should be analyzed.
Methods and patients
Fifty-one patients were included in this study. Patients were divided into three groups dependent on work intensity. Sporting activity was evaluated by an activity score (Naal). Clinical examination includes Tegner-score, Lysholm-score and visual analog pain scale. General health was assessed using the 36-Item Short Form Survey questionnaire.
Results
On an average of 16.7 ± 15.6 weeks after surgery patients returned to work, and 93.8 % of the patients returned to pre-operative work load. The Tegner activity score did not show significant changes pre- and postoperatively. At the time of survey Lysholm score reached a value of 68.7 ± 23.9 points on average. Postoperatively, patients remarked on decreased pain by VAS by an average of 2.6 ± 2.3 points.
Conclusions
In total, 92.3 % returned to pre-operative sports activities after surgery. A shift away from high impact activities to lower impact activities, a significant decrease of the duration of sports activities and number of sports disciplines was detected. In summary, HTO allows the young, active patient with medial osteoarthritis of the knee to return to work with the same work intensity and to return to sports.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High tibial osteotomy (HTO) is a commonly used treatment to correct varus malalignment of the knee in patients with medial compartment osteoarthritis [1, 2].
With the development of new osteotomy techniques and fixation methods, an increasing interest in osteotomies has been noted over the past decade [2–9]. The open-wedge HTO and fixation with a plate fixator allow precise correction and high primary stability of the osteotomy.
In literature, advantages of the open-wedge technique compared with the closed-wedge technique have been described [10, 11]. The open-wedge technique avoids the risk of peroneal nerve damage and detachment of the tibialis anterior muscle [12].
HTO is typically indicated for patients that are still active in sports and work [13]. Most of these patients are employed at the time of treatment. Therefore, important goals of treatment for these patients are not only symptom and pain relief but also prompt return to pre-operative work and sports activities. Although there are many clinical outcome studies that describe the results after HTO [14–24], there are only few published studies assessing the patients’ possibility to return to pre-operative work and sports activities after HTO [25, 26]. Incapacity to promptly return to work can be a considerable problem, particularly for patients with high work load.
The purpose of this study was, first, to determine whether HTO allows return to pre-operative work, depending on the amount of work load. Second, we aimed to analyse the recovery of the ability to perform sports and whether there was a difference in sports performance pre- and postoperatively (duration, sessions per week, different sports activities).
Materials and methods
Patients
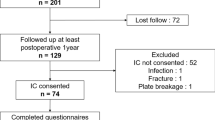
This study was approved by the ethics committee of our institution. Between 2009 and 2011, 104 HTOs were performed at our department. Of these, 51 consecutive HTOs for unicompartmental varus OA were performed by one senior surgeon. After a postoperative average of 22 ± 9.3 months, all patients were contacted by postal questionnaires for the assessment of pre- and postoperative engagement in sports and work. Patients were asked to complete a ‘return to work’ questionnaire (telephone assistance was provided if required). Sports and recreational activity were assessed by the Lysholm [27] and Tegner scores, as well as the Naal ‘sports and activity score’ [28, 29]. The state of general health of our patients was assessed using 36-Item Short Form Survey by RAND® [30]. Forty-eight patients returned the questionnaire, five of which were not complete and were not used. Therefore, 43 questionnaires were considered for evaluation (84.3 %).
Contraindications for HTO included obesity [body mass index (BMI) <35], International Cartilage Repair Society (ICRS) grade III or IV degenerative changes of the lateral femoral cartilage [31], loss of the lateral meniscus, extension deficit >15° and severe ligamentous deficiencies.
The degree of varus malalignment was assessed on pre-operative long-leg weight-bearing hip–knee–ankle radiographs.
Return to work questionnaire
The return to work questionnaire allowed the classification of patients into three different groups depending on work intensity.
-
Group I:
Patients with high work intensity (lifting and wearing of a burden greater than 15 kg, climbing stairs or ladders with load, work in constrained postures like shovelling or digging).
-
Group II:
Patients with moderate work intensity, lifting and wearing of a burden of 10–15 kg.
-
Group III:
Patients with low work intensity, working in a sitting position, handling light work objects, walking or standing.
