Abstract
Purpose
To report the results of combined therapy with transarterial chemoembolization (TACE) and radiofrequency ablation (RFA) for early stage hepatocellular carcinoma (HCC) considered infeasible for ultrasound (US)-guided RFA in comparison with those of TACE monotherapy.
Methods
From January 2007 through December 2010, 91 patients with early or very early stage HCC infeasible for US-guided RFA received either TACE alone (TACE group; n = 54) or TACE immediately followed by RFA (TACE–RFA group; n = 37) as a first-line treatment. 1-month tumor response, time to progression (TTP), and overall survival (OS) rates were calculated. Univariate and multivariate analyses were performed to identify prognostic factors.
Results
TACE–RFA group showed a better 1-month tumor response than TACE group (P < .001). The mean TTP was 29.7 ± 3.4 months (95 % confidence intervals [CIs] 23.0–36.5) in TACE group and 34.9 ± 2.8 months (95 % CIs 29.4–40.4) in TACE–RFA group. TACE–RFA group had a significantly longer TTP (P = .014). Cumulative 1-, 2-, and 3-year OS rates in the TACE and TACE–RFA groups were 91, 79, and 71 % and 100, 97, and 93 %, respectively (P = .008). Initial treatment of TACE was found to be the only significant risk factor for tumor progression and OS in multivariate analysis.
Conclusion
TACE–RFA combination therapy appears superior to TACE monotherapy in terms of 1-month tumor response, TTP, and OS when performed for early stage HCC infeasible for US-guided RFA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recent advances in diagnostic techniques have enabled the diagnosis of small hepatocellular carcinomas (HCCs) at an early stage, and thus, provide HCC patients with potentially curative treatment options, which include surgical resection, transplantation, or local ablation [1, 2]. Liver transplantation and surgical resection have been shown to be most efficacious for early stage HCCs, however, only a portion of the patients with early stage HCC are amenable to these treatments because of a shortage of donor, the presence of multiple tumors, unfavorable anatomy, poor hepatic reserve, or other clinical factors such as old age and comorbidities [1, 2]. Local ablation therapy, such as radiofrequency ablation (RFA), has emerged as an accepted therapy for early HCC because of its effectiveness and safety, and RFA is currently considered as an alternative treatment to surgical resection for early HCC [3, 4].
Ultrasound (US) is the most frequently used guidance modality for percutaneous RFA of hepatic tumors because it is safe, fast, and easily accessible and allows real-time targeting and monitoring of the index tumor during RFA procedure. However, US-guided RFA is not always feasible due to a variety of anatomical and technical factors, such as tumor location and poor conspicuity. In fact, a recent study found that US-guided RFA was not feasible in nearly half of the patients for whom percutaneous RFA was requested [5]. Computed tomography (CT) can be an alternative guidance tool in this setting. However, the US-occult lesions are usually small and therefore likely to be invisible on unenhanced CT also. Furthermore, in some hospitals, CT machines are not available for RFA guidance because their utilizations are high and CT-guided RFA takes considerable time. Newer US techniques, like fusion imaging, are being introduced to overcome the limitations of US guidance [6], but even so, US-guided RFA is not yet a practical option for a substantial proportion of patients [7]. In this clinical scenario, transarterial chemoembolization (TACE) may be an alternative and such patients have undergone TACE for tumor control and survival prolongation despite the fact that TACE is considered a palliative and not curative option like RFA [8, 9].
Recently, the use of RFA combined with TACE is gaining acceptance as a therapeutic strategy for the treatment of intermediate-sized (3–5 cm) HCCs because TACE decreases blood flow to tumors, making subsequent RFA more effective [10]. Also, TACE can add radiographic contrast to an otherwise invisible tumor as a result of intratumoral retention of radio-opaque iodized oil, and allow guidance for subsequent RFA by making the tumor depicted on fluoroscopy, unenhanced CT/cone-beam CT (CBCT), or US. A small number of studies have described the results of this type of combination therapy in cases not feasible for US-guided RFA [11–13]. However, these were non-comparative single-arm studies and the indications of combination therapy used were heterogeneous. In this study, we report the results of TACE plus RFA combination therapy as a first-line therapy for early stage HCC considered infeasible for US-guided RFA and compare the results obtained with those of TACE monotherapy.
