Abstract
Purpose
To compare the clinical outcomes between unilateral and bilateral metal stenting for patients with malignant hilar biliary obstruction (MHO).
Methods
This is a single-center, open-label, prospective, randomized study. Between January 2016 and March 2018, patients with MHO who were treated by percutaneous unilateral or bilateral metal stenting were enrolled. The primary endpoint was stent dysfunction. The secondary endpoints included technical success, clinical success, adverse events, and death. The protocol is registered at ClinicalTrials.gov (identifier: NCT02649712).
Results
A total of 72 patients were randomly grouped for the unilateral (n = 36) or bilateral (n = 36) stenting. The bilateral stenting was performed through the side-by-side technique. While technically, the rates of success of unilateral and bilateral stenting were 83.3% (30/36) in both the cases (P = 1.000), the clinical rates of success in unilateral and bilateral stenting were 90.0% (27/30) and 96.7% (29/30), respectively (P = 0.605). Based on the per-protocol analysis, stent dysfunction was found in 5 and 3 patients in unilateral and bilateral groups, respectively (16.7% vs. 10.0%, P = 0.704). No predictor was observed to influence stent dysfunction. The median cumulative survival in the unilateral group was 122 days and in the bilateral group was 125 days (P = 0.844). We also observed higher levels of post-operative total bilirubin and pre-operative alanine aminotransferase, and the absence of post-operative anticancer treatment as predictors of worse survival.
Conclusion
When compared, the bilateral and unilateral stentings provide a similar clinical effectiveness in patients with MHO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The common causes of malignant hilar biliary obstruction (MHO) include malignant tumors of the hepatobiliary system or metastatic hilar lymph nodule [1,2,3,4,5,6,7], and nearly 70–80% of MHO cases are inoperable [1]. Thus, to alleviate jaundice and improve the liver function, normally a percutaneous or endoscopic stenting is performed [1,2,3,4,5,6,7]. To achieve long-term patency and survival, palliation using metal stent is considered superior to plastic stent [7,8,9].
Notwithstanding, the issue of debate still remains whether unilateral or bilateral stenting should be performed for MHO. While several studies report the superiority of bilateral stenting over unilateral stenting in terms of long-term patency [5,6,7], few other studies reveal a similar clinical effectiveness of unilateral and bilateral stenting [2,3,4]. Although previous studies have compared unilateral and bilateral stenting for MHO, most of them are of retrospective type [2,3,4,5, 7]. In addition, the methods of bilateral stenting were different in previous studies. Some researchers used side-by-side (SBS) technique [2, 5], while some researchers used stent-in-stent (SIS) technique [3, 4].
The aim of our study was to conduct a single-center, randomized, prospective study to compare the clinical outcomes of unilateral and bilateral (SBS technique) metal stenting for patients with MHO.
Materials and methods
The review board of our institute approved this single-center, open-label, prospective, randomized study. Written informed consent was obtained from all enrolled patients. The protocol is registered at ClinicalTrials.gov (identifier: NCT02649712).
Study design
From a total of 91 patients with MHO who were admitted to our center from January 2016 to March 2018, 72 patients met the eligibility criteria and were enrolled in this study (Fig. 1). The criteria for inclusion were: (a) definite diagnosis of MHO; and (b) inoperable cases. The criteria for exclusion were: (a) Bismuth I type MHO; (b) a history of previous hepatolobectomy; (c) Eastern Cooperative Oncology Group (ECOG) performance status (PS) ≥ 4; (d) severely dysfunctional heart, kidney, lung, and coagulation; and (e) inability to provide informed consent.
Diagnosis of hilar biliary obstruction was confirmed by the magnetic resonance cholangiopancreatography (MRCP) and abdominal computed tomography (CT) results. The MHOs were caused by cholangiocarcinoma (38 patients), gallbladder carcinoma (18 patients), hepatocellular carcinoma (7 patients), and metastatic lymph nodule (9 patients). The gallbladder carcinoma and cholangiocarcinoma was confirmed by percutaneous biopsy. The hepatocellular carcinoma was confirmed by abdominal contrast-medium enhanced CT with alpha-fetoprotein results, and finally, patients’ primary tumor history and abdominal CT findings helped establish the metastatic lymph nodule diagnosis.