Patients were asked about the timing of the postoperative return, regarding return to work, if work itself was the same pre- and postoperatively, if the same working activities were performed, toleration of partial weight bearing and the time when they no longer required the assistance of crutches. In addition, the visual analogue scale of pain was included in the work questionnaire and the use of analgesic medication during work or sports was noted.
Patient satisfaction with the procedure was also recorded. The final clinical outcome was rated by them as very satisfied (knee function much exceeded their pre-operative status), satisfied (knee function improved), partially satisfied (knee function improved) and not satisfied (knee function same as pre-operative status).
Sports and activity questionnaire
The sports and activity score by Naal et al. [28, 29] investigated pre- and postoperative engagement in 20 different sports activities. Pre-operative sports engagement was defined as participation in sports before the onset of restricting symptoms. The score included sports frequency and duration of sport activities (length per session). Patients were asked regarding the timing of their return to postoperative work and sports activities.
The state of knee function and activity as well as knee pain of our patients was assessed at the time of survey using the long-term approved and validated scores by Lysholm [27], Tegner and the visual analogue scale (VAS).
36-Item Short Form Survey
The state of general health of our patients was assessed using the 36-Item Short Form Survey [30]. The 36-Item Short Form Survey asks for the patients’ self-assessment in eight different domains that describe health-related quality of life (physical functioning, physical role, bodily pain, general health, vitality, social functioning, emotional role and mental health).
Clinical data
At the date of surgery, clinical data, such as BMI and age at surgery, were collected. During surgery (standardised arthroscopy of the knee before starting HTO) grade of cartilage injury according to the International Cartilage Repair Society ICRS [31] in each compartment (medial, lateral and retropatellar) was recorded. The definite degree of valgus correction was measured on pre- and postoperative long-leg knee radiographs according to Miniaci [4, 7].
Operative technique
Before HTO, an arthroscopy of each knee was performed to evaluate the grade of cartilage injury in the medial and lateral compartments of the knee joint. Osteotomy was not performed in patients with ICRS grades III or IV degenerative changes of the lateral femoral cartilage.
The medial open-wedge osteotomy was performed as described by Staubli and Lobenhoffer [32–34] in a biplanar fashion. To avoid change of the posterior tibial slope, the spreader to expand the osteotomy was dorsally placed and the leg was positioned in full extension. The anterior opening-gap was maintained at half the size of the posterior gap [35]. In addition, the superficial medial collateral ligament was released to allow the transfer of the load to the lateral compartment [4, 7].
The postoperative Mikulicz Line was set to the Fujisawa point, which represents 62 % of the width of the tibial plateau, measured from the medial cortex [4, 7]. The osteotomy was fixed with a plate fixator (Tomofix, Synthes, Switzerland). No graft was used to fill the medial gap of the osteotomy (Fig. 1).
Pre- (a and b) and post (e and f) operative radiographs showing an initiating narrowed medial joint-line and a Mikulicz line through the medial compartment pre-operatively (c). Postoperatively, the Mikulicz line overlies the Fujisawa point (d). The open-wedge osteotomy was fixed by a plate fixator (Tomofix)
Partial weight bearing (20 kg) using crutches was allowed for the first two postoperative weeks. Weight bearing was swiftly increased from week 2 until full weight bearing was achieved. Daily physiotherapy with active and passive flexion and extension exercises of the knee was recommended.
Statistical analysis
Statistical analysis was performed using the software package SPSS (SPSS, IBM Corporation, Armonk, NY, USA). Statistical tests such as Kruskal–Wallis test, t-test and Pearson Correlation test were used. The significance level was defined at p < 0.05 for all tests.
Results
Demographics
The average postoperative follow-up was 22 ± 9.3 months. Mean age of the patients was 42 ± 11.2 years; there were 32 men (74.4 %) and 11 women (25.6 %). Mean BMI was 26.9 ± 3.6 kg/m [3], with a high correlation between BMI and retropatellar osteoarthritis (r = 0.560, p = 0.001). Mean valgus correction was 8.6° ± 2.4° (groups I, II and III were 7.9° ± 1.9°, 9.8° ± 2.5° and 8.4° ± 2.5°, respectively). Mean medial osteoarthritis of the knee was 3.1 (range, 1–4; groups I, II and III were 3.1, 2.8 and 3.2, respectively; no statistical difference between each group), osteoarthritis of the lateral compartment was mean 0.28 (range, 0–1; groups I, II and III were 0.4, 0.2 and 0.2, respectively; no statistical difference) and retropatellar osteoarthritis was median 1.2 (range, 0–4; there was no statistical difference between each group) (Table 1) [31].
