Abstract
Purpose
To compare the safety of regadenoson, a selective agonist of A2A adenosine receptors, combined with low-level exercise, between subjects with mild/moderate chronic obstructive pulmonary disease (COPD) and asthma referred for myocardial perfusion imaging (MPI).
Methods
We studied 116 patients, of whom 67 had COPD and 49 asthma (62 % men, mean age 68.3 ± 11.3 years, range 31 – 87 years). Patient demographics, past medical history, medications, clinical symptoms during stress and changes in blood pressure (BP) and heart rate (HR) were evaluated.
Results
Both groups were comparable with regard to hypertension, dyslipidaemia, diabetes and medications with the exception of a higher rate of use of anticholinergics in patients with COPD and of antileukotrienes in asthmatics (58.2 % vs. 28.6 % and 1.5 % vs. 14.3 %, respectively; all p < 0.01). There was a higher incidence of dyspnoea in COPD patients and of headache and feeling hot in asthmatic patients (40.3 % vs. 22.4 %, 6 % vs. 18.4 % and 10.4 % vs. 26.5 %, respectively; all p < 0.05). Although there was no difference in the incidence of other adverse events, we observed a higher frequency in asthmatics of flushing, dry mouth, sweating and fatigue (1.5 % vs. 6.1 %, 14.9 % vs. 24.5 %, 0 % vs. 4.1 % and 37.3 % vs. 49 %, respectively). Adverse events were self-limiting, except in three patients who suffered persistent dyspnoea (2 of 67 COPD patients; 1 of 49 asthma patients) requiring theophylline administration. We observed no significant changes in BP among either group, but there was a tendency towards a higher increase in systolic BP in COPD patients following regadenoson administration (148.3 ± 27.6 vs. 154.6 ± 31.0 mmHg, p = 0.056).
Conclusion
This study showed a good safety profile in our series of COPD and asthma patients undergoing MPI. Regadenoson was well tolerated by all patients, with dyspnoea, headache and feeling hot showing differences between groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myocardial perfusion imaging (MPI) is a widely used technique to aid in the diagnosis and the management of patients with coronary disease. Dynamic exercise is the method of choice for producing coronary hyperaemia in patients who can achieve adequate exercise endpoints [1]. However, a substantial growth has been observed in the use of pharmacological stress testing. Pharmacological stress agents, such as adenosine, dipyridamole or regadenoson induce coronary artery hyperaemia [2] and are indicated in patients unable to undergo adequate exercise stress due to physical limitations or medical constraints [3]. Adenosine is a nonspecific agonist of all four known adenosine receptor subtypes (A1, A2A, A2B and A3) and coronary dilation is caused by interaction with the A2A receptor present in the vascular wall. The vasodilator properties of dipyridamole are based on increased levels of intrinsic adenosine.
However, patients with bronchoconstrictive disease, such as chronic obstructive pulmonary disease (COPD) or asthma, are at risk of adenosine-induced bronchoconstriction and respiratory compromise [4, 5]. This type of response is mediated through the A2B and A3 receptors. Dobutamine, the commonly used alternative pharmacological stress agent which is considered safe in these patients, is less effective at increasing coronary blood flow and is therefore considered an inferior test agent. Besides, it is associated with a high incidence of adverse events, needs beta-blockers to be stopped completely, and more time is needed for the examination protocol [6].
Regadenoson was approved in September 2010 by the European Medicines Agency (EMA) [7] as a pharmacological stress agent (administered as a single 0.4-mg intravenous bolus) indicated for radionuclide MPI in patients unable to undergo adequate exercise stress [8]. As it has a greater affinity for the A2A receptor and much lower affinity for the other adenosine receptor subtypes than adenosine or dipyridamole, the risk of bronchoconstriction in patients with COPD or asthma may be lower [9]. Several studies have been carried out in subjects with COPD and asthma [10–12]. These studies showed that the effect of regadenoson on pulmonary function is not clinically meaningfully different from the effect of placebo. However, these studies, which were clinical trials, often recruited patients without significant comorbidities and the real-life situation was not represented. Other studies have been performed in patients with a <50 % history of myocardial infarction, a <35 % history of arrhythmia and a <10 % history of COPD or asthma [10, 13, 14]. Moreover we are not aware of studies comparing the safety of regadenoson in COPD and asthmatic patients.
