Abstract
Purpose
Renal radioiodine excretion is ~50% faster during euthyroidism versus hypothyroidism. We therefore sought to assess lesion dose/GBq of administered 131I activity (LDpA) in iodine-avid metastases (IAM) of differentiated thyroid carcinoma (DTC) in athyreotic patients after recombinant human thyroid-stimulating hormone (rhTSH) versus after thyroid hormone withdrawal (THW).
Methods
We retrospectively compared mean LDpA between groups of consecutive patients (N = 63) receiving 124I positron emission tomography/computed tomography (124I PET/CT) aided by rhTSH (n = 27) or THW (n = 36); we prospectively compared LDpA after these stimulation methods within another individual. Data derived from serial PET scans and one CT scan performed 2–96 h post-124I ingestion. A mixed model analysis of covariance (ANCOVA) calculated the treatment groups’ mean LDpAs adjusting for statistically significant baseline intergroup differences: non-IAM were more prevalent, median IAM count/patient lower in cervical lymph nodes and higher in distant sites, median stimulated thyroglobulin higher, mean cumulative radioiodine activity greater and prior diagnostic scintigraphy more frequent in the rhTSH patients.
Results
Mean LDpAs were: rhTSH group (n = 71 IAM), 30.6 Gy/GBq; THW group (n = 66 IAM), 51.8 Gy/GBq. The difference in group means (rhTSH less THW), −21.2 Gy/GBq, was statistically non-significant (p = 0.1667). However, the 95% confidence interval of that difference (−51.4 to + 9 Gy/GBq) suggested a trend favouring THW. The within-patient comparison found 2.9- to 10-fold higher LDpAs under THW.
Conclusion
We found some suggestions, but no statistically significant evidence, that rhTSH administration results in a lower radiation dose to DTC metastases than does THW. A large, well-controlled, prospective within-patient study should resolve this issue.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Radioiodine therapy (RIT) with 131I is a mainstay in the treatment of iodine-avid metastases of differentiated thyroid carcinoma (DTC). To optimise RIT, it is considered necessary to elevate serum thyroid-stimulating hormone (TSH) to compensate for sodium-iodide symporter (NIS) defects in DTC cells [1–3]. In athyreotic patients, such serum TSH elevation traditionally has been attained endogenously, through several weeks of thyroid hormone withdrawal (THW). However, clinical hypothyroidism frequently ensues, leading to important morbidity, with markedly reduced quality of life and ability to perform daily living, work, academic and leisure activities [4–7]. Additionally, THW-related hypothyroidism may exacerbate concomitant cardiovascular, psychological and other conditions [8].
Recombinant human TSH (rhTSH) was developed to elevate serum TSH exogenously, allowing patients to continue on thyroid hormone and to avoid THW-related hypothyroid morbidity [9]. rhTSH has undergone Phase 3 clinical study [10] and received regulatory approval in Europe and North America as an adjunct to the administration of large radioiodine activities for thyroid remnant ablation.
However, although rhTSH has been applied “off-label” safely and sometimes with efficacy in hundreds of patients to aid RIT of iodine-avid metastatic DTC [11, 12], the drug has not undergone Phase 3 study for this indication. Additionally, only limited data have been published on lesional radioiodine kinetics under rhTSH stimulation. Publications to date comprise three individual case reports [13–15] and two small studies [16, 17].
Radioiodine kinetics, and particularly the lesion dose after rhTSH versus after THW, are of clinical interest for two reasons. First, the markedly faster (by ~50%) renal excretion of radioiodine under euthyroid conditions compared to hypothyroid conditions [18, 19] raises the possibility that the radiation dose delivered by a given 131I activity could differ appreciably between the two TSH stimulation methods. Second, use of an effective radioiodine activity is especially important in the RIT of metastatic disease, the DTC setting with, at least theoretically, the most marked NIS defects and the greatest downside to diminished efficacy.
We therefore sought, through a retrospective analysis, to compare the DTC lesion dose after rhTSH versus under THW in a large series of patients with metastatic DTC, employing 124I positron emission tomography/computed tomography (124I PET/CT), a relatively accurate and a clinically useful dosimetric method [20]. We also applied 124I PET/CT to conduct a prospective within-patient comparison in an additional individual from the Hanover University School of Medicine (MHH); we present a case report of this comparison.
Materials and methods
Patients
The retrospective study included all consecutive DTC patients (N = 63) seen from 1 January 2004 through 31 December 2006 at a tertiary referral centre, the University Hospital of Essen, fulfilling two criteria. First, the patients had one or more radioiodine-avid DTC neck lymph node metastases or distant metastases, or both. Second, the patients underwent 124I PET/CT dosimetry before a planned RIT for treatment of unresectable disease, and in some cases, also for thyroid remnant ablation. Only data from each patient’s first 124I PET/CT imaging were used in this analysis. However, more than 40% of patients in either treatment group had received their first 124I PET/CT examination when no longer RIT-naïve, i.e. before a second or subsequent RIT (Table 1).