The underlying diagnosis was medial osteoarthritis in 37 cases and osteonecrosis of the femoral condyle in six cases.
Concomitant side-procedures were performed in 13 cases (six osteochondral autologous transplantations, four partial meniscectomies and three procedures for microfractures of the medial femoral condyle). In group I, only one patient underwent a side procedure (osteochondral autologous transplantation), two patients underwent a side procedure in group II (osteochondral autologous transplantation, partial meniscectomy) and all other side procedures were performed in group III.
Return to work questionnaire
Patients returned to work at 16.7 ± 15.6 weeks on average postoperatively. Group III (n = 15), with the lowest work intensity, was able to work after 11.8 ± 7.8 weeks, group II (n = 12) after 20 ± 17.8 weeks and group I (n = 13), with the highest work intensity, was able to return to work after 19.1 ± 9.1 weeks; however, these differences were not statistically significant (p = 0.325) (Fig. 2). Three patients did not work postoperatively (6.25 %). There were no pre- and postoperative changes among groups. However, one patient in group I, three in group II and two in group III referred small differences in their job activities postoperatively, but remained in each work intensity group.
Patients in group I (mean 6.9 ± 3.1 weeks postoperatively) walked without crutches earlier than those in group II (mean 8.9 ± 3.4 weeks postoperatively) and group III (mean 10.9 ± 5.7 weeks postoperatively); however, these associations were weakly correlated (r = 0.325, p = 0.043). In addition, there was a weak correlation between cessation of partial weight bearing and work intensity (r = 0.313, p = 0.049); group I operated with full weight bearing after 6.5 ± 2.7 week, group II after 8.7 ± 4.5 weeks and group III after 10.2 ± 6.4 weeks.
At the time of the postoperative survey for sports or working activities, analgesic medication was necessary in group I in 23.1 % occasionally and in 15.4 % continuously, in group III in 25 % occasionally and in 8.3 % continuously and in group III in 20 % occasionally; however, these differences were not statistically significant (correlation: r = 0.231, p = 0.156).
In group I, 53.9 % of patients completed rehabilitation after surgery, in group II, 75 % and in group III, 80 %. At the time of the survey, 16.3 % of patients still required physiotherapy and there was no significant difference in each group.
Sports and activity questionnaire (Naal score)
After surgery, 36 (26 men, ten women) of 43 patients (83.7 %) were active in at least one sports activity compared with 39 of 43 patients (90.7 %) pre-operatively, yielding a return to sport rate of 92.3 %. None of the patients who had been inactive before surgery undertook new postoperative activities.
Patients were active in an average of 4.0 ± 1.1 different sports disciplines pre-operatively, but after surgery, only 2.8 ± 1.6 different sports disciplines were performed per patient with a significance of p < 0.005. Men were engaged in an average of 4.1 ± 1.1 sports disciplines pre- and 3.0 ± 1.8 post-operatively (p < 0.005), women in an average of 3.9 ± 1.4 sports disciplines pre-operatively and 2.2 ± 1.0 post-operatively (p < 0.005).
Concerning sports disciplines (Table 2), patient participation in high impact activities (ball games, jogging, tennis) was significantly decreased (ball games −81.8 %, p = 0.002; tennis −45.5 %, p = 0.422; jogging −50 %, p = 0.254). Participation in low impact activities like swimming (−6 %, p = 0.822), cycling (−25 %, p = 0.002) and hiking (−17 %, p = 0.499) presented a lower decrease. Only weight and fitness training activities were increased (+27.3 %, p = 0.571).
The overall sports frequency (sessions per week) did not significantly change pre- and postoperatively [2.14 ± 0.67 and 1.8 ± 1.24 times per week, respectively (p = 0.152)]. There was a decrease of sports frequency performed twice and four times a week and a slight increase in sport activities once a week. There were no specific sex-related differences concerning the decrease of sports frequency. The session length of each sports activity averaged at 82 ± 29.5 minutes pre-operatively and 64 ± 45.3 minutes postoperatively.