Materials and Methods
Patients
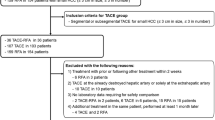
The retrospective review of patients’ images and medical records was approved by our institutional review board, which waived the requirement for patient informed consent. At our institution, HCC patients, in whom percutaneous RFA was considered, were routinely referred for planning US examinations to determine if US-guided RFA was feasible. Our hospital database search found a total of 3054 HCC patients in whom 3702 planning US examinations were performed between January 2007 and December 2010. We included 817 patients with a treatment-naïve HCC of BCLC stage 0 or A, in whom percutaneous RFA was considered due to ineligibility of surgery or patient’s preference and planning US was conducted by one of the three radiologists with at least 4 years of experience with RFA procedures at the beginning of the study period. Of them, 501 patients who were treated with US-guided RFA and 225 patients who were infeasible for US-guided RFA and treated with surgical resection (n = 217), liver transplantation (n = 6), or percutaneous ethanol injection (n = 2) were excluded from the study (Fig. 1). When a BCLC stage 0 or A HCC patient was determined to be infeasible for US-guided RFA and ineligible for other curative treatments (i.e., surgery and transplantation), the patient was routinely treated with TACE at our institution. Since February 2009 when CBCT became available at our institution, instead of TACE, we started treating those patients with a combined TACE and RFA in which RFA was performed immediately after iodized oil TACE. Finally, 91 patients with BCLC stage 0 or A HCC infeasible for US-guided RFA who received either TACE alone (TACE group, n = 54, from January 2007 through October 2009) or combined TACE and RFA (TACE–RFA group, n = 37, from February 2009 through December 2010) as a first-line treatment were enrolled in this study. Patient and tumor characteristics are summarized in Table 1. The diagnosis of HCC was established based on clinical criteria of the American Association for the Study of Liver Disease [2] as follows: typical vascular pattern (hypervascularity in the arterial phase and washout in the portal/delayed phase) of liver nodule in at least one of the dynamic CT or magnetic resonance imaging (MRI). One patient was confirmed to have a HCC by a percutaneous needle biopsy. The reasons for RFA infeasibility in TACE–RFA group were inconspicuous tumor in 33 patients (89 %), the absence of a safe electrode path in four patients (11 %), and high risk of the heat sink effect in four patients in whom a large vessel (>3 mm in diameter) was abutting the tumor (11 %). Four of them had two reasons for RFA infeasibility. The reasons for RFA infeasibility in TACE group were inconspicuous tumor in 36 patients (67 %), the absence of a safe electrode path in 17 patients (31 %), high risk of the heat sink effect in seven patients in whom a large vessel (>3 mm in diameter) was abutting the tumor (13 %), and an organ vulnerable to thermal damage (i.e., the heart) in three patients, and miscellaneous in three patients. Eleven patients of them had two or more reasons for RFA infeasibility. The three patients with an organ vulnerable to thermal damage received TACE alone.
Treatment Procedures
All procedures were performed on an in-patient basis by two radiologists with 7 and 4 years of experience with interventional radiology procedures at the beginning of the study period.
TACE
After catheterization of hepatic and mesenteric arteries with a 5-F catheter (Yashiro; Terumo, Tokyo, Japan or RH; Cook, Bloomington, IN), digital subtraction angiography was performed by monoplane C-arm angiography (Allura Xper FD20; Philips Healthcare, Best, the Netherlands) that had a flat panel detector with a 38 × 30 cm2 field of view to determine the presence of tumor staining and to identify arterial feeders of the tumor. A coaxial 2-F (Progreat; Terumo) or 2.4-F (Microferret; Cook) microcatheter was then selectively inserted into or as close as possible to the tumor feeding artery at least to the segmental branch level. Selective TACE was performed through the microcatheter by transarterially infusing a mixture of 2–5 mL of iodized oil (Lipiodol; Laboratoire Andre Guerbet, Aulnay-sous-Bois, France) and 10–20 mg of doxorubicin hydrochloride (Adriamycin; Dong-A Pharm, Seoul, Korea). The mixture of iodized oil and doxorubicin was emulsified just prior to infusion by vigorous pumping (10–20 times) between two syringes interconnected with a three-way stopcock. The doses of iodized oil and doxorubicin depended on tumor size and vascularity. Transarterial infusion of the mixture of iodized oil and doxorubicin was followed by embolization of the feeding artery with gelatin sponge pledgets (Cutanplast; Mascia Brunelli, Milan, Italy), which were manually cut into ~1 mm3 pieces. Embolization was performed until blood flow in the tumor feeding artery ceased. An intra-arterial injection of 1–3 mL of lidocaine (Lidocaine HCl 2 %; Huons, Sungnam, Korea) was used for pain control during the procedure.
