Abstract
Background
Current evidence for the use of FDG PET/PET-CT in staging thoracic oesophageal and GOJ cancer is reviewed.
Methods
PubMed, Medline, Embase (1988–November 2006) and the Cochrane database identifed studies in which FDG PET and PET CT were used for the assessment of thoracic and GOJ cancer.
Results
Conventional assessment remains the mainstay for evaluating the primary site. EUS is used for assessing the primary site, but when EUS is incomplete or not tolerated FDG PET CT is invaluable. The major of advantage of FDG PET CT lies in the ability to detect metastatic disease beyond the celiac axis. There is growing evidence to show that FDG PET CT is useful for assessment of treatment response. FDG PET CT will also detect other occult primary cancers.
Conclusions
The contribution of FDG PET CT to the investigation of patients with primary thoracic oesophageal and GOJ cancer has resulted in improved staging, so providing the ability to optimise treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Accurate staging of disease is central in the management of patients with thoracic oesophageal and gastro-oesophageal junction cancer. The results accomplished with surgery alone are good in those patients with early stage disease [1]. In tumours with locally advanced disease such as those with invasion into adjacent structures (T4 disease), overall survival figures are less impressive, and non-surgical treatment with radiotherapy and chemotherapy have been combined with surgery in an attempt to improve survival [2, 3]. However, combining therapies increases morbidity and mortality rates, so that it is difficult to justify in patients who would have had a good prognosis after surgery alone, or a poor prognosis due to metastatic disease [3, 4].
The current standard non-invasive modalities for staging thoracic oesophageal cancer and GOJ cancer are computed tomography (CT) and endoscopic ultrasound (EUS) [5].
EUS is accepted as the most accurate way to identify the depth of tumour invasion (T stage) and it may also reveal local regional lymph node metastases. CT is more useful for identifying distant metastases. With these techniques, diagnosis is based on derangement of anatomical characteristics. Detection of metastatic disease within normal sized lymph nodes and distinguishing enlarged inflammatory nodes from those due to tumour infiltration remains a challenge. Furthermore, metastatic lesions causing minimal anatomical distortion, and with similar Hounsfield units to adjacent tissue, may not be identified.
Position emission tomography (PET) is unique in its ability of visualise areas of increased metabolic activity within tissues. [18F] fluorodeoxyglucose (FDG) is preferentially taken up by cells with a high rate of glucose utilization, and this includes most malignant cells.
FDG PET has been recommended for the staging of oesophageal cancer [6, 7]. Current evidence for this recommendation is justified and obtained from the following sources: PubMed (November 1988–2006), Medline (November 1988–2006), and Embase (November 1988–2006). The Cochrane central registry was searched to identify trials and reviews in which FDG PET and PET CT was used for the assessment of thoracic and gastro-oesophageal junction (GOJ) cancer. We also reviewed the reference lists of the articles selected for inclusion. Electronic searches were supplemented by hand searching of recent relevant journals.
Staging primary disease
Primary site (T stage)
FDG PET detects disease at the primary site. Drawing from the cumulative data of 7 studies which included 281 patients (adenocarcinoma 139, squamous cell carcinoma (SCC) 139, other histology 3), where FDG PET was used for staging thoracic and GOJ oesophageal cancer, the technique identified 265/281 (94%) primary sites [8–14]. Fifteen T1 primary tumours and 1 Tis were not visualised (adenocinoma 2, SCC 10, histology not stated 4), with the majority of these cancers being 5 mm or less in diameter.
It should be recognised that since many of these studies were completed, PET technology has advanced considerably. In two of the studies, the scanners used and images obtained would be regarded by today’s standards as less than optimal and this accounted for 11/16 (69%) of the false negative results in the above survey.
FDG PET, and now PET CT, is of value in patients where assessment of the primary site is considered to be inadequate following EUS and CT (Fig. 1).
A 55-year-old man with an adenocarcinoma of the distal thoracic oesophagus A Endoscopic examination was incomplete because of extensive endoluminal disease. B FDG PET CT showed extension of tumour at the primary site to the gastro-oesophageal junction, within a hiatus hernia. There was no significant uptake in the stomach or in distant nodes and viscera. Subsequent surgery confirmed the extent of disease at the primary site and the nodal status as diagnosed by FDG PET CT.
