Abstract
Purpose
We hypothesized that, because of persistent stunning, the extent of post-treatment functional abnormalities detected using gated single-photon emission computed tomography (SPECT) could be representative of the initial risk area in acute myocardial infarction (AMI) treated by reperfusion therapy.
Materials and methods
In 48 AMI patients, we acquired two 99mTc-sestamibi gated SPECT studies (at admission with tracer injection before treatment and at discharge 5 to 10 days later). We assessed the myocardial salvage defined by the admission minus predischarge summed rest score, and we compared it with the value obtained by subtracting the extent of perfusion defect from the extent of wall motion or wall thickening abnormalities in predischarge gated SPECT. Myocardial salvage was expressed as salvage index (salvaged myocardium divided by initial risk area).
Results
There was a good correlation between summed rest score salvage index and wall motion (Spearman’s ρ = 0.754, p < 0.0001) or wall thickening salvage index (Spearman’s ρ = 0.798, p < 0.0001). The wall thickening salvage index was able to classify correctly the patients that had a summed rest score salvage index ≥ 0.10 with 73% sensitivity, 88% specificity, and 83% accuracy. The wall motion salvage index was highly sensitive (91%) but poorly specific (13%, p < 0.002 vs wall thickening salvage index) and less accurate (69%, p < 0.05 vs wall thickening salvage index).
Conclusions
99mTc-sestamibi gated SPECT allows assessing myocardial salvage using only post-treatment data. The salvage index derived using wall thickening as surrogate of admission perfusion defect correlates well with the salvage index measured by comparing pre- and post-treatment perfusion defects.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The success of reperfusion therapy in acute myocardial infarction (AMI) is related to the amount of myocardium at risk, the presence of residual blood flow or collateral circulation, and the duration of coronary occlusion [1-4]. These factors are the major determinants of the extent of myocardial salvage that can be obtained and, thus, of the final infarct size [5]. In turn, infarct size is the main determinant of a patient’s benefit in terms of functional recovery and clinical outcome after reperfusion therapy [6, 7].
Single-photon emission computed tomography (SPECT) with 99mTc-labeled myocardial perfusion agents is considered a most reliable method to identify salvaged myocardium. Perfusion SPECT performed after the tracer has been injected before reperfusion therapy visualizes the area at risk. A second SPECT study performed days to weeks after an intervention permits to assess the final infarct size [8-11]. The difference between the two uptake defects represents the salvaged myocardium. Therefore, this approach allows the direct measurement of myocardial salvage, differently from what happens using the indirect markers of reperfusion success, such as rapid resolution of ST-segment elevation [12] or myocardial blush [13]. Unfortunately, the need to avoid any unnecessary delay in reperfusion treatment limits the feasibility of prereperfusion 99mTc-sestamibi SPECT. Therefore, in clinical practice, the role of 99mTc-sestamibi SPECT for estimating the success of reperfusion therapy is mainly based on the measurement of final infarct size, and no data about the initial risk area are usually provided [14, 15]. After prolonged acute ischemic injury and even if reperfusion has been successful, myocardial stunning may occur and usually lasts for days to weeks [16]. Myocardial stunning is associated with a perfusion-function mismatch [17]. Gated SPECT is an accurate and well-validated method for simultaneously assessing perfusion, and regional and global left ventricular function [18]. As gated SPECT allows the assessment of regional function and perfusion without realignment problems, we hypothesized that the size of the stunned asynergic area in post-treatment gated SPECT could still be representative of the extent of initial area at risk and that the difference between this area and the post-treatment perfusion defect size could be an approximate estimate of salvaged myocardium.
Materials and methods
Patient population
Our patient population consisted of the patients enroled in our institution in the context of the Brave-2 trial [19]. A total of 50 patients were referred to our laboratory for the Brave-2 trial. ST elevation AMI diagnosis was based on chest pain episode lasting ≥20 min between 12 and 48 h before presentation and ST-segment elevation ≥0.1 mV in two or more adjacent limb leads or ≥0.2 mV in two or more contiguous precordial leads or new pathological Q-waves on surface electrocardiogram. Exclusion criteria included persistent anginal chest pain, cardiogenic shock, electrical instability, severe congestive heart failure and/or pulmonary edema, or previous stroke (within the last 3 months); before thrombolysis for index infarction, recent percutaneous coronary intervention (within the last 30 days), active bleeding or bleeding diatheses, recent trauma or major surgery (during the last month), relevant hematologic deviations or malignancies, known or suspected pregnancy, inability to comply with study procedures, and unwillingness or inability to provide written informed consent for participation [19].