On the other hand, the combination of low-level treadmill exercise during infusion of the pharmacological stress agent is safe and results in a significant reduction in the adverse event profile of this agent, and the image quality is improved by decreasing hepatic and gut radiopharmaceutical uptake, which is common in pharmacological stress perfusion imaging [22, 23].
The objective of this study was to investigate the safety and tolerability of regadenoson in combination with low-level treadmill exercise in patients with COPD or asthma and to compare the adverse event profiles.
Materials and methods
We carried out a prospective study in 116 European patients (62 % men) with a mean age of 68.3 ± 11.3 years (range 31 – 87 years). The COPD group comprised 67 patients and the Asthma group 49 patients. All patients underwent a clinically indicated regadenoson stress test with low-level treadmill exercise.
This post-authorization observational study (protocol code CSG-REG-2010-01) has been classified by the Spanish Agency for Medicines and Health Products (AEMPS), and ethical approval was provided by the Regional Committee for Clinical Trials. All patients gave their signed written informed consent.
Inclusion and exclusion criteria
Regadenoson was prescribed by the responsible physician in charge of the patient’s myocardial perfusion test, independently of the study. The exclusion criteria were as follows: (1) severe COPD or asthma or active bronchoconstriction; (2) history of recent acute myocardial infarction, unstable angina or congestive heart failure; (3) history of sick sinus syndrome or greater than first degree AV block, except in patients who had a functional artificial pacemaker; (4) cor pulmonale; (5) current use of dipyridamole, aminophylline or theophylline; (6) long QT syndrome; (7) respiratory distress prior to study; and (8) intake of methylxanthine-containing foods and beverages prior to study.
Study design
This was an observational, comparative study designed to reflect routine clinical practice. Evaluations were carried out by monitoring the patient during the day of drug administration following the standard clinical practice of our department. Detailed clinical and procedure data were collected prospectively and stored in a database. Regadenoson (0.4 mg/5 ml; Lexiscan; Astellas Pharma US, Deerfield, IL) was administered as a peripheral intravenous rapid bolus (10 s) after 1.5 min of low-level exercise (2.7 – 3.5 km/h, 0 % grade) immediately followed by a 5-ml saline flush. MPI radiopharmaceutical (99mTc-tetrofosmin in 40 patients, or 99mTc-sestamibi in 76 patients) was injected approximately 30 s after starting regadenoson into the same catheter. The test ended after 4 min of exercise.
Patient demographics, past medical history, medications, clinical symptoms during stress, ECG changes and changes in blood pressure (BP) and heart rate (HR) were prospectively recorded. ECG monitoring continued during the procedure and for 4 min into recovery following regadenoson administration. Horizontal or down-sloping ST segment depression of ≥1 or up-sloping of ≥1.5 mm at 80 ms after the J point was considered positive. Symptoms during the stress procedure were recorded as reported by the patient. Patients were also asked how they felt. Adverse events were all effects that occurred during or after the stress test (up to 2 h, because the majority of adverse events for regadenoson occur during this time [12]).
Clinical characteristics
The baseline characteristics of the patients are shown in Table 1. There was a high prevalence of comorbidities including hypertension (71.6 %), cardiomyopathy (51.7 %), dyslipidaemia (50.9 %) and diabetes (38.8 %). The age range of both groups was very similar, but there was a significantly greater percentage of men with COPD than asthmatics (79.1 % vs. 36.7 %, respectively). They were comparable (p not significant) with regard to comorbidities and medication type with the exception of a higher rate of use of anticholinergics in COPD patients and of antileukotriene in asthmatics (58.2 % vs. 28.6 %; 1.5 % vs. 14.3 %, respectively, all p < 0.01). Although there was a higher presence of beta 2-agonist and corticosteroid use in COPD patients (58.2 % vs. 55.1 %; 61.2 % vs. 49 %, respectively), the difference was not statistically significant (Table 2).