The accuracy of FDG PET to localise the primary site is based on patients with an established biopsy proven diagnosis of carcinoma of the oesophagus, and further studies are required to evaluate the possible value of FDG PET CT as a screening test. Of particular interest is the application in patients with Barrett’s oesophagus; its ability to detect relatively small cancers against a background of intestinal metaplasia deserves further assessment [15, 16].
Regional nodes (N stage)
There is considerable variation with regards to the accuracy of FDG PET for detecting regional nodal disease.
In a retrospective assessment of 53 patients with SCC limited to the thoracic oesophagus, FDG PET had an accuracy of 84% when compared with oesophagectomy and lymph node dissection [11]. In another retrospective review of 36 patients with thoracic oesophageal carcinoma, mainly adenocarcinoma, FDG PET had an accuracy of 76%; the findings were confirmed by correlation with the trans-thoracic oesophagectomy specimen and examination of selectively resected nodes suspicious of containing tumour [17].
In a prospective evaluation of 74 patients, FDG PET had an accuracy of 61% when correlated to two field lymphadenectomy in 66% (40/61) patients and biopsy findings in the others [18]. By contrast, in 1 prospective study of 42 thoracic oesophageal and GOJ cancer patients (adenocarcinoma 32, SCC 10) FDG PET had an accuracy of 48%; the results verified by 2 and 3 field lymphadenectomy in all patients [19].
Similarly, in a retrospective study of 47 thoracic oesophageal cancer patients (adenocarcinoma 37, SCC 10), FDG PET had an accuracy of 46%, when only definitive results were considered and 49% when equivocal results were included, the FDG PET findings confirmed by minimally invasive surgical techniques [20].
The different patient cohorts studied, the different methodologies including different PET scanners and PET techniques used, and also the varying ways in which the FDG PET findings were confirmed all contribute to the conflicting FDG PET results.
The specificity of FDG PET for detecting regional nodal disease is generally high with false positive results being unusual. The low accuracy for FDG PET is due to low sensitivity: 55% sensitivity in the study where FDG PET had an accuracy of 61%, 22% where it had an accuracy of 48% and in the study where FDG PET had an accuracy of 46%, its sensitivity was 35%. The inability of FDG PET to separately detect nodes containing tumour adjacent to the primary site contributes significantly to the false negative results.
The capability of FDG PET to detect nodal disease compared with CT and EUS is unclear. In two studies, FDG PET was found to be more accurate than CT, in one study both techniques were of similar accuracy and in yet another two studies FDG PET was less accurate. In two studies that compared FDG PET to CT and EUS, EUS was superior to FDG PET and CT although the difference did not reach statistical significance [18, 19]. In the one study comparing FDG PET to CT and the combination of EUS and fine needle aspiration cytology (FNAC), there was no clear advantage of EUS over FDG or CT [21].
It is reasonable to conclude from the literature that a positive node on FDG PET is highly likely to contain active disease, especially if it lies in the usual drainage area. FDG PET cannot, however, reliably and consistently separate the primary site from closely adjacent nodal disease and therefore distinguish between T3/4N0 and T3/4NI disease.
The available data, albeit small, indicates that the main contribution of EUS over FDG PET lies in its superior ability to discriminate between the primary tumour and peritumoural nodes, otherwise there is no definite advantage of FDG PET over EUS for assessing loco regional nodal disease. In centres where EUS is used for assessing the primary site, then there may be no clear benefit obtained from FDG PET CT for evaluating regional nodal disease, except in those patients who cannot tolerate EUS or in which EUS is incomplete, because of a severe stenosis at the primary site.
Distant metastases (M stage)
The literature consistently shows that FDG PET is more accurate compared with other imaging for detecting disease beyond regional nodes [9, 13, 17, 18, 20, 22]. One prospective study which evaluated 91 patients with carcinoma of the oesophagus which was potentially resectable prior to FDG PET, reported that FDG PET was more accurate than CT for detecting disease beyond regional nodes. The authors observed that the group where FDG PET identified metastatic disease had a statistically significantly lower probability of survival compared with the group with no metastatic disease on FDG PET, a difference that was not obtained with CT [22].