The study population was made up of two types of DTC patients routinely receiving pre-RIT 124I PET/CT dosimetry at our centre: (1) those with histologically confirmed advanced disease, namely pT4, pN1 or cM1 status [21] and (2) selected other “high-risk” individuals, e.g. those with unfavourable histology or under 19 years old. All patients or their parents or guardians gave written informed consent for 124I PET/CT dosimetry and for analysis and publication of related data.
Treatment groups
Based on their TSH preparation method for 124I PET/CT, the 63 patients eligible for the present analysis were retrospectively divided into an “rhTSH group” (n = 27) or a “THW group” (n = 36). Those in the rhTSH group were on thyroid hormone therapy, which had been started 2 days after thyroidectomy. They ingested 124I 24 h after the second of two consecutive daily intramuscular injections of rhTSH (Thyrogen®, Genzyme Corporation, Cambridge, MA, USA), 0.9 mg. Patients in the THW group ingested 124I following at least 4 weeks without thyroid hormone, after their serum TSH levels first were measured at ≥ 25 mIU/l.
The criteria for choosing rhTSH versus THW were subjective, case by case and not systematically recorded. Our clinical impression is that rhTSH was most often prescribed due to high risks of tumour progression during prolonged TSH elevation or of concomitant illness exacerbation due to hypothyroidism. However, in some patients, the indication for rhTSH was avoidance of hypothyroid morbidity in order to preserve the ability to work or study.
124I PET/CT dosimetry protocol—University of Essen (retrospective study)
We described our 124I PET/CT dosimetry protocol in detail elsewhere [20, 22]. Briefly, we obtained whole-body 124I PET data 4, 24, 48, 72 and 96 h and 124I PET/CT data 25 h post-oral administration of 24 ± 3 MBq of highly purified 124I from our cyclotron [23, 24]. We gave these low 124I activities to avoid potential “stunning,” i.e. impairment of therapeutic radioiodine uptake due to incomplete treatment or other biological effects of the tracer activity. In our hands, these activities obtain sufficient signal to noise ratios [25].
We used a Biograph Emotion Duo combined PET/CT scanner for the 25-h imaging and an ECAT EXACT HR + PET scanner for all other imaging (both models from Siemens Medical Solutions, Hoffman Estates, IL, USA). Whole-body emission data were acquired by scanning from head to thigh in three-dimensional mode using five to eight bed positions for 5 min each. CT scans were performed with 130 kVp tube voltage, 160 mAs, 5-mm slice width and 1.6 pitch, without contrast agent. For image reconstruction of the corrected emission data, we employed Fourier rebinning attenuation-weighted ordered subsets expectation maximisation at 2 iterations and 8 subsets with a 5-mm post-reconstruction Gaussian filter and attenuation image segmentation. We used CT data to correct for PET/CT scan attenuation.
124I PET/CT dosimetry protocol—MHH (case report of within-patient comparison)
124I PET/CT dosimetry methods for the within-patient comparison were essentially similar to those for the retrospective study, except that scanning was performed at MHH (although the same scanner models were used as at Essen), and except that PET was performed 4, 12, 24 and 48 h and CT approximately 24 h post-124I administration.
Lesion dose per administered activity (LDpA) calculation
Using the 124I PET data, we determined the so-called LDpA, that is, the lesion dose that would be obtained with administration of 1 GBq of 131I, according to the formula:
where Δ denoted the equilibrium dose constant for non-penetrating radiation for 131I, 0.11 (Gy g)/(MBq h) [26], ρ denoted the gland mass density assuming the value of water (1 g/ml) and V denoted the lesion volume in ml. \( C{{\widetilde{ }}} \) represented the cumulative activity of 131I, obtained using the time-activity curves of the serial 124I PET scans corrected with the measured recovery coefficient [27]. \( {A_{\rm{tr}}} \) represented the tracer activity upon capsule administration. The self-irradiation absorbed dose of the ß-particles was calculated using the Medical Internal Radiation Dose formula [28], omitting effects at the lesion border. The penetrating absorbed dose, i.e. γ-rays, was ignored since the lesion volumes were small.