Combination Therapy
In patients who underwent TACE–RFA combination therapy, RFA was performed immediately after TACE. Patients received a continuous intravenous infusion of 0.025–0.05 µg/kg/min of remifentanil HCl (Ultiva; GlaxoSmithKline, Verona, Italy) for pain control from the initiation of the RFA procedure. After completion of TACE, CBCT acquisition using C-arm angiography (XperCT; Philips Healthcare) was performed to obtain anatomical information of tumors that took up iodized oil to determine best tumor access. CBCT acquisition was composed of 244 projection images obtained with 240° rotation of the detector around the patient for a 4.1 s scanning time. When a tumor showed sufficient iodized oil uptake enough for visualization under fluoroscopy, the tumor was targeted using a RFA electrode under fluoroscopy guidance. When a tumor showed scant iodized oil uptake, the tumor was first approached using a 22-gauge Chiba needle (Cook) and CBCT acquisition was used to confirm correct positioning of the needle tip (Fig. 2), which was then used as a guide for RFA electrode positioning. Whenever applicable, US guidance was also used throughout the procedure to determine the safe electrode entry site and monitor the progression of tumor ablation. In all cases, final electrode position was confirmed by CBCT acquisition. We used a 200-W generator (Cool-tip; Valley Lab, Boulder, CO) and a 17-gauge cooled-tip electrode with a 3-cm exposed tip (Cool-tip; Valley lab) or a 17-guage internally cooled electrode with a manually adjustable active tip of 0.5–3 cm (Viva; Starmed, Goyang, Korea). Artificial ascites were infused when they were necessary to improve the sonic window and decrease the risk of thermal injury to adjacent organs such as the diaphragm [14]. In general, for tumors larger than 2.5 cm in diameter, a multiple overlapping ablation technique was applied. The ablation time for each electrode placement was at least 6 min and total ablation times ranged from 6 to 32 min per tumor. After tumor ablation, the RFA electrode tract was cauterized, while the electrode was retracted to prevent bleeding and tumor seeding. The end point was complete ablation of the visible tumor with an ablative margin of at least 5 mm.
Images of a 56-year-old man with a newly diagnosed single HCC. A Arterial phase axial CT scan shows a 1-cm-diameter HCC in hepatic segment VI (arrows), which was not discernible by ultrasound (not shown). B Axial cone-beam CT scan obtained immediately after TACE shows iodized oil retention within the tumor (arrows). C The tumor was approached using a 22-gauge Chiba needle and the needle position was confirmed by cone-beam CT acquisition. D A RFA electrode was then advanced to the tumor guided by the Chiba needle. E The final position of the RFA electrode was confirmed by another cone-beam CT acquisition. F Portal phase axial CT scan obtained 1 day after TACE–RFA shows iodized oil accumulation in the tumor completely surrounded by an ablation zone (arrows), representing complete ablation
Follow-Up and Data Analysis
Patients in TACE–RFA group were examined by contrast-enhanced CT on the following day after the procedure to evaluate immediate therapeutic results and post-procedural complications. Subsequently, patients were followed routinely by contrast-enhanced dynamic CT or MRI at 1 month after the procedure. When no radiological evidence of residual tumor or recurrence was noted, CT or MRI was performed routinely on a 3 monthly basis. The follow-up schedule for the TACE group was the same at that of the TACE–RFA group except that they did not undergo a CT scan on the following day after the procedure. CT was routinely used for the diagnosis and follow-up of tumors, and MRI was performed when CT findings were atypical or inadequate for decision making regarding residual tumor or recurrence or there were concerns about iodine contrast reaction. When recurrence or residual tumor was detected, patients received TACE, RFA, surgical resection, transplantation, radiation therapy, or sorafenib treatment depending on the progression or recurrence pattern and underlying liver function.
Technical success of TACE was defined as successful catheter placement and administration of the drug mixture and gelfoam pledgets [15]. Technical success of TACE–RFA combination therapy was analyzed on a per-tumor basis (n = 48) and determined when the index tumor(s) was treated according to the protocol (TACE plus RFA). Technique effectiveness of the combination therapy was defined when complete replacement of the target tumor by a RFA zone with an ablative margin of at least 5 mm was confirmed on CT 1 day after the procedure [16]. Tumor response at 1 month was evaluated and classified according to the modified Response Evaluation Criteria in Solid Tumor (mRECIST) for HCC [17] as follows: complete response (CR) was defined as the disappearance of all intratumoral enhancement in all target lesions; partial response (PR) was defined as ≥30 % decrease in the sum of the greatest dimension of the viable (enhancing) target lesions; progressive disease (PD) was defined as ≥20 % increase in the sum of the greatest dimension of the viable (enhancing) target lesions; and stable disease (SD) was defined as the measured shrinkage or increase not sufficient to qualify as a PR or PD.
