Abstract
Spain lacks detailed data on hip fracture trends despite being the country with the greatest increase in the pensioner-to-provider ratio in Europe. We reproduced a study on hip fracture incidence in a region of northern Spain (Cantabria) carried out 14 years ago to determine whether a secular trend to change is taking place. If such a trend could be found, our objective was to determine whether the effect is solely due to ageing or whether additional variables are involved. We assessed the incidence of hip fracture in patients aged ≥50 years through clinical records from Emergency Units and Orthopedic Surgical Units of all hospitals in the region of Cantabria in 1988 and 2002. A total of 318 new cases of hip fracture were recorded in 1988 and 490 in 2002 (54% increase; p<0.001). No significant changes were noticed following an adjustment for age. Women accounted for the increase in crude hip fracture incidence [246 women and 72 men suffered a hip fracture in 1988 compared to 404 women and 86 men in 2002 (64% increase in women and 19% increase in men; p<0.005 and not significant, respectively)]. The female:male ratio was 3.4 in 1988 versus 4.7 in 2002; following age-adjustment, no significant changes were found (1.8 in 1988 and 1.9 in 2002). The increase in crude hip fracture incidence was greater at cervical (versus trochanteric) sites. Patient residence, time of the year, site of fracture, kind of injury, previous contralateral hip fracture, length of stay, and peri-operative mortality did not differ significantly. In conclusion, a crude hip fracture incidence increase of about 50% in the northern Spanish region of Cantabria has taken place over the last 14 years. This effect does not persist after adjustments have been made for age. The crude rate increase occurred mainly at the expense of women, with a more noticeable rise in cervical fractures as opposed to trochanteric lesions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of hip fracture has been widely addressed in different parts of the world [1, 2]. Comparisons among many different countries have shown that large variations, sometimes more than tenfold, exist among populations with respect to hip fracture incidence [2], although the data upon which these estimates have been based are derived from studies that do not necessarily coincide with respect to time. On the other hand, some studies have revealed a secular trend toward an increase in the incidence of hip fracture [3–6] that does not always occur at the same pace and time in different countries. Therefore, to know the current relationship of hip fracture incidence between different parts of the world, figures must be brought up to date.
Increases in hip fracture incidence depend upon population ageing and a second age-independent factor [3–6], the nature of which is probably multifactorial and has been linked to industrial development and urbanization [5]. Declines in physical activity may play a major role [7]. Whatever the nature of this multifactorial component, its effect seems to have ended in most developed countries [5–10]. In fact, we might be witnessing a shift in the opposite direction as in some parts of North America age-adjusted annual hip fracture rates have fallen steadily over the past two decades [11, 12]. Current antiosteoporotic medications may account for this decrease [12], although this interpretation of the decline in hip fracture incidence has been questioned [13]. Hence, it is necessary to further analyze the role and behavior of these variables.
Spain is one of the countries for which no detailed data on hip fracture trends are available. However, a Report on Osteoporosis in the European Community (EC) [14] refers to Spain as the country with the highest increase in hip fracture-to-provider (working population) ratio. Moreover, within the EC, Spain has one of the fastest increase in pensioner-to-provider ratio, in concordance with the fact that its ageing index is among the highest in Europe.
Fourteen years ago we carried out a study [15] that established hip fracture incidence in the region of Cantabria, northern Spain. In the present report, we have used clinical information gathered in 2002 from hospitals and clinics in this same region in an attempt to determine whether changes in the incidence of hip fracture are occurring in Cantabria and, if so, which variables explain this trend.
Patients and methods
Study population
We have studied the incidence of hip fracture in patients aged ≥50 years in Cantabria, a region in northern Spain, in the years 1988 and 2002. Risk factors for hip fracture were also evaluated. Cantabria is a community of just over 500,000 inhabitants (see following paragraph), which is autonomous and functionally independent from a health care point of view, so that the patients are cared for in regional hospitals. This fact makes it a suitable place for epidemiological studies of this type.