Clinical outcome
Fourteen patients indicated that they were very satisfied with the surgical procedure, four patients were satisfied and three were partially satisfied.
At the time of the survey no significant difference was shown in seven of eight items concerning SF-36; only physical functioning significantly decreased after surgery to the matched reference population (men, 76.6 versus 88.2; women, 69 versus 82.8) [36] (Fig. 3).
36-Item Short Form Survey results of our patients at the time of the survey, classified by sex. The patients (men = 32, women = 11) scored almost equal to the reference group [2]. A significantly higher score was detected in the women’s group for ‘role physical’ and ‘role emotional’. A significantly lower score was detected in ‘physical functioning’ in both groups
The Tegner activity score did not show significant changes pre- and postoperatively (pre-operatively: mean 3.78 ± 1.9; post-operatively: mean 3.7 ± 1.4). At the time of survey, the Lysholm score resulted in an average of 68.7 ± 23.9 points.
Postoperatively, patients referred a remarkable decrease in pain by VAS with an average of 2.6 ± 2.3 points.
Discussion
The most important finding of the present study was the correlation between work load and time needed to return to work after HTO.
Schröter et al. [25] reported a mean work incapacity of 87 days (12.4 weeks). Hoell et al. [36] reported a mean duration of work incapacity of 13.9 weeks after HTO and that 9.4 % of the patients could not work at the same work load level postoperatively. These studies showed a shorter time of work incapacity in comparison with the present study (16.7 ± 15.6 weeks). There was a relationship between work load and time needed to return to work after HTO but no significance was found. Workers with the highest work load were able to return to work after 19.1 ± 9.1 weeks, while those with the lowest work load returned after 11.8 ± 7.8 weeks. The relationship between work load and work incapacity presented in this study is not surprising. In particular nowadays, it is important to reduce the duration of work incapacity after surgery.
Following the early full weight bearing protocol by Lobenhoffer et al. [37] and Brinkman et al. [38], full weight bearing was allowed after wound healing (after 12–14 days postoperatively). However, complete weight bearing was achieved after 6.5 weeks (group I) and 10.2 weeks (group III), which indicates an inversely proportional relationship to work incapacity after surgery in each group.
The second important finding was that 92.3 % of all patients returned to sport postoperatively after HTO [4, 5, 39]. The participation in sports activities decreased approximately 7 % (from 90.7 to 83.7 %) postoperatively, which indicates a return to a sports level of 92 %. Recent studies show similar findings—Salzmann et al. [26] found a postoperative engagement in sport activities of 90 %, Saragaglia et al. [40] detected a “return to sport”-level of 85.5 %—and these data reflect our findings. Conversely, we found a shift away from high impact activities to lower impact activities. Bonnin et al. [41] showed a return to a higher activity level of 20.8 % and a return to an equal activity level of 44.6 %. In addition, we found a significant decrease of the duration of sports activities and number of sports disciplines after surgery. Overall sports frequency also slightly decreased but this was not significant. Reasons for the observed decreased activity in high impact sports activities may be that patients are advised to be physically active in general, while excessive participation in impact sports like soccer or tennis is not recommended. Naal et al. [29] reported a similar decrease of sport activities and a shift away from high-impact sports activities after unicompartmental knee arthroplasty.
Saragaglia et al. [40] reported about no significant changes of the frequency of sports sessions per week (2.36 versus 2.13), which is comparable to our data (2.14 versus 1.8). But Saragaglia et al. [44] described a decrease of overall length of sessions, which was also found within our data (82 versus 64 minutes).
In the present study, HTO led to decreased overall pain level (VAS postoperatively 2.6 ± 2.3), and thereby the functionality, represented by the Lysholm score, increased. The Lysholm score was 68.7 (±23.9) points postoperatively. In comparison, earlier studies showed a higher postoperative Lysholm score (from 73 [42] to 85.5 points [25]). Niemeyer et al. [43] showed an increase of the Lysholm score from 54.3 ± 20.8 points to 79.1 points 36 months after open-wedge HTO without bone graft using the TomoFix plate for fixation. Kolb et al. [39] used the TomoFix plate without bone graft and observed a Lysholm score of 83 points after 12 months.