Time to progression (TTP) was defined as the time interval between initial treatment and radiological progression. Radiological tumor progression was determined when a follow-up CT or MRI demonstrated ≥20 % increase in the sum of target tumor diameters [17], an enhancing viable tumor located in or adjacent to the treated area where complete uptake of iodized oil or complete tumor ablation had previously been obtained, or the development of any new tumor in the liver separate from the treated area. Overall survival (OS) was defined as the time from either TACE or combination therapy to death, and patients alive at the end of follow-up were censored.
Complications were classified according to the guidelines of the Society of Interventional Radiology [18]. A major complication was defined as any event that resulted in additional therapy, such as an increased level of care, hospital stay beyond observational status, permanent adverse sequelae, and death. All other complications were classified as minor. Postembolization syndrome is the most common side effect of TACE and was not considered a complication but rather an expected outcome [18].
Statistical Analysis
Comparisons between the two groups were done using Student’s t test for continuous data and the χ 2 test or Fisher’s exact test for categorical data. On an intention-to-treat basis, TTP and OS were calculated using the Kaplan–Meier method and compared using the log-rank test. The following variables were analyzed as possible prognostic factors: sex, age (<60 vs. ≥60), Child-Pugh class (A vs. B), positivity for hepatitis B virus surface antigen, positivity for hepatitis C virus antibody, tumor size (≤2 vs. >2 cm), tumor number (single vs. >1), serum α-fetoprotein (AFP) level (≤200 vs. >200 ng/mL), and initial treatment method (TACE–RFA vs. TACE alone). Univariate and multivariate analyses were performed using the Cox proportional hazard models. Variables with a P value <.2 in univariate analysis were subjected to multivariate analysis. P values of <.05 were considered statistically significant. Statistical computer software (SPSS, ver. 22.0; SPSS Inc., Chicago, IL) was used for data analyses.
Results
Technical Success, Technique Effectiveness, and 1-Month Tumor Response
TACE was successfully performed in all 54 patients in the TACE group. One tumor in the TACE–RFA group was not localized after TACE even with CBCT acquisition and RFA was not performed. Therefore, the technical success rate of TACE–RFA combination therapy was 98 % (47/48). Otherwise, all tumors were completely ablated with an adequate ablative margin on next day CT scans, thus a technique effectiveness rate of 98 % was achieved.
As for 1-month tumor response, CR was observed in 31 of 54 TACE patients (57 %), PR in 18 patients, and SD in 5 patients. CR was observed in all the 37 TACE–RFA patients, including one patient with the tumor of technical failure who had two tumors and underwent TACE–RFA for the other tumor. Although the tumor of technical failure was not localized, due to even retention of iodized oil through the hepatic subsegment containing the tumor, on both intra-procedural CBCT immediately after TACE and post-procedural CT 1 day after treatment, compact accumulation of iodized oil in the tumor was found on one-month follow-up CT as iodized oil retention in the surrounding hepatic parenchyma got washed out over time. The TACE–RFA group showed a better tumor response with a higher CR rate than the TACE group (P < .001).
Time to Progression
During follow-up, tumor progression was observed in 32 TACE patients (59 %) and 13 TACE–RFA patients (35 %). The mean TTP was 29.7 ± 3.4 months (95 % confidence intervals [CIs] 23.0–36.5 months) in TACE group and 34.9 ± 2.8 months (95 % CIs 29.4–40.4 months) in TACE–RFA group. The TACE–RFA group had a significantly longer TTP than the TACE group (P = .014) (Fig. 3A). Univariate and multivariate analyses revealed that TACE as an initial treatment was the only significant risk factor for tumor progression (Table 2).