A prospective study which compared FDG PET to CT and EUS in the initial staging of oesophageal carcinoma in 74 patients (thoracic oesophagus 43, GOJ 31) found FDG PET to be superior to CT and EUS when used in combination for detecting metastases beyond regional nodes. This difference was largely due to the greater sensitivity of FDG PET for detecting disease in supraclavicular and retroperitoneal nodes and beyond, 74% compared with 47% [9].
Similar results were obtained in another prospective study of 24 patients. FDG PET compared with combined EUS and CT, was more accurate for detecting M1a disease, i.e., metastases within celiac axis nodes, and also M1b disease, i.e., metastases beyond that; of the three M1b patients, CT identified three of these patients compared with FDG PET which identified 7 [18].
In two studies the additional information provided by FDG PET improved the assessment for resectability. In a study of 42 patients who had FDG PET and CT, 17 patients were reclassified as having unresectable disease following FDG PET compared with only 6 after CT. Unexpected supraclavicular nodal disease was detected by FDG PET in five patients, mediastinal nodal disease in three, coeliac axis nodal disease in one and liver metastases in a further two [8]. In a further prospective study of 26 consecutive patients the accuracy of CT in determining resectability was 65%, compared with 88% for FDG PET and 92% when CT was interpreted in conjunction with the FDG PET [12].
There is therefore a clear advantage of FDG PET for detection of disease beyond the celiac axis (Fig. 2). Distinguishing between a regional node, N1 node, and the celiac axis M1a node can however, be challenging, even with FDG PET CT. Enlarged nodes lying adjacent to the origin of the celiac axis do not pose a dilemma, but an FDG avid node which is minimally enlarged, and lying a short distance from the origin, can be difficult to classify as a regional nodes such as a lesser curve node or alternatively a celiac axis node, particularly when the stomach is distended.
A FDG PET CT shows intense uptake at the primary site in the mid thoracic oesophagus (arrow) B FDG PET CT demonstrates tumour within a coeliac axis node. The node containing tumour is of normal size on CT. C An unexpected bone metastasis is shown on FDG PET CT Patient management plan was changed from surgery to chemotherapy on the basis of the PET CT. D Subsequent FDG PET CT shows progression of the bone metastasis despite chemotherapy.
Impact on management
In a prospective survey of 91 patients planned for surgery, FDG PET revealed unsuspected disease in 16 patients (17%) which led to non-surgical interventions [22]. In a similar study, FDG PET significantly changed management in 17% (6/36) patients [17].
In yet another study, FDG PET provided information which altered treatment in 25% (12/48) of the study population; detecting unsuspected metastases in some patients, and in others identifying suitable biopsy sites which confirmed metastatic disease [8].
Impact based on comparison of a prospectively recorded pre FDG PET plan with the post FDG PET treatment plan in 68 consecutive patients undergoing staging found that FDG PET impacted on management in 27/68 (40%) of patients; in 12 therapy plan was changed from curative to palliative and in 3 from palliative to curative, while in 12 other patients there was a change in treatment modality or delivery. Furthermore, FDG PET provided superior prognostic stratification compared with conventional investigations [23].
Independent prognostic marker
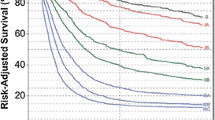
There is a growing body of evidence that demonstrates the value FD PET as prognostic marker in patients with thoracic oesophageal and gastro-oesophageal cancer. A prospective study of 59 patients with locally advanced oesophageal cancer found that upstaging with FDG PET, which occurred in 1/3 of patients, predicted poor 2-year survival, despite comparable treatment [24]. Data from a retrospective review of 150 patients with localised oesophageal cancer on conventional assessment (stage II/III) showed that there was a strong correlation between outcome and the number of FDG avid sites; as a group, patients with only one FDG positive site had higher overall and also disease free survival compared with those with more than one FDG avid site [25].