Data analysis
Continuous data are expressed as means ± standard deviation (SD). Categorical variables were compared using the chi-squared test with Yates’ correction. Changes in BP (systolic and diastolic) and HR were compared using the Wilcoxon Z test for repeated measures and the Mann-Whitney U test. In all analyses, a p value lower than 0.05 was considered statistically significant. The odds ratio (with 95 % confidence interval) was used to compare effect sizes. Cohen’s d was used to compare the means using the following intervals: 0 – 0.09, negligible; 0.10 – 0.29, low effect size; 0.30 – 0.49, medium effect size; and ≥0.50, large effect size.
Results
No serious events occurred following the administration of regadenoson. The incidence of adverse events according to the type of airway disease is summarized in Table 3. Most events were mild, brief and self-limiting, except in three patients who suffered persistent dyspnoea (2 of 67 COPD patients, 1 of 49 asthma patients). Although bronchospasm did not occur in these patients, theophylline was administered and dyspnoea reversed after 2 – 4 min.
The most frequent adverse event occurring after regadenoson administration was fatigue (42.2 %), followed by dyspnoea (32.8 %), dizziness (25.9 %), dry mouth sensation (19 %) and feeling hot (17.2 %). No adverse events occurred in 16 patients after receiving regadenoson, with a higher proportion of COPD patients who reported no symptoms (COPD patients 22.4 %, asthma patients 6.1 %; p < 0.05; Fig. 1).
There was a higher incidence of dyspnoea in COPD patients and of headache and feeling hot in asthma patients (40.3 % vs. 22.4 %, 6 % vs. 18.4 %, 10.4 % vs. 26.5 %, respectively; all p < 0.05). Although there was no difference in the incidence of other adverse events, we observed a higher frequency in asthma patients of flushing (COPD patients 1.5 %, asthma patients 6.1 %), dry mouth (COPD patients 14.9 %, asthma patients 24.5 %), sweating (COPD patients 0 %, asthma patients 4.1 %), and fatigue (COPD patients 37.3 %, asthma patients 49 %). The effects soon reversed (except in the three patients with persistent dyspnoea previously mentioned), and they had a duration of 3 to 5 min and an onset between 0 and 10 s after regadenoson administration. Moreover, some patients had diarrhoea (2 of 67 COPD patients, 3 of 49 asthma patients) as mentioned in the package insert [8] and reported by other authors [13, 14, 25]. Onset was between 5 and 15 min after administration and was self-limiting. There was no significant difference in the incidence of the following adverse events between COPD and asthma patients after regadenoson: fatigue, dizziness, chest discomfort, nausea, dry mouth sensation, flushing and diarrhoea. Furthermore, we observed one patient with down-sloping ST depression in multiple leads (Fig. 2).
Baseline (a) and 4-min (b) ECG findings in an 80-year-old man with COPD. ST depression developed at minute 4 of low-level exercise, 2.5 min following regadenoson administration, in leads II, III, aVF, V5 and V6. The 99mTc-tetrofosmin myocardial perfusion study (c) shows a large reversible inferobasal and lateral defect. Coronary angiography (d, e) shows moderate lesions in the distal segment of the left coronary artery (d, arrow) and in the central segment of the left anterior descending artery (d, dotted arrow), in addition to a large collateral branch to the right coronary artery which is occluded, and diffuse disease of left circumflex artery with a long lesion in its central segment (e, arrows)
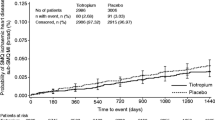
The patients’ BP and HR were recorded at baseline and 2 min after regadenoson administration (Table 4). There were no significant changes in systolic and diastolic BP in either group, although COPD patients tended to show an increase in systolic BP following regadenoson administration (148.3 ± 27.6 vs. 154.6 ± 31.0 mmHg). The mean HR increased significantly in both groups (p < 0.01; Fig. 3).
We determined whether the differences in these three variables were higher in COPD patients than in the asthma group. Although there were no significant differences, there was a trend towards a greater difference in systolic BP in COPD patients than in asthma patients. We also compared the differences in HR response after regadenoson administration between patients with and without diabetes mellitus but found no significant differences.
