Abstract
Receptor targeting with radiolabelled peptides has become very important in nuclear medicine and oncology in the past few years. The overexpression of many peptide receptors in numerous cancers, compared to their relatively low density in physiological organs, represents the molecular basis for in vivo imaging and targeted radionuclide therapy with radiolabelled peptide-based probes. The prototypes are analogs of somatostatin which are routinely used in the clinic. More recent developments include somatostatin analogs with a broader receptor subtype profile or with antagonistic properties. Many other peptide families such as bombesin, cholecystokinin/gastrin, glucagon-like peptide-1 (GLP-1)/exendin, arginine-glycine-aspartic acid (RGD) etc. have been explored during the last few years and quite a number of potential radiolabelled probes have been derived from them. On the other hand, a variety of strategies and optimized protocols for efficient labelling of peptides with clinically relevant radionuclides such as 99mTc, M3+ radiometals (111In, 86/90Y, 177Lu, 67/68Ga), 64/67Cu, 18F or radioisotopes of iodine have been developed. The labelling approaches include direct labelling, the use of bifunctional chelators or prosthetic groups. The choice of the labelling approach is driven by the nature and the chemical properties of the radionuclide. Additionally, chemical strategies, including modification of the amino acid sequence and introduction of linkers/spacers with different characteristics, have been explored for the improvement of the overall performance of the radiopeptides, e.g. metabolic stability and pharmacokinetics. Herein, we discuss the development of peptides as radiopharmaceuticals starting from the choice of the labelling method and the conditions to the design and optimization of the peptide probe, as well as some recent developments, focusing on a selected list of peptide families, including somatostatin, bombesin, cholecystokinin/gastrin, GLP-1/exendin and RGD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tumour imaging through peptide receptor targeting began more than 20 years ago when radiolabelled somatostatin analogs were introduced into nuclear medicine for imaging of human tumours using a gamma camera [1]. A few years later targeted radionuclide therapy with somatostatin analogs followed. Ever since, the use of radiolabelled peptides in nuclear oncology has been an important topic with increasing interest.
The biological actions of the peptides are mediated upon binding with high affinity to specific receptors. Many of these receptors are massively overexpressed in numerous cancers, compared to their relatively low density in physiological organs [2]. This became the molecular basis for the development of radiolabelled peptides as radiopharmaceuticals for tumour imaging and therapy. After intravenous injection the radiopeptide will extravasate and bind to sites with high receptor density, e.g. tumour. Imaging and/or therapy follows depending on the radionuclide used. Table 1 summarizes the expression of peptide receptors on different tumours and lists the peptides currently being studied for receptor targeting. The radionuclides of interest for diagnostic and therapeutic applications along with their physical characteristics are given in Table 2.
The principle of the development of a radiolabelled peptide for successful receptor targeting can be summarized as follows: (1) Identification of the molecular target (receptor) using receptor autoradiography or immunohistochemistry. Receptor density, homogeneity and incidence are important factors in predicting successful in vivo targeting. (2) Synthesis of a peptide and/or its analogs. Usually, the design of a peptide is based on the structure of the endogenous ligand (natural peptide) which exhibits very high affinity for the corresponding receptor. The natural molecule is often modified in various ways in order to produce a metabolically stabilized peptide analog which preserves most of the biological activity of the original molecule. (3) Radiolabelling. The peptide is covalently coupled, often via a spacer, to a chelator which can complex radiometals or it carries a prosthetic group which can be labelled with radioiodine (*I) or 18F. Labelling protocols should allow very high labelling yield, radiochemical purity and specific activity and the radiopeptides should retain the affinity for the receptor. (4) In vitro characterization. Radioligand binding studies in cells or cell membrane preparations and other molecular biology studies allow for screening and evaluation of the radiopeptides, regarding their affinity for the receptor, their internalization rate, dissociation from the tumour cells etc. (5) In vivo evaluation. Biodistribution and imaging techniques are used with suitable animal models to evaluate the pharmacological behaviour and pharmacokinetics of the radiopeptides. Many aspects should be taken into consideration for further development, such as the accumulation in target and non-target tissues, the clearance from the body, the excretory pathway and the in vivo stability of the radiopeptide. (6) The radiolabelled peptides which successfully went through all tests, after toxicological studies and established preparation, may enter clinical studies in humans.
From the design of a new peptide until the use in the clinic is a long way and from a large number of developed radiopeptides only very few fulfil the criteria of a radiopharmaceutical for clinical application. In the following sections, we discuss methods for radiolabelling of peptides with clinically relevant radionuclides and developments of radiopeptide analogs, based on a selected list of peptide families, including somatostatin, bombesin, cholecystokinin/gastrin, glucagon-like peptide-1 (GLP-1)/exendin and arginine-glycine-aspartic acid (RGD).
Radionuclides and radiolabelling
With the exception of 18F and *I the other clinically most relevant radionuclides are metals (Table 2). Peptide-based radiopharmaceuticals labelled with radiometals can be divided into four parts (Fig. 1): (1) the peptide which acts as a target-specific vector, (2) the spacer, (3) the bifunctional chelator (BFC) and (4) the radiometal. The BFC consists of a chelating moiety to complex the radiometal and a functional group for the covalent attachment of the peptide or the spacer. While the nature of the vector molecule is determined by the cellular target (i.e. cell surface receptor), the spacer is dependent on the pharmacokinetic requirements of the pharmaceutical as it often influences its hydrophilicity and improves the pharmacokinetics. The spacer can also act as a separator between the BFC and the peptide to prevent steric influence of the chelator on the binding affinity of the receptor targeting part of the pharmaceutical. The chemical nature of the radiometal determines the choice of the BFC.
Labelling with 99mTc
99mTc is the “workhorse” in diagnostic nuclear medicine, given the fact that about 80% of the radiopharmaceuticals used in the clinic are still 99mTc based. The reasons for this pole position are the very favourable nuclear physical characteristics (Table 2), the price and the ready availability. 99mTc is eluted from the generator in physiological saline as 99mTcO4 − (VII). The chemically rather inert 99mTc(VII) has to be reduced to a lower oxidation state (I–V) with a reducing agent, such as SnCl2, in the presence of suitable ligands.
Labelling of peptides with 99mTc is usually performed with the so-called post-conjugation labelling approach. This approach is widely used because a single kit formulation is possible. The strategy consists of (1) the preparation of the bifunctional chelator-peptide conjugate, (2) addition of the reagents needed for 99mTc labelling such as buffer, reducing agent and supporting ligand, including the conjugate, in one vial, (3) lyophilization and (4) addition of the generator eluate (99mTcO4 −) to the vial. Bifunctional chelators with very high affinity and selectivity to Tc in any of the oxidation states I–V are needed since high specific activities have to be achieved. In addition, the 99mTc-labelled BFC-peptide conjugate must be thermodynamically stable and kinetically inert to survive physiological conditions. A variety of BFCs have been evaluated upon conjugation to peptides in order to achieve this goal. They are of the type N2S2 diamidedithiols, N3S triamidethiols, N4 tetraamines [3–5] or hydrazinonicotinic acid (HYNIC) [6–11]. Relevant chelator structures are shown in Fig. 2. Most of the labelling reactions are performed at 80–100°C [with the exception of N4 which reacts at room temperature (RT)]. 99mTc forms mainly penta- or hexa-coordinated complexes containing TcO3+ (N2S2 and N3S) or TcO2 + (N4) core. Especially in the case of HYNIC one or more coligands with donors such as amine, carboxylate or hydroxyl are needed to complete the coordination sphere of the Tc(V)-HYNIC complex. These coligands usually are ethylenediamine-N,N′-diacetic acid (EDDA), N-(tri(hydroxymethyl)methyl)glycine (tricine), nicotinic acid and such combinations (Fig. 2). Labelling takes place at RT when one coligand is used while using a combination of coligands (EDDA/HYNIC or tricine/HYNIC) demands elevated temperature (100°C). Another labelling approach is based on organometallic Tc carbonyl complexes which allow high stability and high specific activity due to the d6 electron configuration of the Tc(I) metal centre. The active species in this process is the aquo ion 99mTc(CO)3(H2O)3 + which exchanges water molecules with mono-, di- and tridentate chelators to form stable complexes [12]. Tridentate chelators such as picolylamine diacetic acid (PADA) or (NαHis)Ac (Fig. 2) have shown to form stable complexes and are superior to bidentate such as the His in the His-peptide conjugate, where one water molecule remains in the coordination sphere.
Labelling with 3+ and 2+ radiometals (111In, 86/90Y, 177Lu, 67/68Ga and 64/67Cu)
Most of the clinically relevant radiometals are hard Lewis acids (111In, 86/90Y, 177Lu, 67/68Ga), with 3+ as their major oxidation state in aqueous solution, forming stable complexes with hard Lewis bases. 64/67Cu is a 2+ intermediate Lewis acid. Polydentate BFCs with donor groups containing oxygen, nitrogen and sulphur such as carboxylate, phosphonate, hydroxamate and amine, but also softer functional groups such as phenolate and thiol groups, are used for the formation of stable complexes in vivo [13, 14].
In3+, Y3+ and Lu3+ form insoluble colloidal hydroxides at pH > 5 and therefore the labelling with the corresponding radiometals takes place at pH 4–5. Ga3+ can hydrolyse to insoluble colloidal Ga(OH)3 at pH around 5 if its concentration exceeds nanomolar level, while at physiological pH its solubility is high due to the almost exclusive formation of [Ga(OH)4]− ions. Labelling with 68Ga takes place usually at pH 2–4; however, labelling at higher pH has also been reported, depending on the chelator [15]. Cu2+aq is stable in a pH range of 4–9 and labelling is usually performed in the pH range of 5–8, depending on the chelator [16]. In general, the BFC has to form metal complexes with high thermodynamic stability and more important kinetic inertness at 5 < pH < 7.5. These physicochemical properties are needed because the loss of radiometal in vivo would cause undesirable side effects by accumulation of radioactivity in non-target organs, e.g. 177Lu3+ or 90Y3+ are “bone seekers” and would cause bone marrow damage. Moreover, as the BFC is often competing with natural chelators present in the bloodstream, like transferrin or serum albumin, the thermodynamic stability constant (log K) of the (radio)metal-BFC complex should be higher than the log K of the complex the (radio)metal forms with the natural chelators, unless the (radio)metal-BFC complex is kinetically robust.
Acyclic bifunctional chelators based on the structure of diethylenetriaminepentaacetic acid (DTPA) (Fig. 3) have favourable labelling kinetics for most radiometals. DTPA is usually coupled to peptides using one carboxylic acid group forming an amide bond. Bifunctional versions of DTPA in which the carbon backbone is substituted by a functional group for coupling to a peptide, such as CHX-A′′-DTPA (Fig. 3) have also been developed [17]. This may have an additional advantage as all five carboxylate groups are preserved for metal binding. Nevertheless, these acyclic BFCs often lack kinetic stability. DTPA is an ideal chelator for 111In but is not suitable for other radiometals because of in vivo instability.
Labelling with radiometals is preferably performed with BFCs based on a macrocyclic core. The most popular one is the 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid (DOTA) (Fig. 3) which forms stable complexes with many (radio)metals (e.g. In3+, Y3+, Lu3+, Ga3+). The slow formation kinetics, compared to acyclic chelators, can be overcome by heating [18] or the use of microwave technology [19]. The direct coupling of a peptide by one acetic acid function of DOTA leads to a conversion of this group to an amide offering the carbonyl oxygen for potential complexation of the radiometal [20]. This may lead to a decrease in thermodynamic stability compared to the acid. A strategy to prevent this potential loss of complexation functionality is the introduction of an additional coupling site on a modified acetic acid arm via an alkylation step maintaining the full-fledged functionalities of DOTA, such as in the case of 1-(1-carboxy-3-carboxypropyl)-1,4,7,10-tetraazacyclododecane-4,7,10-triacetic acid (DOTAGA) (Fig. 3) [21].