All 1988 and 2002 clinical records from the Emergency Units and the Orthopedic Surgical Units of all hospitals in Cantabria were reviewed. In addition, all 1988 and 2002 admission and discharge files from these hospitals were reviewed for hip fracture diagnoses as a check for any patient that may have been missed from the aforementioned clinical records. The international classification of diseases, ninth edition (ICD-9-CM) codes used were 820.0–820.9. Once the patients were identified, their medical history of each was examined, and the clinical data we intended to analyze were collected. Patients who were not (semi-)permanent residents of the region were excluded from the study.
Working definitions and data collection
A diagnosis of hip fracture was made when there was radiological evidence of a fracture of the proximal femur. The type of fracture (cervical or trochanteric) was verified through radiological assessment. We excluded individuals under the age of 50 because hip fracture in younger adults is primarily due to trauma. Patients with pathological fractures (Paget's disease, neoplasm, bone cyst) were also excluded from this study. Fractures due to a severe traumatism (falling from more than standing height or the equivalent) were also excluded.
The following information was collected in all cases: age, sex, place of residence (urban or rural area), month, season, type and site of fracture, characteristics of the trauma, previous contralateral hip fracture, length of stay in the hospital, and perioperative mortality (defined as occurring during hospitalization or the first month after discharge).
Areas with more than 50,000 inhabitants were considered to be “urban” and represented 44.1% of the total population of the study group. Areas with fewer than 20,000 inhabitants were defined as “rural”. No areas with an intermediate number of inhabitants are found in Cantabria.
Population data
Data on the population of Cantabria for the two study periods were obtained from the census published by the Spanish National Institute of Statistics. In 1988, Cantabria had a population of 524,670 inhabitants. Of these, 161,000 (88,793 women and 72,207 men) were aged 50 years or over. The distribution across residence area showed that 71,041 people (40,581 women and 30,460 men) lived in urban areas and 89,959 (48,212 females and 41,747 males) in rural areas.
In 2002, the total population was 535,131 (2% more than in 1988). There were 189,158 inhabitants aged ≥50 years, 103,706 being women and 85,452 men. Of these, 85,601 lived in urban areas (48,956 females and 36,645 males) and 103,557 (54,750 women and 48,807 men) in rural districts. Therefore, over the 14-year period, there was a 17.5% increase in people older than 50, which was similar in both sexes. This ageing effect was somewhat higher in urban zones (20%) and slightly lower in rural areas (15%). These changes were similar for both sexes.
The increase in people older than 50 did not only occur in absolute terms but also in terms of percentages: 30.7% of the population in 1988; 35.3% in 2002. Furthermore, such an increase was not homogeneous, but higher in people of an older age. For instance, the number of women and men 80–89 years of age and older increased by 31% and 29%, respectively, while that of females and males aged 90 years or older did so by 54% and 52%, respectively.
Statistical analysis
Continuous variables are expressed as the arithmetic mean ± standard deviation and were compared by the two-tailed Student's t-test or Mann-Whitney U-test, as appropriate. Conventional chi-square and Fisher exact tests were used for analyzing discrete variables. A p value <0.05 was taken to indicate statistical significance. All the calculations were performed with SPSS (SPSS Inc., Chicago, Ill.) software.
Hip fracture rates (number of fractures per 100,000 people of the same age) were defined by 5-year intervals for the whole population of patients and for each sex separately. Intervals were settled on from 50 years up to the age of 84 years, with the age of 85 and above being categorized as a unique interval. Curves constructed by plotting fracture rates versus age were logarithmically transformed [ln incidence=a×age+b] in order to compare the slope and intercepts of those corresponding to 1988 and 2002.
