Abstract
Purpose
Fragility hip fractures represent a major health and social burden. To date, there are no reports regarding mortality and factors that influence outcomes after osteoporotic hip fractures in Romania.
Material and methods
The electronic database of the largest healthcare provider in the western part of the country was searched for hip fracture admissions between 2008 and 2012. Inclusion criteria were age over 55 and the diagnosis of intra or extracapsular fractures, corresponding to ICD-10 S72.0 and S72.1 codes, respectively.
Results
A total of 1,866 patients met the criteria and were selected for data analysis. The gain in rates and crude numbers was caused mainly by a rise of fractures in males. The opposite is seen for the female-to-male ratio. Even though the mean age steadily increased for a total of 1.5 over a five-year period the patients are still younger than the European averages, which might explain the slightly better one-year survival. The age–gender adjusted hip fracture incidence increased dramatically with age, especially in women. The relative risk of dying in the first year is 1.359 times higher if the fracture is extracapsular (95 % CI 1.12–1.65). In total, 21.1 % of all patients die by one year after the fracture. This was drastically reduced for the following years. The survival function is significantly dependent on age group, level of fracture and time from hospital admission until surgery (p < 0.001).
Conclusions
Increased age, extracapsular fractures and delayed surgery have worse outcomes. Regarding gender, even if not significant at the 0.05 level, probability of survival for females is higher for all time intervals. Updated, regional studies could be used in patient management to improve outcomes whilst decreasing costs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fragility hip fractures represent a major health and social burden. They occur in elderly and have the potential to limit mobility and self care. In addition, surgery and postoperative care can aggravate pre-existing conditions and precipitate death [1]. In the next four decades a demographic model predicted that the number of osteoporosis related fractures will double and the costs will increase six fold, due to the aging population [2].
The incidence of hip fractures worldwide follows regional trends. In Europe and North America the age-adjusted incidence is now stabilising and even decreasing according to some reports, whereas in Asia the rates are rising [3]. Available data for the Romanian population is mostly confined to a single citation, which used national hospital discharge data from the year 2010, in order to validate the local version of the FRAX® model [4]. This fracture probability was calculated [5]. Small differences can occur within the same country but they are not always significant [6–8].
Regional audit studies could better adjust patient management and improve outcomes whilst decreasing costs. To date, there are no reports regarding factors that influence outcomes after osteoporotic hip fractures in Romania. We therefore aimed to determine the mortality as well as provide an updated model of regional rates for fragility hip fractures in the western part of the country.
Material and methods
Anonymous data was obtained from the hospital’s electronic patient database. The study was approved by the Research Department and Ethics Committee of the Emergency Clinical County Hospital. The Emergency Clinical County Hospital in Timisoara is the largest healthcare provider in the western part of the country which treats virtually all hip fractures from the Timis region. The vast majority of population is white Caucasian and people over 65 years of age represent 16.1 % of the total population as of the 2011 census. The electronic database was searched for hip fracture admissions over five years between January 2008 and December 2012. Inclusion criteria were age over 55 and the main diagnosis of intracapsular/femoral neck or extracapsular/intertrochanteric fractures, corresponding to ICD-10 S72.0 and S72.1 codes, respectively. Only primary hip fractures were included. Patients who were readmitted within this cohort were individually checked to differentiate between a poorly coded revision and contralateral fracture. The same patient was considered a new case only if it had a true second contralateral proximal hip fracture for all analysis except mortality. Patients were not excluded if malignancy was present. The dead/alive status was determined by comparing the personal identification number of the patients (CNP) against the national population evidence records accessed in March 2013. The age–gender adjusted incidence for 2010 was calculated using data from the National Institute of Statistics. Preliminary analysis is mainly based on Kaplan-Meier survival analysis accompanied by simple descriptive statistics related to the yearly life table. Odds ratio and relative risk of dying in the first year after intervention is also computed for different factors (age, gender, place of living, level of fracture, hospitalization duration and time until surgery). We performed a logistic regression to identify risk factors for a consecutive contralateral proximal femoral fracture. Statistical processing was performed using SPSS 20 (IBM) and STATA 12.