Lesion volumetry
For volumetry of each lesion, we chose the method among the CT component of the 124I PET/CT, ultrasonography (US) or a novel PET iterative thresholding (ITM) technique [29] that best visualised the given lesion; these three modalities are listed in descending order of the frequency with which they were applied. US was performed by experienced operators on a Sonoline Elegra system using previously described methods [30]; a 7.5L40 small part transducer at a frequency of 8 MHz was used for neck imaging and a convex array 4C1 transducer at a frequency of 3 MHz was used for abdominal imaging. The ITM method was developed and validated using 18F-fluorodeoxyglucose PET as well as 124I PET and using phantoms as well as DTC metastases and other tumours ≥ 0.7 ml on CT [29]. The average absolute deviation between measurements obtained with ITM and those obtained with CT has been documented elsewhere as ~9% for lesions 0.8–7.5 ml (n = 31) and ~15% for lesions >7.5 ml (n = 8) [29].
Statistics
For patient, disease, treatment and imaging characteristics, we generated baseline statistics, including, as applicable, the frequency, the median and range (minimum-maximum), and the mean ± standard deviation (SD). We statistically compared intergroup differences in the baseline values using Pearson’s χ2 test for dichotomous variables or, when dichotomous variables had a small number of expected frequencies, Fisher’s exact test. We applied the t test to statistically compare intergroup differences in variables having homogeneous variances and following an approximately Gaussian distribution. For variables having heterogeneous variances and following a Gaussian distribution, Welch’s t test was computed. The asymptotic Wilcoxon rank sum test was used to compare variables with a skewed distribution. For all comparisons of baseline values, p < 0.05 was considered statistically significant.
The calculation of the mean LDpA for each treatment group comprised the LDpAs of all lesions in the group that were defined as iodine-avid according to previously described criteria [31]. Since patients varied in their number of iodine-avid lesions, this approach meant that the calculation included more lesions from some individuals than from others. This situation could potentially introduce bias; however, our statistical model attempted to mitigate against such bias (see below). Moreover, we felt that using the mean, median, minimum or maximum LDpA for each patient would be an arbitrary choice that also could potentially introduce bias and beyond that, would obscure the actual dosimetric situation of many lesions.
As its primary statistical analysis, the study tested whether the mean LDpAs of the rhTSH group and the THW group were equivalent. For this purpose, a (1-2α) confidence interval (CI) of the difference between those means (mean rhTSH group LDpA − mean THW group LDpA) was computed using a mixed model analysis of covariance (ANCOVA). Included in the model was the fixed factor, treatment group (rhTSH or THW) and possible covariables adjusting for the patient, disease, treatment or imaging characteristics found to differ significantly between the groups, except for biochemical variables (TSH, thyroid hormones) related to the difference in preparation methods. Most patients had more than one metastasis. Thus, repeated measurements existed and to account for them, the patients were included in the model as the random factor. The type I error, α, was set to 2.5%, resulting in a 95.0% CI. We performed all statistical calculations on SPSS for Windows, release 15.0.1 (SPSS Inc., Chicago, IL, USA, 2006) or on SAS for Windows Release 9.1 (SAS Institute, Inc., Cary, NC, USA, 2003).
Results
Patient and 124I PET characteristics
Table 1 shows selected patient, disease, treatment and imaging characteristics for the rhTSH and THW groups. These groups did not differ statistically with respect to gender, height, weight, age at the study 124I PET/CT, distributions of DTC histology classifications or T, N or M classifications, number of iodine-avid lesions per patient, proportion of patients without visible thyroid remnant, median total thyroid remnant volume, urinary iodine excretion or proportion of patients undergoing 124I PET/CT before versus after their first RIT. The groups also did not differ significantly according to prevalence of anti-thyroglobulin (Tg) antibody seropositivity, interval between diagnosis of metastatic DTC and 124I PET/CT or 124I activity (data not shown).
However, six statistically significant differences between the groups suggested that the rhTSH patients tended to have more advanced disease than did the THW patients (Table 1). Namely, non-iodine-avid metastases were more than half again as prevalent in the rhTSH group as in the THW group. Additionally, the median number of iodine-avid cervical lymph node metastases per patient was lower, but the median number of iodine-avid distant metastases was higher in the rhTSH patients. Further, median stimulated serum Tg was over 16 times as high, and median prior cumulative radioiodine activity was over 3 times as high in the rhTSH group as in the THW group. Lastly, the rhTSH group tended to have received more diagnostic whole-body scintigraphy (dxWBS) scans than had the THW group.
As expected given the exogenous TSH administration and uninterrupted thyroid hormone therapy in the rhTSH patients but not the THW patients, the rhTSH group had significantly higher serum TSH (Table 1), free triiodothyronine and free levothyroxine concentrations (data not shown). However, in no patient did free triiodothyronine or free levothyroxine reach thyrotoxic levels (data not shown).