Semi-quantitative analysis may contribute to the value of FDG PET in this area and preliminary results suggest that avidity of FDG uptake of the primary tumour before treatment can predict treatment outcome. In 23 patients with SUV mean greater than 7.0 at the primary site had a poorer prognosis compared with 25 patients, where the primary tumour had an SUV of less than 7.0 [26]. In another one report, survival was significantly higher in patients with a maximum standardised uptake value (SUV max) of 6.6 or less at the primary site compared with the group with SUV max of more than 6.6 [27]. In yet another study, which included an analysis of surgically managed oesophageal adenocarcinoma patients SUV max predicted overall survival and also identified a group of patients who had a poor prognosis who would otherwise have been considered to have early stage disease [28].
Restaging of primary disease
Neoadjuvant treatment, chemotherapy, radiotherapy and a combination of chemotherapy and radiotherapy, is increasingly being used in conjunction with surgery in an attempt to improve survival in patients with locally advanced thoracic oesophageal and gastro-oesophageal junction cancer. Various pilot studies have shown the value of FDG PET for measurement of treatment response and a recent meta-analysis found FDG PET to be more accurate than CT and as accurate as EUS [29–37]. Endoscopic examination is not always feasible during or shortly after chemotherapy; in the meta-analysis just considered there were no failure rates with FDG PET compared with inadequate EUS in 6% [29]. FDG PET CT, as such, is a promising tool for assessment of treatment response [35].
FDG PET cannot consistently detect small volume residual disease, and the same is true for FDG PET CT [31, 32, 35, 36]. FDG PET CT, however, can potentially identify those patients who will achieve the greatest benefit from surgery, from those with a poor response to neo-adjuvant treatment and have residual bulky disease, who will be unlikely to benefit from surgery [37–41]. Neo-adjuvant treatment in patients with advanced oesophageal cancer is evolving, and with it the role of FDG PET CT in this area [3, 32] (Fig. 3).
Synchronous cancers
When FDG PET CT is used for the staging and restaging of oesophageal cancer other primary cancers are detected [42]. The incidence of synchronous head and neck and lung tumours in patients with oesophageal cancer is 2% and 3%; tobacco and alcohol consumption link these tumours [43]. Unexpected lung cancers are revealed more often than head and neck cancers, since the latter are usually apparent clinically. FDG PET CT also detects other asymptomatic synchronous tumours, the most common being colo-rectal cancer (Fig. 4).
A 63-year-old woman with an adenocarcinoma of the gastro-oesophageal junction A FDG PET CT showed the small primary site (T1). It demonstrated no distal nodal or visceral metastases. B FDG PET CT however, revealed a small focus of abnormal uptake in the rectum. Subsequent sigmoidoscopy confirmed that it represented a small T1 rectal cancer, which was asymptomatic.
PET CT
Imprecise localization of radiotracer is a limitation of PET imaging. Software image fusion is labour intensive and is usually unsuccessful unless data is acquired prospectively. Accurate soft-ware registration of FDG PET and CT data separately acquired is achievable in the cranial cavity, head and neck and the pelvis but is technically challenging in the chest and upper abdomen due to the lack of common 3D points required for registration [44]. PET CT overcomes this by acquiring PET and CT without patient movement, so enabling registration.
With PET CT, CT is acquired first, followed by PET. Using CT for attenuation correction also means shorter scanning times; 25 min or less for a whole body PET CT, compared with 60 min for PET alone.
Advantages of PET CT include superior localisation of lesions and better distinction between physiological uptake and pathology. PET CT augments the information provided by PET and provides potential to improve the accuracy of FDG for detecting distant nodal and distant organ metastases. Several studies in lung cancer have already shown that PET CT improved on localisation of radiotracer uptake which in turn led to a reduction in false positive and false negative results as well as improved diagnostic certainly [45, 46].
A study to assess the additional value of PET CT over PET and CT included 13 patients pre-surgery, where PET CT was compared with FDG PET and high-resolution contrast enhanced CT side by side improved the accuracy of FDG in oesophageal cancer and provided additional data which assisted patient management [47].