Study protocol
The 50 Brave-2 trial eligible patients at our institution underwent the 99mTc-sestamibi injection (740 MBq) at admission before randomization. For that reason, in the invasive therapy group, the injection was performed before reperfusion. Admission gated SPECT imaging at rest was obtained after 1 h in patients randomized to conservative strategy and after coronary angiography and reperfusion in patients randomized to invasive therapy. A second resting gated SPECT study after injection of the same tracer dosage (predischarge gated SPECT) was performed 5 to 10 days later (mean, 5.9 ± 1 days) [19]. In two patients, however, the gated acquisition was unreliable because of technical default in one case and because of atrial fibrillation in the other subject. Therefore, the final study cohort of the present study included 48 patients (mean age, 65.4 ± 11 years, range 41−84). All patients gave informed consent to participate in the study, which was approved by the Ethics Committees of our institution.
Gated SPECT
In 23 patients, scintigraphic images were acquired using a dual-head gamma camera (Skylight, Philips, Milpitas, CA, USA) and in 25 patients using a variable triple-head gamma camera (Irix, Marconi-Philips, Cleveland, OH, USA). Both gamma cameras were equipped with high-resolution collimators and employed a 15% window centered on the 140-keV photopeak of 99mTc. SPECT was acquired in step-and-shoot mode using a 180° elliptical orbit, matrix size 64 × 64, 8 frame/cardiac cycle for both gamma camera systems, with 32 projections and 60 s per projection, or with 34 projections and 30 s per projection, respectively, for the Skylight and for the Irix system. SPECT images were reconstructed using filtered back-projection without attenuation or scatter correction and realigned along the heart axis. For each patient, the same gamma camera was used for the two SPECT acquisitions.
Data analysis
For perfusion and function analysis, the left ventricular polar map was divided into 20 segments. Regional myocardial perfusion, wall motion, and thickening were assessed visually by one blinded experienced observer, unaware of patient’s data and image sequence, and they were scored using a five-point scale (0 = normal, 1 = mildly reduced, 2 = moderately reduced, 3 = severely reduced, 4 = absent uptake) [20], a six-point scale (0 = normal, 1 = mild hypokinesia, 2 = moderate hypokinesia, 3 = severe hypokinesia, 4 = akinesia, 5 = dyskinesia), and a four-point scale (0 = normal, 1 = mildly impaired, 2 = moderately impaired, and 3 = severely impaired thickening), respectively [21].
Because these widely used scoring schemes are heterogeneous, to allow the comparison between perfusion and wall motion or wall thickening, the scores were translated in extent of abnormality on the polar maps and expressed as percentage of the left ventricular wall. Therefore, the extent of any abnormality (perfusion, wall motion, or wall thickening) was
As the perfusion and wall motion scoring schemes included a higher number of degrees, we did not consider abnormal the segments with borderline perfusion or wall motion anomalies (score = 1). We used as reference to establish the salvaged myocardium the difference between the admission and the predischarge summed rest score. The salvaged myocardium divided by the initial risk area defined the salvage index; according to prior data, a salvage index < 0.10 was considered to indicate negligible treatment benefit [22]. The reference salvage index obtained using the summed rest score was compared with the salvage index calculated as (1) the extent of wall motion abnormalities in predischarge gated SPECT minus perfusion defect extent in predischarge gated SPECT divided by the extent of wall motion anomalies in predischarge gated SPECT (wall motion salvage index) and (2) the extent of wall thickening in predischarge gated SPECT minus perfusion defect extent in predischarge gated SPECT divided by extent of wall thickening anomalies in predischarge gated SPECT (wall thickening salvage index).
Statistical analysis
Continuous variables are expressed as mean ± standard deviation. Discrete variables are expressed as median and interquartile range. The comparisons between groups were performed with the Wilcoxon test for dependent samples. The correlation between variables was evaluated using the Spearman’s ρ. The comparison of proportion was made using the Fisher’s exact test. A p value < 0.05 was considered statistically significant.
Results
General findings
The patient population included 34 men and 14 women. Of them, 28 patients were assigned to the invasive group and 20 patients to the conservative group. No patient had history of prior percutaneous coronary intervention and/or coronary artery bypass grafting. As regards the infarct location, 18 patients had anterior, 23 inferior, and 7 lateral infarction. Table 1 summarizes the characteristics of the patient population.