Results
Overall results
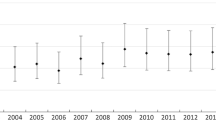
A total of 318 new cases of hip fracture were recorded in 1988 and 490 in 2002. This represents an increase of 54% (p<0.001) in the absolute number of hip fractures for the 14-year period (3.9% per year). When the 5-year interval fracture rates of 1988 were applied to the 2002 population (Table 1), the number of fractures obtained was 446. This figure is not significantly different (p=0.14) from the 490 fractures that were actually found. Therefore, the age-adjusted fracture rate did not change (Fig. 1). In fact, the logarithmic transformation of both curves generates two similar equations of non-significantly different slopes and interceptions: ln incidence=0.159 age−6.715 for 1988, and ln incidence=0.144 age−5.378 for 2002 (95% CI for “a” values are 0.125–0.193 for the first year and 0.107–0.181 for the second year; for “b”, [−9.14]–[−4.29] and [−10.03]–[ −4.51], respectively). Both logarithmic transformations fit adequately onto a straight line (R 2=0.956 and 0.938, respectively).
Sex distribution
With respect to the relation between sex and the incidence of hip fracture, 246 women and 72 men suffered a hip fracture in 1988 compared to 404 women and 86 men in 2002, which represents a 64% increase in women (p<0.005) and only a 19% increase in men (not significant). When 1988 five-year interval rates were applied to the 2002 population (see Table 1), women had 343 fractures and men, 102. These figures are respectively 15% lower (p=0.025) and 18.6% higher (p=0.9) than those actually found. However, Fig. 2 shows that patients 85 or older account for these differences, as the curves of hip fracture incidence in both periods of study do in fact overlap in both sexes, except for the last interval. For people within this interval, hip fracture rate increases in women and decreases in men. It is noteworthy that these two changes counteract one another, so that when both sexes are considered together, no differences are noted between the first and the second period of study with respect to this last interval, as is shown in Fig. 1.
The equations corresponding to the logarithmic transformation of 1988 and 2002 female curves are ln incidence=0.168 age−7.272 and ln incidence=0.164 age−6.824, respectively (“a”, 95% CI 0.130–0.207 and 0.129–0.200; “b”, 95% CI [−10.03]–[−4.51] and [−9.35]–[−4.29]); for male curves, the equations are ln incidence=0.135 age−5.262 and ln incidence=0.106 age−3.086, respectively (“a”, CI 0.094–0.176 and 0.050–0.162; “b”, CI [−8.20]–[−2.32] and [−7.08])–[0.91]). Slopes do not significantly differ in any of the cases.
The female:male ratio was 3.4 in 1988 and 4.7 in 2002. Following an age-adjustment, no significant changes were found (1.8 in 1988 and 1.9 in 2002).
The mean age of hip-fractured women in 1988 was 80±9 years, whereas in 2002, it was 84±8 years (p<0.00001). In men, the difference was smaller (77±11 years in 1988 compared to 78±12 years in 2002), and not significant (p=0.58). As has been repeatedly shown, incidence rates increased with age in both sexes, mainly from the seventh decade of life onwards (Figs. 1, 2).
Urban or rural distribution
In 1988, a total of 176 hip fractures occurred among residents of the rural areas. The corresponding figure for 2002 was 278, representing a 58% increase (p=0.0008). In urban areas, 142 hip fractures took place in 1988 and 212 in 2002 (a 50% increase; p=0.045).
For women in rural areas, 138 fractures occurred in 1988 and 226 in 2002 (a 64% increase; p=0.0006), whereas in urban zones, the corresponding figures were 108 and 178 (65% increase; p=0.01). For men in rural districts, 38 hip fractures were reported in 1988 and 52 in 2002 (a 37% increase, p=0.46); in urban areas, 34 hip fractures were reported in both 1988 and 2002 (p=0.44).
Therefore, the overall increase in hip fracture was similar in both rural and urban areas, as was the increase in the incidence of hip fracture in women. There were no significant differences in the incidence of hip fracture in men.
