Abstract
Prognosis of metastatic melanoma improved with the development of checkpoint inhibitors. The role of tumor infiltrating lymphocytes (TILs) in lymph node metastases of stage III melanoma remains unclear. We retrospectively characterized TILs in primary melanomas and matched lymph node metastases (stage III melanoma) of patients treated with the checkpoint inhibitor ipilimumab. Tumor infiltrating lymphocytes were characterized for CD3, CD4, and CD8 expressions by immunohistochemistry. 4/9 patients (44%) responded to treatment with ipilimumab (1 complete and 2 partial remissions, 1 stable disease). All responders exhibited CD4 and CD8 T-cell infiltration in their lymph node metastases, whereas all non-responders did not show an infiltration of the lymph node metastasis with TILs. The correlation between the presence and absence of TILs in responders vs. non-responders was statistically significant (p = 0.008). Median distant metastases free survival, i.e., progression from stage III to stage IV melanoma, was similar in responders and non-responders (22.1 vs. 19.3 months; p = 0.462). Median progression free and overall survival show a trend in favor of the patients having TIL rich lymph node metastases (6.8 vs. 3.3 months, p = 0.09; and all alive at last follow-up vs. 8.2 months, respectively, p = 0.08). Our data suggest a correlation between the T-cell infiltration of the lymph node metastases in stage III melanoma and the response to ipilimumab once these patients progress to stage IV disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the introduction of immunotherapy with checkpoint inhibitors (anti-CTLA4 and anti-PD-1/anti-PD-L1 monoclonal antibodies), the survival of patients suffering from stage IV melanoma has improved dramatically. However, reliable predictive markers for response and outcome are still sparse [1,2,3,4,5,6]. Both inhibitions of the CTLA-4 and the PD-1/PD-L1 axis lead to activation of T cells against tumor cells [1, 2]. Tumeh et al. showed that the detection of pre-existing CD8 T cells at the tumor margin of melanoma metastases has predictive value for treatment responses [7].
Several publications have emphasized the importance of immune cells and patterns of inflammation within primary melanomas for long-term survival of patients with metastatic disease. Overall, the discovery of the prognostic values of tumor infiltrating lymphocytes (TILs) has been a key event for the subsequent progress in tumor immunology and immunotherapy of solid cancers [8,9,10,11,12].
However, only little is known about the significance of tumor infiltrating immune cells in lymph node metastases. While the lymph node is often the first location of metastases in melanoma patients, it is also likely the first strong contact site of cancer cells and/or tumor antigens with the adaptive immune system. In the lymph node, specialized antigen presenting cells, including dendritic cells, presents antigens in the context of MHC classes I and II to CD8 and CD4 T cells, respectively. The immunological microenvironment in a (sentinel) node may, therefore, influence the risk for tumor spread and may help to sustain the melanoma. Several markers in lymph nodes (i.e., decreased CD8+ and increased CD30+) are associated with tumor growth, supporting the theory that a dysfunctional immunological microenvironment in lymph nodes may play a key role as a predictor of poor clinical outcome [13,14,15,16,17,18]. None of these factors has previously been analyzed in the context of checkpoint inhibitor treatment.
Recently, a phase III study compared ipilimumab with placebo in the adjuvant setting in stage III melanoma. Ipilimumab resulted in a higher rate for overall survival (OS), recurrence free survival, and distant metastases free survival (DMFS). The role of the immunological microenvironment of the metastatic lymph node at diagnosis was not considered [19].
The aim of this pilot study was: (1) to assess the primary tumor and matched lymph node metastases for TILs and (2) to correlate these results with response and survival to immunotherapy with the CTLA-4 antibody ipilimumab.
Materials and methods
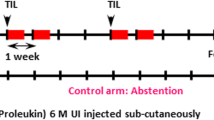
We retrospectively collected data of patients who were initially diagnosed with lymph node positive melanoma (stage III) and later developed stage IV disease requiring systemic treatment with ipilimumab. We chose ipilimumab for two reasons: Ipilimumab was the first checkpoint inhibitor available in Switzerland, and more importantly, adjuvant data for stage III melanoma and ipilimumab had been published, while no adjuvant data for anti-PD-1 were available at the time of the analysis [19].
We identified and included a total of nine patients with tissue available from the primary tumor, the matched lymph node metastases, and complete data from the clinical follow-up during treatment with ipilimumab.
Response to treatment was assessed according to RECIST 1.1. Disease control was defined as stable disease, partial remission, or complete remission [20].