Results
A total of 1,866 patients met the criteria and were selected for data analysis. The total number of hip fracture admissions for patients over 55 years of age fluctuates but clearly increased. The opposite is seen for the female-to-male ratio. The mean age steadily increased for a total of 1.5 years over a five-year period (Table 1).
Hip fracture incidence and total number of fractures as well as 65 years or over population increased in Timis County from 2008 until 2012. The gain in incidence and crude numbers was caused mainly by a rise of fractures in males.
The age–gender adjusted hip fracture incidence in Timis County in 2010 increased dramatically with age. This trend was especially evident in women, where it was 48.5 times higher in patients over 85 compared to patients between 55 and 59 years (Table 2).
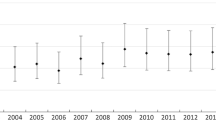
There is a consistently longer hospitalization for patients with femoral neck (intracapsular) fractures (Graph 1). The duration from admittance until surgery is less variable: from 4.20 in 2008 it went up to a maximum of 4.74 in 2009 and then dropped to a minimum of 3.85 in 2012.
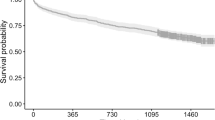
The relative risk of death for the first year is 1.359 times higher if the fracture is extracapsular (95 % CI 1.12–1.65). In total, 21.1 % of all patients died the year after fracture (Fig. 1a).
Cumulative survival function. a Percentage of patients surviving along the time frame (years) from the fracture point. b Seven age groups percentage of patients surviving along the time frame (years) from the fracture point. This shows the linearity seen in the first figure is not maintained when the 55–75 age group is further divided into five-year intervals
The risk of death was significantly higher for the first year after sustaining a proximal hip fragility fracture. This was drastically reduced for the following years, as can be seen in Table 3 and Fig. 1a. The observation was interrupted during 2013 so all surviving patients have been censored after March 2013.
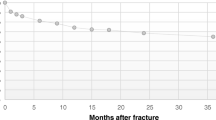
Kaplan–Meier survivor-function by different factor levels is plotted in Figs. 1a and b. Crossing pattern for factors like age (Fig. 1b), residential area (Fig. 2a) and hospitalization time (Fig. 2b) is a clear indicator that the relation between risk of failure and factor differs by surviving time. However, apparently the survival is higher if hospitalization time increases and the patient comes from a rural area. Figure 1 shows how the pattern changes if different grouping levels are chosen for a continuous variable. For the other factors the pattern is more distinct.
Kaplan–Meier survival function. a Residential area adjusted percentage differences of patients surviving along the time frame (years) from the fracture point. b Duration of hospitalization (days) adjusted percentage differences of patients surviving along the time frame (years) from the fracture point
To see if all these differences were significant several equality tests of survival functions were performed (Table 4). The Breslow and Tarone-Ware tests are appropriate when hazard variation is non-proportional. All three tests show that survival function is significantly dependent on age group, level of fracture and time from hospital admission until surgery (p < 0.001). Increased age, extracapsular fractures and delayed surgery have worse outcomes (Fig. 1b and Fig. 3). Regarding gender, even if not significant at the 0.05 level, probability of survival for females is higher for all time intervals.
Only the presence of an extracapsular fracture has a significant influence (at 0.05 level) on the comeback event. The odds of comeback are reduced by 65.2 % if the initial fracture is pertrochanteric. Age, gender, hospital stay, time to surgery, and place of living appear to have no influence.
Discussion
This study is the first to analyse mortality after hip fractures in Romania. In addition, it provides descriptive data regarding age, gender, incidence, length of hospital stay, timing and type of surgical treatment and living environment, as well as their correlation to mortality.
