Abstract
Purpose of review
To review the current status and ideal time interval of the combination therapy of transarterial chemoembolization (TACE) and local ablation for patients with HCCs.
Recent findings
In recent years, local ablation has been proposed as an alternative curative treatment in the management of HCC. Additionally, many treatment options are available including TACE molecular targeted agents and immune checkpoint inhibitors. Similar overall survival rates and prognoses have been obtained with radiofrequency ablation (RFA) microwave ablation (MWA) and cryoablation for patients with HCCs up to 3 cm in diameter. Yet, MWA has shown superiority in treating large HCCs while cryoablation has several advantages compared with RFA or MWA. Furthermore, the treatment strategy of TACE combined with local ablation is widely accepted by many physicians in order to further increase the survival rate and improve the prognosis of patients with HCCs. However, the time interval between the two sessions of combination therapy remains uncertain in the current guidelines.
Summary
Combination therapy of TACE and local ablation has advantages on survival and prognosis in patients with HCC compared with monotherapy. Good patient selection for the right modality needs to be carried out to guarantee the most efficacious treatment for HCC patients. Further studies are needed to find the ideal time interval between TACE and local ablation for HCC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary liver cancer (PLC) is one of the most common malignant tumors and is a leading cause of cancer-related death worldwide [1]. Approximately half of new liver cancer cases and deaths occurred in China [2]. Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer worldwide, which is mainly due to liver cirrhosis resulting from hepatitis infection or alcoholic cirrhosis [3, 4].
Liver transplantation and surgical resection are generally considered to be curative for Barcelona Clinic Liver Cancer (BCLC) stage 0/A HCC. Recently, local ablation, including radiofrequency ablation (RFA), microwave ablation (MWA), and cryoablation, was introduced as an alternative curative treatment for early-stage HCCs [1, 5]. However, this malignant tumor is still associated with dismal survival rates due to its late diagnosis. While the majority of HCCs are non-operable when diagnosed, transarterial chemoembolization (TACE) plays an important role in the management of unresectable HCC.
By delivering chemotherapeutic agents to the tumor site and occluding the tumor-feeding artery with embolic materials, TACE usually results in tumor cell ischemia, hypoxia and even apoptosis. This is because the blood supply of HCC mostly comes from the hepatic artery, while the normal hepatic parenchyma is supplied by both the portal vein and hepatic artery [6]. Therefore, this intravascular treatment is now recommended as the first-line treatment for BCLC stage B HCC according to the BCLC guidelines.
Nevertheless, for patients with HCC undergoing TACE alone, the tumor necrosis rate is low, while the intrahepatic recurrence rate is high. Residual tumors can still be observed in many cases. One possible reason is that it is hard to embolize all the feeding arteries of the tumor. Moreover, recanalization and angiogenesis may occur after TACE, which could promote tumor recurrence and metastasis, and collateral circulation may be established [7].
In past years, many investigators have tried to manage HCC by combining TACE with local ablative treatment as a sequential therapeutic session and achieved better local tumor control and OS. The purpose of this review is to summarize recent clinical findings and provide an overview of the combined therapy of TACE and percutaneous ablation.
Radiofrequency ablation
According to the guidelines, RFA is recommended as a curative treatment for small liver cancer. Tumor tissues undergo coagulation necrosis after RFA, which generates an alternating electric field that leads to ionic agitation. The temperature of ablative region can reach up to 100 °C [8, 9]. In a recent randomized clinical trial (RCT) including 218 patients with early-stage HCC, similar tumor recurrence (71.3% vs 81.7%), disease-free survival (DFS; p = 0.072) and OS (p = 0.531) were observed between surgical resection and RFA [10]. However, RFA is more likely to be incomplete in the management of HCC larger than 3 cm in diameter or localized near major vessels due to the so-called heat-sink effect [11].
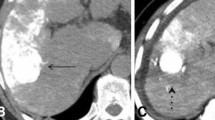
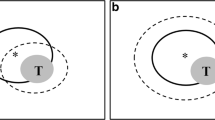
To overcome this limitation and achieve better outcomes, investigators are increasingly applying the combined therapy of TACE and RFA to treat HCC patients, since TACE and RFA have a synergistic effect. On one hand, RFA before TACE can induce a peripheral hyperemic rim, which improves the deposition of the TACE cocktail by increasing local blood supply to the peripheral rim of the tumor nodule. On the other hand, TACE before RFA can result in a larger ablative area by reducing the blood flow to and around the tumor lesion, which helps to overcome the heat-sink effect [12].