The macrocyclic chelator 1,4,7-triazacyclononane-1,4,7-triacetic acid (NOTA) (Fig. 3) has a smaller cavity size than DOTA and is known to be an excellent chelator for the small ion Ga3+ which fits into the cavity, but also for In3+. NOTA has been functionalized via a glutaric acid arm (NODAGA) [22] or via benzyl-isothiocyanato (2-(p-SCN-Bz)-NOTA) [23] for coupling to peptides (Fig. 3) via amide or thiourea formation, respectively. NOTA is labelled with 68Ga at RT which is an additional advantage in regard to DOTA which demands elevated temperatures.
Many DOTA and 1,4,8,11-tetraazacyclotetradecane, 1,4,8,11,tetraacetic acid (TETA) (Fig. 3) derivatives have been used for 64/67Cu labelling of different peptides. However, these complexes suffer from in vivo instability. Attachment of two carboxymethyl pendant arms to cross-bridged (CB)-cyclam leads to CB-TE2A (Fig. 3) which ensures complete envelopment of a six-coordinate Cu2+. BFCs of CB-TE2A coupled to peptides and labelled with 64Cu showed superiority compared to more conventional chelators, such as DOTA and TETA [24, 25]. NOTA was also shown to form complexes with 64Cu with very high in vivo stability [23, 26]. Recently, NODAGA was shown to be an excellent chelator for 64Cu and potentially superior to CB-TE2A as labelling can be performed at RT within 10 min [25, 27]. Another class of BFC for 64/67Cu2+ has been synthesized on the basis of the sarcophagine (3,6,10,13,16,19-hexaazabicyclo [6.6.6] icosane, also called Sar), resulting in very stable in vivo complexes. Carboxylate and amino derivatives of Sar such as SarAr and AmBaSar (Fig. 3) have been developed for conjugation to amine or carboxyl residues on peptides through amide bonds [28, 29]. Labelling of these chelators is performed under very mild conditions (25–37°C, 30 min) with very high specific activity.
Radioiodination
Methods for radioiodination of peptides can be divided in two major groups: (1) direct labelling and (2) indirect labelling via prosthetic groups.
Direct labelling
Iodination can be performed directly by “iodo-deprotonation”. The reaction consists of the electrophilic substitution of an aromatic proton by electrophilic radioiodine (*I+) and it takes place in an amino acid residue of the peptide which affords strong (but also weak) electron donating groups (e.g. -OH, -NH2 or -OR, -SR, -NHCOR). Peptides with Tyr and His residues can be directly radioiodinated on the side chain of the amino acid [1, 30–32]. Because the radioactive iodine is usually available as sodium iodide, which is not an appropriate electrophile, the electrophilic ion *I+ can be generated with the use of oxidants such as Chloramine T (sodium tosylchloroamide), Iodogen® (1,3,4,6-tetrachloro-3α,6α-diphenylglycoluril) or IodoBeads® (polymer-bound Chloramine T) (Fig. 4). The radioiodination takes place under mild conditions (aqueous buffers, pH 7–8). Attention should be paid to the reaction conditions (temperature, time etc.) to avoid oxidative damage of the peptide, especially in the case where Chloramine T is used, and a reducing agent should be added to stop the reaction. The use of reaction vials coated with Iodogen or the use of polymer supported iodobeads where no reducing agent is needed and the reaction can be stopped by physical separation of the aqueous reaction media from the Iodogen or IodoBeads is highly attractive for the radioiodination of peptides.
A very mild alternative to chemical methods is the formation of the active iodine species by an enzyme-catalysed process. Peroxidates, such as lactoperoxidase, can produce electrophilic *I+ in the presence of Na*I and H2O2 and allow radioiodination under mild oxidizing conditions. However, the enzymatic activity is very sensitive to reaction conditions and the labelling yield is low due to self-iodination of the enzyme.
Indirect labelling
If direct labelling is not possible, acylation reactions via pre-labelled prosthetic groups like the Bolton-Hunter reagent (N-succinimidyl-3-(4-hydroxy,5-[*I]iodophenyl)-propionate) (Fig. 4) are being used. The N-hydroxy-succinimidyl ester (NHS) group is reacted with an amine of the peptide to form a stable amide bond. A disadvantage of Bolton-Hunter reagent is the low in vivo stability. In addition reagents like N-succinimidyl-5-[*I]iodo-3-pyridine carboxylate (SIPC) or N-succinimidyl-3-[*I]iodobenzoate (SIB) (Fig. 4) were developed which show higher stability with regard to in vivo deiodination as they lack phenolic aromatic groups [33]. Other valuable radioiodinated precursors have also been developed; however, the attachment of a bulky prosthetic group in a small peptide often significantly influences the binding affinity for the receptor and the in vivo pharmacokinetics of the radiolabelled peptide.
Fluorination
18F is the predominantly used radionuclide in positron emission tomography (PET). Direct labelling using nucleophilic 18F-F− generally requires harsh conditions, such as elevated temperatures and strong base, which may not be compatible with biomolecules, such as peptides. Therefore, fluorination of peptides is often performed using 18F-labelled prosthetic groups under mild conditions through fluoroalkylation, fluoroacylation and fluoroamidation on -NH2, -SH, -OH or -COOH groups. Selected prosthetic groups are shown in Fig. 5. Among several prosthetic groups developed the N-succinimidyl 4-[18F]fluorobenzoate ([18F]SFB) is widely used since it can be produced in good yields and it has high in vivo stability [34, 35]. However, the synthesis involves at least three steps. More chemoselective reactions can be performed with prosthetic groups having 18F-labelled aldehydes. For example 4-[18F]fluorobenzaldehyde ([18F]FBA) reacts with aminooxy or hydrazine groups to form 18F-labelled oxime or hydrazone derivatives, while the synthesis of the prosthetic group is usually a single-step fluorination process [36]. Alternatively, silicon-based building blocks have been coupled to the N terminus of peptides for one-step no-carrier-added (n.c.a.) 18F labelling by nucleophilic displacement of leaving groups, such as alkoxy, hydroxy or hydride [37], or by using the less lipophilic benzonitrile moiety 18F-for-+N(CH3)3 substitution can be used for one-step 18F labelling [38]. Direct [18F]fluoroglycosylation of peptides has been performed by reacting 2-[18F]fluoro-2-deoxyglucose ([18F]FDG) n.c.a. with aminooxy-peptides [39]. Better chemoselectivity can be achieved using prosthetic groups for conjugation to thiol groups, as -SH groups are not as abundant as -COOH and -NH2 groups in peptides. Maleimide derivatives labelled with 18F are used for this purpose, such as 4-[18F]fluorobenzamido-ethylmaleimide ([18F]FBEM) and 4-[18F]fluorobenzaldehyde-butylmaleimide oxime ([18F]FBBO) [40]. A maleimide derivative of FDG ([18F]FDG-maleimidehexyloxime: [18F]FDGMHO) has also been used and it can be produced in one step from available [18F]FDG [41]. More recently, another chemoselective approach has been introduced using the 1,3-dipolar Huisgen cycloaddition of alkynes to azides, known as “click chemistry”. An 18F-alkyne or 18F-azide prosthetic group reacts with an azido- or alkyne-functionalized peptide, respectively, under very mild conditions [42–44]. Many prosthetic groups, such as [18F]fluoroalkynes, [18F]fluoroethylazide, 18F-glycosyl azide (Fig. 5) and others bearing one of the two functionalities, have been tested and 18F labelling via click chemistry is an open field. Recently, the peptide-chelator conjugate approach was applied for 18F labelling. The chelator NOTA coupled to a peptide was labelled with the complex Al18F2+ formed by the addition of AlCl3 in acetate buffer in target water [45]. For efficient fluorination it is important to choose the most appropriate prosthetic group for each individual peptide, based on its chemical and biological characteristics, as fluorination often demands multi-step labelling procedures, deprotection steps and purification of the final product.
Development of peptide-based probes
Somatostatin analogs
The somatostatin family consists of two cyclic disulphide-containing peptide hormones, one with 14 amino acids (SS-14, Table 3) and one with 28 amino acids (SS-28). Somatostatin inhibits the secretion of peptide hormones, biogenic amines and neurotransmitters from a variety of neuroendocrine tumours and, in some cases, reduces tumour growth. The biological actions of somatostatin are mediated by five G protein-coupled receptor subtypes (sst1–sst5) located on the plasma membrane of the target cell. Somatostatin receptors are overexpressed in a majority of neuroendocrine tumours [2] and among all subtypes the sst2 was found to be predominantly expressed [46].
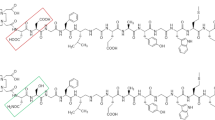
Somatostatin itself turned out to be unsuitable for in vivo use such as treatment of neuroendocrine tumours or development of radiolabelled probes for tumour localization, as it has a short plasma half-life of about 3 min. Therefore, somatostatin analogs more resistant to enzymatic degradation than somatostatin itself were developed by various modifications of the natural molecule. Introduction of D-amino acids and shortening of the molecule to the bioactive core sequence resulted in eight amino acid-containing somatostatin analogs, such as octreotide (OC). Table 3 shows the most well studied analogs and some of the most recent developments. The first commercially available agent was [111In-DTPA0]octreotide for somatostatin receptor scintigraphy. However, this radiopeptide has moderate binding affinity to sst2 and DTPA is not a suitable chelator for β− emitters such as 90Y and 177Lu. For these radiometals, DTPA has been replaced by DOTA, which is a better choice as it forms thermodynamically and kinetically stable complexes with 3+ radiometals. The replacement of Phe3 in octreotide by Tyr3 (TOC) leads to an improved sst2 affinity, while the C-terminal introduction of Thr (TATE) for Thr(ol) (TOC) resulted in a further improvement of the sst2 affinity [47]. The somatostatin conjugates DOTA-TOC and DOTA-TATE, labelled with 111In and 68Ga for single photon emission computed tomography (SPECT) and PET imaging, respectively, and with 90Y and 177Lu for targeted radionuclide therapy, are routinely used in many hospitals, especially in Europe [48–50]. 99mTc-labelled octreotide analogs have also been developed and clinically evaluated for SPECT imaging, such as HYNIC-TOC [51], which is commercially available in some European countries, HYNIC-TATE and N4-TATE [49]. 18F-labelled octreotate coupled to carbohydrates in order to improve pharmacokinetics has shown to be suitable for clinical application [36]. Recently, other approaches for 18F labelling have been proposed, including “click radiochemistry” [44] and the use of the chelator NOTA [45]. Finally, 64Cu-labelled octreotide analogs have also been developed [52].
All of the above analogs have high affinity for sst2. However, radiolabelled somatostatin-based probes with a broader receptor subtype affinity profile may target a broader spectrum of tumours but also they may increase the net tumour uptake, given the presence of several receptor subtypes on the same tumour cell. Modifications of the octreotide at position 3 by introducing the unnatural amino acids 1-naphthyl-alanine (1-NaI) and benzothienyl-alanine (BzThi) led to the analogs NOC and BOC, respectively [53]. The same modifications on the C-terminally Thr octreotide led to the analogs NOC-ATE and BOC-ATE, respectively [54]. All these analogs showed affinity to sst2, sst3 and sst5. Interestingly, it was seen that a change of radiometal may profoundly influence receptor affinity, as all Ga-DOTA conjugates of these analogs have improved sst2 affinity compared to the corresponding Y/Lu/In-DOTA conjugates [55]. Currently, modification of the physicochemical properties of somatostatin analogs has led to the development of bicyclic somatostatin-based analogs with affinity to sst2, sst3 and sst5, such as the AM3 (Table 3) [56]. These molecules have fast background clearance and therefore high tumour to non-tumour ratios and look ideal for imaging with short-lived radionuclides, such as 68Ga.