Incidence of hip fractures continues to show variability among countries and regions, accountable possibly by differences in demographics or diversities in treatment methods with a definite downward trend with regard to intracapsular fractures [9]. Some reports continue to find increased rates [7, 10] although this secular trend has been generally reversing over the last decade [11–13]. Overall, the rates are higher in older ages [7, 13]. The trend is attributable to either increased ratios of females [10] or males [7] or decreased ratios in women [13] or men [12], respectively.
The mean age in our study group increased at higher rates but is still approximately five years younger than reported in the literature [9]. This might account for the slightly lower one-year mortality compared to the relatively constant percentage of 22–29 % reported in the literature [9, 14]. In addition, in our study, pertrochanteric location has worse outcomes, although other reports found no significantly different mortality rates between intra and extracapsular fractures [14].
Age–gender adjusted mortality rates are increased following any fragility fracture but especially after proximal hip location and they persist for five to ten years. With regard to comorbidities, the same study found that these do not appear to influence mortality [15]. After hip fractures there is a higher mortality among males even when adjusted for age and fracture level despite men being younger at the time of fracture [7, 16].
The extracapsular fractures were internally fixed using many implant types, with a special focus on the DHS (dynamic hip screw) and the Gamma nail. However, the exact proportions were not determined and therefore the fixation method was not tested for relevance. Such heterogeneity in type of osteosynthesis has also been previously encountered and should not affect the global outcome [17]. Regarding the intracapsular femoral neck fractures, the estimate use of implant type in our study is also qualitative. The most popular was uncemented bipolar hemiarthroplasty, followed by uncemented Moore type implant. However, data from the literature has shown little interference of the hip arthroplasty type to survival after femoral neck fractures in healthy elderly [18].
Associated diseases and fractures, bone mineral density, early complications such as pressure sores as well as late complications of arthroplasty and internal fixation were not retrieved from the electronic database. Comorbidities assessed with the American Society of Anesthesiologists (ASA) score and a high postoperative plasma concentration of troponin T have been shown in previous studies to be predictive of early postoperative mortality [19]. We did observe that patients operated less than 48 hours after admission have better survival that could be maintained for more than four years. Comparable situations are also encountered in the literature [20].
One important factor that was not analysed in our study is the ambulatory status at discharge. Even if patients do survive, the functional status could be extremely low. Age over 80 years, dementia and especially prior fracture ambulatory status confined to indoors have been shown to have a significant negative impact on the return to independent living [21]. This can be paramount since in our current settings, most patients are sent home and daily care will be provided by spouse, family or a caregiver. On the other hand, the limited use of long-term home care facilities for elderly in our region might contribute to the improved survival.
Bisphosphonates treatment aimed at increasing bone mineral density was found to significantly reduce mortality after hip fractures [22]. However, a close insight into adherence to treatment found that the decreased trend in mortality was expressed even for patients who filled only one prescription. This led to the supposition that bisphosphonate therapy may be primarily initiated in patients with potentially increased life expectancy [23].
Fragility hip fracture rates in the western part of Romania are rising, predominantly at the expense of elderly males. Even though the mean age is increasing steadily, the patients are still younger than the European averages, which might explain the slightly better one-year survival. The regional age–gender adjusted hip fracture rates increase abruptly with age, especially in women. Increased age and extracapsular location have worse survival. Furthermore, the probability of survival is higher for females and those operated less than 48 hours after admittance. We hope these findings will lead to improvements in the management of fragility hip fracture patients.