TACE combined with RFA
In a recent retrospective observational study on 69 patients with small-sized HCC (≤ 3 cm in diameter) infeasible for US-guided RFA, combined therapy of TACE and RFA resulted in favorable 1-, 2-, 3-, 5-, 7-year local tumor progression (LTP; 4.4, 6.8, 8.2, 9.5, and 9.5%, respectively) and OS (100, 95, 89, 80, and 80%, respectively) and seems to be an effective treatment for small HCCs in unfavorable location or with poor conspicuity [13].
In the management of intermediate-sized (3–5 cm) HCCs, biplane fluoroscopy and ultrasonography (US)-guided RFA were performed on 21 patients within 14 days after TACE; cumulative rates of 1- and 3-year local tumor progression were estimated at 9.5% and 19.0%, respectively, and the incidence of complications was low (1/21) [14]. Similar therapeutic effects of combination therapy were achieved for the treatment of larger HCCs [15]. Thus, combined therapy of TACE and RFA is safe and effective for early and non-early HCCs, with low tumor progression rates and favorable OS.
TACE combined with RFA versus TACE alone
To further investigate the treatment effect of combined therapy of TACE and RFA, some investigators compared TACE-RFA with TACE alone. Yin et al. analyzed the clinical materials of 211 patients with intermediate (BCLC B stage) HCCs and reported that TACE combined with RFA achieved a higher complete tumor necrosis rate (76.9% vs. 46.5%, p = 0.02), with a lower major complication rate (1.8% vs. 2.6%) in comparison with TACE alone. Meanwhile, the results showed that the combination group had a higher total tumor control rate (74.5% vs. 54.5%, p < 0.001) and 1-, 3- and 5-year survival rates (p = 0.01) than TACE alone [16]. In a retrospective study in 59 patients with intermediate HCCs, the multivariate analysis in this study identified additional RFA as an independent factor significantly associated with positive OS [17].
In addition, Hyun et al. ran a retrospective study comparing the efficacy of combination therapy with that of TACE alone; 37 patients underwent TACE with sequential RFA, while TACE alone was performed on 54 cases for which surgical resection and US-guided RFA were unfeasible or refused by them or their family. In their study, the combination therapy group had a significantly longer time to progression (TTP; p = 0.014) and higher cumulative 1-, 2-, and 3-year overall survival rates (p = 0.008) than those in TACE alone group [18].
Moreover, by comparing the expression level of hypoxia-inducible factor (HIF-1a), early growth response protein 2 (EGR2) and alpha fetal protein (AFP) of patients with HCCs between the TACE–RFA group (n = 72) and TACE alone group (n = 72), Yuan et al. found that the combination therapy of TACE plus RFA improved both short- and long-term treatment effects by enhancing immune function, suppressing angiogenesis and reducing tumor cell proliferation [19]. In a recent meta-analysis comprising 1 RCT study and 10 retrospective studies with 928 patients also treated with TACE–RFA or TACE alone, tumor response rates; recurrence-free survival (RFS) rates; and 1-, 3-, and 5-year OS rates were superior in the TACE–RFA group (all p < 0.001) [20].
Thus, compared with TACE alone, the combination of TACE and RFA can increase the tumor necrosis rate, slow tumor progression, and improve the OS of patients with HCCs, especially intermediate HCCs.
TACE combined with RFA versus RFA alone
RFA is one of the most widely used non-surgical treatments for HCCs. In most cases, RFA is used as an alternative curative treatment for patients with early HCCs who are not suitable for surgical resection and liver transplantation. During the last decade, investigators are increasingly combining TACE with RFA to achieve better therapeutic outcomes.
In a small-scale RCT study comparing RFA combined with TACE to RFA alone in 37 patients with intermediate (3.1–5 cm) HCCs, the mean diameter of the short axis of the RFA-induced ablated areas in the RFA alone group was smaller than that in the TACE–RFA group, with significant differences (p = 0.012). Although no significant difference was observed in terms of survival rates of the patients in the two groups, RFA combined with TACE resulted in decreased local tumor progression than RFA alone at the end of the third year (6% vs. 39%, p = 0.012) [21].
A prospective randomized trial enrolling 189 patients with HCC less than 7 cm was conducted in China. The 1-, 3-, and 4-year OS (p = 0.002) and RFS (p = 0.009) of the TACE–RFA group were longer than those for the RFA group. Multivariate Cox regression analysis identified treatment allocation as one of the significant prognostic factors of RFS and OS [22].
In a recent study, 83 patients with 83 small hypervascular HCCs (range 6–30 mm) underwent RFA with or without TACE; TACE + RFA, compared to RFA alone, significantly improved OS (p < 0.001), intrahepatic distant recurrence (IDR; p = 0.038) and tumor-free survival (DFS; p = 0.010) [23]. However, different results were reported in a retrospective study, whereby Siriapisith et al. found that additional TACE might not be necessary if RFA is performed while controlling for the important factors in the management of small unresectable HCCs [24].