Our own recently completed prospective study comparing the accuracy of FDG PET CT, FDG PET and diagnostic CT side by side, and diagnostic CT alone for the staging of thoracic oesophageal and GOJ cancer is in concordance with these results. Following local ethical committee approval, 48 patients were recruited between June 2004 and February 2005 (males 36, females 12; age 47.7–77.8 years [mean 66.2 years]); thoracic oesophageal cancer 14 patients, GOJ cancer 13 patients; adenocarcinoma 38 patients, squamous cell carcinoma 10 patients). All patients were considered to be suitable for treatment with curative intent on standard assessment which included full clinical assessment and whole body CT. All patients had a whole body diagnostic CT and FDG PET CT. The diagnostic CT was reviewed independent of FDG PET CT by one experienced observer. The PET and the diagnostic CT were reported side by side in consensus by two experienced observers. PET CT was then reported in consensus by the two observers who had previously reported the PET and diagnostic CT side by side. The impact of PET CT on management was assessed using a questionnaire completed by the referring medical personnel. The diagnostic CT was obtained within 1 month of the PET CT, and all scans were technically satisfactory on review. Surgical correlation was obtained in 20 patients, with M1b disease confirmed by biopsy in 2, other imaging in 1 and follow-up in 4 patients, the latter between 12 and 16 months (mean 14 months). PET and diagnostic CT side by side upstaged four patients from M0 to M1b, by detecting liver metastases in one, characterising indeterminate lung nodules in two, and discovering a scalene node containing active disease in one patient. PET CT further upstaged three patients by detecting liver metastases in two patients and bone metastases in one. In addition, PET CT found an asymptomatic caecal cancer in one patient and a villous adenoma in one another. PET CT altered overall management in eight (17%) patients compared with PET and CT side by side in three (6%).
Pitfalls
The oesophagus is usually not avid for FDG. Inflammation, however, can mimic oesophageal malignancy. At the gastro-oesophageal junction, accumulation of FDG due to reflux oeosphagitis needs to be distinguished from a gastro-oeosphageal junction carcinoma [48]. Widespread candidiasis of the upper gastro-intestinal tract can result in diffuse FDG uptake within the oesophagus; however, this should not cause a clinical dilemma, as the condition is usually apparent clinically.
Intense FDG uptake occurs in nodes infiltrated with sarcoid and lymphoma as well as in HIV patients with persistent generalized lymphadenopathy and also in patients suffering from other viral infections including Epstein Barr and cytomegalo-viral infections [49]. With regards to lymphoma, follicular lymphoma, is the one lymphoma that is not consistently avid for FDG; however, it may be FDG avid and it is this subtype that is most likely to cause confusion as many of these patients will be asymptomatic from their lymphoma [50].
That brown adipose tissue exhibits FDG uptake is well recognised, and is should not be mistaken for metastases once it is appreciated that this phenomenon can occur in the vicinity of potential sites of metastases including around the adrenal glands and in the posterior mediastinum.
Identification of small sub-centimeter hepatic deposits can prove to be a challenge with FDG PET CT. It may be necessary to correlate the FDG PET CT to a post-intravenous contrast diagnostic CT to distinguish between noise and liver metastases in this situation. Liver abscess can be detected by FDG PET CT, and is indistinguishable from metastatic liver disease [51]. Fortunately, distinguishing the two conditions is not usually a clinical problem.
Uptake of FDG in the adrenal due to benign lesions is unusual. Occasionally, bilateral adrenal hyperplasia can demonstrate intense FDG uptake.
False positive results due to inflammatory foci including tuberculosis, histoplasmosis and aspergillosis should always be considered in patients with focal FDG lung parenchymal uptake, especially if solitary [52, 53]. Furthermore, spatial resolution limitations of PET should be remembered in assessment of lesions less than 10 mm [54].
Intense FDG uptake occurs with benign bone lesions including Pagets disease of bone and also around joints in patients with arthritis including osteoarthritis, commonly; review of CT component of PET CT soon however, resolves the diagnostic dilemma [53].
In the hands of experienced interpreters, false positive results are low, if careful correlation of the FDG is made with the CT, and in cases where there is doubt, FDG is compared with other relevant imaging and the imaging findings are interpreted in conjunction with the clinical pattern of disease; one recent study found that it was in the order of 5% [55].