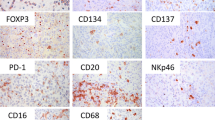
Immunohistochemistry of formalin-fixed paraffin-embedded full tissues sections (4 μm) was performed as previously described [21]. Briefly, sections were pre-incubated on the BondMax system (Leica, Mannheim, Germany) in Bond Epitope Retrieval Solution 2 for 30 min at 95 °C and then stained for CD3, CD4, CD8, and Melan-A. The Bond Polymer Refine Red Detection kit (DS9390, Leica) was used for these biomarkers.
Immunohistochemical staining was carried out on the VENTANA BenchMark ULTRA automated staining platform using the OptiView detection kit (VMSI, Catalog No. 760-700).
Stained samples were scored on a three-point scale based on the percentages of infiltrating TILs in the tumor: none: no infiltration; poor: 1–30% infiltration; and rich: 31–100% infiltration.
All histopathological slides of each case were independently reviewed by two board-certified pathologists in a blinded fashion with respect to the samples and clinical data (Viktor H. Koelzer and Kirsten D. Mertz). The list of antibodies used for the analysis can be found in the Supplementary Table 1.
Kaplan–Meier curves and the Gehan–Breslow test were used to assess different time-to-event outcomes in patient subgroups [DMFS, progression free survival (PFS), OS].
Results
The median age of the patients was 63 years. Five patients were diagnosed with a nodular subtype melanoma (55%) and BRAF was mutated in three patients (33%). Detailed patient characteristics including sites of metastases and tumor burden with the number of involved organs are shown in Table 1. Four out of nine (44%) patients showed a response to treatment with ipilimumab, including one complete remission, two partial responses, and one stable disease.
Our analysis of lymphocyte infiltration (CD3, CD4, and CD8 positive T cells) in primary melanoma showed rich TILs in two responders compared to poor TILs in non-responders (Fig. 1a). However, this was not statistically significant with a p value of 0.167 (Fisher’s exact test). The localization of the metastasis within the lymph node did not correlate with survival.
Representative comparison of histology panels of primary tumors and matched lymph node metastases of stage III melanoma (responders vs. non-responders to ipilimumab treatment). a Primary melanoma of a good responder (upper panel) and a non-responder (lower panel). b Lymph node metastasis of a good responder (upper panel) and a non-responder (lower panel). Note the marked infiltration of lymphocytes present only in the lymph node metastasis of the good responder. c Combined Melan-A/CD8 staining of lymph node metastases of melanoma. While the metastasis of a good responder to ipilimumab therapy shows rich infiltration with CD8 T lymphocytes (left), there is no such infiltrate in the metastasis of a non-responder (right). Melan-A in red and CD8 T lymphocytes in brown
In contrast to the primary tumors, the investigated lymph nodes showed a difference in tumor infiltrating T cells between responders and non-responders. All responders showed infiltration by CD3, CD4, and CD8 T cells within the lymph node metastases (Fig. 1b, c). Furthermore, the correlation between the presence and the absence of TILs in responders vs. non-responders was statistically significant using Fisher’s exact test (p = 0.008).
Detailed characteristics of primary tumors and lymph nodes metastases are presented in Tables 2 and 3.
The median PFS, i.e., time from start ipilimumab to progression, was 6.8 months in responders and 3.3 months in non-responders. All four responders were alive at the time of our analysis (median follow-up of 41.8 months), while the median survival in non-responders was 8.2 months (p = 0.08 after right censoring). In the group of non-responders, three out of five patients had already passed away due to disease progression. DMFS was not significantly different in responders vs. non-responders (22.1 months vs. 19.3 months). Results are shown in Table 1. p values were 0.462 for DMFS, 0.086 for PFS and 0.081 for OS (calculated using the Gehan–Breslow test). While these clinical read-outs show a trend, they are not significant.
Discussion
Although prognosis of metastatic melanoma has significantly improved in the era of checkpoint inhibitor therapy, there are still no reliable and validated predictive and prognostic biomarkers for response and survival. The role of PD-L1 expression on tumor cells as predictive factor for response to the two PD-1 inhibitors nivolumab and pembrolizumab or the combination of ipilimumab and nivolumab is being established but still require further refinements. Different cutoffs and methods for analysis are used [2, 3, 5, 6]. LDH seems to be a good clinical marker correlating with response and outcome in patients treated with ipilimumab and PD-1 inhibitors, even though responses can also be seen in LDH-high patients [6, 22,23,24,25]. Tumeh and colleagues suggested a correlation between pre-existing CD8 T-cell infiltrates in tumor metastases before anti-PD-1 treatment and objective clinical response [7]. No such data with CTLA-4 antibodies are available. Sentinel lymph node biopsy is used in many countries for refined staging, but removing the sentinel lymph node itself does not improve survival, as has been shown in a large phase III trial [26].