Several meta-analyses have shown that TACE combined with RFA results in longer OS of patients [25, 26] and RFS [27] in comparison with RFA alone. These findings suggest that combined TACE with RFA may be more effective for managing patients with unresectable HCCs than RFA alone.
TACE combined with RFA versus surgical resection
Although TACE combined with RFA has become one of the most important curative treatments for patients with HCCs, the effect of combination of TACE and RFA compared with surgical resection remains controversial. Surgical resection and liver transplantation are still the priority for early-stage HCCs.
In a retrospective matched case–control study published in 2017, 74 HCC patients within the Milan criteria underwent the combination therapy, and 148 patients who received surgical resection were selected as matched controls. Patients treated with TACE and sequential RFA had similar 1-, 3-, and 5-year overall survival (p = 0.488) as patients who underwent surgical resection (94.6, 75.1 and 55.3% vs. 91.2, 64.4, and 47.7%, respectively). The 1-, 3-, and 5-year disease-free survivals (DFS) in the TACE–RFA group were also similar (p = 0.619) to those in the surgical resection group [28]. In another multicenter case-matched study of 420 HCC patients, patients who received surgical resection had significantly longer OS (p = 0.004) than those who received the combination treatment. However, after the propensity score matching, no significant differences were observed in OS (p = 0.138) between the two groups. Subgroup analysis showed that TACE with sequential RFA provided a prolonged median OS compared to surgical resection in patients beyond the Milan criteria [29].
The above studies confirmed that combination treatment was comparable to surgical resection. However, in an RCT with 200 patients, the 1-, 3- and 5-year OS rates in the partial hepatectomy group were significantly higher than those in the TACE–RFA group (p = 0.007), and patients treated with partial hepatectomy had a significantly longer RFS than those in the combination therapy group. On further subgroup analysis of patients with HCC ≤ 3 cm in diameter, OS and RFS become comparable between the two treatments [30].
Therefore, the combination of TACE and RFA may have comparable therapeutic outcomes with surgical resection among patients with early HCCs. Additionally, the minimally invasive combined treatments result in shorter hospital stays and lower incidence of complications [31].
Microwave ablation
Microwave heating relies on a dielectric heating mechanism that generates an electromagnetic field around the electrode, resulting in homogeneous heating and coagulation necrosis of the target lesions.
TACE combined with MWA
Microwave ablation (MWA), such as RFA, has been established as an efficacious minimally invasive thermal technique that causes coagulation necrosis of tumor tissues. In a recent systematic review and meta-analysis, MWA was demonstrated to be as effective as RFA for HCC (OR 1.01, 95% CI 0.53–1.87, p = 0.98), and it provide superior outcomes compared with RFA in cases of larger nodules (OR 0.46, 95% CI 0.24–0.89, p = 0.02) [32].
In comparison with RFA, MWA heats up more quickly, and this feature contributes to shortening the time of ablation; besides, MWA can reach a higher temperature than RFA. Moreover, MWA may have the advantage of synchronously treating more target lesions in a shorter time than RFA [9, 33]. Unlike RFA, MWA has been considered to be less affected by the heat-sink effect. Thus, MWA applied after TACE has a potential benefit for patients with HCCs, since the combination therapy may surmount the heat-sink effect and thus achieve better local tumor responses than monotherapy.
TACE combined with MWA versus TACE alone
To test this hypothesis, Chen et al. studied the clinical data of 244 patients with HCC nodules not exceeding 5 cm who were treated with TACE and MWA or TACE alone. The results showed that patients in the combination therapy group had higher tumor necrosis rates and tumor response (CR + PR + SD) rates at 6 months than those in the TACE alone group (both p < 0.001). Furthermore, the combination therapy resulted in better time to tumor progression than monotherapy, and the same outcome was described in patients with tumors < 3 cm and 3–5 cm in diameter in subgroup analysis (both p < 0.005). Nonetheless, TACE combined with MWA did not show significantly better overall survival than TACE alone (p = 0.317) [34].
However, despite the similar OS of patients with HCCs not exceeding 5 cm, MWA still has potential clinical benefits for managing HCCs larger than 5 cm, since the long-term outcome of TACE and other treatments has proven disappointing. The results of a retrospective study conducted on 136 patients with 189 unresectable large HCCs (≥ 5 cm in diameter) showed that the combination therapy obtained satisfactory long-term survival as well as TTP and liver function. Additionally, the 1-, 3- and 5-year OS rates were significantly higher in the combination therapy group than those in the TACE alone group (p < 0.001) [35].