Other radio-tracers
Carbon-11 choline has been compared with FDG for the staging of oesophageal cancer in two studies. In one, carbon-11 choline showed an advantage over FDG for detecting mediastinal nodal disease compared with FDG. It was however, ineffective for detecting abdominal nodal disease [56]. The authors noted that this was because nodal uptake in the abdomen was obscured by high uptake of the tracer in liver. The other study confirmed the limited value of carbon-11 choline for detecting abdominal nodal disease and also suggested that it was also less accurate than FDG for detecting lung, liver and bone metastases [57].
Pre-therapeutic identification of patients likely to benefit from neo-adjuvant treatment would allow enhanced treatment stratification, so that potentially toxic treatments could be avoided in non-responders, who instead could be offered alternative therapies [58–60]. The profiling of tumours using PET tracers that focus on specific aspects of tumour metabolism such as the use of 3′-deoxy-3′-fluoro thymidine (FLT) as an index of tumour proliferation may contribute in this area [61].
Concluding remarks
There is substantial evidence from non-randomised prospective studies for the use of FDG PET in staging primary oesophageal cancer. The contribution of FDG PET CT to the investigation of the patient with primary thoracic oesophageal and GOJ cancer is still evolving, and ultimately, this may be influenced by individual clinical practice as well as local availability. There is no doubt however, that it will contribute to improved management of this group of patients, leading to more appropriate treatment, and so spare some patients unnecessary medical or surgical intervention which will provide no benefit.
References
Lerut T, Decker G (1999) Oesophageal cancer Curr Opin Gastroenterol 15:364–369
Muller JM, Erasmi H, Stelzner M, Zieran U, Pichlman H (1990) Surgical therapy of oesophageal cancer Br J Surg 77:845–857
Geh JI, Crellin AM, Glynn Jones R (2001) Pre-operative (neo-adjuvant) chemotherapy in oesophageal cancer Br J Surg 88:338–356
Blazeby JM, Sanford E, Falk SJ, Alderson D, Donovan JL (2005) Health related quality of life during neoadjuvant treatment and surgery for localised oesophageal carcinoma Cancer 103:1791–1799
Rice TW (2000) Clinical staging of oesophageal cancer CT EUS and PET, Chest Surgery Clin N Am 10:471–485
Czernin J, Phelps ME (2002) Positron emission tomography scanning: current and future applications Ann Rev Med 53:89–112
A framework for the development of PET services in England. Department of Health document October 2005 gateway number 5265
Block MI, et al. (1997) Improvement in staging of esophageal cancer with the addition of Positron Emission Tomography, Ann Thorac Surg 64:770–777
Flamen P, et al. (2000) Utility of positron emission tomography for the staging of patients with potentially operable esophageal carcinoma J Clin Oncol 18:3202–3210
Kato, et al. (2002) Comparison between positron emission tomography and computed tomography in the use of the assessment of esophageal carcinoma Cancer 4:921–928
Kim , et al. (2001) Evaluation of lymph node metastases in squamous cell carcinoma of the esophagus with positron emission tomography Ann Thorac Surg 71:290–294
Kole AC, et al. (1988) Positron emission tomography for staging of oesophageal and gastroesophageal malignancy Br J Cancer 78: 521–527
Rankin SC, et al. (1988) Computed tomography and positron emission tomography in the pre-operative staging of oesophageal carcinoma Clin Radiol 53: 659–665
McTeer D, et al. (1999) Evaluation of 18 F-FDG positron emission tomography gastric and oesophageal carcinoma BJR 72:525–529
Neto C, Zhuang H, Ghesani N, Alavi A (2001) Detection of Barretts oeophagus superimposed by oesophageal cancer by FDG positron emission tomography Clin Nucl Med 26:1060