Myocardial perfusion
At admission, the median (25th, 75th percentiles) of summed rest score was 21.5 (14.5, 32), and the extent of perfusion abnormalities was 35% (25%, 50%). The median predischarge summed rest score was 17 (6.25, 22.5; p < 0.0001 vs admission) and the extent of perfusion abnormalities was 30% (10%, 40%; p < 0.0001 vs admission). The salvage index derived from the admission vs predischarge summed rest score was 0.33 (0, 0.57). The salvage index derived from percent extent of perfusion defects was 0.25 (0, 0.56). This value showed a close correlation with the summed rest score salvage index, with Spearman’s ρ = 0.943 (p < 0.0001).
Salvage index according to functional vs perfusion abnormalities in predischarge gated SPECT
The wall motion salvage index was 0.44 (0.27, 0.60). The correlation between the summed rest score salvage index and the wall motion salvage index was good, with Spearman’s ρ = 0.754, p < 0.0001. The wall thickening salvage index was 0.25 (0, 0.60). The correlation between summed rest score salvage index and wall thickening salvage index was good, with Spearman’s ρ = 0.798, p < 0.0001.
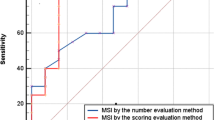
The sensitivity, specificity, and accuracy of a wall motion salvage index ≥0.10 for recognizing a summed rest score salvage index ≥0.10 were 91, 13, and 69%, respectively. Conversely, a wall thickening salvage index ≥0.10 showed 73% sensitivity, 88% specificity (p < 0.002 vs wall motion salvage index), and 83% accuracy (p < 0.05 vs wall motion salvage index) for recognizing a summed rest score salvage index ≥0.10 (Fig. 1). Moreover, the wall thickening salvage index was able to classify correctly as belonging to the same quartile as the summed rest score salvage index 10 of 13 patients of the lower quartile, 10 of 14 patients of the upper quartile, and 13 of 21 patients of the two intermediate quartiles.
Discussion
In the present investigation, we tested the hypothesis that the stunned asynergic area size in predischarge gated SPECT could still be representative of the extent of initial ischemia (myocardium at risk) and that the difference between this area and the corresponding perfusion defect size could be an approximate estimate of salvaged myocardium. This hypothesis was based on the concept that myocardial stunning persists days to weeks after reperfusion therapy, and it is associated with a flow-functional mismatch [17]. For this particular aim, we took advantage from the use of gated SPECT that is very well suited to allow the direct comparison of regional functional and perfusion abnormalities, without realignment problems [18].
We registered a good correlation between the salvage index derived from admission vs predischarge summed rest score, which we used as reference standard, and the salvage indexes derived from the difference in predischarge gated SPECT between the extent of wall motion or wall thickening abnormalities and the extent of perfusion defects. Our results showed that the correlation between summed rest score salvage index and the salvage index derived using the wall thickening abnormalities as surrogate for the admission perfusion defect was higher than the corresponding value derived using the wall motion abnormalities. The latter approach was indeed highly sensitive but unacceptably poorly specific for recognizing the presence of summed rest score salvage index ≥0.10 and, hence, to exclude a negligible treatment benefit [22]. On the other hand, the wall thickening salvage index was significantly more accurate and, particularly, much more specific in identifying the patients with a summed rest score salvage index ≥0.10. Moreover, the wall thickening salvage index was able to correctly classify the majority of the patients (33 of 48 = 69%) in the same quartile of the summed rest score salvage index. The superiority of wall thickening over wall motion for the detection of myocardial stunning could be explained by the differences between wall motion and wall thickening abnormalities already described by others using gated SPECT visual assessment in the setting of myocardial infarction [23]. However, we cannot exclude some influence of the relatively prolonged delay of the second gated SPECT on the difference in accuracy between wall motion and thickening for the estimate of the salvage index.