Pan-somatostatin radiopeptides with high affinity for all receptor subtypes have also been developed. The first such peptide, KE108, was modified by replacing Tyr as a prosthetic group for iodination NH2-terminally [57] by DOTA, resulting in the analog KE88 (Table 3) [58]. 111In-KE88 was able to bind with high affinity to all five receptor subtypes (sst1–sst5) but was efficiently internalized only in sst3. Consequently, only the sst3-expressing tumours had high and persistent tumour uptake, whereas the sst2-expressing tumours showed low uptake and fast washout in vivo. It has been observed that some established somatostatin agonists, in particular those belonging to the pan-somatostatin family, were biased ligands, stimulating only a subset of receptor activity. KE108 and pasireotide (SOM230), both established as full and potent sst2 agonists on growth hormone release or in the adenylate cyclase assay, were found to be sst2 antagonists in calcium assays and extracellular signal-regulated kinase phosphorylation assays [59].
All somatostatin analogs mentioned above, with the exception of the biased ligands, are agonists which induce receptor internalization. Until recently there has been a consensus to develop compounds with good internalization properties, as this was accepted to be an important mechanism for their tumour uptake, accumulation and retention in vivo. However, high-affinity sst2- and sst3-selective somatostatin antagonists (sst2-ANT and sst3-ODN-8, respectively) can perform as well as or even better than agonists in terms of in vivo uptake in corresponding tumour xenografts, despite their poor internalization [60]. This unexpected phenomenon initiated the development of more potent sst2 antagonists inverting the chirality at Cys2 and amino acid at position 1 as well as by introducing amide bond-rich moieties, such as carbamoyl functionalities [61]. A recent study on the newly developed sst2 antagonist LM3 (Table 3) demonstrated that the chelator and the radiometal make the difference in the affinity and also tumour uptake and retention of radiolabelled somatostatin antagonists [27]. This study clearly showed the sensitivity of the antagonists to N-terminal modifications, a result that was not found to the same extent with the octreotide-type agonists, as well as the high and persistent tumour uptake of the antagonists. The first clinical study of somatostatin antagonists confirmed the preclinical data as it showed higher tumour uptake of the antagonist 111In-DOTA-sst2-ANT compared to the agonist 111In-DTPA-OC and improved tumour to background contrast, in particular tumour to kidney [62].
Bombesin analogs
Bombesin (BN) is an amphibian 14-amino acid analog of the 27-amino acid mammalian regulatory gastrin-releasing peptide (GRP). Four bombesin receptor subtypes are known, among them three mammalian: BB1 (neuromedin B receptor), BB2 [GRP receptor (GRPR)] and BB3 (orphan bombesin receptor) and one amphibian: BB4. Bombesin has high affinity for the human GRPR, a G protein-coupled receptor which is overexpressed by a variety of cancers, including prostate, breast, pancreas, gastrointestinal and small cell lung cancer [2], making radiolabelled bombesin analogs attractive candidates for targeting GRPR. The natural BN has a plasma half-life of about 2–3 min and therefore more resistant analogs have been developed. Table 4 shows the sequence of BN and selectively some of these analogs.
Radiolabelled BN analogs are based on the full-length BN(1–14) but mostly on the C-terminal 7–14 amino acid sequence [BN(7–14)] or on BN(6–14), known to be critical for receptor binding and more stable in vivo than the full-length. These analogs are usually modified at position 3 by replacing Arg by Lys for coupling of a suitable chelator for labelling and at positions 11 (Gly), 13 (Leu) and 14 (Met) using unnatural amino acids, like norleucine (Nle14). The first proof of concept of in vivo GRPR targeting with BN analogs was reported by Van de Wiele et al. using a 99mTc-labelled BN(7–14) conjugate (99mTc-RP527) in breast and prostate cancer patients [63]. Later on, a series of 99mTc-labelled N4-functionalized BN analogs based on BN(6–14) (demobesin 1) [3], or on the full-length BN (demobesin 3 and 4) and BN(7–14) (demobesin 5 and 6) [4], were synthesized. Among them 99mTc-demobesin 4 was shownd to be a very promising agonist which entered clinical trials (http://clinicaltrials.gov/show/NCT00989105). However, side-by-side comparison of 99mTc-demobesin 4 with 99mTc-demobesin 1, a potent BN antagonist with similar affinity for GRPR, showed superiority of the antagonist in terms of high and prolonged tumour retention in GRPR-positive xenografts and rapid background clearance [64].
The effect of the spacer between the chelator and the pharmacophoric group was studied in a series of 99mTc-N3S-X-BN(7–14) derivatives (N3S = dimethylglycyl-L-seryl-L-cysteinylglycinamide), with different lengths of the hydrocarbon spacer, X = 0 (no spacer), 3 (β-Ala), 5 (5-Ava = 5-aminovaleric acid), 8 (8-Aoc = 8-aminooctanoic acid) or 11 (11-Aun = 11-aminoundecanoic acid) carbon atoms [65]. The derivatives with 3, 5 and 8 carbon atoms demonstrated better binding characteristics in vitro, while in vivo as the chain length (X) increased the extent of the clearance of the radiopeptides by the urinary pathway and the uptake in the pancreas (GRPR-positive organ) decreased. The derivative with a 3 carbon spacer (β-Ala) exhibited the highest pancreas uptake. Other 99mTc-labelled BN analogs have been developed using HYNIC as a chelator and full-length BN [7] or BN(7–14) with β-Ala as a spacer [8, 66]. β-Ala-β-Ala has also been used in (NαHis)Ac-functionalized BN(7–14) modified at position 13 (Cha = cyclohexylalanine) and 14 (Nle) (BBS-38 and BBS-42, respectively) for labelling with 99mTc(CO)3 [67, 68]. These 99mTc(CO)3-conjugated analogs showed high lipophilicity and unfavourable hepatobiliary excretion. Introduction of hydrophilic carbohydrated linker moieties, such as amino acid linkers containing lysine or propargylglycine residues, substantially improved the biodistribution profile [69]. The introduction of polar linkers with different charge, such as the positively charged β3-homolysine (β3hLys), the uncharged β3-homoserine (β3hSer) and the single negatively charged β3-homoglutamic acid (β3hGlu), significantly influenced the biodistribution profile with better performance for the β3hGlu, which exhibited higher tumour uptake and tumour to background ratios compared to the β-Ala-β-Ala derivative [70].
The influence of the different linking groups has also been evaluated in a series of 111In-DOTA-X-BN(7–14) derivatives, with X = 8-Aoc (8-aminooctanoic acid), 5-Ads (5-amino-3-oxapentyl-succinamic acid), 8-Aos (8-amino-3,6-dioxaoctyl-succinamic acid), p-aminobenzoic acid, Gly-p-aminobenzoic acid and Gly-p-aminomethylbenzoic acid [71]. The In-metallated 8-Aoc and Gly-p-aminomethylbenzoic acid derivatives had the highest affinity followed by the p-aminobenzoic acid and Gly-p-aminobenzoic acid derivatives. The derivatives with an aromatic (aminobenzoic) group demonstrated in vivo higher uptake in the gastrointestinal tract but also higher tumour retention. BN(7–14) has been coupled via 8-Aoc to the chelators DOTA, NOTA and CB-TE2A for labelling with 64Cu [26, 72] where the superiority of 64Cu-NOTA-Aoc-BN(7–14) and 64Cu-CB-TE2A-BM(7–14) over 64Cu-DOTA-Aoc-BN(7–14) in terms of in vivo performance was demonstrated due to higher in vivo stability of the 64Cu-NOTA and 64Cu-CB-TE2A complexes. Recently, BN(7–14) was labelled with 64Cu conjugated to the chelator SarAr [28].
Slightly modified analogs (Thi13 instead of Phe13) of the universal ligand (D-Tyr6,β-Ala11,Phe13,Nle14-NH2) BN(6–14) [73] bind with high affinity to all bombesin receptor subtypes and were coupled to DTPA and DOTA using γ-aminobutyric acid as a spacer. The resulting pan-bombesin analogs BZH1 (for labelling with 111In) and BZH2 (for labelling with 177Lu and 90Y), respectively, exhibited high and specific uptake in GRPR-positive tissue (pancreas) and tumour [74]. Later on, using PEG2 as a spacer the resulting pan-bombesin analog BZ3 was studied with 68Ga in animal models [75] and in patients [76].
The first radiolabelled BN analog for therapeutic application is 177Lu-AMBA developed by Bracco. It is based on the BN(7–14) conjugated to DOTA via Gly-4-aminobenzoyl spacer for targeting BB1 and BB2 receptors in human cancers [77, 78]. This compound showed very promising results in preclinical models and was studied in clinical settings (phase I) [79]. BN(7–14) conjugated to DOTA via PEG4 spacer led to the analog DOTA-PESIN which showed high tumour uptake and retention and favourable in vivo profile labelled with 67Ga and 177Lu [80]. Recently, DOTA-PESIN was used for therapeutic purposes labelled with 177Lu versus the α emitter 213Bi in a prostate carcinoma xenograft model [81], where it was shown that α therapy was more efficacious than β therapy. Interestingly, 213Bi-DOTA-PESIN exhibited a better safety profile when compared to 213Bi-AMBA [81]. 111In-AMBA has been evaluated side by side with the newly developed bombesin antagonist 111In-RM1, a statin analog (Table 4) sharing the same spacer and chelator as AMBA [82]. Despite the lower affinity of 111In-RM1 compared to 111In-AMBA, the antagonist showed superior GRPR-targeting properties. Replacement of the spacer on RM1 by the positively charged 4-amino-1-carboxymethyl-piperidine resulted in a new derivative, RM2, with improved affinity [83]. The same statin analog with a PEG4 spacer (AR) was coupled to four different chelators, DOTA, N4, NODAGA and CB-TE2A for labelling with 111In, 99mTc, 68Ga and 64Cu, respectively, showing that spacer and chelate were important determinants of the overall performance of the radiopeptide [84]. The encouraging performance of these radiopeptides, especially of 64Cu-CB-TE2A-AR, led to a preliminary study of this probe in a limited number of patients [85].
Finally, 18F-labelled full tetradecapeptide sequence, 18F-FB-[Lys3]BN, showed better receptor binding and pharmacokinetic characteristics than the BN(7–14) analog 18F-FB-Aca-BBN(7–14) (Aca = aminocaproic acid) [35]. In a series of 18F-labelled statin analogs it was shown that a negatively charged bombesin derivative in which L-cysteic acid was used as the spacer had much higher tumour uptake than the corresponding positively charged analog in which Arg was used [37, 38]. Among all analogs, the 18F-BAY 86–4367 (Table 3) containing two L-cysteic moieties [86] showed the most favourable preclinical data and it is being considered for clinical evaluation.
Cholecystokinin/gastrin analogs
Cholecystokinin (CCK) and gastrin are peptide hormones that perform several regulatory functions in the gastrointestinal tract and in the nervous system. Three types of CCK receptors are known. The CCK1 (or CCK-A) which has limited expression in humans, the CCK2 (or CCK-B or gastrin receptor) which has high affinity for gastrin and CCK and is frequently expressed in human tumours, including medullary thyroid carcinomas, small cell lung cancer, stromal ovarian cancers, astrocytomas and some gastroenteropancreatic cancers [2] and the CCK2i4sv receptor, the splice variant of the CCK2 receptor, which is expressed in human colorectal cancers and pancreatic cancers, but not in normal colorectal mucosa. All CCK receptors belong to the G protein-coupled receptor family.