Bakheet S, Amin T, Alia A-G, Kuzo R, Powe J (1999) f-18 FDG uptake in benign oesophageal cancer Clin Nucl Med 24:995
Flanagan FL, et al. (1997) Staging of esophageal cancer with 18 F-fluorodeoxyglucose positron emission tomography AJR 168:417–424
Heeren , et al. (2004) Detection of distant metastases in esophageal cancer with 18 F-FDG PET JNM 45:980–987
Lerut T, et al. (2000) Histopathologic validation of lymph node staging with FDG-PET scan in cancer of the esophagus and gastroesophageal junction: a prospective study based on primary surgery with extensive lymphadenectomy Ann Surg 232:743–752
Meltzer CC, et al. (2000) Whole-body FDG positron emission tomographic imaging for staging esophageal cancer: comparison with computed tomography Clin Nucl Med 25:882–887
Lowe VJ, Booya F, Fletcher JG, et al. (2006) Comparision of PET, CT and EUS in the initial staging of patients with oesophageal cancer Mol Imaging Biol 7:422–430
Luketich JD, et al. (1999) Evaluation of distant metastases in esophageal cancer: 100 consecutive positron emission tomography scans Ann Thorac Surg 68:1133–1137
Duong CP, et al. (2006) Significant clinical impact and prognostic stratification provided by FDG PET in the staging of oesophageal cancer Eur J Nucl Med Mol Imaging 33:759–769
Blackstock AW, et al. (2006) A prospective evaluation of the impact of FDG PET staging on survival for patients with locally advanced oesophageal cancer Int J Radiat Oncol Biol Phys 64:455–460
Hong D, et al. (2005) Value of baseline PET for predicting overall survival in patient with non-metastatic oesophageal or gastro-oesophageal junction cancer Cancer 104:1602–1606
Fukunaga T, et al. (1988) Evaluation of esophageal cancers using fluorine-18-fluorodeoxyglucose PET J Nucl Med 39:1002–1007
Cerfolio RJ, Bryant AS (2006) Maximum standardized uptake values on positron emission tomography of oesophageal cancer predicts stage, tumour biology and survival Ann Thorac Surg 82:391–395
Rizk N, et al. (2006) Preoperative FDG PET SUV predict survival after oesophageal adenocarcinoma resection Ann Thorac Surg 81:1076–1082
Westreenen M, et al. (2005) Esophageal cancer: CT, endoscopic US and FDG PET for assessment of response to neoadjuvant therapy- systematic review Radiology 236:841–851
Downey RJ, et al. (2003) Whole body 18-FDG PET and the response of oesophageal cancer to induction therapy: results of a prospective study J Clin Oncol 21:428–432
Flamen P, et al. (2002) PET for assessment of the response to induction radiochemotherapy in locally advanced oesophageal cancer Ann Oncol 13:361–368
Weber et al. (2001) Prediction of response to pre-operative chemotherapy in adenocarcinomas of the esophageal junction by metabolic imaging J Clin Oncol 19:3058–3065
Brucher BJDM, et al. (2001) Neoadjuvant therapy of oesophageal squamous cell carcinoma: response evaluation by PET Ann Surg 233:300–309
Couper GW, et al. (1998) Detection of response to chemotherapy using PET in patients with oesophageal and gastric cancer Br J Surg 85:1403–1406
Cefolio RJ, Bryant AS, Ohja B, Bartolucci AA, Eloubeidi MA (2005) The accuracy of EUS with FNA, integrated PET CT and CT in restaging patients with oesophageal cancer after neo-adjuvant chemotherapy J Thorac Cadiovas Surg 129:1232–1241
Melcher L, Wong WL, Sanghera B, et al. (2004) Sequential FDG-PET scanning in the assessment of response to neoadjuvant chemotherapy in operable esophageal cancer. J Clin Oncol 22,14S:4056
Melcher L, Sanghera B, Wong WL, et al (2006) The relationship between FDG PET values histological response and survival in patients undergoing neoadjuvant chemotherapy for potentially operable oesophageal cancer. J Clin Oncol 24:18S
Korst RJ, Kansler AL, Port JL, Lee PC, Kerem Y, Altorki NK (2006) Downstaging of T or N predicts long term survival after pre-operative chemotherapy and radical resection for oesophageal cancer Ann Thorac Surg 82:480–485