The importance of achieving an estimate of area at risk in the evaluation of AMI cannot be overemphasized because only the direct measurement of myocardial salvage allows assessment of the individual response to intervention in AMI [24]. Moreover, myocardial salvage has a major prognostic meaning [25]. The measurement of area at risk by 99mTc-sestamibi SPECT injected during coronary occlusion has been extensively validated, and the salvaged myocardium can be accurately obtained by the comparison with a subsequent pre discharge rest perfusion scan that identifies the final infarct size [8-11], but the early images can be challenging to obtain. A retrospective evaluation of the area at risk on an image acquired after the acute presentation would be highly desirable. Various experimental and human studies have aimed to this goal. The fatty acid tracer 123I-β-methyl-p-iodophenyl-pentadecanoic acid (BMIPP) has been shown to demonstrate the persistence of decrease in β-oxidation after inducible ischemia, and thus, the BMIPP uptake defect early after myocardial infarction could approximate the area at risk in comparison with the 201Tl perfusion defect showing the infarct size [26]. The unavailability of BMIPP in most countries has limited the feasibility of this combined tracer method. In the experimental animal, 18F-fluorodeoxyglucose also shows persistent glucose metabolism derangement after ischemia [27]. Using an approach quite similar to ours, Main et al. identified the stunned, reperfused myocardium after AMI as perfusion-contraction mismatch in real-time myocardial contrast echocardiography performed in a mean of 2.2 days after hospital admission [28]. In this instance, the total extent of abnormal contraction would be the expression of the risk area and the contrast defect of the final infarct size. The several advantages of echocardiography over the other imaging modalities would support the use of this method; however, poor acoustic window and the additional technical problems specific to myocardial contrast echocardiography could limit its feasibility and reliability in a minority of patients. Most recently, the comparison of T2 signal increase and late-gadolinium-enhancement in magnetic resonance imaging has been proposed, according to the hypothesis that T2-weighted sequences depict myocardial edema (and then the area at risk), while hyperenhancement is confined to necrotic tissue (and then corresponds to the final infarct size) [29]. The high resolution of magnetic resonance imaging makes this last approach very attractive, but so far no demonstration of its practicability and reliability in humans is available.
Our results must be evaluated taking into account the limitations of our study. A crucial issue to consider for the retrospective evaluation of the risk area is the time course of the changes of the parameter used to define the risk area itself. In our study, the pre discharge gated SPECT acquired five or more days after hospital admission could underestimate the area at risk because part of the stunning-related functional abnormality could have already disappeared. As above stated, this prolonged delay could have had as well some influence of the different accuracy of wall motion vs wall thickening salvage index. On the other hand, it must be noted that, in our series, the wall motion (but not the wall thickening) abnormalities still overestimate the area at risk. Certainly, it would be reasonable and highly recommended to anticipate the post-intervention gated SPECT acquisition to further improve the reliability of our combined approach. The patient population was quite small and heterogeneous, including both patients submitted to mechanical reperfusion and patients treated conservatively. Moreover, the number of patients with prior infarction was very small, and none had history of previous revascularization procedures. Therefore, further studies on cohorts that better represent the usual patient population submitted to percutaneous coronary intervention for AMI are warranted. In addition, our patients were admitted for AMI after a more prolonged delay than usual, and this could have affected the absolute rate of treatment success. However, each patient served as his/her own control, as the salvage index was assessed with an established method by means of the summed rest score. The criteria used to compare perfusion and functional data by translating the related scores in extent of abnormalities on the polar maps were somewhat arbitrary. Using the automatic definition of abnormalities in percent of left ventricle that is offered by various processing algorithms for gated SPECT could improve the reliability and reproducibility of our method. Further studies on larger patient population submitted to the same treatment within a more reasonable time frame will be needed to definitively establish the value of the estimate of salvaged myocardium by the comparison of functional vs perfusion abnormalities in a single post-treatment gated SPECT.
Conclusions
This study suggests that by comparing the extent of wall thickening and perfusion abnormalities in a single post-treatment gated SPECT, it is possible to have an approximate but clinically effective estimate of the salvage index in AMI patients. In spite of its limitations, the simplicity and feasibility of this assessment would support its use to define the success of reperfusion treatment in the individual patient and increases the diagnostic value of perfusion imaging using gated SPECT over its already established role in defining the infarct size. Further studies on larger and less selected patient populations using a more controlled timetable for the post-intervention gated SPECT are needed to confirm our preliminary results.
References
Gruppo Italiano per lo Studio della Streptochinasi nell’ Infarto Miocardico (GISSI). Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Lancet 1986;1:397-402.
Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003;361:13-20.
Stone GW, Cox D, Garcia E, Morice MC, Griffin J, Mattos L, et al. Normal flow (TIMI-3) before mechanical reperfusion therapy is an independent determinant of survival in acute myocardial infarction: analysis from the primary angioplasty in myocardial infarction trials. Circulation 2001;104:636-41.
Schöming A, Ndrepepa G, Kastrati A. Late myocardial salvage: time to recognize its reality in reperfusion therapy of acute myocardial infarction. Eur Heart J 2006;27:1900-7.