However, the question of why patients with reduced knee pain and improved knee function did not increase their sporting activity remains. It may be that patients are more cautious with their knees after accepting the fact that their knees have irreparable defects. Hence potentially harmful activities may be avoided.
The satisfaction rate (satisfied or very satisfied with the intervention) for patients’ expectations in our study reached 72.1 % (very satisfied 39.5 %, satisfied 32.6 %). Nagel et al. [44] reported a satisfaction rate of 82 %, Bonnin et al. of 56 % [7] in 2004 and 77.7 % (40.3 % very satisfied, 37.4 % satisfied) in 2013 [41].
The median Tegner score did not show any pre- or postoperative improvement (3.8 versus 3.7). Other studies reported a Tegner score between 3.8 and 4.3 points [36, 42].
We have no pre-operative data of 36-Item Short Form Survey, but comparison of the postoperative data with those of a matched reference population shows that only physical functioning showed a significant postoperative decrease [30]. Bonnin et al. [41] showed a postoperative SF-12 of 53.6 for the physical score and 44.5 for the mental score. In the present study, a physical functioning score of 72 was obtained.
There were a total of 13 surgical side procedures (not more than one in each patient) performed within the same operative setting as HTO. However, we found no significant difference in outcomes between singular HTO and HTO with an additional surgical procedure. Thus, side procedures allow surgeons to address other articular or pathologic cartilage changes at the time of HTO without fear of affecting the results.
We used in our cohort a fixed plate with no graft at the medial gap. If the gap is bigger than 1 cm we favour an interposition of an iliac crest bone graft [45]. An internal fixation (“Puddu”-plate [46]) shows a higher implant failure (up to 6 %), especially when the medial gap is more than 1 cm, obese patients and osteoporotic bone conditions [47]. Maffulli et al. [48] show the possibility of a significant loss of correction at mid-term follow up using a non-locking Puddu-plate.
The postoperative Mikulicz line was set to the Fujisawa point, which represents 62 % of the width of the tibial plateau [4, 7]. Recent studies [49] have focused on a variation of the Fujisawa point. So Feucht et al. [49] propose an individual approach with a weight-bearing line of 50–65 % depending on patient clinical characteristics. This individualisation of the weight-bearing line has to be proved in further studies.
This study had several limitations. First, it was a retrospective investigation. Second, it involved only a postal questionnaire. No postoperative clinical examination was performed. Third, the short-term nature of the study did not allow us to draw conclusions concerning the relationship between continued sporting activities and the progression of knee OA or the need for change in work activities after HTO.
Conclusion
We demonstrated that after HTO, all patients returned to work with approximately the same work intensity. None of the patients underwent an occupational re-training, and none sufficiently reduced the work load to transition into a different work intensity group (see above). A longer follow-up is needed to detect possible changes of work activities in the future.
In total, 92 % of the patients who underwent HTO returned to sports activities, although they reduced the frequency, duration and quantity of sports disciplines compared with pre-operative levels. There was a shift of sports disciplines from high impact activities such as football, tennis and ball sports to swimming and cycling.
Clinical scores of Lysholm, Tegner, VAS and patients satisfaction were equal or increased but did not reach previously reported levels.
Therefore, HTO can be considered a clinically successful procedure that allows the working and active patient with early stage OA of the knee to return to work at equal work intensity and promptly return to sports activities.