Type of trauma leading to hip fracture
Falling from standing height was the most frequent cause of fracture in both sexes (95% for women in both periods, and 95% versus 98% in men for the first and last year of the study, respectively). Therefore, no differences were noted with respect to the traumatic cause of the hip fracture.
Side and type of fracture
Some 61% of women and 58% of men suffered a left hip fracture in 1988. For the year 2002, the percentages were 53% and 54%, respectively.
Trochanteric fracture was the most frequent type of hip fracture in both sexes, with a total of 187 in 1988 and 264 in 2002 (a 41% increase, p=0.05). The absolute number of cervical fractures was 131 in 1988 and 226 in 2002 (a 72.5% increase, p=0.0004). Therefore, the rise in hip fracture incidence was higher for cervical than for trochanteric fractures.
In women, the number of trochanteric fractures was 147 in 1988 and 216 in 2002 (a 48% increase, p=0.027). For men, these figures were 40 and 47, respectively (18% increase, p=0.97). Cervical fractures in women amounted to 99 in 1988 and 188 in 2002 (a 90% increase, p=0.00007). In men, the number of cervical fractures was 32 in 1988 and 38 in 2002 (a 20% increase, p=0.98). Thus, the increase in hip fracture incidence between the two study periods not only occurred mostly at the expense of women, but was mainly due to cervical fractures.
A second hip fracture was diagnosed in 12.8% of the 2002 patients, a figure twice the 6% found in 1988. The cervical:trochanteric fracture ratio was similar in patients with a second hip fracture and in patients with their first hip fracture (44:56 and 46:54, respectively).
Seasonal variations
No seasonal differences were seen in 1998 or 2002. It may be worth mentioning, however, that when both sexes were considered separately in the second year of the study, men showed a higher incidence of fractures in the summer and winter (Fig. 3), a difference that was not observed in men or in either sex in 1988.
An interesting seasonal difference was also found between the occurrence of trochanteric and cervical fracture (Fig. 4): the incidence of the former peaked in the autumn, while that of the latter was at its lowest during this season.
Perioperative mortality
Overall mortality during hospitalization and within the first month after discharge was 6% (19 patients) in 1988 and 6.3% (31 patients) in 2002. By sex, 5% of women and 9% of men died in 1988 compared to 5% of women and 12.8% of men in 2002. No statistical differences were found in overall or sex-related mortality between the two periods.
Discussion
A marked increase in hip fracture incidence over time has been reported in the second half of the last century [1–6]. This rise has been shown to be due to ageing and another independent factor of uncertain nature [3, 6], which is probably related to industrial development [5]. Lower levels of physical activity [7] and a longer hip axis [16] related to a greater height account for some of the risk factors that may have shown a secular drift to change. A leveling off of the age-adjusted trend to an increase in the incidence of hip fracture has occurred in most Western countries during the second half of the last century [5–10], and some very recent studies even report a decrease [11, 12]. However, there are some European countries in which hip fracture incidence is increasing at more than the expected rate due to an ageing population; an example of this is Greece [17], with an annual incidence rise of 7.6%. Therefore, the concept that the increase in age-adjusted hip fracture incidence has ended in Western countries cannot be generalized, and further studies across Europe are much needed.
Large differences in hip fracture incidence have been reported between those countries with the highest values (Scandinavian countries, USA) and those with the lowest (Mediterranean countries) [2]. However, because of the different secular trends commented on above, these differences may have changed. Consequently, we consider it worthwhile to carry out up-to-date studies on hip fracture incidence. Such updating may be of particular interest if intervention thresholds based on absolute fracture risk are to be implemented internationally [1].
No detailed data on the trends in hip fracture incidence in Spain are available. Fourteen years ago we carried out [15] a study of hip fracture incidence in Cantabria (a region in northern Spain). The study reported here was carried out to analyze the changes in hip fracture incidence and characterize them. We found a 50% increase in crude hip fracture incidence; this accounts for about a 4% increase per annum, a figure slightly greater than the 1–3% usually mentioned in Western countries. However, this cipher remains within the expected limits when estimates for future hip fracture incidence are made assuming no age-specific increments [18].