Discussion
COPD and asthma are conditions with a high and increasing prevalence. Adenosine package labelling carries a warning against its use in patients with these reactive airway diseases that require diagnostic procedures to evaluate myocardial ischaemia. This is due to the bronchoconstrictive effects that are mediated through the A2B and/or A3 receptors. The A2B receptor expressed on mast cells and smooth muscle cells has proinflammatory mediators and cytokines. A3 receptor expression is elevated on eosinophils in patients with asthma [15] and facilitates degranulation of mast cells. Furthermore, expression of the A1 adenosine receptor is elevated in the bronchial epithelium and smooth muscle of patients with bronchoconstrictive disease [16]. This receptor mediates bronchoconstriction induced by exogenous adenosine [17] which increases mucous secretion and activates neutrophils and monocytes via this receptor.
We report the results of a comparative study combining regadenoson with exercise for the purpose of MPI in patients with mild/moderate COPD and asthma. The Reg asthma trial [10] and the Reg COPD trial [11] were randomized controlled trials of selected patients with stable asthma or COPD and excluded patients with any chronic medical illness other than reactive airway disease. Our prospective study was designed to address the question focusing on the adverse events and haemodynamic response after regadenoson administration in consecutive unselected patients with many coexisting comorbidities along with either COPD or asthma. In this observational study, administration of a regadenoson bolus of 0.4 mg during low-level stress testing was safe and well tolerated. We found no significant differences between the adverse event profile of either group, except dyspnoea, headache and feeling hot. Thus, COPD patients had a higher incidence of dyspnoea, whereas asthma patients showed a higher incidence of headache and feeling hot. Moreover, other studies have shown a higher ratio of dyspnoea in patients with COPD than in asthmatics (61 % of COPD patients [11] vs. 34 % of asthma patients [10]). Al Jaroudi et al. [27] reported recently that patients with COPD have a higher frequency of shortness of breath than those with asthma. Our study showed a lower incidence of this adverse event (40.3 % among COPD patients vs. 22.4 % asthma patients), probably because the use of low-level treadmill reduces the adverse event profile. Thomas et al. [18] reported a similar incidence of dyspnoea (16 of 39 patients, 41 %) combining regadenoson with low-level exercise, but they did not include patients with bronchoconstrictive diseases.
Adverse events were self-limiting, except in three patients who suffered persistent dyspnoea (2 of 67 COPD patients, 1 of 49 asthma patients) requiring theophylline administration. However, clinically apparent bronchospasm (physical examination) did not develop in any patient. This effect and others, such as chest pain and flushing, may not be a result of A2A receptor activation only, but may also be mediated by sympathetic stimulation and increased ventilation [20]. Although no statistically significant differences were found in other symptoms, there was a higher, albeit nonsignificant, frequency of dry mouth sensation, dizziness, flushing and fatigue in asthma patients. There is an increased awareness of gastrointestinal adverse events, particularly diarrhoea [8]. In this regard, five patients had diarrhoea (4.3 %) in our study. We observed a lower incidence of this effect than found in the ASSUAGE trial (13 of 124 patients, 10.5 %). The difference was probably due to the lower prevalence of patients with chronic kidney disease in our study (n = 5), because these patients tend to show a higher baseline incidence of diarrhoea [22]. Nevertheless, Iskandrian et al. [23] were not able to find a clear reason for the higher incidence of diarrhoea in this patient group, and the greater half-life of regadenoson does not appear to fully explain this effect.
With regard to the haemodynamic effects of regadenoson, several studies have revealed that they include a transient decrease in BP [13, 19, 21]. Other studies have shown an increased mean systolic BP in asthma patients [10] and a slightly lower diastolic BP in COPD patients [11]. However, we found no significant changes in BP between rest conditions and after regadenoson administration, except a slightly increased systolic BP in COPD patients. As others have confirmed [10, 11], the mean HR increased significantly following regadenoson administration in both groups. This tachycardia is probably secondary to noradrenaline release through direct stimulation of the sympathetic nervous system [20]. However, the blunted HR response reported in COPD patients by others [24] was not observed in our series. Contrary to the findings of other studies [25, 26], we did not observe a blunting in the HR response after regadenoson administration in patients with diabetes mellitus compared with nondiabetics.