LDpA
Table 2 presents the results of the primary analysis, a mixed model ANCOVA addressing the treatment groups’ mean LDpAs and the differences between these values. To adjust the estimated treatment effect for the statistically significant intergroup differences in patient, disease, treatment or imaging characteristics, the model factored in the prevalence of non-iodine-avid metastases, the median lesion counts/patient for cervical lymph node or distant metastases, the median stimulated serum Tg value, the mean cumulative prior 131I activity and the median number of prior dxWBS scans.
As seen in Table 2, the mean LDpA computed by the mixed model ANCOVA for the rhTSH group was under 60% of that of the THW group. Nonetheless, the difference between the group mean LDpAs was not statistically significant. However, 85% of the CI, i.e. 51.4 Gy/GBq of the 60.4 Gy/GBq total, encompassed differences favouring THW.
Prospective within-patient comparison, MHH
Table 3 presents selected biochemical, 124I PET and dosimetric variables for a 78-year-old woman at the MHH participating in a prospective within-patient comparison of LDpAs on 124I PET/CT under rhTSH stimulation versus under THW stimulation. This comparison was conducted under an experimental protocol that was approved by the MHH Ethics Committee, and the patient provided written informed consent to participate.
The patient had pT4b N0 M1 disease according to the 5th edition of the Union Internationale Contre le Cancer staging system [21]. After total thyroidectomy, she received four THW-aided RITs totalling 44.4 GBq to ablate thyroid remnant (first RIT) or to treat pulmonary metastases (all four RITs). Throughout this patient’s course, thoracic CT showed small lung metastases, which decreased in size after each RIT, remaining stable at the smaller sizes between therapies. Six days after her most recent RIT (7.4 GBq given 5 months before study entry), post-therapy whole-body scintigraphy revealed local recurrence on the left side of the thyroid bed and pathological uptake in the left adrenal gland. Shortly before study entry, neck US showed the same local recurrence, while FDG PET was slightly positive at this site and the left adrenal gland. The patient’s most recent Tg measurement (THW-aided and performed 3 months before study entry) was 226.6 μg/l. At the time of study entry, she was on suppressive thyroid hormone therapy (serum TSH <0.1 mU/l).
After two consecutive IM injections of rhTSH, 0.9 mg, she ingested 27.7 MBq 124I and underwent 124I PET/CT as described in the “Materials and methods” section. The patient began THW the day after the last rhTSH-aided PET scan at 48 h following the rhTSH injection. After approximately 4 weeks off thyroid hormone, when her TSH measured 96.91 mIU/l, she ingested 32.4 MBq 124I. She received 124I PET/CT at the same time points, performed according to the same methods and by the same operators as she had after rhTSH administration.
As seen in Table 3, the LDpA for this individual’s local recurrence was tenfold higher and the mean LDpA for her distant metastases nearly threefold higher after THW than after rhTSH administration.
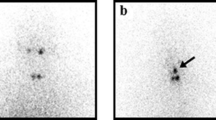
Figure 1 compares 124I PET/CT images for the patient under rhTSH stimulation (a, c) versus under THW stimulation (b, d). As seen in the figures, THW-aided scans (using 32.4 MBq 124I) provided superior image quality with respect to a cervical metastasis (Fig. 1a, b) and unlike the rhTSH-aided scans (using 27.7 MBq 124I), visualised the adrenal gland metastasis (Fig. 1c, d).
Discussion
The present retrospective study and within-patient comparison aimed to apply 124I PET/CT, the state-of-the-art method of measuring radioiodine kinetics in DTC [20], to answer an important clinical question: does use of rhTSH as a stimulation method for 131I treatment of iodine-avid DTC metastases deliver an equivalent radiation dose to such lesions as does THW? As noted in the “Introduction” section, there is a paucity of published data on this issue using any dosimetric method. In our retrospective comparison, we sought to capitalise on data from a relatively large group of patients, while our within-patient comparison had the advantages of being prospective and controlled.
Taken together, the results of our work were suggestive: rhTSH delivered appreciably lower doses than did THW in both our retrospective study (Table 2) and our within-patient comparison (Table 3). However, in the retrospective study, the primary end-point was non-significant despite multiple significant intergroup differences in baseline patient characteristics indicating more advanced, poorer prognosis and more pretreated disease in the rhTSH group. Additionally, the prospective within-patient comparison involved only a single individual and hence must be considered anecdotal. Therefore, at the end of the day, the present study must be regarded as inconclusive. Nonetheless, we believe that our data provide a useful input to clinical decision making until such time as data from a large, prospective, within-patient lesion dose comparison become available.