The radiolabelled CCK/gastrin analogs are mostly based on CCK8 and minigastrin. CCK8 is the C-terminal octapeptide amide fragment of the biologically active CCK in non-sulphated form (CCK8) or in sulphated form (sCCK8) (Table 5). Minigastrin (MG) is a C-terminal truncated non-sulphated form having 13 amino acid residues (Table 5). The presence of the C-terminal sequence Trp-Met-Asp-Phe-NH2 is crucial for receptor binding, where the Met residue may be replaced by Leu or Nle [30, 87]. Sulphation of the Tyr7 moiety in CCK8 appears to be necessary for high affinity to either CCK1 or CCK2 receptors [88], while non-sulphated CCK8 analogs showed high specificity towards CCK2 [89]. Replacement of Met at positions 3 and 6 by Nle in order to prevent oxidation [89] and also replacement of the Tyr(OSO3H) moiety by a robust isosteric sulphonate, Phe(p-CH2SO3H) [90] showed increased plasma stability and high affinity to CCK2. 99mTc-labelled sCCK8 and CCK8 showed that the uptake of the sulphated analog, in both CCK1 and CCK2 receptor-expressing tumours in mice, was significantly higher than that of the non-sulphated analog [91].
Radioiodinated analogs of minigastrin and CCK8 showed that minigastrin analogs had greater uptake in receptor-positive tissues but also extremely high kidney uptake whereas CCK8 analogs exhibited low kidney uptake but also low tumour uptake [92]. 111In-DTPA-derivatives of MG and D-Glu1-minigastrin [replacement of the first amino acid Leu1 with D-Glu1 results in an analog containing six glutamic acid chains (MG0)] showed that 111In-DTPA-MG0 displayed improved metabolic stability and better pharmacokinetics (fast blood clearance, low background radioactivity) than 111In-DTPA-MG in tumour xenografts and humans [93]. The high kidney uptake was shown to be mediated through a receptor that recognized the pentaglutamate sequence, as injection of oligo-glutamic acid chains with five or more amino acids significantly reduced kidney uptake without influence on the tumour uptake [94].
In a series of 111In-DOTA-minigastrin analogs with reduced number of glutamic acid residues (reduced negative charge) it was shown that reducing the number of glutamates improved binding affinity, significantly reduced kidney uptake and increased tumour to kidney ratio [95]. However, the absolute tumour uptake and the metabolic stability of the analog in which the glutamate sequence has been removed (MG11) were lower compared to MG0. In the same study it was shown that replacement of Met by norleucine (Nle), isoleucine (Ile), methionine-sulphoxide [Met(O)] or methionine-sulphone [Met(O2)] resulted in significant decrease of receptor affinity. From a library of 111In-labelled DTPA and DOTA conjugates based on the C-terminal structure of minigastrin [96] it was shown that removal of the pentaglutamate sequence resulted in a strong reduction in kidney uptake but also in tumour uptake. Replacement of the pentaglutamate with a hexahistidine tag resulted in a similar reduction in kidney and tumour uptake, while a di-histidine (H2) analog (H2-Met) showed the best results in terms of tumour to kidney ratios. Replacement of Met in H2-Met by Nle (H2-Nle) led to reduction of receptor affinity and also tumour uptake in vivo.
99mTc-labelled N4-derivatized minigastrin analogs, such as N4-D-Glu1-minigastrin (demogastrin 1) or N4-Gly0-D-Glu1-minigastrin (demogastrin 2) showed that the Gly spacer resulted in favourable biodistribution profile in terms of tumour to non-tumour ratios [97]. 99mTc-Demogastrin 2 appeared to be a more promising diagnostic tool in preliminary clinical studies than 111In-DOTA-CCK8 and 111In-DOTA-MG11 [98]. MG0 and MG11 were labelled with 99mTc using EDDA/HYNIC [99]. Both showed similar tumour uptake in vivo, with 99mTc-EDDA/HYNIC-MG11 showing lower kidney uptake, but lower metabolic stability as well. Cyclic variants of MG11 have been developed in an attempt to improve metabolic stability [100]. D-Glu1 was incorporated in the peptide through the γ carboxylic acid group (γ-D-Glu1), while Gly9 was replaced by D-Lys9 (cyclo-MG1) and also Met11 was replaced by Nle11 (cyclo-MG2). The peptides were derivatized with HYNIC on the N terminus and labelled with 99mTc. Cyclization reduced the affinity for the receptor, even though tumour uptake of the cyclic analogs was higher than the corresponding linear analog. The overall biodistribution of 99mTc-HYNIC-cyclo-MG1 was similar to that of 99mTc-HYNIC-MG11. Improvement of the in vivo performance and metabolic stability was attempted by dimerization of MG11 (MGD5, Table 5) [101] which conjugated to DOTA and labelled with 111In showed an increase in binding affinity and tumour uptake in vivo.
Recently, DOTA conjugates of MG11 have been developed by introducing hydrophilic but uncharged spacers of different lengths, such as PEG or D-amino acids (D-Ser or D-Gln) [102]. Whereas increasing the number of PEG or D-Ser had only very limited effect on serum stability, the number of D-Gln residues played an important role and the length of the spacer determined metabolic stability as this was significantly improving from (D-Gln)2 to (D-Gln)6 (PP-F10). 111In-DOTA analogs with nonionic D-Gln spacers exhibited highly improved pharmacokinetics. In a very interesting collaboration within the COST Action on Targeted Radionuclide Therapy (BM0607) 12 DOTA-conjugated analogs, developed by different groups (including analogs discussed above such as MG0, MG11, cyclo-MG1, MGD5 and others), have been evaluated side by side for their affinity, metabolic stability and in vivo profile [103–105]. Even though all analogs showed very high affinity and internalization rates in vitro [103] significant differences were found in their metabolic stability and biodistribution. Replacement of the hexaglutamate of the MG0 analog by hexa-D-Glu (PP-F11) showed to be the most stable analog in tissue homogenates, while a major cleavage site of all minigastrin derivatives between Asp and Phe-NH2 at the C-terminal end was found [104]. Based on these comparative studies optimal analogs were the linear minigastrin analog with six D-Glu residues (PP-F11), the divalent analog MGD5 and the cyclic peptide cyclo-MG1, combining high tumour uptake with low kidney retention [105].
GLP-1/exendin analogs
GLP-1 is one of the most important glucose-dependent insulin secretagogues released mainly from the small intestine in response to nutrient intake. The corresponding receptor (GLP-1R) is a member of the G protein-coupled receptor family and is mainly expressed in the pancreatic islet cells, the intestine, lung, kidney, breast and the brainstem. GLP-1R was found to be overexpressed in insulinomas, an usually benign insulin-secreting neuroendocrine tumour of the pancreas [106]. Also, gastrinomas, phaeochromocytomas, paragangliomas and medullary thyroid carcinomas express GLP-1R but with lower density and/or incidence.
The natural ligand GLP-1 (30 amino acids) has a half-life of less than 2 min. Exendin-4 (H-His1-Gly2-Glu3-Gly4-Thr5-Phe6-Thr7-Ser8-Asp9-Leu10-Ser11-Lys12-Gln13-Met14-Glu15-Glu16-Glu17-Ala18-Val19-Arg20-Leu21-Phe22-Ile23-Glu24-Trp25-Leu26-Lys27-Asn28-Gly29-Gly30-Pro31-Ser32-Ser33-Gly34-Ala35-Pro36-Pro37-Pro38-Ser39-NH2) is a metabolically resistant naturally occurring peptide identified in the saliva of the Gila monster and it shares 53% homology with the human GLP-1. Exendin-3 is also a highly stable 39-amino acid peptide isolated from the Mexican beaded lizard, which differs by only two amino acid residues (H-His1-Ser2-Asp3-Gly4-…-Ser39-NH2) near the amino terminus.
The first radiolabelled exendin analog was 125I-[Y39]exendin-4 where Ser39 has been replaced by Tyr39 for iodination and it was developed as a radioligand to study and characterize exendin receptors [107]. Preclinical data on iodinated 125I-GLP-1(7–36)amide and on the metabolically more stable 125I-exendin-3 demonstrated specific targeting in insulinoma tumours and high uptake in the pancreas, as insulinoma cells derive from pancreatic β cells, but also in the kidneys due to the renal elimination of the radiopeptides [32]. The low radioiodination efficiency of exendin-3 and the low stability of GLP-1 were limiting factors for clinical use. Later on, exendin-4 was modified C-terminally with Lys40-NH2, whereby the Lys side chain was coupled to DTPA using aminohexanoic acid (Ahx) as a spacer [Lys40(Ahx-DTPA)NH2]-exendin-4 and it was labelled with 111In [108, 109]. In vivo evaluation of 111In-DTPA-exendin-4 in tumour-bearing transgenic Rip1Tag2 mice (tumours of the pancreatic β cells with extremely high density of GLP-1R) showed remarkably high uptake in the tumour and excellent tumour visualization on SPECT images, corroborating the high potential of the probe to specifically localize GLP-1R-positive lesions within the pancreas [108]. High uptake was also found in lungs and pancreas, whereas the high kidney uptake was shown to be not mediated by GLP-1R. Based on the Auger electrons of 111In, 111In-DTPA-exendin-4 was evaluated for its therapeutic efficiency in the same tumour model [110]. A dose-dependent reduction of the tumour volume was found without significant acute organ toxicity. Late toxic side effects were detected in the kidneys after injection of intermediate to high doses. The therapeutic effect was due to increased apoptosis and necrosis of the tumour cells and also decreased proliferation.
The first trial of the corresponding 111In-DOTA-exendin-4 conjugate in patients showed promising results in the noninvasive localization of insulinomas [111]. SPECT/CT imaging successfully detected pancreatic and ectopic insulinomas, which had previously not been identified with certainty using conventional methods, and showed to be highly beneficial as tumours were localized in situ using a gamma probe [112]. Additionally, 111In-DTPA-exendin-4 scan seems to be an option to distinguish between benign and malignant insulinomas as there are indications that malignant insulinomas often lack GLP-1R and therefore a negative scan may potentially indicate malignant insulinoma [113].
To overcome the drawbacks of 111In-DTPA/DOTA-exendin-4 related to the use of 111In, such as the relatively high radiation burden for the patient, 99mTc- and 68Ga-labelled exendin conjugates were developed, such as [Lys40(Ahx-HYNIC-99mTc/EDDA)NH2]-exendin-4, [Lys40(Ahx-DOTA-68Ga)NH2]-exendin-4 [11] and [Lys40(Ahx-DOTA-68Ga)NH2]-exendin-3 [114]. An in vivo side-by-side evaluation of 99mTc-HYNIC-exendin-4, 68Ga-DOTA-exendin-4 and 111In-DOTA-exendin-4 showed that 68Ga- and 111In-labelled conjugates have very similar behaviour and tumour uptake, while the 99mTc-labelled conjugate showed significantly lower tumour uptake but lower uptake in the non-targeted organs as well [11]. As a consequence tumour to background ratios and image quality were high for all three probes and the high kidney uptake could be reduced using polyglutamic acid, gelofusine or a combination of the two [11]. 99mTc-HYNIC-exendin-4 had the lowest estimated effective dose and this probe is currently under clinical evaluation [115, 116]. The biodistribution of 111In-DTPA-exendin-3 is identical to the biodistribution of 111In-DTPA-exendin-4 [114], while side-by-side comparison of 111In-DTPA-exendin-3 with 68Ga-DOTA-exendin-3 showed that the 68Ga-labelled conjugate has significantly lower tumour uptake compared to the 111In-labelled conjugate [114].