Overall Survival
The mean follow-up times of TACE and TACE–RFA groups were 41.5 ± 18.0 months (median 47.6) and 32.0 ± 9.5 months (median 32.5), respectively. At the end of follow-up, 32 of 37 TACE–RFA patients were alive, two patients died of hepatic failure without tumor progression, and three patients were lost to follow-up. Twenty-five of 54 TACE patients remained alive, 9 patients were lost to follow-up, and 20 patients died of HCC progression (n = 17), hepatic failure without tumor progression (n = 2), or gastric variceal bleeding (n = 1). Eighty percent (43/54) of TACE patients received additional therapy following initial TACE, including TACE (n = 40), RFA (n = 18), radiation therapy (n = 6), sorafenib (n = 4), living donor liver transplantation (n = 3), and TACE–RFA (n = 1). Thirty-five percent (13/37) of TACE–RFA patients received additional therapy following initial TACE–RFA, including surgical resection (n = 7), TACE (n = 5), TACE–RFA (n = 5), living donor liver transplantation (n = 1), and radiation therapy (n = 1).
Cumulative 1-, 2-, and 3-year OS rates in the TACE and TACE–RFA groups were 91, 79, and 71 % and 100, 97, and 93 %, respectively (P = .008) (Fig. 3B). Univariate analysis showed α–fetoprotein >200 ng/mL and initial treatment of TACE were the significant poor prognostic factor for survival (Table 2). In multivariate analysis, TACE–RFA as an initial treatment was the only significant favorable factor for longer survival (hazard ratio 0.21; 95 % CIs 0.05–0.94; P = .041).
Complications of Each Initial Treatment
In the TACE group, two major complications occurred in two patients (3.7 %, 2/54). Acute cholecystitis developed in one patient and hepatic failure manifested by jaundice and newly formed ascites developed in the other; both resolved on conservative treatment. In the TACE–RFA group, two major and four minor complications occurred in six patients (16.2 %, 6/37), including two biliary strictures, two subsegmental portal vein thromboses, and two subsegmental hepatic infarctions. None of these complications led to any additional therapy, and the patients concerned remain on routine follow-up. Nonetheless, two biliary strictures (5.4 %, 2/37) were considered as a major complication because it resulted in segmental intrahepatic bile duct dilatation. No statistical difference was found in major and total complication rates between TACE and TACE–RFA groups (P = 1.000 for major complication rate, P = 0.058 for total complication rate). There were no procedure-related mortalities.
Discussion
Although TACE is considered a palliative method in the treatment of HCC, it has been applied as an alternative first-line treatment of early stage HCC in cases that curative treatments (i.e., surgery and ablation) were ineligible or refused [8, 9]. A few authors compared TACE with RFA in single HCC ≤2 cm [19] or HCC within the Milan criteria [20] or compared TACE with RFA or surgical resection in early stage HCC [21, 22], and they suggested that with careful patient selection, TACE could provide survival benefits similar to those of RFA or surgical resection for patients with early stage HCC. However, it is noteworthy that, even in these studies, TACE was associated with earlier TTP, higher tumor recurrence rates, and poorer recurrence-free survival than RFA or surgical resection. TACE–RFA combination can be another first-line treatment of early stage HCC and its therapeutic potential has been confirmed in a recent study reporting that TACE–RFA combination provides overall and recurrence-free survival rates similar to surgical resection in patients with early stage HCC [23]. Our study, comparing TACE and TACE–RFA in the clinical setting of early stage HCC infeasible for US-guided RFA, has shown that TACE–RFA combination is better than TACE monotherapy in terms of 1-month tumor response, TTP, and OS.
Our results showing better 1-month tumor response and TTP in TACE–RFA group than TACE group are similar to those of previous studies comparing TACE and RFA [19, 20]. On the other hand, the OS result of this study is different from a presumption from previous studies comparing TACE with RFA or comparing TACE–RFA with RFA [19, 20, 24, 25]. Because the previous studies showed similar results in OS between TACE and RFA or between TACE–RFA and RFA, it can be presumed that OS between TACE and TACE–RFA would be similar. However, this comparison study showed the superiority of TACE–RFA to TACE in OS. In our multivariate analysis, initial treatment of TACE–RFA was the only significant favorable factor for longer TTP and OS. Considering that TACE–RFA combination is known to create larger ablation zones than RFA monotherapy and local tumor control has a significant impact on patient survival [23, 26, 27], the superiority of TACE–RFA in this study might be explained. Nonetheless, it can be raised that the cumulative 3-year OS of 93 % in the current study seems to be excessively high. However, a recent study by Xie et al. [28] reported a 4-year OS rate of ~95 % when combination therapy was performed in patients with treatment-naïve HCCs, which is concordant with our results.
