Abstract
Purpose
To determine the clinical efficiency and long-term outcomes between unilateral and bilateral stent insertion in patients with malignant hilar biliary obstruction.
Methods
From August 2012 to February 2016, 63 consecutive patients with malignant hilar biliary obstruction were treated with unilateral or bilateral stent insertion at our center. The bilateral stents were inserted using the side-by-side technique. The clinical efficiency and long-term outcomes were compared between the two groups.
Results
Unilateral and bilateral stent insertions were successfully performed in 31 of 33 and 27 of 30 patients, respectively (P = 0.912). No procedure-related complication occurred. Clinical success was achieved in 29 of 31 patients in the unilateral stent group and in 26 of 27 patients in the bilateral stent group (P = 0.637). During the follow-up, re-obstruction of stent occurred in five patients in the unilateral stent group and in three patients in the bilateral stent group (P = 0.58). The significant differences were not observed in the stent patency time (368 vs. 387 days, P = 0.685) and survival (200 vs. 198 days, P = 0.751) between two groups. Based on the univariate and multivariate analyses, the independent risk factors for decreasing the survival time included higher Eastern Cooperative Oncology Group performance status (P = 0.018), higher alanine aminotransferase level (P = 0.009), and absence of anticancer treatment after stent insertion (P = 0.002).
Conclusion
Compared to bilateral stent insertion for malignant hilar biliary obstruction, unilateral stent insertion can provide comparable clinical efficiency and long-term outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Malignant hilar biliary obstruction can be caused by cholangiocarcinoma, gallbladder carcinoma, hepatocellular carcinoma, or metastases lymph nodule [1,2,3]. A majority of the patients with malignant hilar biliary obstruction are inoperable because of the advanced tumor stage [1,2,3]. Palliative biliary drainage is commonly the first-line treatment option in patients with malignant hilar biliary obstruction [1,2,3].
The frequently used biliary drainage methods include catheter drainage and biliary stent insertion [1,2,3,4,5]. Catheter drainage is not convenient for patients' daily life [4, 5]. Therefore, stent insertion is considered as optimal in patients with malignant hilar biliary obstruction [1,2,3,4,5]. Several studies suggested that bilateral stent insertion should be performed in patients with malignant hilar biliary obstruction so that the bilateral biliary tracts can be drained effectively [4,5,6,7]. Other researchers considered that unilateral stent insertion could afford clinical efficiency in patients with malignant hilar biliary obstruction, as the drainage of 25% of the liver area can bring about the recovery of the liver biochemical indicators [8,9,10]. However, the comparative study of unilateral and bilateral stent insertion for malignant hilar biliary obstruction is yet lacking.
In this study, we aimed to determine the clinical efficiency and long-term outcomes between unilateral and bilateral stent insertion for malignant hilar biliary obstruction.
Methods
The present single-center, retrospective study was approved by our Institutional Review Board. Informed consent for the procedure and clinical data management was obtained.
Study design
From August 2012 to February 2016, 63 consecutive patients with malignant hilar biliary obstruction were treated with unilateral or bilateral stent insertion at our center. Before the procedure, patients or their family members received detailed information about unilateral and bilateral stent insertion. The decision of the type of stent insertion to be used was made by the patients or their family members after considering the economic situation and the advantages/disadvantages of both the stent insertion. The inclusion criteria were as follows: (a) patients with definite diagnosis of malignant hilar biliary obstruction and (b) patients with inoperable malignant hilar biliary obstruction. The exclusion criteria were as follows: patients with Bismuth type I obstruction; (b) patients who previously underwent biliary stent insertion; (c) patients who previously underwent hepatolobectomy.
Diagnosis
The diagnosis of hilar biliary obstruction was established by the abdominal computed tomography (CT) and magnetic resonance cholangiopancreatography (MRCP) findings from the patient. The diagnosis of malignancy was established by percutaneous transhepatic forceps biopsy, previous surgical findings, or clinical findings (patients’ history, imaging findings, and neoplastic markers). The tumor stage was evaluated according to the criteria of the American Joint Committee on Cancer/International Union Against Cancer (AJCC/UICC).