Our observations of lower tumoural radiation doses per GBq of administered activity after rhTSH than after THW agree with the findings of the only previously published comparison of lesional radiation dose under the two TSH stimulation methods, a small pilot study by Pötzi et al. [17]. That prospective investigation included four patients with ten metastases in total (seven lung, two bone and one cervical), who served as their own controls. The investigators measured kinetics with 123I scintigraphy/single photon emission CT. Because of uncertainties surrounding volumetry of metastases, especially small lesions, Pötzi and coworkers chose to use lesion cumulative activity in μCi*h as a surrogate marker for lesion dose. They found that in all ten lesions the cumulative activity was higher after THW than after rhTSH administration; the mean ± SD (median) activities were 5.6 ± 13.7 μCi*h (1.3 μCi*h) with rhTSH versus 9.5 ± 26.3 μCi*h (3.4 μCi*h) with THW, and this difference was statistically significant (p < 0.05).
One may speculate about factors that might contribute to our observations of lower LDpAs with rhTSH administration than with THW. As noted above, in our retrospective study, one such factor may be later-stage disease in the rhTSH patients than in their THW counterparts. The significantly different profiles of the treatment groups were unsurprising given the lack of formal treatment group inclusion criteria inherent in the retrospective nature of this study. Our mixed model ANCOVA that calculated the group mean LDpAs did adjust for six statistically significant differences between the groups in variables related to the advanced disease itself or to greater prior radioiodine exposure. Nonetheless, this adjustment may not have fully compensated for a more unfavourable outlook in the rhTSH patients. For example, the adjustment did not factor in their far greater proportion of lesions affecting the bone (41.4 vs 9.1%), which a large study [32] has shown to be significantly associated with poor radiation responsiveness. Nor did our analysis factor in the rhTSH group’s older age and greater prevalences of N1 or M1 disease, i.e. nodal or distant metastases at diagnosis, and of follicular histology. While these differences did not attain statistical significance, they still may have been biologically and clinically relevant.
Another potential explanatory factor for the lower mean LDpAs with rhTSH than with THW is the contrasting characteristics of the two stimulation methods: the TSH elevation achieved with rhTSH is sharper but much shorter lived than that attained by THW [33]. More protracted TSH stimulation might result in enhanced DTC cell expression or trafficking of NIS, which might lead to higher radioiodine uptake. Studies correlating the level of NIS on DTC cell surfaces with the area under the curve of TSH elevation are needed to investigate this possibility.
Of note, we have reported elsewhere [34] that in a retrospective comparison rhTSH and THW groups did not differ statistically with respect to thyroid remnant dose per GBq of administered activity which, indeed, was numerically higher with rhTSH. That finding dovetails with observations of ablation success rates that were not statistically different, i.e. healthy thyroid cell eradication rates, for the two methods in all seven clinical studies [7, 10, 35–39] comparing rhTSH-aided ablation when the radioiodine was given at the indicated 24 h after the second rhTSH injection against THW ablation.
Moreover, the large retrospective study of Tuttle et al. [38] noted low medium-term DTC recurrence rates that were not statistically different in rhTSH and THW ablation groups, both of which were overwhelmingly M0. This observation awaits confirmation in longer-term follow-up. However, the finding of Tuttle et al. suggests that at the micrometastatic level large radioiodine activities may have similar antitumour efficacy, presumably reflecting similar radiation doses, when aided by either TSH stimulation method. NIS might be sufficiently abundant on healthy thyroid remnant cell surfaces or even DTC micrometastatic cell surfaces that the difference (if any) between rhTSH and THW in their degree of NIS stimulation remains subclinical in these settings. In macrometastatic DTC cells with presumably greater NIS deficiencies, the difference in stimulation might be clinically apparent. It should be noted that rhTSH is not indicated for thyroid remnant ablation in patients with evidence of distant metastasis at the time of the procedure.
It has been speculated that “cold iodine” from continued thyroid hormone therapy might interfere with therapeutic radioiodine uptake [36, 40]. However, in our retrospective study, the treatment groups did not differ statistically in median urinary iodine excretion. Moreover, in neither that study nor our within-patient comparison did urinary iodine excretion levels ever exceed the 150 μg/l level widely considered to reflect clinically relevant iodine excess. Similarly, urinary iodine excretion did not differ significantly in the rhTSH phase versus the THW phase of the Pötzi et al. study [17].
We found wide inter- and intra-patient variation in tumour dose with either stimulation method, including lesions with a very low LDpA precluding safe and effective RIT. This observation was in line with our earlier results [20] and those of others performing post-therapeutic dosimetry using 131I aided by rhTSH [16] or pre-therapeutic dosimetry using 124I aided by THW [41] or by an unspecified stimulation method [42]. These findings highlight the need to individualise radioiodine activities and therapeutic modalities for patients with advanced DTC, and the value of 124I PET/CT in helping to do so [20].