Overexpression of GLP-1R on native pancreatic β cells provides the possibility of monitoring the β cell mass (BCM) during the course of diabetes development and antidiabetic treatment. Furthermore, the method might be used for monitoring of islet cell graft survival after transplantation. It has been shown that the uptake of 111In-DTPA-exendin-3 correlates with the BCM in a linear manner in rats with alloxan-induced diabetes [117]. Ex vivo autoradiography using 64Cu-labelled [Lys40(Ahx-DOTA-64Cu)NH2]-exendin-4, along with anti-insulin immunohistochemistry, showed specific binding of the 64Cu-DOTA-exendin-4 to pancreatic islet cells and the potentiality of these probes for quantitative in vivo measurement of BCM using PET [118]. In a proof-of-principle study, the new analog Cys40-VS-DOTA-exendin-4 (VS = vinyl sulphone) labelled with 64Cu detected transplanted human islets in the liver of mice [119]. Recently, 111In-DTPA-exendin-4 was used to follow β cell viability of an islet transplantation into the forearm of a human patient [120]. One year after the transplantation, focal accumulation of the probe was observed in planar images.
Finally, a conformationally constrained GLP-1 analog via lactam bridges between the residues 18–22 and 30–34, namely EM3106B, has been recently developed bearing a C-terminal Cys residue allowing labelling with 18F through the maleimide-based prosthetic group, N-2-(4-18F-fluorobenzamido)ethylmaleimide (18F-FBEM) [40]. The probe showed specific and high uptake in GLP-1R-positive tumours and low uptake in tumours with low GLP-1R expression.
RGD analogs
Integrins are a family of heterodimeric transmembrane glycoproteins which are involved in a wide range of cell-extracellular matrix interactions and cell-cell interactions. At least 24 distinct integrins are formed by a combination of 18 α and 8 β subunits, such as ανβ3, ανβ5, α5β1 etc. Among them ανβ3 has a crucial role in the regulation of tumour growth and metastasis as it is highly expressed on activated and proliferating endothelial cells during tumour angiogenesis and metastasis [121]. The ανβ3 integrin binds to Arg-Gly-Asp (RGD)-containing components of the extracellular matrix like vitronectin and fibronectin. Thus, a variety of linear and mostly cyclic RGD-based probes have been developed for monitoring expression of ανβ3 in vivo [122].
Development of radiolabelled RGD-based probes has focused on cyclic pentapeptides based on the lead structure cyclo(Arg-Gly-Asp-D-Phe-Val) (c(RGDfV)). Often D-Phe has been replaced by D-Tyr to facilitate radioiodination [c(RGDyV)] and Val by Lys [c(RGDfK) or c(RGDyK)] for coupling of a chelator or a prosthetic group. First in vivo evaluation of radioiodinated RGD peptides in xenografts showed receptor-specific tumour uptake but also unfavourable hepatobiliary elimination [31]. Improvement of the pharmacokinetics was achieved by glycosylation (conjugation with sugar moieties). The introduction of galactose-based sugar amino acid to the ε-NH2 group of a Lys residue led to the development of Galacto-RGD [Galacto-c(RGDfK)] which, labelled with 18F ([18F]Galacto-RGD), has been successfully used in patients [123, 124]. [18F]-AH111585 (also called [18F]fluciclatide), a RGD-containing probe based on an aminooxy-functionalized double-bridged peptide [125], has been evaluated in a phase I clinical study on patients with metastasized breast cancer [126] and is currently in clinical trial (http://clinicaltrials.gov/show/NCT00918281, GE Healthcare). [18F]RGD-K5, a click chemistry-derived RGD-containing peptidomimetic probe, has been evaluated as well in a small number of patients with breast cancer [127] and is in a phase II clinical trial (http://clinicaltrials.gov/show/NCT00988936, Siemens Molecular Imaging).
The radiolabelling with 18F is relatively complex (especially for [18F]Galacto-RGD) which makes large-scale clinical studies challenging. Thus, the clinical use of RGD peptides would clearly be enhanced by probes that are less complex to prepare, such as RGD-chelator conjugates for labelling with radiometals. DOTA-conjugated RGD peptides have been developed and labelled with 64Cu [64Cu-DOTA-c(RGDyK)] [128] 111In and 68Ga [111In/68Ga-DOTA-c(RGDfK)] [129]. More recent developments are based on RGD conjugates with the chelator NOTA for 68Ga labelling, such as 68Ga-NOTA-Bz-SCN-c(RGDyK) [130] or 68Ga-NODAGA-c(RGDfK) [15, 25]. The facile preparation of 68Ga-NODAGA-c(RGDfK) makes it an attractive alternative to 18F-labelled RGD peptides. NODAGA has been used as well for labelling with 64Cu along with CB-TE2A. Both 64Cu-NODAGA-c(RGDfK) and 64Cu-CB-TE2A-c(RGDfK) showed improved characteristics compared to the corresponding 64Cu-DOTA-c(RGDfK) [25]. An interesting finding of this study was that delayed imaging with 64Cu-CB-TE2A-c(RGDfK) or 64Cu-NODAGA-c(RGDfK) dramatically improves image contrast, since these compounds are only slowly cleared from ανβ3 integrin-expressing tumours while their clearance from normal tissues is much faster. These data indicated that imaging at later times than feasible with 18F or 68Ga may be advantageous for visualization of ανβ3 integrin-expressing tumours.
Optimization in the development of RGD-based probes includes PEGylation (conjugation of polyethylene glycol) for improvement of the pharmacokinetics and multimerization (more than one RGD moiety in the same targeting molecule) for improvement of the binding affinity for the ανβ3 receptor and prolonged retention in the target. PEGylated 64Cu-DOTA-PEG-c(RGDyK) (PEG, MW = 3,400) showed the same uptake and retention in the tumour compared to 64Cu-DOTA-c(RGDyK), but lower activity in the liver and small intestine and also faster blood clearance [131]. However, the same PEG spacer led to slower blood pool clearance and higher accumulation in the liver and kidneys for [18F]FB-PEG-c(RGDyK) ([18F]FB = [18F]fluorobenzoyl) compared to [18F]FB-c(RGDyK); nevertheless, tumour uptake and retention were higher for [18F]FB-PEG-c(RGDyK) [132]. Dimerization via glutamic acid ([18F]FB-E-[c(RGDyK)]2) increased tumour uptake and prolonged tumour retention compared to [18F]FB-c(RGDyK) [133, 134]. Additionally, the dimer was predominantly excreted through the kidneys, whereas the monomer primarily through the biliary route. Initial studies with the dimer E-[c(RGDfK)]2 conjugated to DOTA (for labelling with 111In and 90Y) and HYNIC (for labelling with 99mTc) showed the potentiality of these probes for imaging but for therapy as well [135]. Polyvalency has a profound effect on the receptor binding affinity and in vivo kinetics. 68Ga- and 111In-labelled DOTA conjugates of mono-, di- and tetramers, E-c(RGDfK), E-[c(RGDfK)]2 and E{E-[c(RGDfK)]2}2, respectively, showed that affinity but also in vivo tumour uptake increases by increasing the RGD moieties [136]. The 64Cu-labelled DOTA-conjugated octamer E(E{E-[c(RGDyK)]2}2)2 also had higher affinity and tumour uptake than the corresponding tetramer E{E-[c(RGDyK)]2}2 [137]. Unfortunately, higher uptake is often found in different organs such as kidney and muscles by increasing the number of RGD moieties. However, different linkers can influence the targeting properties. For example, 68Ga-NOTA-conjugated dimers with 3 Gly (G3) and PEG4 linkers (NOTA-E[PEG4-c(RGDfK)]2 and NOTA-E[G3-c(RGDfK)]2) showed to have higher affinity than the corresponding no-linker dimers and they also exhibited significantly higher tumour uptake and tumour to normal tissue ratios [138]. Even though multimerization does not guarantee improvement on tumour to background ratios, a favourable balance between the number of binding moieties and the size of the molecule as well as the use of an appropriate linker may significantly improve the overall performance of the RGD probe.
Finally, a 99mTc-labelled RGD containing a double-bridged peptide, 99mTc-NC100692, introduced by GE Healthcare, has been evaluated in breast cancer patients [139]. Recently, the PEGylated dimer [18F]FP-PEG3-E-[c(RGDyK)]2, (18F-FP = 2-18F-fluoropropionic acid) has received exploratory investigative new drug application (eIND) approval from the US Food and Drug Administration (FDA). This probe has shown tumour to background ratios similar to [18F]Galacto-RGD but higher tumour uptake [140]. To our knowledge, at the moment many centres in Europe are planning to start clinical trials with 68Ga-NODAGA-RGD.
Summary
The clinical success of somatostatin receptor imaging (SPECT and PET) and of targeted radionuclide therapy with somatostatin analogs opened new horizons in nuclear medicine and oncology. At the same time, the discovery of new receptor targets overexpressed in human tumours led to the design of new peptide analogs with high affinity for these receptors. This, along with the progress in radiochemistry, including the development of bifunctional chelators, advances in the production of radionuclides, optimization of radiolabelling protocols etc., resulted in a wide variety of radiopeptide candidates for tumour receptor targeting. Although many of these probes showed very promising results in preclinical evaluation only a limited number of them have found the way to the clinic so far. However, the acquired knowledge and the continuous research guarantee the development of new peptide-based radiopharmaceuticals for clinical application.
References
Krenning EP, Bakker WH, Breeman WA, Koper JW, Kooij PP, Ausema L, et al. Localisation of endocrine-related tumours with radioiodinated analogue of somatostatin. Lancet 1989;1:242–4.
Reubi JC. Peptide receptors as molecular targets for cancer diagnosis and therapy. Endocr Rev 2003;24:389–427.
Nock B, Nikolopoulou A, Chiotellis E, Loudos G, Maintas D, Reubi JC, et al. [99mTc]Demobesin 1, a novel potent bombesin analogue for GRP receptor-targeted tumour imaging. Eur J Nucl Med Mol Imaging 2003;30:247–58.
Nock BA, Nikolopoulou A, Galanis A, Cordopatis P, Waser B, Reubi JC, et al. Potent bombesin-like peptides for GRP-receptor targeting of tumors with 99mTc: a preclinical study. J Med Chem 2005;48:100–10.
Abiraj K, Mansi R, Tamma ML, Forrer F, Cescato R, Reubi JC, et al. Tetraamine-derived bifunctional chelators for technetium-99m labelling: synthesis, bioconjugation and evaluation as targeted SPECT imaging probes for GRP-receptor-positive tumours. Chemistry 2010;16:2115–24.
Bangard M, Béhé M, Guhlke S, Otte R, Bender H, Maecke HR, et al. Detection of somatostatin receptor-positive tumours using the new 99mTc-tricine-HYNIC-D-Phe1-Tyr3-octreotide: first results in patients and comparison with 111In-DTPA-D-Phe1-octreotide. Eur J Nucl Med 2000;27:628–37.
Ferro-Flores G, Arteaga de Murphy C, Rodriguez-Cortés J, Pedraza-López M, Ramírez-Iglesias MT. Preparation and evaluation of 99mTc-EDDA/HYNIC-[Lys 3]-bombesin for imaging gastrin-releasing peptide receptor-positive tumours. Nucl Med Commun 2006;27:371–6.
Shi J, Jia B, Liu Z, Yang Z, Yu Z, Chen K, et al. 99mTc-labeled bombesin(7–14)NH2 with favorable properties for SPECT imaging of colon cancer. Bioconjug Chem 2008;19:1170–8.
von Guggenberg E, Behe M, Behr TM, Saurer M, Seppi T, Decristoforo C. 99mTc-labeling and in vitro and in vivo evaluation of HYNIC- and (Nalpha-His)acetic acid-modified [D-Glu1]-minigastrin. Bioconjug Chem 2004;15:864–71.