Duong CP, et al. (2006) FDG PET status following chemoradiation provides high management impact and powerful prognostic stratification in oesophageal cancer Eur J Nucl Med Mol Imaging 33:770–778
Levine EA, et al. (2006) Predictive value of FDG PET in the identification of responders to chemoradiation therapy for the treatment of locally advanced oesophageal cancer Ann Surg 243:472–478
Westerterp M, van Westreenen HL, Sloof GW, Plukker J, Th M, van Lanschot JJB (2006) Role of PET in the (re-) staging of oesophageal cancer Scaninavian J Gastroent 41(suppl 243):116–122
van Westreenen et al. (2005) Synchronous primary neoplasms detected on FDG in staging of patients with oesophageal cancers J Nucl Med 46:1321–1325
Assessment(2000) In: Watkinson Gaze MN, Wilson JA, (eds). Stell & Maran’s Head and neck surgery, 4th edn. Butterworth Heinemann publication, Oxford, chap 2, pp 11–28
Wong WL, et al. (1996) Validation and clinical application of computer combined CT and PET with FDG head and neck images Am J Surg 172:628–632
Lardinosis D, et al. (2003) Integrated PET CT imaging improves staging of NSCLC n Eng J Med
Shim SS, et al. (2005) Non-small cell lung cancer prospective comparision of intergrated FDG PET CT and CT alone for pre-operative staging Radiology 1011:1019
Bar-Shalom R, et al. (2005) The additional valyue of PET/ CT over PET and FDG imaging of oesophageal cancer Eur J Nucl Med Mol Imaging 32:918–924
Rampin L, Rubello D, Nanni C, Fanti S (2005) Value of PET CT fusion imaging in avoiding potential pitfalls in the interpretation of 18-F-FDG accumulation in the distal oesophagus Eur J Nucl Med Mol Imaging 32:990–992
O’Doherty MJ, Barrington S (2003) PET imaging in HIV infection. In: Valk P, Bailey DL, Townsend DW, Maisey MN, (eds). PET Basic science and clinical practice. Springer, London, chap 43, pp 741–752
Wohrer S, et al. (2006) FDG PET visualizes follicular lymphoma irrespective of grading Ann Oncol 17:780–784
Hany TF (2003) PET and PET/CT of the liver and pancreas In: Von Schulthess GK, (ed). Clinical molecular imaging. Williams & Wilkins, Philadelphia, chap 46, pp 334–340
Strauss LG (1996) FDG and false positive results: a major problem in the diagnosis of oncology patients Eur J Nucl Med 23:1309–1414
Cook GJR (2003) Artifacts and normal variants in whole body PET imaging. In Valk P, Bailey DL, Townsend DW, Maisey MN, (eds). PET Basic science and clinical practice. Springer, London, chap 24, pp 495–505
Wong WL, Saunders M (2002) Role of FDG PET in the assessment of indeterminate pulmonary lesions Clin Oncol 14:123–128
Van Westreenen HL, et al. (2003) Pitfalls of positive findings in staging oesophageal cancer with FDG PET Ann Surg Oncol 10:1100–1105
Kobori et al. (1999) Positron emission tomography of esophageal carcinoma using 11C-choline and 18 F-fluorodoexyglucose Cancer 86:638–1648
Jager PL, et al. (2001) Carbon-11 choline or FDG-PET for staging of oesophageal cancer? Eur J Nucl Med 28:1845–1849
Stein HJ, Brucher BLDM, Sendler A, Siewert JR (2001) Oesopahageal cancer: patient evaluation and pre-treatment staging Surg Oncol 10:103–111
Forshaw MJ, Gossage JA, Mason RC (2005) Neoadjuvant chemotherapy for oesophageal cancer: the need for accurate response prediction and evaluation Surgeon 3:6373–6382
Minsky BD, (2006) Primary combined modality therapy for oesophageal cancer Oncol 20:497–505
Vesselle et al. (2001) FLT PET imaging of non-small cell lung cancer: comparison to Ki67 proliferation index J Nucl Med 42:21
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wong, W.L., Chambers, R.J. Role of PET/PET CT in the staging and restaging of thoracic oesophageal cancer and gastro-oesophageal cancer: a literature review. Abdom Imaging 33, 183–190 (2008). https://doi.org/10.1007/s00261-007-9241-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-007-9241-1