These studies indicate that combination therapy may provide better local tumor control rates and survival rates than TACE alone, especially for patients with larger HCCs. Further prospective studies with large samples, comparing combination therapy with TACE alone, are still needed.
TACE combined with MWA versus MWA alone
Thus far, several studies have compared the combination of TACE and MWA with MWA alone. In a prospective RCT study involving 94 HCC patients not exceeding 7 cm in diameter, the clinical benefits and long-term survival rate of patients treated with combination therapy or thermal ablation alone were evaluated. The 1-year, 3-year, and 5-year OS rates in the TACE combined with RFA or MWA group were 93.6, 68.1, and 61.7%, respectively, which were significantly higher (p = 0.002) than those in the thermal ablation alone group (85.1, 59.6 and 44.7%, respectively). In addition, combined treatment also achieved better RFS than the thermal ablation alone group (p = 0.008) [36]. TACE may enhance the killing effect of thermal ablation, leading to favorable therapeutic outcomes because it can block the arteries that feed tumors, which diminishes the influence of the heat-sink effect and reveals small tumors or satellite lesions.
TACE combined with MWA versus radioembolization
In western countries, patients with unresectable HCC can be treated with radioembolization using Yttrium-90 (Y90) or Technetium-99 (Tc99) microspheres. Y90 radioembolization has been demonstrated to be safe and effective for patients with HCC across clinical stages [37]. Unlike TACE, Y90 radioembolization does not induce tumoral death by embolic effect, but rather by radiation, which allows future treatments with other arterial therapies [37, 38]. The result of a recent randomized phase 2 study comparing the effect of conventional TACE (cTACE) and Y90 radioembolization in patients with HCC are encouraging. In this study, the median TTP in the Y90 radioembolization group (> 26 months) was significantly longer than that in the cTACE group (6.8 months) [39]. However, similar to previous studies, durable local control did not result in a survival benefit when comparing Y90 radioembolization with TACE or sorafenib [37].
Radiation segmentectomy (RS) is a type of radioembolization treatment protocol that allows for dose escalation to the tumor while minimizing radiation exposure to the adjacent healthy parenchyma [37]. A previous study demonstrated that RS could achieve excellent tumor responses with low toxicity [40]. However, the appropriate extent to which RS is capable of obtaining similar effectiveness outcomes compared with thermal ablation remains controversial, and few findings have directly compared RS with ablative techniques. In 2016, Biederman et al. reported a retrospective clinical study comparing the outcomes of RS and TACE combined with MWA in the management of unresectable HCC up to 3 cm in diameter. No significant differences in the survival outcomes or tumor responses were found between the combination treatment group and RS group based on follow-up imaging [41].
Radiation lobectomy is a variation of the radioembolization treatment protocol, which offers volumetric liver changes as well as tumor control [37]. In a previous time-dependent analysis, significant reductions of tumor volume were observed, indicating adequate tumor control. Furthermore, greater hypertrophy was observed in patients with portal vein thrombosis treated with radiation lobectomy who were not suitable for portal vein embolization [42]. In summary, many studies and trials have demonstrated the safety and efficacy of radioembolization in the treatment of HCC, and Y90 radioembolization may have potential for HCC patients across clinical stages due to its multiple uses [37]. However, further larger, randomized, prospective studies with optimal patient populations comparing Y90 radioembolization with other locoregional treatments are still needed.
TACE combined with MWA versus TACE combined with RFA
Comparisons of tumor response rates and survival outcomes of TACE combined with MWA and monotherapy have suggested that the combination treatment may have superior, or at least similar, clinical effects to monotherapy. To further evaluate the efficacy of TACE combined with MWA, some studies have compared TACE plus MWA with other thermal ablation in combination with TACE.
In a retrospective study comparing the response rates and survival rates between TACE combined with MWA and TACE combined with RFA, the complete response (CR) rate was similar between the two groups (p = 0.06), but TACE combined with MWA resulted in a significantly higher CR rate than TACE combined with RFA for tumors measuring 3–5 cm (100% vs. 81.2%, p = 0.01) [43]. In another retrospective study evaluating the two combination therapy regimens by histopathology, 11 patients underwent DEB-TACE plus RFA, and 31 patients underwent DEB-TACE plus MWA. The complete tumor coagulation rate was similar between the two groups (p = 0.74). Even when separating tumors < 3 cm and > 3 cm in the subgroup analysis, the complete tumor coagulation rates were still not significantly different [44].
It is reasonable to believe that MWA combined with TACE is at least similar to RFA combined with TACE and possibly has potential survival benefits for patients with intermediate-size HCC.