To date, no study has investigated the predictive value on therapy response of the immunological environment of metastatic lymph nodes in stage III melanoma and subsequent treatment with checkpoint inhibitors when the patients develop metastatic stage IV disease. Previous work from the chemotherapy era suggests that there is an association between outcome and the immunological environment in lymph node metastases [13,14,15,16,17]. Kakavan et al. analyzed lymph node metastases for CD3, CD4, CD8, PD-1, and PD-L1. They found a statistically significant association between recurrence free survival and OS and the number of intratumoral CD3+ TILs [17]. Nevertheless, these findings were reported in the era before checkpoint inhibitors.
Our data suggest that TILs in the lymph node may be a positive predictive factor for response to ipilimumab with improvement of DMFS, PFS an OS. TILs in the primary tumor did not predict the response to immunotherapy. Our findings indicate that the immunologic environment in the lymph node may be more relevant than previously assumed in the context of the new treatment options with checkpoint inhibitors. Possibly, T-cell infiltration in tumor metastases in the lymph node may correlate with clinical outcome as opposed to T-cell infiltration in primary tumors or metastases at other locations.
Our data may also be meaningful for the adjuvant setting. Eggermont et al. recently showed that adjuvant treatment of high-risk stage III melanoma patients with ipilimumab results in prolonged survival. A subgroup analysis demonstrated a clear benefit in patients with ≥four positive lymph nodes (stage IIIC). However, the survival benefit of this expensive treatment option has to be put in the context of potentially severe autoimmune-related side effects [19]. To our knowledge, currently, no predictive or prognostic markers are available to predict those effects. The fact that survival benefit increases with the number of lymph node metastases may underline the importance of their immunological microenvironment. Our finding that TILs in tumor positive lymph nodes may correlate with response and outcome after developing stage IV disease may thus be helpful to select patients who may potentially benefit from adjuvant treatment in stage III melanoma using ipilimumab.
We are aware that the small case number of nine patients is a major limiting factor. We would like to point out that this is a hypothesis generating pilot study. Our data suggest studying TILs in lymph nodes in larger patient cohorts, preferably in a prospective setting with patients treated with CTLA-4 and PD-1/PD-L1 specific antibodies.
Abbreviations
- DMFS:
-
Distant metastases free survival
- PFS:
-
Progression free survival
References
Hodi FS, O’Day SJ, McDermott DF et al (2010) Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 363(8):711–723. doi:10.1056/NEJMoa1003466
Robert C, Schachter J, Long GV et al (2015) Pembrolizumab versus ipilimumab in advanced melanoma. N Engl J Med 372(26):2521–2532. doi:10.1056/NEJMoa1503093
Weber JS, D’Angelo SP, Minor D et al (2015) Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol 16(4):375–384. doi:10.1016/S1470-2045(15)70076-8
Robert C, Long GV, Brady B et al (2015) Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med 372(4):320–330. doi:10.1056/NEJMoa1412082
Larkin J, Chiarion-Sileni V, Gonzalez R et al (2015) Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med 373(1):23–34. doi:10.1056/NEJMoa1504030
Ribas A, Puzanov I, Dummer R et al (2015) Pembrolizumab versus investigator-choice chemotherapy for ipilimumab-refractory melanoma (KEYNOTE-002): a randomised, controlled, phase 2 trial. Lancet Oncol 16(8):908–918. doi:10.1016/S1470-2045(15)00083-2
Tumeh PC, Harview CL, Yearley JH et al (2014) PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature 515(7528):568–571. doi:10.1038/nature13954
Oble DA, Loewe R, Yu P et al (2009) Focus on TILs: prognostic significance of tumor infiltrating lymphocytes in human melanoma. Cancer Immun 9:3
Clark WH Jr, Elder DE, Dt Guerry et al (1989) Model predicting survival in stage I melanoma based on tumor progression. J Natl Cancer Inst 81(24):1893–1904
Clemente CG, Mihm MC Jr, Bufalino R et al (1996) Prognostic value of tumor infiltrating lymphocytes in the vertical growth phase of primary cutaneous melanoma. Cancer 77(7):1303–1310. doi:10.1002/(SICI)1097-0142(19960401)77:7<1303:AID-CNCR12>3.0.CO;2-5