Randomization
Eligible patients were randomized in a 1:1 ratio to the unilateral or bilateral stenting groups with the method of block randomization (block size: 4). The computer-generated random numbers were kept in sequentially numbered, opaque, sealed envelopes. Before starting the stent insertion, the randomized assignments were opened by a staff member of the Science and Education department, who had no further role in this trial.
Procedures
The stent insertion was performed within 24 h after randomization. The procedure of puncturing the intrahepatic biliary tract was performed under the combined fluoroscopic and ultrasonic guidance.
For the unilateral stenting, the right intrahepatic biliary route was initially considered. A 21G Chiba needle (Cook, Bloomington, IN, USA) was used to puncture the intrahepatic biliary tract. The extent and degree of the obstruction were visualized by injecting the contrast medium through the needle. After that, a 6F sheath (Cook) was placed into the intrahepatic biliary tract. The obstructed site was detected by a 5F VER catheter (Cordis, Hialeah, FL, USA) and a 0.035-inch guide wire (Terumo, Tokyo, Japan) that were maneuvered through the sheath. As the catheter and guide wire crossed the obstructed site and went into the duodenum, the guide wire was exchanged by a 0.035-inch stiff guide wire (Cook). Finally, at the site of obstruction, the bare self-expanded metal stent (Micro-Tech, Nanjing, China) was released. It was ensured that the stent extended on either side at least 10 mm past the obstruction.
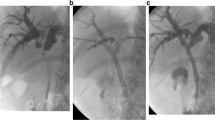
For the bilateral stenting, bilateral intrahepatic biliary tracts were punctured individually, then two stiff guide wires were placed side by side. Finally, two stents were released simultaneously by SBS technique (Fig. 2).
After stenting, all patients in both group were inserted with a 8.5F temporary biliary drainage catheter (Cook) for 5 days. All patients were treated by hemostasis and anti-inflammatory drugs for 5 days.
Follow-up and definitions
In both groups, post-stenting follow-up was routinely performed at 2 weeks, 1 and 3, and then every 3 months and included physical examination, CT test, and liver function test. The patients were advised to visit the hospital any time if they experienced recurrent cholangitis or jaundice. The last follow-up was conducted until the patients’ death or 31 October 2019 (the date of the last follow-up).
Technical success was defined as release of the unilateral or bilateral stent successfully beyond the obstructed site, together with a flow of contrast medium through the stent [2, 6]. Clinical success was defined as a pre-operative reduction by at least 30% in the level of total bilirubin within 2 weeks after stenting [2, 10]. Stent dysfunction was defined as a recurrence of jaundice and/or cholangitis due to tumor growth (in- or over-growth), sludge, stent migration, or other reasons. Ingrowth was defined as stenosis inside the stent that could not be cleared by balloon sweep or biliary drainage [11]. Overgrowth was defined as stenosis above or below the stent [11]. Sludge was defined as an obstruction that could be cleared by balloon sweep or biliary drainage [4]. Adverse events were divided into early (≤ 30 days) and late (> 30 days) events. Patency was defined as the period from stent insertion to stent dysfunction, death, or the date of the last follow-up.
The primary endpoint was stent dysfunction. The secondary endpoints included technical success, clinical success, adverse events, and death.
Statistical analyses
The primary analysis was evaluated on the basis of comparison of superiority among unilateral and bilateral stenting for the stent dysfunction primary endpoint. Based on a previous study of unilateral and bilateral (SBS technique) stenting for MHO [5], the stent dysfunction rate was expectedly 36% higher (59% vs. 23%) in the unilateral stent group compared with that in the bilateral group. At total of 66 patients (33 patients in each group) were required to discern a difference of 36% in the stent dysfunction rate with a power of 0.8 and an alpha of 0.05 after considering of a dropout rate of 10%.