This study shows that the combination therapy under fluoroscopy and CBCT guidance is a safe and effective procedure when US-guided percutaneous RFA is not feasible. Most tumors (47/48, 98 %) were depicted by CBCT after TACE, and RFA was successfully performed. A few studies have already showed that this type of combination therapy under fluoroscopy and CBCT guidance is technically feasible for HCCs inconspicuous at US [11, 12]. However, our study is unique in that combination therapy was performed as a first-line therapy for the treatment of early stage HCCs and that it compared the clinical results of TACE monotherapy and TACE–RFA combination therapy. CT or CT fluoroscopy can be another way to guide RFA shortly after TACE [23, 29], but in some hospitals like our institution, CT machines are not available for RFA guidance because their utilization is high. Also, CT-guided RFA tends to be time-consuming and CT fluoroscopy is complicated by the high radiation dose delivered to the patient and the operator. In view of safety, CT-guided RFA for tumors located near the dome of the liver may be associated with a high risk of pulmonary complications (i.e., pneumothorax) because CT-guided RFA is often performed using a transpulmonary approach [30, 31]. Instead, the use of fluoroscopy guidance allows a greater degree of freedom for electrode insertion than US or CT guidance, an oblique approach to a dome lesion is straightforward under fluoroscopy guidance, and thus subsequent occurrence of pulmonary complications by a transpulmonary approach can be avoided [32]. The drawback that fluoroscopy does not provide cross-sectional imaging with soft-tissue contrast of CT can be eliminated by adding CBCT guidance. On the other hand, it should be mentioned that TACE–RFA combination cannot be applied for some HCCs of US-guided RFA infeasibility. For a HCC near an organ vulnerable to thermal damage (i.e., the heart) by RFA, TACE–RFA combination has the same risk of critical thermal injury to the organ. Due to the limitation of RFA in itself, all the three patients with a HCC locating near the vulnerable organs (i.e., the heart) were treated with TACE monotherapy in this study, which might have created a selection bias.
Some limitations of our study need to be mentioned. First, there is an inherent limitation of the retrospective observational design. Second, the number of patients included is relatively small. Third, historical control was used. TACE–RFA was performed more recently with use of CBCT, thus there is a possibility that patients in the TACE–RFA group received more advanced medical care. A randomized prospective study with a larger sample size would do much to overcome these limitations, but it is not practical to conduct such a study in view of the different statuses of TACE and RFA in the treatment strategy of HCC (palliative vs. curative). Fourth, a substantial portion of the patients received multimodal treatment during follow-up, which makes it difficult to analyze the therapeutic impact of first-line therapy on final outcomes, although we do not believe that the insistence of monotherapy in HCC is either practical or ethical in this era of multimodal therapies.
In conclusion, TACE–RFA combination therapy was found to be technically feasible and superior to TACE monotherapy in terms of 1-month tumor response, TTP, and OS for the treatment of early stage HCC infeasible for US-guided RFA. We recommend that this combination strategy be considered a useful therapeutic option for HCCs inconspicuous by conventional imaging guidance.
References
Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42(5):1208–36.
Bruix J, Sherman M. American Association for the Study of Liver D. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020–2.
Livraghi T. Single HCC smaller than 2 cm: surgery or ablation: interventional oncologist’s perspective. J Hepatobiliary Pancreat Sci. 2010;17(4):425–9.
Massarweh NN, Park JO, Farjah F, Yeung RS, Symons RG, Vaughan TL, Baldwin LM, Flum DR. Trends in the utilization and impact of radiofrequency ablation for hepatocellular carcinoma. J Am Coll Surg. 2010;210(4):441–8.
Rhim H, Lee MH, Kim YS, Choi D, Lee WJ, Lim HK. Planning sonography to assess the feasibility of percutaneous radiofrequency ablation of hepatocellular carcinomas. Am J Roentgenol. 2008;190(5):1324–30.
Song KD, Lee MW, Rhim H, Cha DI, Chong Y, Lim HK. Fusion imaging-guided radiofrequency ablation for hepatocellular carcinomas not visible on conventional ultrasound. Am J Roentgenol. 2013;201(5):1141–7.
Lim S, Lee MW, Rhim H, Cha DI, Kang TW, Min JH, Song KD, Choi SY, Lim HK. Mistargeting after fusion imaging-guided percutaneous radiofrequency ablation of hepatocellular carcinomas. J Vasc Interv Radiol. 2014;25(2):307–14.