No significant changes appeared when adjustment for age was allowed for. Thus, we conclude that the observed increase in crude hip fracture incidence was only attributable to ageing – and not to an age-adjusted trend. Group analysis by sex confirmed the same phenomenon. In this case, however, there was an exception to this general rule, as in the group of patients over 84 years, fracture incidence was higher in women and lower in men in 2002 than in 1988. These differences must be considered in the light of the fact that this last age interval is less reliable than the rest of the intervals for the following reasons. Firstly, there is no upper limit defined in this subset of the sample. Hence, comparisons between both periods are limited by a greater variance in the variables we analyzed (for instance, female longevity was greater in the second period of the study). Second, in several studies of hip fracture incidence [19–21], particularly those referring to men, a decline was observed in the very elderly. This finding could reflect a selection bias or simply fewer “hips at risk”, since a large proportion of these patients has already broken one or more hips. If this oldest group is deleted from our dataset, our overall results support the conclusion that even if we have found an increase in crude hip fracture incidence, no changes in age-adjusted incidence in either sex have occurred.
The observed increase in crude hip fracture incidence took place mainly at the expense of women, in whom it rose by 64%, in contrast with a 19% rise in men. Recent reports emphasize that osteoporosis must be considered to be not only a female, but also a male problem. However, it seems that the increase in the osteoporosis burden mostly affects women in relation to their greater life expectancy because, as anticipated, the rise in the absolute number of fractures mainly occurred at the expense of the oldest population.
A surprising finding in our study relates to the cervical-to-trochanteric fracture ratio. We found a greater increase in cervical fractures (72.5%) than in trochanteric fractures (41%), as opposed to previous reports [19, 22, 23]. Trochanteric fractures are considered to be more typical of osteoporosis than cervical fractures [24]. In fact, the ratio of cervical-to-trochanteric fractures is higher at younger ages [25–27]. Therefore, we expected a greater increase in trochanteric fractures. We can offer no explanation for our finding, although there are some differences between elderly people in both periods of study which merit consideration. For instance, according to data provided by the Inspección de Farmacia del Servicio Cántabro de Salud, osteoporosis drug consumption has greatly increased between 1988 and 2002 as indicated by the number of calcium and vitamin D packages that were sold (tripled over the 14 years), the number of bisphosphonate packages sold (significant increase from almost zero in 1988 to a very large number in 2002; currently, the number sold is fourfold that for calcium+vitamin D packages), and the increase in calcitonin packages sales (fivefold). It is conceivable that osteoporosis medications decrease the tendency to suffer the most typically osteoporotic fracture. In fact, in a recent paper, Jaglal et al. [12] have reported data supporting the possibility that the use of osteoporosis drugs may be changing osteoporosis epidemiology. A National Health System survey on physical activity conducted in Spain shows a relevant growth in the proportion of people older than 65 that carry out physical activity in 2001 as compared to 1987 (for example, in 1987, 80% of elderly people were classified as carrying out no physical activity, while 20% carried out sporadic activity; in 2001, only 45% were classified in the nonphysical activity group). Physical activity could decrease osteoporosis prevalence and, therefore, the most typical osteoporotic (trochanteric) fractures. Finally, the average height in people older than 65 in Cantabria, as personally recalled in survey questionnaires, was 161.4 cm in 1987 and 163.5 cm in 2001 (data from an epidemiological survey currently under way, carried out by one of the authors, J. Llorca). This increase in height may imply a longer hip axis, and a greater tendency for femoral neck fractures. On the other hand, we did not find (data not shown) that risk factors typically associated with low bone mass (smoking, surgical menopause, previous fragility fracture, hyperthyroidism, diabetes) or osteoporotic fractures (visual problems or benzodiazepine use) showed a stronger relationship with trochanteric than with cervical fractures. Clearly, more studies are required to clarify this point.