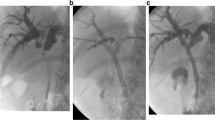
Unilateral stent insertion
All patients were placed in the supine position. Puncture of the right intrahepatic biliary tract was considered initially because the right hepatic lobe encompasses 55–60% of the whole life [10]. The intrahepatic biliary tract was punctured under the ultrasound guidance. 5 mL of 2% lidocaine was administrated at the puncture point, a 21-G Chiba needle (Cook, Bloomington, IN, USA) was punctured into the intrahepatic biliary tract. Then, under the fluoroscopic guidance, cholangiography was performed to visualize the location and extent of biliary obstruction. Subsequently, a 6F sheath (Cook) was placed into the intrahepatic biliary tract. A 5F VER (Cordis, Hialeah, FL, USA) and a 0.035-inch guidewire (Terumo, Tokyo, Japan) were introduced through the obstructed lesion into the duodenum. Then the guidewire was exchanged by a 0.035-inch stiff guidewire (Cook). Finally, the uncovered self-expanding nitinol stent (Micro-Tech, Nanjing, China) was inserted (Fig. 1). The stent extended at least 1 cm beyond either end of the occluded section.
A 61-year-old man with malignant hilar biliary obstruction underwent unilateral stent insertion. A Right cholangiography demonstrated the location and extent of biliary obstruction (arrow). B The stent (arrows) was inserted at the right intrahepatic biliary tract and common biliary tract. C Cholangiography demonstrated patency of the stent
Bilateral stent insertion
Bilateral stent insertion was performed using side-by-side (SBS) technique. Right and left intrahepatic biliary tracts were punctured individually. Subsequently, two 0.035-inch stiff guidewires were placed into the duodenum, followed by the insertion of two stents to form a Y-configuration (Fig. 2).
Postoperative management
After stent insertion (unilateral and bilateral), an 8.5F drainage catheter (Cook) was placed across the hilar obstruction to the duodenum for temporary biliary drainage for 3 days. All patients were treated with appropriate antibiotics and hemostasis for 3 days.
Definition and endpoints
Technical success of biliary stent insertion was defined as the passage of stent across the obstruction, along with the flow of contrast medium through the stent. Clinical success was defined as at least a 30% decrease in the pre-procedure total bilirubin (TBIL) level within 2 weeks after stent placement [11]. The stent patency time was defined as the period between stent insertion and stent dysfunction (occlusion or migration) or patient death. Stent dysfunction was suspected when the patients experienced the recurrence of jaundice. The survival was calculated from the day of stent insertion. While estimating the stent patency time, patients who died without stent dysfunction and living patients without stent dysfunction were classified as censored data. In previous studies, the patients’ survival was shorter than the cumulative stent patency owing to the loss of censored data [11,12,13].
The primary endpoint was stent dysfunction. The secondary endpoints included stent-related complication and death.
Follow-up
Patients were followed until death or the end of the study period (December 2016). The follow-up data were obtained from medical records at specific intervals (1, 2, 3, 6, and then every 6 months) or from telephonic interviews with the patients or their families. The routine follow-up protocol included clinical examination and abdominal CT. If patients experienced recurrence of jaundice, they were encouraged to visit the hospital at any time.
Statistical analysis
Statistical analysis was performed using SPSS 16.0 (SPSS Inc., Chicago, IL, USA). Data regarding the clinical efficiency and long-term outcomes were compared between the two groups. Continuous variables were analyzed by t test and represented as the mean or median. Numerical data were analyzed using the χ 2 test or Fisher’s exact test. Patency and survival time were calculated by Kaplan–Meier curves and log-rank test. The predictors of the patency and survival were determined using univariate and multivariate Cox regression analysis. The covariates incorporated into the multivariate analysis included the variables with P < 0.1 in univariate analyses. A P value <0.05 was considered statistically significant.
Results
Patients
Unilateral and bilateral stent insertion were successfully performed in 31 of 33 and 27 of 30 patients, respectively (93.9 vs. 90%, P = 0.912). The baseline data of these 58 patients with technical success was demonstrated in Table 1. The size of these stents was 8 mm in diameter and 50–70 mm in length. Five patients failed to undergo stent insertion, even after two attempts, as the guidewire could not pass through the obstructed site. These patients were treated with external biliary drainage. No procedure-related complication occurred.