Bargellini I, Sacco R, Bozzi E, Bertini M, Ginanni B, Romano A, Cicorelli A, Tumino E, Federici G, Cioni R, Metrangolo S, Bertoni M, Bresci G, Parisi G, Altomare E, Capria A, Bartolozzi C. Transarterial chemoembolization in very early and early-stage hepatocellular carcinoma patients excluded from curative treatment: a prospective cohort study. Eur J Radiol. 2012;81(6):1173–8.
Song YG, Shin SW, Cho SK, Choi D, Rhim H, Lee MW, Kim YS, Park KB, Park HS, Choo SW, Do YS, Choo IW, Hyun D. Transarterial chemoembolization as first-line therapy for hepatocellular carcinomas infeasible for ultrasound-guided radiofrequency ablation: a retrospective cohort study of 116 patients. Acta Radiol. 2015;56(1):70–7.
Ni JY, Liu SS, Xu LF, Sun HL, Chen YT. Meta-analysis of radiofrequency ablation in combination with transarterial chemoembolization for hepatocellular carcinoma. World J Gastroenterol. 2013;19(24):3872–82.
Lee MW, Kim YJ, Park SW, Hwang JH, Jung SI, Jeon HJ, Kwon WK. Percutaneous radiofrequency ablation of small hepatocellular carcinoma invisible on both ultrasonography and unenhanced CT: a preliminary study of combined treatment with transarterial chemoembolisation. Br J Radiol. 2009;82(983):908–15.
Kang SG, Yoon CJ, Jeong SH, Kim JW, Lee SH, Lee KH, Kim YH. Single-session combined therapy with chemoembolization and radiofrequency ablation in hepatocellular carcinoma less than or equal to 5 cm: a preliminary study. J Vasc Interv Radiol. 2009;20(12):1570–7.
Wang ZJ, Wang MQ, Duan F, Song P, Liu FY, Wang Y, Yan JY, Li K, Yuan K. Clinical application of transcatheter arterial chemoembolization combined with synchronous C-arm cone-beam CT guided radiofrequency ablation in treatment of large hepatocellular carcinoma. Asian Pac J Cancer Prev. 2013;14(3):1649–54.
Song I, Rhim H, Lim HK, Kim YS, Choi D. Percutaneous radiofrequency ablation of hepatocellular carcinoma abutting the diaphragm and gastrointestinal tracts with the use of artificial ascites: safety and technical efficacy in 143 patients. Eur Radiol. 2009;19(11):2630–40.
Brown DB, Nikolic B, Covey AM, Nutting CW, Saad WE, Salem R, Sofocleous CT, Sze DY. Quality improvement guidelines for transhepatic arterial chemoembolization, embolization, and chemotherapeutic infusion for hepatic malignancy. J Vasc Interv Radiol. 2012;23(3):287–94.
Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD 3rd, Dupuy DE, Gervais D, Gillams AR, Kane RA, Lee FT Jr, Livraghi T, McGahan J, Phillips DA, Rhim H, Silverman SG. Image-guided tumor ablation: standardization of terminology and reporting criteria. Radiology. 2005;235(3):728–39.
Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30(1):52–60.
Brown DB, Gould JE, Gervais DA, Goldberg SN, Murthy R, Millward SF, Rilling WS, Geschwind JF, Salem R, Vedantham S, Cardella JF, Soulen MC. Transcatheter therapy for hepatic malignancy: standardization of terminology and reporting criteria. J Vasc Interv Radiol. 2009;20(Suppl 7):S425–34.
Kim JW, Kim JH, Sung KB, Ko HK, Shin JH, Kim PN, Choi HK, Ko GY, Yoon HK, Chun SY, Gwon DI. Transarterial chemoembolization vs. radiofrequency ablation for the treatment of single hepatocellular carcinoma 2 cm or smaller. Am J Gastroenterol. 2014;109(8):1234–40.
Hsu CY, Huang YH, Chiou YY, Su CW, Lin HC, Lee RC, Chiang JH, Huo TI, Lee FY, Lee SD. Comparison of radiofrequency ablation and transarterial chemoembolization for hepatocellular carcinoma within the Milan criteria: a propensity score analysis. Liver Transpl. 2011;17(5):556–66.
Yang HJ, Lee JH, Lee DH, Yu SJ, Kim YJ, Yoon JH, Kim HC, Lee JM, Chung JW, Yi NJ, Lee KW, Suh KS, Lee HS. Small single-nodule hepatocellular carcinoma: comparison of transarterial chemoembolization, radiofrequency ablation, and hepatic resection by using inverse probability weighting. Radiology. 2014;271(3):909–18.