Study limitations
In the patient questionnaire, the intensity of symptoms was not classified as mild, moderate or severe, and thus the possible grading of effects is not reflected in our results. In addition, we do not have long-term follow-up of adverse events, although the majority of events related to regadenoson administration occurred during the 2-h period after administration [12], so we do not consider that relevant data were lost.
Conclusion
In this observational study of 116 unselected patients with mild/moderate COPD or asthma, regadenoson in combination with low-level treadmill exercise was safe and well tolerated. There were no significant differences between the adverse event profile of COPD and asthma patients, except dyspnoea, headache and feeling hot. No changes in BP were found, except a mild increase in systolic BP in COPD patients.
Our data are consistent with the hypothesis that selective A2A agonists do not cause bronchospasm in patients with mild/moderate bronchoconstrictive disease. However, we did not include subjects with severe lung disease. Further studies are still necessary in this group, because the results cannot necessarily be extrapolated to patients with severe lung disease.
References
Strauss HW, Miller DD, Wittry MD, Cerqueira MD, Garcia EV, Iskandrian AS, et al. Procedure guideline for myocardial perfusion imaging 3.3. J Nucl Med Technol. 2008;36:155–61.
McGeoch RJ, Oldroyd KG. Pharmacological options for inducing maximal hyperemia during studies of coronary physiology. Catheter Cardiovasc Interv. 2008;71:198–204.
Henzlova MJ, Cerqueira MD, Taillefer R, Mahmarian JJ, Yao SS. Quality Assurance Committee of the American Society of Nuclear Cardiology. Stress protocols and tracers. J Nucl Cardiol. 2009. doi:10.1007/s12350-009-9062-4.
Burkhart KK. Respiratory failure following adenosine administration. Am J Emerg Med. 1993;11:249–50.
Adenoscan. Package insert. 2008. Health Ministry. Spain.
Thompson RC. Regadenoson stress in patients with asthma and COPD: a breath of fresh air. J Nucl Cardiol. 2012;19(4):647–8.
European Medicines Agency. Assessment report for Rapiscan. London: European Medicines Agency; 2010. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Public_assessment_report/human/001176/WC500097103.pdf. Accessed 29 Jun 2013.
Lexiscan (Regadenoson) injection [package insert]. Deerfield: Astellas Pharma US, Inc; 2011.
Cerqueira MD. Advances in pharmacologic agents in imaging: new A2A receptor agonists. Curr Cardiol Rep. 2006;8:119–22.
Leaker BR, O’Connor B, Hansel TT, Barnes PJ, Meng L, Mathur VS, et al. Safety of regadenoson, an adenosine A2A receptor agonist for myocardial perfusion imaging, in mild asthma and moderate asthma patients: a randomized, double-blind, placebo-controlled trial. J Nucl Cardiol. 2008;15:329–36.
Thomas GS, Tammelin BR, Schiffman GL, Marquez R, Rice DL, Milikien D, et al. Safety of regadenoson, a selective adenosine A2A agonist, in patients with chronic obstructive pulmonary disease: a randomized, double-blind, placebo-controlled trial (RegCOPD trial). J Nucl Cardiol. 2008;15:319–28.
Prenner BM, Bukofzer S, Behm S, Feaheny K, McNutt BE. A randomized, double-blind, placebo-controlled study assessing the safety and tolerability of regadenoson in subjects with asthma or chronic obstructive pulmonary disease. J Nucl Cardiol. 2012;19(4):681–92.
Iskandrian AE, Bateman TM, Beladinelli L, Blackburn B, Cerqueira MD, Hendel RC. Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: results of the ADVANCE phase 3 multicenter international trial. J Nucl Cardiol. 2007;14(5):645–58.