The present study and within-patient comparison have certain limitations besides those mentioned earlier. First, because small numbers of lesions at a given site in a given treatment group not infrequently precluded meaningful statistical analyses, our retrospective study did not compare the mean LDpAs of the TSH stimulation methods by site of metastasis. This could diminish generalisability to specific patient types.
Second, 124I PET/CT is influenced by a variety of physical and radiobiological uncertainties that can lead to an error margin of up to 30%, as we have discussed in greater depth elsewhere [25]. However, these uncertainties may be presumed to similarly affect both treatment groups in the retrospective study and both phases of the within-patient comparison, given that essentially identical 124I PET/CT methodology was applied under rhTSH and THW stimulation. We have not assessed methodology-related error rates in euthyroidism versus hypothyroidism, however.
Lastly, though in the retrospective study mean 124I activities did not differ statistically between the treatment groups, in the within-patient comparison a 17% larger activity was given with THW than with rhTSH (Table 3; no statistical test performed). However, this discrepancy is unlikely to have influenced the LDpA findings in that comparison, since our methodology normalises that variable to the administered activity.
It is worth noting that based on the data in our retrospective study the mean LDpA after rhTSH, 30.6 Gy/GBq, would be sufficiently high that treatment with a typical empirical fixed 7.4 GBq activity would deliver 226 Gy to an “average metastasis”, well above the 80–100 Gy that is widely considered to be effective. However, based on the data in our within-patient comparison, the subject would receive adequate lesion doses of 86–111 Gy with THW, but insufficient lesion doses of 11–30 Gy with rhTSH. These estimates suggest that if our findings regarding relative LDpAs between rhTSH and THW are borne out, differences in this variable might have little clinical relevance in many, but not all instances.
In conclusion, we found some suggestions, but no statistically significant evidence, that rhTSH stimulation may result in a lower radiation dose to advanced DTC lesions per GBq of administered activity than does THW stimulation. A large, well-controlled, prospective, within-patient study is needed to resolve the clinically important question of whether lesion doses significantly differ between the two TSH stimulation methods. Until data from such a study become available, we suggest reserving rhTSH-aided treatment of metastatic DTC to patients who are at high risk of tumour progression under THW or unable to tolerate THW, or to cases in which it is essential to preserve baseline abilities to work or study despite RIT.
References
Dohán O, De la Vieja A, Paroder V, Riedel C, Artani M, Reed M, et al. The sodium/iodide symporter (NIS): characterization, regulation, and medical significance. Endocr Rev 2003;24:48–77.
Bruno R, Ferretti E, Tosi E, Arturi F, Giannasio P, Mattei T, et al. Modulation of thyroid-specific gene expression in normal and nodular human thyroid tissues from adults: an in vivo effect of thyrotropin. J Clin Endocrinol Metab 2005;90:5692–7.
Schlumberger M, Lacroix L, Russo D, Filetti S, Bidart JM. Defects in iodide metabolism in thyroid cancer and implications for the follow-up and treatment of patients. Nat Clin Pract Endocrinol Metab 2007;3:260–9.
Luster M, Felbinger R, Dietlein M, Reiners C. Thyroid hormone withdrawal in patients with differentiated thyroid carcinoma: a one hundred thirty-patient pilot survey on consequences of hypothyroidism and a pharmacoeconomic comparison to recombinant thyrotropin administration. Thyroid 2005;15:1147–55.
Schroeder PR, Haugen BR, Pacini F, Reiners C, Schlumberger M, Sherman SI, et al. A comparison of short-term changes in health-related quality of life in thyroid carcinoma patients undergoing diagnostic evaluation with recombinant human thyrotropin compared with thyroid hormone withdrawal. J Clin Endocrinol Metab 2006;91:878–84.
Borget I, Corone C, Nocaudie M, Allyn M, Iacobelli S, Schlumberger M, et al. Sick leave for follow-up control in thyroid cancer patients: comparison between stimulation with Thyrogen and thyroid hormone withdrawal. Eur J Endocrinol 2007;156:531–8.
Taïeb D, Sebag F, Cherenko M, Baumstarck-Barrau K, Fortanier C, Farman-Ara B, et al. Quality of life changes and clinical outcomes in thyroid cancer patients undergoing radioiodine remnant ablation (RRA) with recombinant human TSH (rhTSH): a randomized controlled study. Clin Endocrinol (Oxf) 2009;71:115–23.
Duntas LH, Biondi B. Short-term hypothyroidism after levothyroxine-withdrawal in patients with differentiated thyroid cancer: clinical and quality of life consequences. Eur J Endocrinol 2007;156:13–9.
Haugen BR, Pacini F, Reiners C, Schlumberger M, Ladenson PW, Sherman SI, et al. A comparison of recombinant human thyrotropin and thyroid hormone withdrawal for the detection of thyroid remnant or cancer. J Clin Endocrinol Metab 1999;84:3877–85.