Hsu KF, Chu CH, Chan DC, Yu JC, Shih ML, Hsieh HF, Hsieh TY, Yu CY, Hsieh CB. Superselective transarterial chemoembolization vs hepatic resection for resectable early-stage hepatocellular carcinoma in patients with Child-Pugh class a liver function. Eur J Radiol. 2012;81(3):466–71.
Yamakado K, Nakatsuka A, Takaki H, Yokoi H, Usui M, Sakurai H, Isaji S, Shiraki K, Fuke H, Uemoto S, Takeda K. Early-stage hepatocellular carcinoma: radiofrequency ablation combined with chemoembolization versus hepatectomy. Radiology. 2008;247(1):260–6.
Kim JW, Kim JH, Won HJ, Shin YM, Yoon HK, Sung KB, Kim PN. Hepatocellular carcinomas 2–3 cm in diameter: transarterial chemoembolization plus radiofrequency ablation vs. radiofrequency ablation alone. Eur J Radiol. 2012;81(3):e189–93.
Shibata T, Isoda H, Hirokawa Y, Arizono S, Shimada K, Togashi K. Small hepatocellular carcinoma: is radiofrequency ablation combined with transcatheter arterial chemoembolization more effective than radiofrequency ablation alone for treatment? Radiology. 2009;252(3):905–13.
Okuwaki Y, Nakazawa T, Shibuya A, Ono K, Hidaka H, Watanabe M, Kokubu S, Saigenji K. Intrahepatic distant recurrence after radiofrequency ablation for a single small hepatocellular carcinoma: risk factors and patterns. J Gastroenterol. 2008;43(1):71–8.
Xu HX, Lu MD, Xie XY, Yin XY, Kuang M, Chen JW, Xu ZF, Liu GJ. Prognostic factors for long-term outcome after percutaneous thermal ablation for hepatocellular carcinoma: a survival analysis of 137 consecutive patients. Clin Radiol. 2005;60(9):1018–25.
Xie H, Wang H, An W, Ma W, Qi R, Yang B, Liu C, Gao Y, Xu B, Wang W. The efficacy of radiofrequency ablation combined with transcatheter arterial chemoembolization for primary hepatocellular carcinoma in a cohort of 487 patients. PLoS One. 2014;9(2):e89081.
Takaki H, Yamakado K, Nakatsuka A, Yamada T, Uraki J, Kashima M, Yamanaka T, Shiraki K, Takei Y, Takeda K. Computed tomography fluoroscopy-guided radiofrequency ablation following intra-arterial iodized-oil injection for hepatocellular carcinomas invisible on ultrasonographic images. Int J Clin Oncol. 2013;18(1):46–53.
Shibata T, Shibata T, Maetani Y, Kubo T, Itoh K, Togashi K, Hiraoka M. Transthoracic percutaneous radiofrequency ablation for liver tumors in the hepatic dome. J Vasc Interv Radiol. 2004;15(11):1323–7.
Toyoda M, Kakizaki S, Horiuchi K, Katakai K, Sohara N, Sato K, Takagi H, Mori M, Nakajima T. Computed tomography-guided transpulmonary radiofrequency ablation for hepatocellular carcinoma located in hepatic dome. World J Gastroenterol. 2006;12(4):608–11.
Lee MW, Kim YJ, Park SW, Yu NC, Choe WH, Kwon SY, Lee CH. Biplane fluoroscopy-guided radiofrequency ablation combined with chemoembolisation for hepatocellular carcinoma: initial experience. Br J Radiol. 2011;84(1004):691–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dongho Hyun, Sung Ki Cho, Sung Wook Shin, Kwang Bo Park, Hong Suk Park, Sung Wook Choo, Young Soo Do, In-wook Choo, Min Woo Lee, Hyunchul Rhim, and Hyo Keun Lim declare that they have no conflict of interest.
Ethical Approval and Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Hyun, D., Cho, S.K., Shin, S.W. et al. Early Stage Hepatocellular Carcinomas Not Feasible for Ultrasound-Guided Radiofrequency Ablation: Comparison of Transarterial Chemoembolization Alone and Combined Therapy with Transarterial Chemoembolization and Radiofrequency Ablation. Cardiovasc Intervent Radiol 39, 417–425 (2016). https://doi.org/10.1007/s00270-015-1194-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-015-1194-0