In this study, intention-to-treat (ITT) and per-protocol (PP) analyses were applied. ITT analysis was performed on the basis of the total number of patients who enrolled in the study. PP was analyzed on the basis of the number of patients with technically successful stenting. The ITT analysis was applied to evaluate the technical success; the PP analysis was used to evaluate patency, clinical success, survival, stent dysfunction, adverse events, and predictors of stent dysfunction and survival. Finally, both ITT and PP analyses were used to evaluate the baseline data.
Continuous data were analyzed by Mann–Whitney or t test and were expressed as mean ± SD (standard deviation). Analysis of categorical data was carried out by Fisher exact test or χ2 test. The calculation of patency and survival was done using Kaplan–Meier analysis and the curves were compared through the log-rank test. The stent dysfunction and survival predictions were done using the Cox regression analysis. For the subsequent multivariate analyses variables with P < 0.10 in univariate analyses were chosen. Statistically, a P value < 0.05 was considered significant. The SPSS 16.0 (SPSSInc., Chicago, IL, USA) was used to carry out all statistical analysis.
Results
ITT analysis
Baseline data
Of the 72 enrolled patients, 36 patients each were assigned to the unilateral and the bilateral groups (Table 1). There was no remarkable difference between the two groups with respect to baseline data (gender-wise distribution ratio, age, causes of MHO, stage of the tumor, liver function test, Bismuth type, and the number of patients who underwent anticancer treatment). No patient was lost in follow-up.
Technical success
The technical successful rates of unilateral and bilateral stenting were 83.3% (30/36) and 83.3% (30/36), respectively (P = 1.000). The length and diameter of the stents were 50–70 and 8 mm, respectively. All stents in the unilateral group were inserted through the right intrahepatic biliary duct. However, in 12 patients, the guide wire could not pass through the obstructed site; thus, they failed to undergo insertion of the stent in the first attempt. These 12 patients were placed with an extra-biliary drainage catheter and were managed by a second attempt of stent insertion 5 days after being placed in the catheter. Nevertheless, none of them could successfully undergo insertion of the stent. Among these 12 patients, 10 were treated by extra-biliary drainage and 2 patients underwent palliative resection treatment.
PP analysis
Clinical success
The clinical successful rates of unilateral and bilateral stenting were 90.0% (27/30) and 96.7% (29/30), respectively (P = 0.605, Table 2). In the unilateral stenting group, an improvement before and after treatment in the total bilirubin (TBIL; 205.7 ± 122.5 to 102.0 ± 53.0 μmol/L (P < 0.001), aspartate transaminase (AST; 132.6 ± 73.6 U/L to 67.1 ± 50.0 U/L (P < 0.001), and alanine aminotransferase (ALT; 130.9 ± 84.7 U/L to 60.5 ± 30.0 U/L (P < 0.001)were observed. In the bilateral stenting group, the TBIL, AST, and ALT improved from 216.7 ± 86.3 μmol/L, 123.1 ± 75.3 U/L, and 125.6 ± 99.2 U/L before treatment to 112.4 ± 73.5 μmol/L (P < 0.001), 61.0 ± 41.7 U/L (P < 0.001), and 56.8 ± 36.0 U/L (P < 0.001), respectively after treatment.
Stent dysfunction and patency
To unilateral and bilateral groups, stent dysfunction was found in 5 and 3 patients respectively (16.7% vs. 10.0%, P = 0.704, Table 2). Among these 8 patients, five patients experienced tumor ingrowth and 2 patients experienced sludge. The tumor ingrowth was treated by percutaneous intraductal radiofrequency ablation (n = 1), insertion of another stent (n = 2), and percutaneous transhepatic biliary drainage (n = 2). The percutaneous transhepatic drainage of the bile was carried out to treat the sludge. The remaining one patient did not receive any further percutaneous intraductal intervention, and therefore, the reason for stent malfunction was not clear in this case. Further, no risk factor influencing the stent dysfunction was observed on Cox regression analysis.