Clinical success
Clinical success was achieved in 29 of 31 patients in the unilateral stent group and 26 of 27 patients in the bilateral stent group (93.5 vs. 96.3%, P = 0.637). Three patients (unilateral stent group: 2; bilateral stent group: 1) experienced clinical failure of stent insertion. In these three patients, although the postoperative TBIL level decreased, the decreasing amplitude did not achieve the standard of clinical success. The improvement of TBIL was shown in Table 2.
Outcome
Five patients who experienced technical failure of stent insertion were not followed up. During the follow-up, 11 patients (unilateral stent group: 4; bilateral stent group: 7) experienced stent-related complications. Among these 11 patients, six patients experienced cholangitis, four patients experienced cholecystitis, and the remaining one patient experienced liver abscess (Table 3). The cholangitis was treated by conservative treatment (n = 4) or percutaneous biliary drainage (n = 2), the cholecystitis was treated by conservative treatment, and the liver abscess was treated by percutaneous transhepatic drainage.
Twenty-three patients underwent subsequent anticancer treatment (unilateral stent group: 12; bilateral stent group: 11) after stent insertion. In the unilateral stent group, eight patients underwent high-intensity focused ultrasound ablation, and four patients underwent chemotherapy. In the bilateral stent group, five patients underwent chemotherapy, three patients underwent chemoradiotherapy, and three patients underwent high-intensity focused ultrasound ablation. Re-obstruction of stent occurred in five and three patients in the unilateral and bilateral stent groups (16.1 vs. 11.1%, P = 0.58). The reasons of re-obstruction included tumor ingrowth (n = 6) and sludge (n = 2). Among these eight patients, six patients were treated by percutaneous biliary drainage, one patient was treated by secondary stent insertion, and the remaining one patient was treated by intraductal radiofrequency ablation. The median stent patency time was 368 and 387 days in the unilateral and bilateral stent groups, respectively (P = 0.685, Fig. 3). At univariate analysis, no risk factor was found with influencing the stent patency time.
Fifty-seven patients (unilateral stent group: 31; bilateral stent group: 26) died during the follow-up. The cause of death was tumor progression in all these 57 patients. The median survival time was 200 and 198 days in the unilateral and bilateral stent groups, respectively (P = 0.751 Fig. 4). At univariate analysis, the risk factors of decreasing the survival time included higher tumor stage, higher Eastern Cooperative Oncology Group (ECOG) performance status (PS), higher alanine aminotransferase (ALT) level, and absence of anticancer treatment after stent insertion. At multivariate analysis, the independent risk factors of decreasing the survival time included higher ECOG PS (P = 0.018), higher ALT level (P = 0.009), and absence of anticancer treatment after stent insertion (P = 0.002, Table 4).
Discussion
The present study compared the clinical efficiency and long-term outcomes between unilateral and bilateral stent insertions for malignant hilar biliary obstruction. The results demonstrated no significant differences in the clinical efficiency and long-term outcome between unilateral and bilateral stent groups.
Hilar cholangiocarcinoma is the most common type of biliary duct cancer, accounting for 46–97% of all the biliary duct cancers, while surgical resection can be performed in only 20–30% of the patients [2]. Palliative biliary stent insertion has been widely used as the first-line treatment for patients with malignant hilar biliary obstruction [4,5,6,7,8,9]. The purpose of biliary stent insertion is to relieve the symptoms of jaundice and improve the liver function [4,5,6,7,8,9]. Furthermore, stent insertion has little or no influence on the decision of the oncologist to continue with scheduled therapies including chemotherapy and radiation therapy [14].
The Asia-Pacific Working Group on Hepatobiliary Cancer recommends draining >50% of the liver volume, and bilateral biliary drainage has been found to have better outcomes in recent studies [15, 16]. The bilateral stent insertion techniques mainly include SBS and stent-in-stent (SIS) techniques [17,18,19,20]. Naitoh et al. [18] compared the outcomes between unilateral and bilateral stent insertion for malignant hilar biliary obstruction. The bilateral stent insertion was performed using SBS technique. The results demonstrated no significant differences between the two groups with respect to technical success, clinical success, and complications; however, the stent patency time was significantly longer in the bilateral than the unilateral stent insertion group (488 vs. 210 days, P = 0.009). Iwano et al. [17] also compared the outcomes between unilateral and bilateral stent insertion (SIS technique) for malignant hilar biliary obstruction and found no significant difference in the stent patency time between two groups (125 vs. 133 days, P = 0.322). In addition, Naitoh et al. and Iwano et al. both did not reveal any significant difference in the survival time between two groups. Naitoh et al. [19] compared the outcomes between SBS and SIS techniques in bilateral stent insertion for malignant hilar biliary obstruction. The results showed that stent patency time was significantly longer in the SBS group than in the SIS group (469 vs. 181 days, P = 0.047).