References
Johnell O, Kanis JA (2004) An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int 15(11):897–902
Bleibler F, Konnopka A, Benzinger P, Rapp K, König HH (2013) The health burden and costs of incident fractures attributable to osteoporosis from 2010 to 2050 in Germany—a demographic simulation model. Osteoporos Int 24(3):835–847
Cooper C, Cole ZA, Holroyd CR, Earl SC, IOF CSA Working Group on Fracture Epidemiology et al (2011) Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int 22(5):1277–1288
Grigorie D, Sucaliuc A, Johansson H, Kanis JA, McCloskey E (2013) Incidence of hip fracture in Romania and the development of a Romanian FRAX model. Calcif Tissue Int 92(5):429–436
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl D, IOF Working Group on Epidemiology and Quality of Life et al (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23(9):2239–2256
Bjørgul K, Reikerås O (2007) Incidence of hip fracture in southeastern Norway a study of 1,730 cervical and trochanteric fractures. Int Orthop 31:665–669
Icks A, Haastert B, Wildner M, Becker C, Meyer G (2008) Trend of hip fracture incidence in Germany 1995–2004: a population-based study. Osteoporos Int 19(8):1139–1145
Grambsch PM, Therneau TM (1994) Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 81:515–526
Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ (2008) Mortality following hip fracture: trends and geographical variations over the last 40 years. Injury 39(10):1157–1163
Hernández JL, Olmos JM, Alonso MA, González-Fernández CR, Martínez J et al (2006) Trend in hip fracture epidemiology over a 14-year period in a Spanish population. Osteoporos Int 17(3):464–470
Dimai HP, Svedbom A, Fahrleitner-Pammer A, Pieber T, Resch H et al (2011) Epidemiology of hip fractures in Austria: evidence for a change in the secular trend. Osteoporos Int 22(2):685–692
Nymark T, Lauritsen JM, Ovesen O, Röck ND, Jeune B (2006) Decreasing incidence of hip fracture in the Funen County, Denmark. Acta Orthop 77(1):109–113
Chevalley T, Guilley E, Herrmann FR, Hoffmeyer P, Rapin CHR et al (2007) Incidence of hip fracture over a 10-year period (1991–2000): reversal of a secular trend. Bone 40(5):1284–1289
Giversen IM (2007) Time trends of mortality after first hip fractures. Osteoporos Int 18(6):721–732
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA et al (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301(5):513–521
Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B (2010) Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing 39(2):203–209
Kok LM, van der Steenhoven TJ, Nelissen RGH (2011) A retrospective analysis of bilateral fractures over sixteen years: localisation and variation in treatment of second hip fractures. Int Orthopaedics 35:1545–1551
Burgers PTP, Van Geene AR, Van den Bekerom MPJ, Van Lieshout EMM, Blom B, Aleem IS, Bhandari M, Poolman RW (2012) Total hip arthroplasty versus hemiarthroplasty for displaced femoral neck fractures in the healthy elderly: a meta-analysis and systematic review of randomized trials. Int Orthopaedics 36:1549–1560
Talsnes O, Hjelmstedt F, Dahl OE, Pripp AH, Reikerås O (2011) Clinical and biochemical prediction of early fatal outcome following hip fracture in the elderly. Int Orthopaedics 35:903–907
Marsland D, Chadwick C (2010) Prospective study of surgical delay for hip fractures: impact of an orthogeriatrician and increased trauma capacity. Int Orthopaedics 34:1277–1284
Vochteloo AJH, Tuinebreijer WE, Maier AB, Nelissen RGH, Bloem RM, Pilot P (2012) Predicting discharge location of hip fracture patients; the new discharge of hip fracture patients score. Int Orthop 36:1709–1714
Beaupre LA, Morrish DW, Hanley DA, Maksymowych WP, Bell NR et al (2011) Oral bisphosphonates are associated with reduced mortality after hip fracture. Osteoporos Int 22(3):983–991
Bondo L, Eiken P, Abrahamsen B (2013) Analysis of the association between bisphosphonate treatment survival in Danish hip fracture patients—a nationwide register-based open cohort study. Osteoporos Int 24(1):245–252
Acknowledgements
Cristina Nuta
Aura Careba
Horia Vermesan
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Poenaru, D.V., Prejbeanu, R., Iulian, P. et al. Epidemiology of osteoporotic hip fractures in Western Romania. International Orthopaedics (SICOT) 38, 2329–2334 (2014). https://doi.org/10.1007/s00264-014-2407-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2407-x