Decristoforo C, Mather SJ, Cholewinski W, Donnemiller E, Riccabona G, Moncayo R. 99mTc-EDDA/HYNIC-TOC: a new 99mTc-labelled radiopharmaceutical for imaging somatostatin receptor-positive tumours; first clinical results and intra-patient comparison with 111In-labelled octreotide derivatives. Eur J Nucl Med 2000;27:1318–25.
Wild D, Wicki A, Mansi R, Béhé M, Keil B, Bernhardt P, et al. Exendin-4-based radiopharmaceuticals for glucagonlike peptide-1 receptor PET/CT and SPECT/CT. J Nucl Med 2010;51:1059–67.
Alberto R. The chemistry of technetium–water complexes within the manganese triad: challenges and perspectives. Eur J Inorg Chem 2009:21–31.
Wadas TJ, Wong EH, Weisman GR, Anderson CJ. Coordinating radiometals of copper, gallium, indium, yttrium, and zirconium for PET and SPECT imaging of disease. Chem Rev 2010;110:2858–902.
Fani M, Good S, Maecke HR. Radiometals (non-Tc, non-Re) and bifunctional labeling chemistry. In: Vértes A, Nagy S, Klencsár Z, Lovas RG, Rösch F, editors. Handbook of nuclear chemistry. Heidelberg: Springer; 2011. p. 2143–78.
Knetsch PA, Petrik M, Griessinger CM, Rangger C, Fani M, Kesenheimer C, et al. [68Ga]NODAGA-RGD for imaging alphavbeta3 integrin expression. Eur J Nucl Med Mol Imaging 2011;38:1303–12.
Wadas TJ, Anderson CJ. Radiolabeling of TETA- and CB-TE2A-conjugated peptides with copper-64. Nat Protoc 2006;1:3062–8.
Clifford T, Boswell CA, Biddlecombe GB, Lewis JS, Brechbiel MW. Validation of a novel CHX-A″ derivative suitable for peptide conjugation: small animal PET/CT imaging using yttrium-86-CHX-A″-octreotide. J Med Chem 2006;49:4297–304.
Breeman WA, De Jong M, Visser TJ, Erion JL, Krenning EP. Optimising conditions for radiolabelling of DOTA-peptides with 90Y, 111In and 177Lu at high specific activities. Eur J Nucl Med Mol Imaging 2003;30:917–20.
Velikyan I, Beyer GJ, Långström B. Microwave-supported preparation of (68)Ga bioconjugates with high specific radioactivity. Bioconjug Chem 2004;15:554–60.
Heppeler A, Froidevaux S, Mäcke HR, Jermann E, Behe M, Powell P, et al. Radiometal-labelled macrocyclic chelator-derivatised somatostatin analogue with superb tumour-targeting properties and potential for receptor-mediated internal radiotherapy. Chem Eur J 1999;5:1974–81.
Eisenwiener KP, Powell P, Mäcke HR. A convenient synthesis of novel bifunctional prochelators for coupling to bioactive peptides for radiometal labelling. Bioorg Med Chem Lett 2000;10:2133–5.
Eisenwiener KP, Prata MI, Buschmann I, Zhang HW, Santos AC, Wenger S, et al. NODAGATOC, a new chelator-coupled somatostatin analogue labeled with [67/68Ga] and [111In] for SPECT, PET, and targeted therapeutic applications of somatostatin receptor (hsst2) expressing tumors. Bioconjug Chem 2002;13:530–41.
Liu Z, Li ZB, Cao Q, Liu S, Wang F, Chen X. Small-animal PET of tumors with (64)Cu-labeled RGD-bombesin heterodimer. J Nucl Med 2009;50:1168–77.
Sprague JE, Peng Y, Sun X, Weisman GR, Wong EH, Achilefu S, et al. Preparation and biological evaluation of copper-64-labeled tyr3-octreotate using a cross-bridged macrocyclic chelator. Clin Cancer Res 2004;10:8674–82.
Dumont RA, Deininger F, Haubner R, Maecke HR, Weber WA, Fani M. Novel (64)Cu- and (68)Ga-labeled RGD conjugates show improved PET imaging of alpha(nu)beta(3) integrin expression and facile radiosynthesis. J Nucl Med 2011;52:1276–84.
Prasanphanich AF, Nanda PK, Rold TL, Ma L, Lewis MR, Garrison JC, et al. [64Cu-NOTA-8-Aoc-BBN(7–14)NH2] targeting vector for positron-emission tomography imaging of gastrin-releasing peptide receptor-expressing tissues. Proc Natl Acad Sci U S A 2007;104:12462–7.
Fani M, Del Pozzo L, Abiraj K, Mansi R, Tamma ML, Cescato R, et al. PET of somatostatin receptor-positive tumors using 64Cu- and 68Ga-somatostatin antagonists: the chelate makes the difference. J Nucl Med 2011;52:1110–8.
Lears KA, Ferdani R, Liang K, Zheleznyak A, Andrews R, Sherman CD, et al. In vitro and in vivo evaluation of 64Cu-labeled SarAr-bombesin analogs in gastrin-releasing peptide receptor-expressing prostate cancer. J Nucl Med 2011;52:470–7.
Cai H, Fissekis J, Conti PS. Synthesis of a novel bifunctional chelator AmBaSar based on sarcophagine for peptide conjugation and (64)Cu radiolabelling. Dalton Trans 2009;27:5395–400.
Behr TM, Jenner N, Béhé M, Angerstein C, Gratz S, Raue F, et al. Radiolabeled peptides for targeting cholecystokinin-B/gastrin receptor-expressing tumors. J Nucl Med 1999;40:1029–44.
Haubner R, Wester HJ, Reuning U, Senekowitsch-Schmidtke R, Diefenbach B, Kessler H, et al. Radiolabeled alpha(v)beta3 integrin antagonists: a new class of tracers for tumor targeting. J Nucl Med 1999;40:1061–71.
Gotthardt M, Fischer M, Naeher I, Holz JB, Jungclas H, Fritsch HW, et al. Use of the incretin hormone glucagon-like peptide-1 (GLP-1) for the detection of insulinomas: initial experimental results. Eur J Nucl Med Mol Imaging 2002;29:597–606.
Garg S, Garg PK, Zalutsky MR. N-succinimidyl 5-(trialkylstannyl)-3-pyridinecarboxylates: a new class of reagents for protein radioiodination. Bioconjug Chem 1991;2:50–6.
Vaidyanathan G, Zalutsky MR. Synthesis of N-succinimidyl 4-[18F]fluorobenzoate, an agent for labeling proteins and peptides with 18F. Nat Protoc 2006;1:1655–61.
Zhang X, Cai W, Cao F, Schreibmann E, Wu Y, Wu JC, et al. 18F-labeled bombesin analogs for targeting GRP receptor-expressing prostate cancer. J Nucl Med 2006;47:492–501.
Schottelius M, Poethko T, Herz M, Reubi JC, Kessler H, Schwaiger M, et al. First (18)F-labeled tracer suitable for routine clinical imaging of sst receptor-expressing tumors using positron emission tomography. Clin Cancer Res 2004;10:3593–606.
Höhne A, Mu L, Honer M, Schubiger PA, Ametamey SM, Graham K, et al. Synthesis, 18F-labeling, and in vitro and in vivo studies of bombesin peptides modified with silicon-based building blocks. Bioconjug Chem 2008;19:1871–9.
Mu L, Honer M, Becaud J, Martic M, Schubiger PA, Ametamey SM, et al. In vitro and in vivo characterization of novel 18F-labeled bombesin analogues for targeting GRPR-positive tumors. Bioconjug Chem 2010;21:1864–71.
Hultsch C, Schottelius M, Auernheimer J, Alke A, Wester HJ. (18)F-Fluoroglucosylation of peptides, exemplified on cyclo(RGDfK). Eur J Nucl Med Mol Imaging 2009;36:1469–74.
Gao H, Niu G, Yang M, Quan Q, Ma Y, Murage EN, et al. PET of insulinoma using (18)F-FBEM-EM3106B, a new GLP-1 analogue. Mol Pharm 2011;8:1775–82.
Wuest F, Berndt M, Bergmann R, van den Hoff J, Pietzsch J. Synthesis and application of [18F]FDG-maleimidehexyloxime ([18F]FDG-MHO): a [18F]FDG-based prosthetic group for the chemoselective 18F-labeling of peptides and proteins. Bioconjug Chem 2008;19:1202–10.
Hausner SH, Marik J, Gagnon MK, Sutcliffe JL. In vivo positron emission tomography (PET) imaging with an alphavbeta6 specific peptide radiolabeled using 18F-“click” chemistry: evaluation and comparison with the corresponding 4-[18F]fluorobenzoyl- and 2-[18F]fluoropropionyl-peptides. J Med Chem 2008;51:5901–4.
Glaser M, Arstad E. “Click labeling” with 2-[18f]fluoroethylazide for positron emission tomography. Bioconjug Chem 2007;18:989–93.
Leyton J, Iddon L, Perumal M, Indrevoll B, Glaser M, Robins E, et al. Targeting somatostatin receptors: preclinical evaluation of novel 18F-fluoroethyltriazole-Tyr3-octreotate analogs for PET. J Nucl Med 2011;52:1441–8.
Laverman P, McBride WJ, Sharkey RM, Eek A, Joosten L, Oyen WJ, et al. A novel facile method of labeling octreotide with (18)F-fluorine. J Nucl Med 2010;51:454–61.
Reubi JC, Waser B, Schaer JC, Laissue JA. Somatostatin receptor sst1-sst5 expression in normal and neoplastic human tissues using receptor autoradiography with subtype-selective ligands. Eur J Nucl Med 2001;28:836–46.
Reubi JC, Schar JC, Waser B, Wenger S, Heppeler A, Schmitt JS, et al. Affinity profiles for human somatostatin receptor subtypes SST1-SST5 of somatostatin radiotracers selected for scintigraphic and radiotherapeutic use. Eur J Nucl Med 2000;27:273–82.
Maecke HR, Reubi JC. Somatostatin receptors as targets for nuclear medicine imaging and radionuclide treatment. J Nucl Med 2011;52:841–4.
Rufini V, Calcagni ML, Baum RP. Imaging of neuroendocrine tumors. Semin Nucl Med 2006;36:228–47.
Nicolas G, Giovacchini G, Müller-Brand J, Forrer F. Targeted radiotherapy with radiolabeled somatostatin analogs. Endocrinol Metab Clin North Am 2011;40:187–204.
Hubalewska-Dydejczyk A, Fröss-Baron K, Mikolajczak R, Maecke HR, Huszno B, Pach D, et al. 99mTc-EDDA/HYNIC-octreotate scintigraphy, an efficient method for the detection and staging of carcinoid tumours: results of 3 years’ experience. Eur J Nucl Med Mol Imaging 2006;33:1123–33.
Shokeen M, Anderson CJ. Molecular imaging of cancer with copper-64 radiopharmaceuticals and positron emission tomography (PET). Acc Chem Res 2009;42:832–41.
Ginj M, Schmitt JS, Chen J, Waser B, Reubi JC, de Jong M, et al. Design, synthesis, and biological evaluation of somatostatin-based radiopeptides. Chem Biol 2006;13:1081–90.
Ginj M, Chen J, Walter MA, Eltschinger V, Reubi JC, Maecke HR. Preclinical evaluation of new and highly potent analogues of octreotide for predictive imaging and targeted radiotherapy. Clin Cancer Res 2005;11:1136–45.
Antunes P, Ginj M, Zhang H, Waser B, Baum RP, Reubi JC, et al. Are radiogallium-labelled DOTA-conjugated somatostatin analogues superior to those labelled with other radiometals? Eur J Nucl Med Mol Imaging 2007;34:982–93.
Fani M, Mueller A, Tamma ML, Nicolas G, Rink HR, Cescato R, et al. Radiolabeled bicyclic somatostatin-based analogs: a novel class of potential radiotracers for SPECT/PET of neuroendocrine tumors. J Nucl Med 2010;51:1771–9.