The median cumulative stent patency duration was 118 days in unilateral group and 125 days in bilateral group (P = 0.571, Fig. 3a).
Survival
Through the follow-up period after stenting, 28 patients in unilateral group and 29 patients in the bilateral group died and the median cumulative survival in the unilateral and bilateral groups were 122 and 125 days, respectively (P = 0.844, Fig. 3b). The univariate and multivariate Cox regression analyses revealed a increased post-operative TBIL level (HR 1.009, 95% CI 1.004–1.015, P = 0.001), increased pre-operative ALT level (HR 1.006, 95% CI 1.002–1.010, P = 0.001), and no post-operative anticancer treatment (HR 0.377, 95% CI 0.204–0.700, P = 0.002), which are the worse survival predictors (Table 3).
Adverse events
In unilateral stenting group, the adverse events included cholangitis (n = 2) and self-limited bleeding (n = 1). In bilateral stenting group, the adverse events included cholangitis (n = 1), cholecystitis (n = 1), and hepatic pseudoaneurysm (n = 1).
The cholangitis were successfully treated by percutaneous transhepatic biliary drainage in 2 patients. One patient with cholangitis did not undergo further treatment. The cholecystitis was successfully treated by medical treatment. The durative bleeding led to the speculation of pseudoaneurysm, which was further confirmed by hepatic angiogram and was treated successfully by coil embolization.
Discussion
Metal stenting has been the best option for the palliative treatment of patients with inoperable MHO [12,13,14,15]. Although bilateral biliary drainage has become generally accepted in many studies, most studies are retrospective studies [5,6,7, 16, 17]. Therefore, the superiority of bilateral stenting over unilateral stenting cannot be definitely established. Most previous studies describe the results of endoscopic unilateral and bilateral stenting for MHO [4,5,6,7]. This prospective, randomized controlled trial compared the outcomes between percutaneous unilateral and bilateral stenting for MHO.
The unilateral and bilateral stenting procedures have been shown to be clinically and technically successful. However, in most of the studies, no remarkable difference was observed in the technical and successful rates between the unilateral and bilateral stenting procedures [2,3,4,5,6,7]. Accordingly, we did not observe any significant variation in successful (90.0% vs. 96.7%, P = 0.605) and technical (83.3% vs. 83.3%, P = 1.000) rates between the 2 groups in this study. As it is already known that to attain relief from jaundice, the drainage of only 25%–30% of the liver requires to be attained [18]. Thus, in these cases, unilateral stenting is enough because the volume of both right and left lobes is greater than 30% of the liver [19].
The stent dysfunction rate and patency were the main controversies in the previous comparative studies of unilateral and bilateral stenting [2,3,4,5,6,7]. Recently, Lee et al. [6] reported a lower reintervention rate (42.6% vs. 60.3%, P = 0.049) and a longer patency duration in bilateral group (252 days vs. 139 days, P < 0.01). Although these results were obtained from the randomized controlled trial, the study did not unify the method of bilateral stenting (both SBS and SIS were used) [6]. Unlike that report, the duration of patency (368 days vs. 387 days, P = 0.685) and the rate of stent dysfunction (16.1% vs. 11.1%, P = 0.58) were alike between unilateral and bilateral groups, as reported by Chang et al. [2], in a retrospective study using only SBS mode of bilateral stenting. Thus, to identify an optimum treatment modality and to confirm the above-mentioned outcomes, a randomized controlled trial for MHO applying unique bilateral and unilateral stenting is needed.