The long-term stent patency time was usually longer in patients with SBS bilateral stent insertion [18, 19]. SBS bilateral stent insertion has two drainage passages, if one passage is obstructed, another passage can keep on draining [19]. In this study, the median stent patency time in the bilateral stent (SBS technique) group is 387 days, which is longer than that (125 and 181 days) after bilateral stent insertion (SIS technique) in previous studies [17, 19]. However, no significant difference was noted in the stent patency time between unilateral and bilateral stent groups (368 vs. 387 days, P = 0.696) in this study. The univariate analysis did not reveal any risk factor influencing the stent patency time. These results were different from that of Naitoh et al. [18]. These results may be attributed to the following factors: (a) limited sample size; (b) most patients had a short life expectancy and the stent remained patent until death. In addition, the subsequent anticancer treatment was not mentioned in Naitoh’s study [18]. In the present study, anticancer treatment was performed in a subset of patients in both groups (12/31 vs. 11/27, P = 0.875). Owing to the anticancer treatment, the stent patency time might be improved in both groups. Therefore, no significant difference in the stent patency time between both groups can be explained.
The survival time was not significantly different between unilateral and bilateral stent insertion groups (203 vs. 198 days, P = 0.813) in this present study. This result is comparable to the previous studies of unilateral versus bilateral stent insertion for malignant hilar biliary obstruction [17, 18]. However, no risk factor associated with survival time was made in previous studies about bilateral stent insertion for malignant hilar biliary obstruction [17,18,19,20]. In this present study, we made the risk factor associated with survival time after stent insertion. According to the univariate and multivariate analyses, the independent risk factors of decreasing the survival time included higher ECOG PS, higher ALT level, and absent of anticancer treatment after stent insertion. Stent insertion can relieve the symptoms of jaundice; however, it cannot effectuate the treatment of primary cancer. Several studies have proven that subsequent anticancer treatment can increase patients’ survival time [4, 11, 14]. Higher ECOG PS and ALT level usually indicate that patients exhibit a bad general condition and liver function, and thus, it is reasonable that higher ECOG PS and ALT level are associated with the shorter survival time.
The complication rates were also not significant different between unilateral and bilateral stent insertion groups (12.9 vs. 25.9%, P = 0.207) in this present study. This result is similar to the previous study of unilateral versus bilateral stent insertion for malignant hilar biliary obstruction [18].
In this study, no significant difference was observed in the clinical efficiency between unilateral and bilateral stent insertion groups. However, the advantages of unilateral stent insertion include low cost and simple procedure, which are crucial in medical processes. Owing to similar efficiency between unilateral and bilateral stent insertion, unilateral stent insertion can be recommended, and the saving money can be used in subsequent anticancer treatment.
This study has some limitations. First, this is a retrospective review, and therefore the selection bias inherently associated with such studies does exist. Further randomized controlled trial should be performed. Second, the sample size is rather small. Due to this reason, we do not obtain a risk factor which is associated with the patency time. Third, these patients only came from a single center.
In conclusion, although further clinical trials are needed, our study does not demonstrate any differences in clinical efficiency and long-term outcomes between unilateral and bilateral stent insertion for patients with malignant hilar biliary obstruction. Thus, unilateral stent insertion is recommended because of easier procedure and lower cost.