Reubi JC, Eisenwiener KP, Rink H, Waser B, Mäcke HR. A new peptidic somatostatin agonist with high affinity to all five somatostatin receptors. Eur J Pharmacol 2002;456:45–9.
Ginj M, Zhang H, Eisenwiener KP, Wild D, Schulz S, Rink H, et al. New pansomatostatin ligands and their chelated versions: affinity profile, agonist activity, internalization, and tumor targeting. Clin Cancer Res 2008;14:2019–27.
Cescato R, Loesch KA, Waser B, Mäcke HR, Rivier JE, Reubi JC, et al. Agonist-biased signaling at the sst2A receptor: the multi-somatostatin analogs KE108 and SOM230 activate and antagonize distinct signaling pathways. Mol Endocrinol 2010;24:240–9.
Ginj M, Zhang H, Waser B, Cescato R, Wild D, Wang X, et al. Radiolabeled somatostatin receptor antagonists are preferable to agonists for in vivo peptide receptor targeting of tumors. Proc Natl Acad Sci U S A 2006;103:16436–41.
Cescato R, Erchegyi J, Waser B, Piccand V, Maecke HR, Rivier JE, et al. Design and in vitro characterization of highly sst2-selective somatostatin antagonists suitable for radiotargeting. J Med Chem 2008;51:4030–7.
Wild D, Fani M, Behe M, Brink I, Rivier JE, Reubi JC, et al. First clinical evidence that imaging with somatostatin receptor antagonists is feasible. J Nucl Med 2011;52:1412–7.
Van de Wiele C, Dumont F, Vanden Broecke R, Oosterlinck W, Cocquyt V, Serreyn R, et al. Technetium-99m RP527, a GRP analogue for visualisation of GRP receptor-expressing malignancies: a feasibility study. Eur J Nucl Med 2000;27:1694–9.
Cescato R, Maina T, Nock B, Nikolopoulou A, Charalambidis D, Piccand V, et al. Bombesin receptor antagonists may be preferable to agonists for tumor targeting. J Nucl Med 2008;49:318–26.
Smith CJ, Gali H, Sieckman GL, Higginbotham C, Volkert WA, Hoffman TJ. Radiochemical investigations of (99m)Tc-N(3)S-X-BBN[7–14]NH(2): an in vitro/in vivo structure-activity relationship study where X = 0-, 3-, 5-, 8-, and 11-carbon tethering moieties. Bioconjug Chem 2003;14:93–102.
Faintuch BL, Teodoro R, Duatti A, Muramoto E, Faintuch S, Smith CJ. Radiolabeled bombesin analogs for prostate cancer diagnosis: preclinical studies. Nucl Med Biol 2008;35:401–11.
García Garayoa E, Rüegg D, Bläuenstein P, Zwimpfer M, Khan IU, Maes V, et al. Chemical and biological characterization of new Re(CO)3/[99mTc](CO)3 bombesin analogues. Nucl Med Biol 2007;34:17–28.
García Garayoa E, Schweinsberg C, Maes V, Rüegg D, Blanc A, Bläuenstein P, et al. New [99mTc]bombesin analogues with improved biodistribution for targeting gastrin releasing-peptide receptor-positive tumors. Q J Nucl Med Mol Imaging 2007;51:42–50.
Schweinsberg C, Maes V, Brans L, Bläuenstein P, Tourwé DA, Schubiger PA, et al. Novel glycated [99mTc(CO)3]-labeled bombesin analogues for improved targeting of gastrin-releasing peptide receptor-positive tumors. Bioconjug Chem 2008;19:2432–9.
García Garayoa E, Schweinsberg C, Maes V, Brans L, Bläuenstein P, Tourwe DA, et al. Influence of the molecular charge on the biodistribution of bombesin analogues labeled with the [99mTc(CO)3]-core. Bioconjug Chem 2008;19:2409–16.
Garrison JC, Rold TL, Sieckman GL, Naz F, Sublett SV, Figueroa SD, et al. Evaluation of the pharmacokinetic effects of various linking group using the 111In-DOTA-X-BBN(7–14)NH2 structural paradigm in a prostate cancer model. Bioconjug Chem 2008;19:1803–12.
Garrison JC, Rold TL, Sieckman GL, Figueroa SD, Volkert WA, Jurisson SS, et al. In vivo evaluation and small-animal PET/CT of a prostate cancer mouse model using 64Cu bombesin analogs: side-by-side comparison of the CB-TE2A and DOTA chelation systems. J Nucl Med 2007;48:1327–37.
Pradhan TK, Katsuno T, Taylor JE, Kim SH, Ryan RR, Mantey SA, et al. Identification of a unique ligand which has high affinity for all four bombesin receptor subtypes. Eur J Pharmacol 1998;343:275–87.
Zhang H, Chen J, Waldherr C, Hinni K, Waser B, Reubi JC, et al. Synthesis and evaluation of bombesin derivatives on the basis of pan-bombesin peptides labeled with indium-111, lutetium-177, and yttrium-90 for targeting bombesin receptor-expressing tumors. Cancer Res 2004;64:6707–15.
Schuhmacher J, Zhang H, Doll J, Mäcke HR, Matys R, Hauser H, et al. GRP receptor-targeted PET of a rat pancreas carcinoma xenograft in nude mice with a 68Ga-labeled bombesin(6–14) analog. J Nucl Med 2005;46:691–9.
Dimitrakopoulou-Strauss A, Seiz M, Tuettenberg J, Schmieder K, Eisenhut M, Haberkorn U, et al. Pharmacokinetic studies of 68Ga-labeled bombesin (68Ga-BZH3) and F-18 FDG PET in patients with recurrent gliomas and comparison to grading: preliminary results. Clin Nucl Med 2011;36:101–8.
Lantry LE, Cappelletti E, Maddalena ME, Fox JS, Feng W, Chen J, et al. 177Lu-AMBA: synthesis and characterization of a selective 177Lu-labeled GRP-R agonist for systemic radiotherapy of prostate cancer. J Nucl Med 2006;47:1144–52.
Waser B, Eltschinger V, Linder K, Nunn A, Reubi JC. Selective in vitro targeting of GRP and NMB receptors in human tumours with the new bombesin tracer 177Lu-AMBA. Eur J Nucl Med Mol Imaging 2007;34:95–100.
Bodei L, Ferrari M, Nunn A, Lull JB, Cremonesi M, Martano L, et al. 177Lu-AMBA Bombesin analogue in hormone refractory prostate cancer patients: a phase I escalation study with single-cycle administrations. Eur J Nucl Med Mol Imaging 2007;34 Suppl 2:S221.
Zhang H, Schuhmacher J, Waser B, Wild D, Eisenhut M, Reubi JC, et al. DOTA-PESIN, a DOTA-conjugated bombesin derivative designed for the imaging and targeted radionuclide treatment of bombesin receptor-positive tumours. Eur J Nucl Med Mol Imaging 2007;34:1198–208.
Wild D, Frischknecht M, Zhang H, Morgenstern A, Bruchertseifer F, Boisclair J, et al. Alpha- versus beta-particle radiopeptide therapy in a human prostate cancer model (213Bi-DOTA-PESIN and 213Bi-AMBA versus 177Lu-DOTA-PESIN). Cancer Res 2011;71:1009–18.
Mansi R, Wang X, Forrer F, Kneifel S, Tamma ML, Waser B, et al. Evaluation of a 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid-conjugated bombesin-based radioantagonist for the labeling with single-photon emission computed tomography, positron emission tomography, and therapeutic radionuclides. Clin Cancer Res 2009;15:5240–9.
Mansi R, Wang X, Forrer F, Waser B, Cescato R, Graham K, et al. Development of a potent DOTA-conjugated bombesin antagonist for targeting GRPr-positive tumours. Eur J Nucl Med Mol Imaging 2011;38:97–107.
Abiraj K, Mansi R, Tamma ML, Fani M, Forrer F, Nicolas G, et al. Bombesin antagonist-based radioligands for translational nuclear imaging of gastrin releasing peptide receptor positive tumors. J Nucl Med 2011. doi:10.2967/jnumed.111.094375.
Gornik G, Mansi R, Maecke H, Weber WA, et al. Evaluation of the GRPR radioantagonist 64Cu-CB-TE2A-AR-06 in mice and men. J Nucl Med 2011;52 Suppl 1:7P.
Honer M, Mu L, Stellfeld T, Graham K, Martic M, Fischer CR, et al. 18F-labeled bombesin analog for specific and effective targeting of prostate tumors expressing gastrin-releasing peptide receptors. J Nucl Med 2011;52:270–8.
Behr TM, Béhé MP. Cholecystokinin-B/Gastrin receptor-targeting peptides for staging and therapy of medullary thyroid cancer and other cholecystokinin-B receptor-expressing malignancies. Semin Nucl Med 2002;32:97–109.
Wank SA. G protein-coupled receptors in gastrointestinal physiology. I. CCK receptors: an exemplary family. Am J Physiol 1998;274:G607–13.
Reubi JC, Waser B, Schaer JC, Laederach U, Erion J, Srinivasan A, et al. Unsulfated DTPA- and DOTA-CCK analogs as specific high-affinity ligands for CCK-B receptor-expressing human and rat tissues in vitro and in vivo. Eur J Nucl Med 1998;25:481–90.
Roosenburg S, Laverman P, Joosten L, Eek A, Oyen WJ, de Jong M, et al. Stabilized (111)in-labeled sCCK8 analogues for targeting CCK2-receptor positive tumors: synthesis and evaluation. Bioconjug Chem 2010;21:663–70.
Laverman P, Béhé M, Oyen WJ, Willems PH, Corstens FH, Behr TM, et al. Two technetium-99m-labeled cholecystokinin-8 (CCK8) peptides for scintigraphic imaging of CCK receptors. Bioconjug Chem 2004;15:561–8.
Behr TM, Béhé M, Angerstein C, Gratz S, Mach R, Hagemann L, et al. Cholecystokinin-B/gastrin receptor binding peptides: preclinical development and evaluation of their diagnostic and therapeutic potential. Clin Cancer Res 1999;5:3124s–38s.
Béhé M, Becker W, Gotthardt M, Angerstein C, Behr TM. Improved kinetic stability of DTPA-dGlu as compared with conventional monofunctional DTPA in chelating indium and yttrium: preclinical and initial clinical evaluation of radiometal labelled minigastrin derivatives. Eur J Nucl Med Mol Imaging 2003;30:1140–6.
Béhé M, Kluge G, Becker W, Gotthardt M, Behr TM. Use of polyglutamic acids to reduce uptake of radiometal-labeled minigastrin in the kidneys. J Nucl Med 2005;46:1012–5.
Good S, Walter MA, Waser B, Wang X, Müller-Brand J, Béhé MP, et al. Macrocyclic chelator-coupled gastrin-based radiopharmaceuticals for targeting of gastrin receptor-expressing tumours. Eur J Nucl Med Mol Imaging 2008;35:1868–77.
Mather SJ, McKenzie AJ, Sosabowski JK, Morris TM, Ellison D, Watson SA. Selection of radiolabeled gastrin analogs for peptide receptor-targeted radionuclide therapy. J Nucl Med 2007;48:615–22.
Nock BA, Maina T, Béhé M, Nikolopoulou A, Gotthardt M, Schmitt JS, et al. CCK-2/gastrin receptor-targeted tumor imaging with (99m)Tc-labeled minigastrin analogs. J Nucl Med 2005;46:1727–36.