Likewise, a similar patency duration (118 days vs. 125 days, P = 0.571) and stent dysfunction rates (16.7% vs. 10.0%, P = 0.704) between unilateral and bilateral groups were observed in our study, which used bilateral stenting only through the SBS mode. This may insinuate that a similar long-term biliary drainage effect may be acquired through unilateral stenting, like the bilateral stenting. Our results are also in accordance with those in the previous studies which compared unilateral and bilateral percutaneous stenting for MHO [2, 3]. There were no predictors to influence stent dysfunction, as evaluated by Cox regression analysis. The cause of these observations may be because of the facts that the sample size was limited and the patency of stent in a majority of the patients until death.
When the survival of patients between unilateral and bilateral stenting was evaluated, no remarkable variation was observed [2,3,4,5, 7]. While no notable variation in the probability of survival between the two groups (P = 0.053) was reported by Lee et al. [6], they did report a positive association (95% CI 0.259–0.666; P < 0.01) between bilateral drainage and survival. In the case of bilateral stenting, better survival rates have been seen on draining > 50% of the liver volume and is thus highly recommended by The Asia–Pacific Working Group on Hepatobiliary Cancer [20]. In our study, on comparing the unilateral and bilateral groups, a similar duration of survival (122 days vs. 125 days, P = 0.844) was observed. This result may be because unilateral stenting was carried out via the right intrahepatic biliary route. Nearly 55–60% of the whole liver comprises the right hepatic lobe and this is in accordance with the drainage volume recommended by the Asia-Pacific Working Group [2, 20]. Higher TBIL and ALT levels usually indicate that patients exhibit an unsatisfactory liver function, which is associated with reduced chances of survival [2]. After the operation, no post-operative anticancer treatment is also the predictors of worse survival. Besides the palliative stenting to alleviate jaundice, survival of the patients can be enhanced by the subsequent modes of cancer treatment, including chemotherapy, radiotherapy, a high-intensity focused ultrasound ablation, etc. [2, 6, 10].
There was no notable dissimilarity between the two groups regarding the occurrence rate of cholangitis, and only 3 patients (3/60, 5%) experienced cholangitis after stenting. This result was achieved mainly because a temporary biliary drainage was carried out in all patients for 5 days. The rate of early stent dysfunction can also be decreased by halting cholangitis, which may potentially cause a similar duration of patency between unilateral and bilateral stenting. However, a rare complication called hepatic pseudoaneurysm may occur when durative bleeding happens post-biliary stenting and can be managed by coil embolization.
A few limitations include hindrance in definitive conclusions concerning the clinical effectiveness due to the limited sample size from a single center. In addition, a potential bias may occur because of the open-label design. Second, the inability to exclude a bias of unbalanced stage distribution because randomization was not performed with stratification by tumor stage. Third, a selection bias may be caused because of the multiple cancer types. Thus, clinical trials are needed which include unique disease. Fourth, since the anticancer treatment was carried out depending on the specific condition of the patient, a selection bias may be caused.
In conclusion, there are no significant differences between unilateral and bilateral metal stenting for MHO in terms of technical and clinical success, duration of stent patency and survival, and adverse events. Moreover, the patient’s survival chances could be enhanced by subsequent anticancer treatment. Therefore, being a simple procedure, unilateral metal stenting with anticancer treatment may be recommended in patients with MHO.