References
Aglietti P, Rinonapoli E, Stringa G, Taviani A (1983) Tibial osteotomy for the varus osteoarthritic knee. Clin Orthop Relat Res 176:239–251
Coventry MB (1985) Upper tibial osteotomy for osteoarthritis. J Bone Joint Surg Am 67:1136–1140
Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P (2004) Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Arch Orthop Trauma Surg 124:575–584
Agneskirchner JD, Hurschler C, Wrann CD, Lobenhoffer P (2007) The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy 23:852–861
Akizuki S, Shibakawa A, Takizawa T, Yamazaki I, Horiuchi H (2008) The long-term outcome of high tibial osteotomy: a ten- to 20-year follow-up. J Bone Joint Surg (Br) 90:592–596
Amendola A, Bonasia DE (2010) Results of high tibial osteotomy: review of the literature. Int Orthop 34:155–160
Bonnin M, Chambat P (2004) Der stellenwert der valgisierenden, zuklappenden tibiakopfosteotomie bei der medialen gonarthrose. Orthopade 33:135–142
Coventry MB (1979) Upper tibial osteotomy for gonarthrosis. The evolution of the operation in the last 18 years and long term results. Orthop Clin N Am 10:191–210
Hinterwimmer S, Beitzel K, Paul J, Kirchhoff C, Sauerschnig M, von Eisenhart-Rothe R, Imhoff AB (2011) Control of posterior tibial slope and patellar height in open-wedge valgus high tibial osteotomy. Am J Sports Med 39(4):851–856
Luites JWH, Brinkmann JM, Wymenga AB, Van Heerwaarden RJ (2009) Fixation stability of opening- versus closing-wedge high tibial osteotomy. J Bone Joint Surg (Br) 91:1459–1465
Tunggal JAW, Higgins GA, Waddell JP (2010) Complications of closing wedge high tibial osteotomy. Int Orthop 34:255–261
Song EK, Seon JK, Park SJ, Jeong MS (2010) The complications of high tibial osteotomy. J Bone Joint Surg (Br) 92:1245–1252
Kohn L, Sauerschnig M, Iskansar S, Lorenz S, Meidinger G, Imhoff AB, Hinterwimmer S (2013) Age does not influence the clinical outcome after high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):146–151
Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. J Bone Joint Surg (Br) 75:745–749
Dejour H, Neyret P, Boileau P, Donell ST (1994) Anterior curciate reconstruction combined with valgus tibial osteotomy. Clin Orthop Relat Res 299:220–228
DeMeo PJ, Johnson EM, Chiang PP, Flamm AM, Miller MC (2010) Midterm follow-up of opening-wedge high tibial osteotomy. Am J Sports Med 38:2077–2084
Hernigou PH, Medevielle D, Debeyre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. J Bone Joint Surg Am 69:332–354
Imhoff AB, Linke RD, Agneskirchner J (2004) Korrekturosteomie bei primary-, varus-, double-varus- und triple-varus-knieinstabilität mit kreuzbandersatz. Orthopade 33:201–207
Koshino T (2010) Osteotomy around young deformed knees: 38-year super-long-term follow-up to detect osteoarthritis. Int Orthop 34:263–269
Maquet P (1976) Valgus osteotomy for osteoarthritis of the knee. Clin Orthop Relat Res 120:143–148
Rudan JF, Simurda MA (1990) High tibial osteotomy. A prospective clinical and roentgenographic review. Clin Orthop Relat Res 255:251–256
Schallberger A, Jacobi M, Wahl P, Maestretti G, Jakob RP (2011) High tibial valgus osteotomy in unicompartmental medial osteoarthritis of the knee: a retrospective follow-up study over 13–21 years. Knee Surg Sports Traumatol Arthrosc 19:122–127
Akizuki S, Shibakawa A, Takizawa T, Yamazaki I, Horiuchi H (2008) The long-term outcome of high tibial osteotomy: a ten- to 20-year follow-up. J Bone Joint Surg (Br) 90:592–596
Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P (2013) Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc 21(1):170–180
Schröter S, Mueller J, van Heerwaarden R, Lobenhoffer P, Stöckle U, Albrecht D (July 10, 2012) Return to work and clinical outcome after open wedge HTO. Knee Surg Sports Traumatol Arthrosc 21(1):213–219
Salzmann GM, Ahrens P, Naal FD, El-Azab H, Spang JT, Imhoff AB, Lorenz S (2009) Sporting activity after high tibial osteotomy for the treatment of medial compartment knee osteoarthritis. Am J Sports Med 37(2):312–318
Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10(3):150–154
Naal FD, Maffiuletti NA, Munzinger U, Hersche O (2007) Sports after hip resurfacing arthroplasty. Am J Sports Med 35(5):705–711