A seasonal pattern for hip fracture incidence was found for men in 2002, but not in 1988. The pattern consisted of an increase in fracture rate in the summer and winter relative to the spring and autumn. A winter increase has been widely described in countries with temperate climates [7], perhaps related to shorter daylight time and frozen ground. The summer peak could be related to an increase in physical activity outdoors at this time of the year, particularly since it appears in men, who are more prone to taking part in sports. In addition, it may be worth pointing out that summer was the only season in which the absolute number of cervical fractures was greater than the absolute number of trochanteric fractures. However, a simple chance association cannot be ruled out. No seasonal differences were found in women.
Large differences in hip fracture incidence have been reported between countries. The highest values have been described [2] in the Scandinavian countries, with a relative incidence in women of 1.3 compared to the incidence of hip fractures in the US. In Southern European countries the figures have been lower. Specifically, the incidence in Spain was reported as being about 70% of the US incidence (and therefore, about 55% of the Scandinavian incidence). However, changes in secular trends may modify these relationships. To check this, we have compared the hip fracture incidence found in our region with that recently published by Finsen et al. [23] for Norway by applying our 2002 five-year interval-rates to the Norwegian female population. The Spanish:Norwegian women fracture ratio we found was 0.43, which is not very different from the one previously described. We have also applied our 2002 5-year interval rates to the US population [28] and compared the results to the American rates published in the review by Gullberg et al. [18]. The Spanish:American women fracture ratio was found to be 0.63, again quite similar the one previously described. Therefore, it seems that the relationship between hip fracture incidence in Western countries, once the secular trend has leveled off, is quite stable.
Our study has the limitations of any retrospective study. However, as stated above, epidemiological studies are particularly reliable in the Cantabria region because of its health system characteristics (public, centralized, autonomous and independent from that of other regions), which allow us to gather information easily. This reliability is even greater for acute events needing surgical treatment, which are taken care of in hospital settings.
In conclusion, we have found an increase in crude hip fracture incidence of about 50% in the northern Spanish region of Cantabria over the last 14 years. No changes however, were observed in terms of age-adjusted rates, indicating the absence of a secular trend to hip fracture increase or decrease due to factors unrelated to ageing. The crude rate increase occurred mainly at the expense of women who, consequently, are going to be the population mainly responsible for the increase in the osteoporosis economical burden. Finally, the relationship between age-adjusted hip fracture incidence in Spain and that of those countries with the highest values seems to have remained constant.
References
Kanis JA, Johnell O, De Laet C, Jonsson B, Oden A, Ogelsby AK (2002) International variations in hip fracture probabilities: implications for risk assessment. J Bone Miner Res 17:1237–1244
De Laet C, Reeve J (2001) Epidemiology of osteoporotic fractures in Europe. In: Marcus R, Feldman D, Kelsey J (eds) Osteoporosis. Academic, San Diego, pp 585–597
Boyce WJ, Vessey MP (1985) Rising incidence of fracture of the proximal femur. Lancet 1:150–151
Rodrigues JG, Sattin RW, Waxweiler RJ (1989) Incidence of hip fractures. United States 1970–1983. Am J Prev Med 5:175–181
Melton LJ III, O´Fallon WM, Riggs BL (1987) Secular trends in the incidence of hip fractures. Calcif Tissue Int 41:57–64