Pacini F, Ladenson PW, Schlumberger M, Driedger A, Luster M, Kloos RT, et al. Radioiodine ablation of thyroid remnants after preparation with recombinant human thyrotropin in differentiated thyroid carcinoma: results of an international, randomized, controlled study. J Clin Endocrinol Metab 2006;91:926–32.
Luster M, Lippi F, Jarzab B, Perros P, Lassmann M, Reiners C, et al. rhTSH-aided radioiodine ablation and treatment of differentiated thyroid carcinoma: a comprehensive review. Endocr Relat Cancer 2005;12:49–64.
Robbins RJ, Driedger A, Magner J, U.S. and Canadian Thyrogen Compassionate Use Program Investigator Group. Recombinant human thyrotropin-assisted radioiodine therapy for patients with metastatic thyroid cancer who could not elevate endogenous thyrotropin or be withdrawn from thyroxine. Thyroid 2006;16:1121–30.
Robbins RJ, Voelker E, Wang W, Macapinlac HA, Larson SM. Compassionate use of recombinant human thyrotropin to facilitate radioiodine therapy: case report and review of literature. Endocr Pract 2000;6:460–4.
Rotman-Pikielny P, Reynolds JC, Barker WC, Yen PM, Skarulis MC, Sarlis NJ. Recombinant human thyrotropin for the diagnosis and treatment of a highly functional metastatic struma ovarii. J Clin Endocrinol Metab 2000;85:237–44.
Song H, He B, Prideaux A, Du Y, Frey E, Kasecamp W, et al. Lung dosimetry for radioiodine treatment planning in the case of diffuse lung metastases. J Nucl Med 2006;47:1985–94.
de Keizer B, Brans B, Hoekstra A, Zelissen PM, Koppeschaar HP, Lips CJ, et al. Tumour dosimetry and response in patients with metastatic differentiated thyroid cancer using recombinant human thyrotropin before radioiodine therapy. Eur J Nucl Med Mol Imaging 2003;30:367–73.
Pötzi C, Moameni A, Karanikas G, Preitfellner J, Becherer A, Pirich C, et al. Comparison of iodine uptake in tumour and nontumour tissue under thyroid hormone deprivation and with recombinant human thyrotropin in thyroid cancer patients. Clin Endocrinol (Oxf) 2006;65:519–23.
Park S-G, Reynolds JC, Brucker-Davis F, Whatley M, McEllin K, Maxted D, et al. Iodine kinetics during I-131 scanning in patients with thyroid cancer: comparison of studies with recombinant human TSH (rhTSH) vs. hypothyroidism [abstract 49]. J Nucl Med 1996;37:15P.
Ladenson PW, Braverman LE, Mazzaferri EL, Brucker-Davis F, Cooper DS, Garber JR, et al. Comparison of administration of recombinant human thyrotropin with withdrawal of thyroid hormone for radioactive iodine scanning in patients with thyroid carcinoma. N Engl J Med 1997;337:888–96.
Freudenberg L, Jentzen W, Görges R, Petrich T, Marlowe RJ, Knust J, et al. 124I-PET dosimetry in advanced differentiated thyroid cancer: therapeutic impact. Nuklearmedizin 2007;46:121–8.
Fleming I, Cooper JS, Henson DE, Hutter RVP, Kennedy BJ, editors. AJCC cancer staging manual. 5th ed. Philadelphia: Lippincott-Raven; 1997.
Freudenberg L, Bockisch A, Jentzen W. 124I positron emission tomographic dosimetry and positron emission tomography/computed tomography imaging in differentiated thyroid cancer. In: Biersack H, Grunwald F, editors. Thyroid cancer. 2nd ed. Berlin: Springer; 2005.
Weinreich R, Knust EJ. Quality assurance of iodine-124 produced via the nuclear reaction 124Te(d, 2n)124I. J Radioanal Nucl Chem 1996;213:253–61.
Knust EJ, Dutschka K, Weinreich R. Preparation of 124I solutions after thermodistillation of irradiated 124TeO2 targets. Appl Radiat Isot 2000;52:181–4.
Jentzen W, Freudenberg L, Eising EG, Sonnenschein W, Knust J, Bockisch A. Optimized 124I PET dosimetry protocol for radioiodine therapy of differentiated thyroid cancer. J Nucl Med 2008;49:1017–23.
Snyder W, Ford MR, Warner GG, Watson SB. S, absorbed dose per unit cumulated activity for selected radionuclides and organs. New York: Society of Nuclear Medicine; 1975.
Furhang EE, Larson SM, Buranapong P, Humm JL. Thyroid cancer dosimetry using clearance fitting. J Nucl Med 1999;40:131–6.