Cryoablation
Cryoablation is also a thermal ablation technique; but unlike RFA and MWA, it can destroy tumor tissues by the application of a device using argon gas and/or helium gas to decrease the temperature by the Joule–Thomson effect around the needle. The mechanisms of tissue destruction induced by cryoablation can be concluded as direct cellular and vascular-related injury [45].
For the management of patients with HCC, cryoablation has some advantages compared with RFA, such as cryoablation, which can create an ice ball that is well visualized with US, CT, or MRI during the procedure and is helpful to monitor treatment and control the ablation zone. Furthermore, cryoablation barely causes damage to adjacent large blood vessels and the gallbladder. Compared with other thermal ablation methods, cryoablation is a comparatively painless. Thus, patients are usually stable during the procedure [45].
However, cryoablation may cause both local and systemic side effects, such as hemorrhage, biliary injury, liver abscesses, and cryoshock. Cryoshock, also known as cytokine-mediated systemic shock, following cryoablation, including acute renal failure, acute respiratory distress syndrome, disseminated intravascular coagulation, and liver failure, is a fatal systemic complication that limits the use of cryoablation for liver tumors. The complete syndrome is very rare, while the incomplete syndrome appears to be common [46,47,48].
TACE combined with cryoablation versus cryoablation alone
Some investigators have tried to combine cryoablation with intraarterial treatment to yield better therapeutic outcomes for the treatment of patients with HCC. A retrospective study was conducted on 420 patients with unresectable HCC in consideration of their location, size or comorbidity. In this study, cryoablation was performed under the guidance of US 2 to 4 weeks after TACE. Patients in the combination therapy group tended to have larger tumors and a greater number of tumors than those in the cryoablation alone group. Although the 1- and 2-year OS rates were similar (p = 0.69 and 0.147, respectively) in the two groups, the 4- and 5-year OS rates of patients undergoing combination therapy were higher than those that underwent cryoablation alone (p = 0.001). Patients with larger HCC (> 5 cm) in the two groups were further compared, and the results showed that no patients with large HCC in the cryoablation alone group survived for more than 5 years, while 18 patients survived for more than 5 years in the sequential group [49].
TACE combined with cryoablation versus TACE alone
In another retrospective study of 122 patients with large unresectable HCC, Huang et al. found that the effective rate (p = 0.011) and control rate (p = 0.042) of patients treated with TACE and sequential cryoablation were significantly higher than those of patients treated with TACE alone. Meanwhile, the combination therapy of TACE and cryoablation prolonged the median survival time and also resulted in higher 6-, 12-, and 18-month OS rates (all p < 0.05) [50].
Similarly, in a recently published prospective study conducted on 120 patients with advanced HCC who were treated with TACE alone or TACE combined with cryoablation, TACE combined with cryoablation resulted in a higher CR rate and effective rate (p < 0.05) and longer survival time than those in the TACE alone group [51].
However, the mechanism of the combination treatment remains unclear. With this question in mind, Huang et al. recently investigated the effects of the combination therapy on changes of immune cells in the peripheral blood of HCC patients. The results showed that TACE combined with cryoablation has a good effect on patients’ immune systems; the CD4 + cells, CD4 +/CD8 + ratio, and NK cells were dramatically increased (p < 0.05), while CD8 + cells were significantly decreased (P < 0.05) [52].
Overall, these are grounds for believing that precryoablation TACE can improve the survival rate of patients treated with cryoablation, since it can shrink the tumor, especially those with HCC smaller than 3 cm in diameter.
Time intervals between TACE and local ablation
The purpose of applying the combination therapy of TACE and local ablation is to strengthen the synergistic effect of TACE and local ablation and then increase the therapeutic effect. Some studies have reported the application of pre-TACE RFA to induce peripheral hyperemic areas of the target tumor and increase the drug concentrations [53]. However, the effect of RFA may interfere with the blood circulation inside the tumor if the RFA was performed before TACE. Thus, in most situations, TACE is performed before local ablation, since it might mitigate the “heat-sink” effect and result in a larger ablation volume. However, in clinical practice, long intervals are required for recovery of liver function after TACE. In the meantime, the extended time interval leads to recanalization and neoangiogenesis, which might impair the synergistic effect of the combination therapy and weaken the therapeutic effect. An appropriate time interval of the combination therapy is one of the most critical influences on the overall therapeutic effect; however, unfortunately, the ideal time interval between TACE and local ablation is still uncertain in the current guidelines.