Gullberg B, Duppe H, Nilsson B, Redlund-Johnell I, Sernbo I, Obrant K, Johnell O (1993) Incidence of hip fractures in Malmö, Sweden (1950–1991). Bone 14[Suppl 1]:S23–S29
Cooper C (2003) Epidemiology of osteoporosis. Primer on the metabolic bone disease and disorders of mineral metabolism. American Society for Bone and Mineral Research, Washington D.C., pp 307–313
Huusko TM, Karppi P, Avikainen V, Kautiainen H, Sulkava R (1999) The changing picture of hip fractures: dramatic change in age distribution and no change in age-adjusted incidence within 10 years in Central Finland. Bone 24:257–259
Agnusdei D, Camporeale A, Gerardi D, Rossi S, Bocchi L, Genneari C (1993) Trends in the incidence of hip fracture incidence in Siena, Italy, from 1980 to 1991. Bone 14[Suppl 1]:S24–S34
Rogmark C, Sernbo I, Johnell O, Nilsson JA (1999) Incidence of hip fractures in Malmo, Sweden, 1992–1995. A trend-break. Acta Orthop Scand 70:19–22
Melton LJ III, Atkinson EJ, Madhok R (1996) Downturn in hip fracture incidence. Public Health Rep 111:146–150
Jaglal SB, Weller I, Mamdani M, Hawker G, Kreder H, Jaakkimainen L, Adachi JD (2005) Population trends in BMD testing, treatment, and hip and wrist fracture rates: are the hip fracture projections wrong? J Bone Miner Res 20:898–905
Melton LJ III, Kanis JA, Johnell O (2005) Potential impact of osteoporosis treatment on hip fracture trends. J Bone Miner Res 20:895–897
Working Party from European Union Member States. Report on osteoporosis in the European Community: current status and recommendations for the future. http://www.effo.org
Olmos JM, Martinez J, Garcia J, Matorras P, Moreno JJ, Gonzalez-Macias J (1992) Incidencia de fractura de cadera en Cantabria. Med Clin (Barc) 99:729–731
Reid IR, Chin K, Evans MC, Jones JG (1994) Relation between increase in length of hip axis in older women between 1950s and 1990s and increase in age specific rates of hip fracture. BMJ 309:508–509
Paspati I, Galanos A, Lyritis GP (1998) Hip fracture epidemiology in Greece during 1977–1992. Calcif Tissue Int 62:542–547
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7:407–413
Lauritzen JB, Schwarz P, Lund B, McNair P, Transbol I (1993) Changing incidence and residual lifetime risk of common osteoporosis-related fractures. Osteoporos Int 3:127–132
Chang KP, Center JR, Nguyen TV, Eisman JA (2004) Incidence of hip and other osteoporotic fractures in elderly men and women: dubbo osteoporosis epidemiology study. J Bone Miner Res 19:532–536
Löfman O, Berglund K, Larsson L, Toss G (2002) Changes in hip fracture epidemiology: redistribution between ages, genders and fracture types. Osteoporos Int 13:18–25
Nagant de Deuxchaisnes C, Devogelaer JP (1988) Increase in the incidence of hip fractures and of the ratio of trochanteric to cervical hip fractures in Belgium. Calcif Tissue Int 42:201–203
Finsen V, Johnsen LG, Trano G, Hansen B, Sneve KS (2004) Hip fracture incidence in central Norway: a followup study. Clin Orthop Relat Res 419:173–178
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16[Suppl 2]:S3–S7
Yan L, Zhou B, Prentice A, Wang X, Golden MH (1999) Epidemiological study of hip fracture in Shenyang, People's Republic of China. Bone 24:151–155
Hinton RY, Lennox DW, Ebert FR, Jacobsen SJ, Smith GS (1995) Relative rates of fracture of the hip in the United States. Geographic, sex and age variations. J Bone Joint Surg 77:695–702
Levy AR, Mayo NE, Grimard G (1995) Rates of transcervical and pertrochanteric hip fractures in the province of Quebec, Canada, 1981–1992. Am J Epidemiol 142:428–436
Census Bureau, census 2000, summary file 1 http://factfinder.census.gov
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hernández, J.L., Olmos, J.M., Alonso, M.A. et al. Trend in hip fracture epidemiology over a 14-year period in a Spanish population. Osteoporos Int 17, 464–470 (2006). https://doi.org/10.1007/s00198-005-0008-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-005-0008-7