Loevinger R, Budinger TF, Watson EE. MIRD primer for absorbed dose calculations. New York: Society of Nuclear Medicine; 1991.
Jentzen W, Freudenberg L, Eising EG, Heinze M, Brandau W, Bockisch A. Segmentation of PET volumes by iterative image thresholding. J Nucl Med 2007;48:108–14.
Görges R, Eising EG, Fotescu D, Renzing-Köhler K, Frilling A, Schmid KW, et al. Diagnostic value of high-resolution B-mode and power-mode sonography in the follow-up of thyroid cancer. Eur J Ultrasound 2003;16:191–206.
Freudenberg LS, Antoch G, Jentzen W, Pink R, Knust J, Görges R, et al. Value of (124)I-PET/CT in staging of patients with differentiated thyroid cancer. Eur Radiol 2004;14: 2092–8.
Durante C, Haddy N, Baudin E, Leboulleux S, Hartl D, Travagli JP, et al. Long-term outcome of 444 patients with distant metastases from papillary and follicular thyroid carcinoma: benefits and limits of radioiodine therapy. J Clin Endocrinol Metab 2006;91:2892–9.
Rosário PW, Salles DS, Purisch S. Area under the curve of TSH after levothyroxine withdrawal versus administration of recombinant human TSH (rhTSH): possible implications for tumor growth. Arq Bras Endocrinol Metabol 2009;53:767–70.
Freudenberg LS, Frömke C, Petrich T, Marlowe RJ, Koska WW, Brandau W, et al. Thyroid remnant dose: 124I-PET/CT dosimetric comparison of rhTSH versus thyroid hormone withholding before radioiodine remnant ablation in differentiated thyroid cancer. Exp Clin Endocrinol Diabetes 2010;118:393–9.
Robbins RJ, Larson SM, Sinha N, Shaha A, Divgi C, Pentlow KS, et al. A retrospective review of the effectiveness of recombinant human TSH as a preparation for radioiodine thyroid remnant ablation. J Nucl Med 2002;43:1482–8.
Barbaro D, Boni G, Meucci G, Simi U, Lapi P, Orsini P, et al. Recombinant human thyroid-stimulating hormone is effective for radioiodine ablation of post-surgical thyroid remnants. Nucl Med Commun 2006;27:627–32.
Rosário PW, Borges MA, Purisch S. Preparation with recombinant human thyroid-stimulating hormone for thyroid remnant ablation with 131I is associated with lowered radiotoxicity. J Nucl Med 2008;49:1776–82.
Tuttle RM, Brokhin M, Omry G, Martorella AJ, Larson SM, Grewal RK, et al. Recombinant human TSH-assisted radioactive iodine remnant ablation achieves short-term clinical recurrence rates similar to those of traditional thyroid hormone withdrawal. J Nucl Med 2008;49:764–70.
Chianelli M, Todino V, Graziano FM, Panunzi C, Pace D, Guglielmi R, et al. Low-activity (2.0 GBq; 54 mCi) radioiodine post-surgical remnant ablation in thyroid cancer: comparison between hormone withdrawal and use of rhTSH in low-risk patients. Eur J Endocrinol 2009;160:431–6.
Löffler M, Weckesser M, Franzius C, Kies P, Schober O. Iodine excretion during stimulation with rhTSH in differentiated thyroid carcinoma. Nuklearmedizin 2003;42:240–3.
Eschmann SM, Reischl G, Bilger K, Kupferschläger J, Thelen MH, Dohmen BM, et al. Evaluation of dosimetry of radioiodine therapy in benign and malignant thyroid disorders by means of iodine-124 and PET. Eur J Nucl Med Mol Imaging 2002;29:760–7.
Sgouros G, Kolbert KS, Sheikh A, Pentlow KS, Mun EF, Barth A, et al. Patient-specific dosimetry for 131I thyroid cancer therapy using 124I PET and 3-dimensional-internal dosimetry (3D-ID) software. J Nucl Med 2004;45:1366–72.
Acknowledgments
LSF and TP have received speakers’ fees and RJM fees for editorial/logistical assistance on prior rhTSH-related papers from Genzyme Corporation, the rhTSH manufacturer. The University of Essen and MHH Departments of Nuclear Medicine received grants from Genzyme supporting 124I PET/CT data analysis in general, and the prospective in-patient comparison reported in this paper, respectively.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Freudenberg, L.S., Jentzen, W., Petrich, T. et al. Lesion dose in differentiated thyroid carcinoma metastases after rhTSH or thyroid hormone withdrawal: 124I PET/CT dosimetric comparisons. Eur J Nucl Med Mol Imaging 37, 2267–2276 (2010). https://doi.org/10.1007/s00259-010-1565-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-010-1565-3