Cerqueira MD, Nguyen P, Staehr S, Underwood R, Iskandrian AE; ADVANCE-MPI Trial Investigators. Effects of age, gender, obesity and diabetes on the efficacy and safety of the selective A2A agonist regadenoson versus adenosine in myocardial perfusion imaging: integrated ADVANCE-MPI trial results. J Am Coll Cardiol Imaging. 2008;1(3):307–16.
Walker BA, Jacobson MA, Knight DA, Salvatore CA, Weir T, Zhou D, et al. Adenosine A3 receptor expression and function in eosinophils. Am J Respir Cell Mol Biol. 1997;16(5):531–7.
Brown RA, Clarke GW, Ledbetter CL, Hurle MJ, Denyer JC, Simcock DE, et al. Elevated expression of adenosine A1 receptor in bronchial biopsy specimens from asthmatic subjects. Eur Respir J. 2008;31(2):311–9.
Bjorck T, Gustafsson LE, Dahlen SE. Isolated bronchi from asthmatics are hyperresponsive to adenosine, which apparently acts indirectly by liberation of leukotrienes and histamine. Am Rev Respir Dis. 1992;145(5):1087–91.
Thomas GS, Thompson RC, Miyamoto MI, Ip TK, Rice DL, Milikien D, et al. The RegEx trial: a randomized, double-blind, placebo- and active-controlled pilot study combining Regadenoson, a selective A2A adenosine agonist, with low-level exercise, in patients undergoing myocardial perfusion imaging. J Nucl Cardiol. 2009;16(1):63–72.
Kwon DH, Cerqueira MD, Young R, Houghtaling P, Lieber E, Menon V, et al. Lessons from regadenoson and low-level treadmill/regadenoson myocardial perfusion imaging: initial clinical experience in 1263 patients. J Nucl Cardiol. 2010;17(5):853–7.
Dhalla AK, Wong M, Wang W, Biaggioni I, Belardinelli L. Tachycardia caused by A2A adenosine receptor agonist is mediated by direct sympathoexcitation in awake rats. J Pharmacol Exp Ther. 2006;316(2):695–702.
Al Jaroudi WA, Iskandrian AE. Regadenoson: a new myocardial stress agent. J Am Coll Cardiol. 2009;54(13):1123–30.
Doukky R, Morales Demori R, Jain S, Kiriakos R, Mwansa V, Calvin JE. Attenuation of the side effect profile of regadenoson: a randomized double-blinded placebo-controlled study with aminophylline in patients undergoing myocardial perfusion imaging. “The ASSUAGE trial”. J Nucl Cardiol. 2012;19(3):448–57.
Iskandrian AE, Hage FG, Heo J. Use of regadenoson in end-stage renal disease. J Nucl Cardiol. 2013;20:182–4.
Husain Z, Palani G, Cabrera R, Karthikeyan AS, Dhanalakota S, Pathmanathan S, et al. Hemodynamic response, arrhythmic risk, and overall safety of regadenoson as a pharmacologic stress agent for myocardial perfusion imaging in chronic obstructive pulmonary disease and bronchial asthma patients. Int J Cardiovasc Imaging. 2012;28:1841–9.
Hage FG, Heo J, Franks B, Belardinelli L, Blackburn B, Wang W, et al. Differences in heart rate response to adenosine and regadenoson in patients with and without diabetes mellitus. Am Heart J. 2009;157(4):771–6.
Bengalorkar GM, Bhuvana K, Sarala N, Kumar TN. Regadenoson. J Postgrad Med. 2012;58:140–6.
Al Jaroudi WA, Alraies MC, Cerqueira MD, Jaber WA. Safety and tolerability of regadenoson in 514 SPECT MPI patients with and without coronary artery disease and submaximal exercise heart rate response. Eur J Nucl Med Mol Imaging. 2013;40:341–8.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Garcia, C.S., Heffernan, A.J., Sanchez de Mora, E. et al. Comparative study of the safety of regadenoson between patients with mild/moderate chronic obstructive pulmonary disease and asthma. Eur J Nucl Med Mol Imaging 41, 119–125 (2014). https://doi.org/10.1007/s00259-013-2493-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-013-2493-9