Up to now, few papers have studied the different time intervals between TACE and local ablation. Recently, Feng et al. retrospectively studied the clinical data of patients who underwent combination therapy of TACE and RFA with different time intervals (1–7 weeks) and tried to explore the ideal time interval between the two sessions of combination therapy. The results indicated that the complete remission rate and total effective rate decreased when the time interval was prolonged (p < 0.05). Taking liver function, complications and median survival time into consideration, they suggested that a period of 3–5 weeks is the ideal time interval of combination therapy for HCC patients of Child–Pugh classification A or B [54]. However, further studies exploring the ideal time interval between TACE and local ablation are still needed.
Conclusions
Although we are now faced with increased options for the treatment of HCC patients, including molecular targeted agents and immune checkpoint inhibitors, TACE and local ablation still play important roles in the management of HCC patients. However, both TACE and local ablation are impaired by local and distant tumor recurrence. The current literature supports the idea that the combination therapy of TACE and local ablation has advantages on survival and prognosis in patients with HCC compared with monotherapy. Different ablation techniques have different advantages.
Therefore, good patient selection for the right modality needs to be carried out to guarantee the most efficacious treatment for HCC patients. Further studies are needed to find the ideal time interval between TACE and local ablation for HCC patients.
References
Forner A, Reig M, Bruix J (2018) Hepatocellular carcinoma. Lancet 391:1301–1314
Torre L, Bray F, Siegel R, et al. (2015) Global cancer statistics, 2012. Ca Cancer J Clin 65:87–108
Bertuccio P, Turati F, Carioli G, et al. (2017) Global Trends and Predictions in Hepatocellular Carcinoma Mortality. J Hepatol 67:302–309
Chen W, Zheng R, Baade PD, et al. (2016) Cancer statistics in China, 2015. Ca Cancer J Clin 66:115–132
Crocetti L, Bargellini I, Cioni R (2017) Loco-regional treatment of HCC: current status. Clin Radiol 72:626–635
Kishore S, Friedman T, Madoff DC (2017) Update on Embolization Therapies for Hepatocellular Carcinoma. Curr Oncol Rep 19:40
Sakr OS, Berndt S, Carpentier G, et al. (2016) Arming embolic beads with anti-VEGF antibodies and controlling their release using LbL technology. J Control Release 224:199–207
Jeng WJ, Lin CC, Chen WT, et al. (2014) Adjuvant Therapy for Hepatocellular Carcinoma after Curative Treatment. Dig Dis 32:747–754
Nault JC, Sutter O, Nahon P, et al. (2017) Percutaneous treatment of hepatocellular carcinoma: state of the art and innovations. J Hepatol 68:783–797
Ng KKC, Chok KSH, Chan ACY, et al. (2017) Randomized clinical trial of hepatic resection versus radiofrequency ablation for early-stage hepatocellular carcinoma. Br J Surg 104:1775–1784
Kang TW, Lim HK, Lee MW, et al. (2015) Aggressive Intrasegmental Recurrence of Hepatocellular Carcinoma after Radiofrequency Ablation: Risk Factors and Clinical Significance. Radiology 276:274–285
Carmi L, Georgiades C (2010) Combination percutaneous and intraarterial therapy for the treatment of hepatocellular carcinoma: a review. Semin Intervent Radiol 27:296–301
Hyun D, Cho SK, Shin SW, et al. (2017) Combined transarterial chemoembolization and radiofrequency ablation for small treatment-naïve hepatocellular carcinoma infeasible for ultrasound-guided radiofrequency ablation: long-term outcomes. Acta Radiol 59:773–781
Min JH, Lee MW, Cha DI, et al. (2013) Radiofrequency Ablation Combined with Chemoembolization for Intermediate-Sized (3–5 cm) Hepatocellular Carcinomas Under Dual Guidance of Biplane Fluoroscopy and Ultrasonography. Korean J Radiol 14:248–258
Tanaka M, Ando E, Simose S, et al. (2014) Radiofrequency ablation combined with transarterial chemoembolization for intermediate hepatocellular carcinoma. Hepatol Res 44:194–200
Yin X, Zhang L, Wang YH, et al. (2014) Transcatheter arterial chemoembolization combined with radiofrequency ablation delays tumor progression and prolongs overall survival in patients with intermediate (BCLC B) hepatocellular carcinoma. BMC Cancer 14:849