Fröberg AC, de Jong M, Nock BA, Breeman WA, Erion JL, Maina T, et al. Comparison of three radiolabelled peptide analogues for CCK-2 receptor scintigraphy in medullary thyroid carcinoma. Eur J Nucl Med Mol Imaging 2009;36:1265–72.
von Guggenberg E, Dietrich H, Skvortsova I, Gabriel M, Virgolini IJ, Decristoforo C. 99mTc-labelled HYNIC-minigastrin with reduced kidney uptake for targeting of CCK-2 receptor-positive tumours. Eur J Nucl Med Mol Imaging 2007;34:1209–18.
von Guggenberg E, Sallegger W, Helbok A, Ocak M, King R, Mather SJ, et al. Cyclic minigastrin analogues for gastrin receptor scintigraphy with technetium-99m: preclinical evaluation. J Med Chem 2009;52:4786–93.
Sosabowski JK, Matzow T, Foster JM, Finucane C, Ellison D, Watson SA, et al. Targeting of CCK-2 receptor-expressing tumors using a radiolabeled divalent gastrin peptide. J Nucl Med 2009;50:2082–9.
Kolenc-Peitl P, Mansi R, Tamma M, Gmeiner-Stopar T, Sollner-Dolenc M, Waser B, et al. Highly improved metabolic stability and pharmacokinetics of indium-111-DOTA-gastrin conjugates for targeting of the gastrin receptor. J Med Chem 2011;54:2602–9.
Aloj L, Aurilio M, Rinaldi V, D’ambrosio L, Tesauro D, Peitl PK, et al. Comparison of the binding and internalization properties of 12 DOTA-coupled and (111)In-labelled CCK2/gastrin receptor binding peptides: a collaborative project under COST Action BM0607. Eur J Nucl Med Mol Imaging 2011;38:1417–25.
Ocak M, Helbok A, Rangger C, Peitl PK, Nock BA, Morelli G, et al. Comparison of biological stability and metabolism of CCK2 receptor targeting peptides, a collaborative project under COST BM0607. Eur J Nucl Med Mol Imaging 2011;38:1426–35.
Laverman P, Joosten L, Eek A, Roosenburg S, Peitl PK, Maina T, et al. Comparative biodistribution of 12 (111)In-labelled gastrin/CCK2 receptor-targeting peptides. Eur J Nucl Med Mol Imaging 2011;38:1410–6.
Reubi JC, Waser B. Concomitant expression of several peptide receptors in neuroendocrine tumours: molecular basis for in vivo multireceptor tumour targeting. Eur J Nucl Med Mol Imaging 2003;30:781–93.
Singh G, Eng J, Raufman JP. Use of 125I-[Y39]exendin-4 to characterize exendin receptors on dispersed pancreatic acini and gastric chief cells from guinea pig. Regul Pept 1994;53:47–59.
Wild D, Béhé M, Wicki A, Storch D, Waser B, Gotthardt M, et al. [Lys40(Ahx-DTPA-111In)NH2]exendin-4, a very promising ligand for glucagon-like peptide-1 (GLP-1) receptor targeting. J Nucl Med 2006;47:2025–33.
Gotthardt M, Lalyko G, van Eerd-Vismale J, Keil B, Schurrat T, Hower M, et al. A new technique for in vivo imaging of specific GLP-1 binding sites: first results in small rodents. Regul Pept 2006;137:162–7.
Wicki A, Wild D, Storch D, Seemayer C, Gotthardt M, Behe M, et al. [Lys40(Ahx-DTPA-111In)NH2]-Exendin-4 is a highly efficient radiotherapeutic for glucagon-like peptide-1 receptor-targeted therapy for insulinoma. Clin Cancer Res 2007;13:3696–705.
Wild D, Mäcke H, Christ E, Gloor B, Reubi JC. Glucagon-like peptide 1-receptor scans to localize occult insulinomas. N Engl J Med 2008;359:766–8.
Christ E, Wild D, Forrer F, Brändle M, Sahli R, Clerici T, et al. Glucagon-like peptide-1 receptor imaging for localization of insulinomas. J Clin Endocrinol Metab 2009;94:4398–405.
Wild D, Christ E, Caplin ME, Kurzawinski TR, Forrer F, Brändle M, et al. Glucagon-like peptide-1 versus somatostatin receptor targeting reveals 2 distinct forms of malignant insulinomas. J Nucl Med 2011;52:1073–8.
Brom M, Oyen WJ, Joosten L, Gotthardt M, Boerman OC. 68Ga-labelled exendin-3, a new agent for the detection of insulinomas with PET. Eur J Nucl Med Mol Imaging 2010;37:1345–55.
Hubalewska-Dydejczyk A, Sowa-Staszczak A, Mikolajczak R, Pach D, Janota B, Tomaszuk M, et al. 99mTc labeled GLP-1 scintigraphy with the use of [Lys40-(Ahx-HYNIC/EDDA)NH2]-Exendin-4 in the insulinoma localization. J Nucl Med 2011;52 Suppl 1:561.
Sowa-Staszczak A, Stefanska A, Pach D, Tomaszuk M, Jabrocka-Hybel A, Glowa B, et al. First clinical application of 99mTc labelled long-acting agonist of GLP-1 (Exendin-4) in endocrine diagnosis. Eur J Nucl Med Mol Imaging. 2011;38 Suppl 2:S206.
Brom M, Baumeister P, Melis M, Laverman P, Joosten L, Behe M, et al. Determination of the beta-cell mass by SPECT imaging with In-111-DTPA-Exendin-3 in rats. J Nucl Med 2009;50 Suppl 2:147.
Connolly BM, Vanko A, McQuade P, Guenther I, Meng X, Rubins D, et al. Ex vivo imaging of pancreatic beta cells using a radiolabeled GLP-1 receptor agonist. Mol Imaging Biol 2011. doi:10.1007/s11307-011-0481-7.
Wu Z, Todorov I, Li L, Bading JR, Li Z, Nair I, et al. In vivo imaging of transplanted islets with 64Cu-DO3A-VS-Cys40-Exendin-4 by targeting GLP-1 receptor. Bioconjug Chem 2011;22:1587–94.
Pattou F, Kerr-Conte J, Wild D. GLP-1-receptor scanning for imaging of human beta cells transplanted in muscle. N Engl J Med 2010;363:1289–90.
Desgrosellier JS, Cheresh DA. Integrins in cancer: biological implications and therapeutic opportunities. Nat Rev Cancer 2010;10:9–22.
Haubner R, Beer AJ, Wang H, Chen X. Positron emission tomography tracers for imaging angiogenesis. Eur J Nucl Med Mol Imaging 2010;37 Suppl 1:S86–S103.
Haubner R, Weber WA, Beer AJ, Vabuliene E, Reim D, Sarbia M, et al. Noninvasive visualization of the activated alphavbeta3 integrin in cancer patients by positron emission tomography and [18F]Galacto-RGD. PLoS Med 2005;2:e70.
Beer AJ, Haubner R, Sarbia M, Goebel M, Luderschmidt S, Grosu AL, et al. Positron emission tomography using [18F]Galacto-RGD identifies the level of integrin alpha(v)beta3 expression in man. Clin Cancer Res 2006;12:3942–9.
Indrevoll B, Kindberg GM, Solbakken M, Bjurgert E, Johansen JH, Karlsen H, et al. NC-100717: a versatile RGD peptide scaffold for angiogenesis imaging. Bioorg Med Chem Lett 2006;16:6190–3.
Kenny LM, Coombes RC, Oulie I, Contractor KB, Miller M, Spinks TJ, et al. Phase I trial of the positron-emitting Arg-Gly-Asp (RGD) peptide radioligand 18F-AH111585 in breast cancer patients. J Nucl Med 2008;49:879–86.
Cho HJ, Lee JD, Park JY, Yun M, Kang WJ, Walsh JC, et al. First in human evaluation of a newly developed PET tracer, 18F-RGD-K5 in patients with breast cancer: comparison with 18F-FDG uptake pattern and microvessel density. J Nucl Med 2009;50 Suppl 2:1910.
Chen X, Park R, Tohme M, Shahinian AH, Bading JR, Conti PS. MicroPET and autoradiographic imaging of breast cancer alpha v-integrin expression using 18F- and 64Cu-labeled RGD peptide. Bioconjug Chem 2004;15:41–9.
Decristoforo C, Hernandez Gonzalez I, Carlsen J, Rupprich M, Huisman M, Virgolini I, et al. 68Ga- and 111In-labelled DOTA-RGD peptides for imaging of alphavbeta3 integrin expression. Eur J Nucl Med Mol Imaging 2008;35:1507–15.
Jeong JM, Hong MK, Chang YS, Lee YS, Kim YJ, Cheon GJ, et al. Preparation of a promising angiogenesis PET imaging agent: 68Ga-labeled c(RGDyK)-isothiocyanatobenzyl-1,4,7-triazacyclononane-1,4,7-triacetic acid and feasibility studies in mice. J Nucl Med 2008;49:830–6.
Chen X, Hou Y, Tohme M, Park R, Khankaldyyan V, Gonzales-Gomez I, et al. Pegylated Arg-Gly-Asp peptide: 64Cu labeling and PET imaging of brain tumor alphavbeta3-integrin expression. J Nucl Med 2004;45:1776–83.
Chen X, Park R, Hou Y, Khankaldyyan V, Gonzales-Gomez I, Tohme M, et al. MicroPET imaging of brain tumor angiogenesis with 18F-labeled PEGylated RGD peptide. Eur J Nucl Med Mol Imaging 2004;31:1081–9.
Chen X, Tohme M, Park R, Hou Y, Bading JR, Conti PS. Micro-PET imaging of alphavbeta3-integrin expression with 18F-labeled dimeric RGD peptide. Mol Imaging 2004;3:96–104.
Zhang X, Xiong Z, Wu Y, Cai W, Tseng JR, Gambhir SS, et al. Quantitative PET imaging of tumor integrin alphavbeta3 expression with 18F-FRGD2. J Nucl Med 2006;47:113–21.
Janssen ML, Oyen WJ, Dijkgraaf I, Massuger LF, Frielink C, Edwards DS, et al. Tumor targeting with radiolabeled alpha(v)beta(3) integrin binding peptides in a nude mouse model. Cancer Res 2002;62:6146–51.
Dijkgraaf I, Yim CB, Franssen GM, Schuit RC, Luurtsema G, Liu S, et al. PET imaging of alphavbeta3 integrin expression in tumours with 68Ga-labelled mono-, di- and tetrameric RGD peptides. Eur J Nucl Med Mol Imaging 2011;38:128–37.
Li ZB, Cai W, Cao Q, Chen K, Wu Z, He L, et al. (64)Cu-labeled tetrameric and octameric RGD peptides for small-animal PET of tumor alpha(v)beta(3) integrin expression. J Nucl Med 2007;48:1162–71.
Liu Z, Niu G, Shi J, Liu S, Wang F, Chen X. (68)Ga-labeled cyclic RGD dimers with Gly3 and PEG4 linkers: promising agents for tumor integrin alphavbeta3 PET imaging. Eur J Nucl Med Mol Imaging 2009;36:947–57.
Bach-Gansmo T, Danielsson R, Saracco A, Wilczek B, Bogsrud TV, Fangberget A, et al. Integrin receptor imaging of breast cancer: a proof-of-concept study to evaluate 99mTc-NC100692. J Nucl Med 2006;47:1434–9.
Liu S, Liu Z, Chen K, Yan Y, Watzlowik P, Wester HJ, et al. 18F-labeled galacto and PEGylated RGD dimers for PET imaging of alphavbeta3 integrin expression. Mol Imaging Biol 2010;12:530–8.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fani, M., Maecke, H.R. Radiopharmaceutical development of radiolabelled peptides. Eur J Nucl Med Mol Imaging 39 (Suppl 1), 11–30 (2012). https://doi.org/10.1007/s00259-011-2001-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-011-2001-z