References
Singhal D, van Gulik TM, Gouma DJ (2005) Palliative management of hilar cholangio carcinoma. Surg Oncol 14:59–74
Jang SI, Lee DK (2015) Update on pancreatobiliary stents: stent placement in advanced hilar tumors. Clin Endosc 48:201–208
Di Mitri R, Mocciaro F (2014) Y-shaped bilateral self-expandable metallic stent placement for malignant hilar biliary obstruction: data from a referral center for palliative care. Sci World J 2014:151502
Li M, Bai M, Qi X, et al. (2015) Percutaneous transhepatic biliary metal stent for malignant hilar obstruction: results and predictive factors for efficacy in 159 patients from a single center. Cardiovasc Intervent Radiol 38:709–721
Li M, Li K, Qi X, et al. (2016) Percutaneous transhepatic biliary stent implantation for obstructive jaundice of perihilar cholangiocarcinoma: a prospective study on predictors of stent patency and survival in 92 patients. J Vasc Interv Radiol 27:1047–1055
Yun JH, Jung GS, Park JG, et al. (2016) Malignant hilar biliary obstruction: treatment by means of placement of a newly designed Y-shaped branched covered stent. Cardiovasc Intervent Radiol 39:582–590
Jiao D, Huang K, Zhu M, et al. (2017) Placement of a newly designed Y-configured bilateral self expanding metallic stent for hilar biliary obstruction: a pilot study. Dig Dis Sci 62:253–263
Son RC, Gwon DI, Ko HK, et al. (2015) Percutaneous unilateral biliary metallic stent placement in patients with malignant obstruction of the biliary hila and contralateral portal vein steno-occlusion. Korean J Radiol 16:586–592
Yi R, Gwon DI, Ko GY, et al. (2012) Percutaneous unilateral placement of biliary covered metallic stent in patients with malignant hilar biliary obstruction and contralateral portal vein occlusion. Acta Radiol 53:742–749
Yasuda I, Mukai T, Moriwaki H, et al. (2013) Unilateral versus bilateral endoscopic biliary stenting for malignant hilar biliary strictures. Dig Endosc 25:81–85
Niu S, Cheng L, Qiao Y, et al. (2016) Combined stent insertion and high-intensity focused ultrasound ablation for patients with malignant obstructive jaundice. Surg Laparosc Endosc Percutan Tech 26:488–492
Kitano M, Yamashita Y, Tanaka K, et al. (2013) Covered self-expandable metal stents with an anti-migration system improve patency duration without increased complications compared with uncovered stents for distal biliary obstruction caused by pancreatic carcinoma: a randomized multicenter trial. Am J Gastroenterol 108:1713–1722
Telford JJ, Carr-Locke DL, Baron TH, et al. (2010) A randomized trial comparing uncovered and partially covered self-expandable metal stents in the palliation of distal malignant biliary obstruction. Gastrointest Endosc 72:907–914
Li TF, Chen C, Han XW, et al. (2014) Clinical efficacy of metallic biliary stents combined with different anti-cancer treatments in the management of bile duct cancer. Hepatogastroenterology 61:22–26
Rerknimitr R, Angsuwatcharakon P, Ratanachu-ek T, et al. (2013) Asia-Pacific consensus recommendations for endoscopic and interventional management of hilar cholangiocarcinoma. J Gastroenterol Hepatol 28:593–607
Sawas T, Al Halabi S, Parsi MA, et al. (2015) Self-expandable metal stents versus plastic stents for malignant biliary obstruction: a meta-analysis. Gastrointest Endosc 82:e257
Iwano H, Ryozawa S, Ishigaki N, et al. (2011) Unilateral versus bilateral drainage using self-expandable metallic stent for unresectable hilar biliary obstruction. Dig Endosc 23:43–48
Naitoh I, Ohara H, Nakazawa T, et al. (2009) Unilateral versus bilateral endoscopic metal stenting for malignant hilar biliary obstruction. J Gastroenterol Hepatol 24:552–557
Naitoh I, Hayashi K, Nakazawa T, et al. (2012) Side-by-side versus stent-in-stent deployment in bilateral endoscopic metal stenting for malignant hilar biliary obstruction. Dig Dis Sci 57:3279–3285
Law R, Baron TH (2013) Bilateral metal stents for hilar biliary obstruction using a 6Fr delivery system: outcomes following bilateral and side-by-side stent deployment. Dig Dis Sci 58:2667–2672
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Chang, G., Xia, FF., Li, HF. et al. Unilateral versus bilateral stent insertion for malignant hilar biliary obstruction. Abdom Radiol 42, 2745–2751 (2017). https://doi.org/10.1007/s00261-017-1174-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1174-8