Naal FD, Fischer M, Preuss A, Goldhahn J, von Knoch F, Preiss S, Munzinger U, Drobny T (2007) Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med 35(10):1688–1695
http://www.rand.org/health/surveys_tools/mos/mos_core_36item.html
Van den Borne MP, Raijmakers NJ, Vanlauwe J, Victor J et al (2007) International cartilage repair society (ICRS) and Oswestry macroscopic cartilage evaluation scores validated for use in autologous chondrocyte implantation (ACI) and microfracture. Osteoarthr Cartil 15(12):1397–1402
Lobenhoffer P, Agneskirchner J, Zoch W (2004) [Open valgus alignment osteotomy of the proximal tibia with fixation by medial plate fixator].[Article in German]. Orthopade 33:153–160
Staubli AE, De Simoni C, Babst R, Lobenhoffer P (2003) Tomofix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia - early results in 992 cases. Injury 34:55–62
Staubli AE, Jacob HAC (2010) Evolution of open-wedge high-tibial osteotomy: experience with a special angular stable device for internal fixation without interposition material. Int Orthop 34:167–172
Noyes FR, Barber-Westin SE, Hewett TE (2000) High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med 28:282–296
Hoell S, Suttmoeller J, Stoll V, Fuchs S, Gosheger G (2005) The high tibial osteotomy, open versus closed wedge, a comparison of methods in 108 patients. Arch Orthop Trauma Surg 125(9):638–643
Lobenhoffer P, Agneskircher JD (2003) Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 11(3):132–138
Brinkman JM, Luites JW, Wymenga AB, van Heerwaarden RJ (2010) Early full weight bearing is safe in open-wedge high tibial osteotomy. Acta Orthop 81(2):193–198
Kolb W, Guhlmann J, Windisch C, Kolb K, Koller H, Grützner P (2009) Opening-wedge high tibial osteotomy with a locked low-profile plate. J Bone Joint Surg Am 91:2581–2588
Saragaglia D, Rouchy RC, Krayan A, Refaie R (2014) Return to sports after valgus osteotomy of the knee joint in patients with medial unicompartmental osteoarthritis. Int Orthop 38(10):2109–2114
Bonnin M, Laurent J, Zadegan F et al (2013) Can patients really participate in sport after high tibial osteotomy? Knee Surg Sports Traumatol Arthrosc 21(1):64–73
Sterett WI, Steadman JR, Huang MJ, Matheny LM, Briggs KK (2010) Chondral resurfacing and high tibial osteotomy in the varus knee: survivorship analysis. Am J Sports Med 38(7):1420–1424
Niemeyer P, Schmal H, Hauschild O, von Heyden J, Sudkamp NP, Kostler W (2010) Open-wedge osteotomy using an internal plate fixator in patients with medial-compartment gonarthritis and varus malalignment: 3-year results with regard to preoperative arthroscopic and radiographic findings. Arthroscopy 26(12):1607–1616
Nagel A, Insall JN, Scuderi GR (1996) Proximal tibial osteotomy: a subjective outcome study. J Bone Joint Surg Am 78:1353–1358
Schröter S, Mueller J, van Heerwaarden R, Lobenhoffer P, Stöckle U, Albrecht D (2013) Return to work and clinical outcome after open wedge HTO. Knee Surg Sports Traumatol Arthrosc 21(1):213–219
Puddu G, Cipolla M, Cerullo G, Franco V, Giannì E (2007) Osteotomies: the surgical treatment of the valgus knee. Sports Med Arthrosc 15(1):15–22
Lobenhoffer P, Agneskirchner J, Zoch W (2004) Open valgus alignment osteotomy of the proximal tibia with fixation by medial plate fixator. Orthopade 33(2):153–160
Maffulli N, Loppini M, Longo UG, Denaro V, Oliva F (2013) Bovine xenograft locking Puddu plate versus tricalcium phosphate spacer non-locking Puddu plate in opening-wedge high tibial osteotomy: a prospective double-cohort study. Int Orthop 37(5):819–826
Feucht MJ, Minzlaff P, Saier T, Cotic M, Südkamp NP, Niemeyer P, Imhoff AB, Hinterwimmer S (2014) Degree of axis correction in valgus high tibial osteotomy: proposal of an individualised approach. Int Orthop 38(11):2273–2280
Conflict of interest
I certify that I have not signed any agreement with commercial interest related to this study, which would, in any way, limit publication of any and all data generated for the study or to delay publication for any reason.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Faschingbauer, M., Nelitz, M., Urlaub, S. et al. Return to work and sporting activities after high tibial osteotomy. International Orthopaedics (SICOT) 39, 1527–1534 (2015). https://doi.org/10.1007/s00264-015-2701-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2701-2