References
Jang SI, Lee DK (2015) Update on pancreatobiliary stents: stent placement in advanced hilar tumors. Clin Endosc 48:201–208
Chang G, Xia FF, Li HF, et al (2017) Unilateral versus bilateral stent insertion for malignant hilar biliary obstruction. Abdom Radiol (NY) 42:2745-2751
Gwon DI, Ko GY, Sung KB, et al (2011) Percutaneous biliary metallic stent placement in patients with unilobar portal vein occlusion caused by advanced hilar malignancy: outcome of unilateral versus bilateral stenting. AJR Am J Roentgenol 197:795-801
Iwano H, Ryozawa S, Ishigaki N, et al (2011) Unilateral versus bilateral drainage using self-expandable metallic stent for unresectable hilar biliary obstruction. Dig Endosc 23:43–48
Naitoh I, Ohara H, Nakazawa T, et al (2009) Unilateral versus bilateral endoscopic metal stenting for malignant hilar biliary obstruction. J Gastroenterol Hepatol 24:552–557
Lee TH, Kim TH, Moon JH, et al (2017) Bilateral versus unilateral placement of metal stents for inoperable high-grade malignant hilar biliary strictures: a multicenter, prospective, randomized study (with video). Gastrointest Endosc 86:817-827
Liberato MJ, Canena JM (2012) Endoscopic stenting for hilar cholangiocarcinoma: efficacy of unilateral and bilateral placement of plastic and metal stents in a retrospective review of 480 patients. BMC Gastroenterol 12:103
Perdue DG, Freeman ML, DiSario JA, et al (2008) Plastic versus self-expanding metallic stents for malignant hilar biliary obstruction: a prospective multicenter observational cohort study. J Clin Gastroenterol 42:1040-1046
Sawas T, Al Halabi S, Parsi MA, et al (2015) Self-expandable metal stents versus plastic stents for malignant biliary obstruction: a meta-analysis. Gastrointest Endosc 82:256-267
Niu S, Cheng L, Qiao Y, et al (2016) Combined stent insertion and high-intensity focused ultrasound ablation for patients with malignant obstructive jaundice. Surg Laparosc Endosc Percutan Tech 26:488–492
Son RC, Gwon DI, Ko HK, et al (2015) Percutaneous unilateral biliary metallic stent placement in patients with malignant obstruction of the biliary hila and contralateral portal vein steno-occlusion. Korean J Radiol 16:586–592
Li M, Bai M, Qi X, et al (2015) Percutaneous transhepatic biliary metal stent for malignant hilar obstruction: results and predictive factors for efficacy in 159 patients from a single center. Cardiovasc Intervent Radiol 38:709–721
Li M, Li K, Qi X, et al (2016) Percutaneous transhepatic biliary stent implantation for obstructive jaundice of perihilar cholangiocarcinoma: a prospective study on predictors of stent patency and survival in 92 patients. J Vasc Interv Radiol 27:1047–1055
Yun JH, Jung GS, Park JG, et al (2016) Malignant hilar biliary obstruction: treatment by means of placement of a newly designed Y-shaped branched covered stent. Cardiovasc Intervent Radiol 39:582–590
Jiao D, Huang K, Zhu M, et al (2017) Placement of a newly designed Y-configured bilateral self expanding metallic stent for hilar biliary obstruction: a pilot study. Dig Dis Sci 62:253–263
Naitoh I, Hayashi K, Nakazawa T, et al (2012) Side-by-side versus stent-in-stent deployment in bilateral endoscopic metal stenting for malignant hilar biliary obstruction. Dig Dis Sci 57:3279–3285
Law R, Baron TH (2013) Bilateral metal stents for hilar biliary obstruction using a 6Fr delivery system: outcomes following bilateral and side-by-side stent deployment. Dig Dis Sci 58:2667–2672
Yasuda I, Mukai T, Moriwaki H, et al (2013) Unilateral versus bilateral endoscopic biliary stenting for malignant hilar biliary strictures. Dig Endosc 25:81–85
Larghi A, Tringali A, Lecca PG, et al (2008) Management of hilar biliary strictures. Am. J Gastroenterol 103:458–473
Rerknimitr R, Angsuwatcharakon P, Ratanachu-ek T, et al (2013) Asia-Pacific consensus recommendations for endoscopic and interventional management of hilar cholangiocarcinoma. J Gastroenterol Hepatol 28:593–607
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed consent
Written informed consent was obtained from all patients.
Research involving animal rights
This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fu, YF., Zhou, WJ., Shi, YB. et al. Percutaneous stenting for malignant hilar biliary obstruction: a randomized controlled trial of unilateral versus bilateral stenting. Abdom Radiol 44, 2900–2908 (2019). https://doi.org/10.1007/s00261-019-02010-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-02010-6