Azuma S, Asahina Y, Nishimurasakurai Y, et al. (2016) Efficacy of additional radiofrequency ablation after transcatheter arterial chemoembolization for intermediate hepatocellular carcinoma. Hepatol Res 46:312–319
Hyun D, Cho SK, Shin SW, et al. (2016) Early Stage Hepatocellular Carcinomas Not Feasible for Ultrasound-Guided Radiofrequency Ablation: Comparison of Transarterial Chemoembolization Alone and Combined Therapy with Transarterial Chemoembolization and Radiofrequency Ablation. Cardiovasc Intervent Radiol 39:417–425
Yuan G, Zeng CL, Zhu DD, et al. (2017) Influences of RFA combined with TACE on the HIF-1α and EGR level of patients with primary hepatic carcinoma. Eur Rev Med Pharmacol Sci 21:1738–1745
Yang D, Luo K, Liu H, et al. (2016) Meta-analysis of transcatheter arterial chemoembolization plus radiofrequency ablation versus transcatheter arterial chemoembolization alone for hepatocellular carcinoma. Oncotarget 8:2960–2970
Morimoto M, Numata K, Kondou M, et al. (2010) Midterm outcomes in patients with intermediate-sized hepatocellular carcinoma: a randomized controlled trial for determining the efficacy of radiofrequency ablation combined with transcatheter arterial chemoembolization. Cancer 116:5452–5460
Peng ZW, Zhang YJ, Chen MS, et al. (2013) Radiofrequency ablation with or without transcatheter arterial chemoembolization in the treatment of hepatocellular carcinoma: a prospective randomized trial. J Clin Oncol 31:426–432
Tamai T, Oshige A, Tabu K, et al. (2017) Utility of percutaneous radiofrequency ablation alone or combined with transarterial chemoembolization for early hepatocellular carcinoma. Oncol Lett 14:3199–3206
Siriapisith T, Siwasattayanon P, Tongdee T (2012) Radiofrequency ablation alone versus radiofrequency ablation combined with chemoembolization in unresectable hepatocellular carcinoma. J Med Assoc Thai 95:430–436
Lan T, Chang L, Rahmathullah MN, et al. (2016) Comparative Efficacy of Interventional Therapies for Early-stage Hepatocellular Carcinoma: A PRISMA-compliant Systematic Review and Network Meta-analysis. Medicine 95:e3185
Li L, Tian J, Liu P, et al. (2016) Transarterial chemoembolization combination therapy vs monotherapy in unresectable hepatocellular carcinoma: a meta-analysis. Tumori 2016:301–310
Wang X, Hu Y, Ren M, et al. (2016) Efficacy and Safety of Radiofrequency Ablation Combined with Transcatheter Arterial Chemoembolization for Hepatocellular Carcinomas Compared with Radiofrequency Ablation Alone: A Time-to-Event Meta-Analysis. Korean J Radiol 17:93–102
Bholee AK, Peng K, Zhou Z, et al. (2017) Radiofrequency ablation combined with transarterial chemoembolization versus hepatectomy for patients with hepatocellular carcinoma within Milan criteria: a retrospective case–control study. Clin Transl Oncol 19:844–852
Pan T, Mu LW, Wu C, et al. (2017) Comparison of Combined Transcatheter Arterial Chemoembolization and CT-guided Radiofrequency Ablation with Surgical Resection in Patients with Hepatocellular Carcinoma within the Up-to-seven Criteria: A Multicenter Case-matched Study. J Cancer 8:3506–3513
Liu H, Wang ZG, Fu SY, et al. (2016) Randomized clinical trial of chemoembolization plus radiofrequency ablation versus partial hepatectomy for hepatocellular carcinoma within the Milan criteria. Br J Surg 103:348–356
Jin WK, Sang SS, Kim JK, et al. (2013) Radiofrequency Ablation Combined with Transcatheter Arterial Chemoembolization for the Treatment of Single Hepatocellular Carcinoma of 2 to 5 cm in Diameter: Comparison with Surgical Resection. Korean J Radiol 14:626–635
Facciorusso A, Maso MD, Muscatiello N (2016) Microwave ablation versus radiofrequency ablation for the treatment of hepatocellular carcinoma: A systematic review and meta-analysis. International. Int J Hyperthermia 32:339–344
Poggi G, Tosoratti N, Montagna B, et al. (2015) Microwave ablation of hepatocellular carcinoma. World J Hepatol 7:2578–2589
Chen QF, Jia ZY, Yang ZQ, et al. (2017) Transarterial Chemoembolization Monotherapy Versus Combined Transarterial Chemoembolization-Microwave Ablation Therapy for Hepatocellular Carcinoma Tumors ≤ 5 cm: A Propensity Analysis at a Single Center. Cardiovasc Intervent Radiol 40:1748–1755
Xu LF, Sun HL, Chen YT, et al. (2013) Large primary hepatocellular carcinoma: Transarterial chemoembolization monotherapy versus combined transarterial chemoembolization-percutaneous microwave coagulation therapy. J Gastroenterol Hepatol 28:456–463