Mackensen A, Ferradini L, Carcelain G et al (1993) Evidence for in situ amplification of cytotoxic T-lymphocytes with antitumor activity in a human regressive melanoma. Cancer Res 53(15):3569–3573
Tefany FJ, Barnetson RS, Halliday GM et al (1991) Immunocytochemical analysis of the cellular infiltrate in primary regressing and non-regressing malignant melanoma. J Invest Dermatol 97(2):197–202
Rodolfo M, Castelli C, Rivoltini L (2014) Immune response markers in sentinel nodes may predict melanoma progression. Oncoimmunology 3:e28498. doi:10.4161/onci.28498
Cochran AJ, Huang RR, Lee J et al (2006) Tumour-induced immune modulation of sentinel lymph nodes. Nat Rev Immunol 6(9):659–670. doi:10.1038/nri1919
Takeuchi H, Kitajima M, Kitagawa Y (2008) Sentinel lymph node as a target of molecular diagnosis of lymphatic micrometastasis and local immunoresponse to malignant cells. Cancer Sci 99(3):441–450. doi:10.1111/j.1349-7006.2007.00672.x
Mohos A, Sebestyen T, Liszkay G et al (2013) Immune cell profile of sentinel lymph nodes in patients with malignant melanoma - FOXP3 + cell density in cases with positive sentinel node status is associated with unfavorable clinical outcome. J Transl Med 11:43. doi:10.1186/1479-5876-11-43
Kakavand H, Vilain RE, Wilmott JS et al (2015) Tumor PD-L1 expression, immune cell correlates and PD-1 + lymphocytes in sentinel lymph node melanoma metastases. Mod Pathol 28(12):1535–1544. doi:10.1038/modpathol.2015.110
Vallacchi V, Vergani E, Camisaschi C et al (2014) Transcriptional profiling of melanoma sentinel nodes identify patients with poor outcome and reveal an association of CD30(+) T lymphocytes with progression. Cancer Res 74(1):130–140. doi:10.1158/0008-5472.CAN-13-1672
Eggermont AM, Chiarion-Sileni V, Grob JJ et al (2016) Prolonged survival in stage III melanoma with ipilimumab adjuvant therapy. N Engl J Med 375(19):1845–1855. doi:10.1056/NEJMoa1611299
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–247. doi:10.1016/j.ejca.2008.10.026
Kempf W, Zollinger T, Sachs M et al (2014) Granulomas are a source of interleukin-33 expression in pulmonary and extrapulmonary sarcoidosis. Hum Pathol 45(11):2202–2210. doi:10.1016/j.humpath.2014.07.011
Kelderman S, Heemskerk B, van Tinteren H et al (2014) Lactate dehydrogenase as a selection criterion for ipilimumab treatment in metastatic melanoma. Cancer Immunol Immunother 63(5):449–458. doi:10.1007/s00262-014-1528-9
Diem S, Kasenda B, Martin-Liberal J et al (2015) Prognostic score for patients with advanced melanoma treated with ipilimumab. Eur J Cancer 51(18):2785–2791. doi:10.1016/j.ejca.2015.09.007
Diem S, Kasenda B, Spain L et al (2016) Serum lactate dehydrogenase as an early marker for outcome in patients treated with anti-PD-1 therapy in metastatic melanoma. Br J Cancer 114(3):256–261. doi:10.1038/bjc.2015.467
Delyon J, Mateus C, Lefeuvre D et al (2013) Experience in daily practice with ipilimumab for the treatment of patients with metastatic melanoma: an early increase in lymphocyte and eosinophil counts is associated with improved survival. Ann Oncol 24(6):1697–1703. doi:10.1093/annonc/mdt027
Morton DL, Thompson JF, Cochran AJ et al (2014) Final trial report of sentinel-node biopsy versus nodal observation in melanoma. N Engl J Med 370(7):599–609. doi:10.1056/NEJMoa1310460
Acknowledgements
We would like to thank Burkhard Ludewig for scientific input. This work was funded by the Swiss National Science Foundation, the Philanthropic Research Foundation and the Stiftung für naturwissenschaftliche und technische Forschung. Lukas Flatz holds a Swiss National Science Foundation-professorship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
The study was approved by the local Research Ethics Committee (Ethikkommission Ostschweiz): BASEC- Project ID: 2016-01161 “Retrospective histopathological characterization of lymph node metastases and correlation with response to immunotherapy in melanoma patients”.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Diem, S., Hasan Ali, O., Ackermann, C.J. et al. Tumor infiltrating lymphocytes in lymph node metastases of stage III melanoma correspond to response and survival in nine patients treated with ipilimumab at the time of stage IV disease. Cancer Immunol Immunother 67, 39–45 (2018). https://doi.org/10.1007/s00262-017-2061-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-017-2061-4