Yi YX, Zhang YF, Wei Q, et al. (2014) Radiofrequency ablation or microwave ablation combined with transcatheter arterial chemoembolization in treatment of hepatocellular carcinoma by comparing with radiofrequency ablation alone. Chin J Cancer Res 26:112–118
Saini A, Wallace A, Alzubaidi S, et al. (2019) History and Evolution of Yttrium-90 Radioembolization for Hepatocellular Carcinoma. J Clin Med 8:55
Sangro B, Iñarrairaegui M, Bilbao JI (2012) Radioembolization for hepatocellular carcinoma. J Hepatol 56:464–473
Salem R, Gordon AC, Mouli S, et al. (2016) Y90 radioembolization significantly prolongs time to progression compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology 151:1155–1163
Riaz A, Gates VL, Atassi B, et al. (2011) Radiation segmentectomy: a novel approach to increase safety and efficacy of radioembolization. Int J Radiat Oncol Biol Phys 79:163–171
Biederman DM, Titano JJ, Bishay VL, et al. (2016) Radiation Segmentectomy versus TACE Combined with Microwave Ablation for Unresectable Solitary Hepatocellular Carcinoma Up to 3 cm: A Propensity Score Matching Study. Radiology 283:895–905
Vouche M, Lewandowski RJ, Atassi R, et al. (2013) Radiation Lobectomy: Time-Dependent Analysis of Future Liver Remnant Volume in Unresectable Liver Cancer as a Bridge to Resection. J Hepatol 59:1029–1036
Abdelaziz AO, Abdelmaksoud AH, Nabeel MM, et al. (2017) Transarterial Chemoembolization Combined with Either Radiofrequency or Microwave Ablation in Management of Hepatocellular Carcinoma. Asian Pac J Cancer Prev 18:189–194
Vasnani R, Ginsburg M, Ahmed O, et al. (2016) Radiofrequency and microwave ablation in combination with transarterial chemoembolization induce equivalent histopathologic coagulation necrosis in hepatocellular carcinoma patients bridged to liver transplantation. Hepatobiliary Surg Nutr 5:225–233
Song KD (2016) Percutaneous cryoablation for hepatocellular carcinoma. Clin Mol Hepatol 22:509–515
Bageacu S, Kaczmarek D, Lacroix M, et al. (2007) Cryosurgery for resectable and unresectable hepatic metastases from colorectal cancer. Eur J Surg Oncol 33:590–596
Kerkar S, Carlin AM, Sohn RL, et al. (2004) Long-term follow up and prognostic factors for cryotherapy of malignant liver tumors. Surgery (St Louis) 136:770–779
Seifert JK, Morris DL (1999) World survey on the complications of hepatic and prostate cryotherapy. World J Surg 23:109–113
Xu KC, Niu LZ, Zhou Q, et al. (2009) Sequential use of transarterial chemoembolization and percutaneous cryosurgery for hepatocellular carcinoma. World J Gastroenterol 15:3664–3669
Huang KB, Fan WZ, Zhang YY, et al. (2016) Transarterial chemoembolization combined with cryoablation for unresectable large hepatocellular carcinoma: a controlled study. Zhonghua Yi Xue Za Zhi 96:2978–2982
Huang C, Zhuang W, Feng H, et al. (2016) Analysis of therapeutic effectiveness and prognostic factor on argon-helium cryoablation combined with transcatheter arterial chemoembolization for the treatment of advanced hepatocellular carcinoma. J Cancer Res Ther 12:C148–C152
Huang M, Wang X, Huang B (2015) Effect of Transcatheter Arterial Chemoembolization Combined with Argon-Helium Cryosurgery System on the Changes of NK Cells and T Cell Subsets in Peripheral Blood of Hepatocellular Carcinoma Patients. Cell Biochem Biophys 73:787–792
Lencioni R, Crocetti L, Petruzzi P, et al. (2008) Doxorubicin-eluting bead-enhanced radiofrequency ablation of hepatocellular carcinoma: a pilot clinical study. J Hepatol 49:217–222
Feng YM, Wang X, Wang L, et al. (2017) Efficacy and safety of combination therapy of chemoembolization and radiofrequency ablation with different time intervals for hepatocellular carcinoma patients. Surg Oncol 26:236–241
Funding
This work was supported by the Innovative Team of Jiangsu Province (Grant No. 3101030420000606).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Statement of informed consent was not applicable, since the manuscript does not contain any patient data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, W., Ni, CF. Current status of the combination therapy of transarterial chemoembolization and local ablation for hepatocellular carcinoma. Abdom Radiol 44, 2268–2275 (2019). https://doi.org/10.1007/s00261-019-01943-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-019-01943-2