Christian TF, Schwartz RS, Gibbons RJ. Determinants of infarct size in reperfusion therapy for acute myocardial infarction. Circulation 1992;86:81-90.
Simoons ML, Serruys PW, van den Brand M, de Zwaan C, Res J, Verheugt FW, et al. Improved survival after early thrombolysis in acute myocardial infarction. A randomised trial by the Interuniversity Cardiology Institute in the Netherlands. Lancet 1985;2:578-82.
The GUSTO Angiographic Investigators. The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function, and survival after acute myocardial infarction. N Engl J Med 1993;329:1615-22. (Erratum in N Engl J Med 1994;330:516).
Gibbons MK, Mahmarian JJ, Chesebro JH, Wackers FJ. Feasibility of tomographic 99mTc-hexakis-2-methoxy-2-methylpropyl-isonitrile imaging for the assessment of myocardial area at risk and the effect of treatment in acute myocardial infarction. Circulation 1989;80:1277-85.
Santoro GM, Bisi G, Sciagrà R, Leoncini M, Fazzini PF, Meldolesi U. Single photon emission tomography with technetium-99 m hexakis 2-methoxyisobutyl isonitrile in acute myocardial infarction before and after thrombolytic treatment: assessment of salvaged myocardium and prediction of late functional recovery. J Am Coll Cardiol 1990;150:301-14.
Gibbons RJ, Holmes DR, Reeder GS, Bailey KR, Hopfenspinger MR, Gersh BJ. Immediate angioplasty compared with the administration of thrombolytic agent followed by conservative treatment for myocardial infarction. The Mayo Coronary Care Unit and Catheterization Laboratory Groups. N Engl J Med 1993;328:685-91.
Kastrati A, Mehilli J, Dirschinger J, Schricke U, Neverve J, Pache J, et al. Stent versus Thrombolysis for Occluded Coronary Arteries in Patients With Acute Myocardial Infarction (STOPAMI-2) Study. Myocardial salvage after coronary stenting plus abciximab versus fibrinolysis plus abciximab in patients with acute myocardial infarction: a randomised trial. Lancet 2002;359:920-5.
Santoro GM, Antoniucci D, Valenti R, Bolognese L, Buonamici P, Trapani M, et al. Rapid reduction of ST-segment elevation after successful direct angioplasty in acute myocardial infarction. Am J Cardiol 1997;80:685-9.
van’t Hof AW, Liem A, Suryapranata H, Hoorntje JC, de Boer MJ, Zijlstra F. Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction: myocardial blush grade. Zwolle Myocardial Infarction Study Group. Circulation 1998;97:2302-6.
Gibbons RJ, Miller TD, Christian TF. Infarct size measured by single photon emission computed tomographic imaging with (99m)Tc-sestamibi: a measure of the efficacy of therapy in acute myocardial infarction. Circulation 2000;101:101-8.
Klocke FJ, Baird MG, Lorell BH, Bateman TM, Messer JV, Berman DS, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging—executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 Guidelines for the Clinical Use of Cardiac Radionuclide Imaging). Circulation 2003;108:1404-8.
Braunwald E, Kloner RA. The stunned myocardium: prolonged, postischemic ventricular dysfunction. Circulation 1982;66:1146-9.
Spinelli L, Petretta M, Cuocolo A, Nicolai E, Acampa W, Vicario L, et al. Prediction of recovery of left ventricular dysfunction after acute myocardial infarction: comparison between 99mTc-sestamibi cardiac tomography and low-dose dobutamine echocardiography. J Nucl Med 1999;40:1683-92.
Sciagrà R, Leoncini M. Gated single-photon emission computed tomography. The present-day “one-stop-shop” for cardiac imaging. Q J Nucl Med Mol Imaging 2005;49:19-29.
Schömig A, Mehilli J, Antoniucci D, Ndrepepa G, Markwardt C, Di Pede F, et al. Beyond 12 hours Reperfusion Alternative Evaluation (BRAVE-2) Trial Investigators. Mechanical reperfusion in patients with acute myocardial infarction presenting more than 12 hours from symptom onset: a randomized controlled trial. JAMA 2005;293:2865-72.
Sharir T, Germano G, Waechter PB, Kavanagh PB, Areeda JS, Gerlach J, et al. A new algorithm for the quantitation of myocardial perfusion SPECT. II: validation and diagnostic yield. J Nucl Med 2000;41:720-7.
Germano G, Erel J, Lewin H, Kavanagh PB, Berman DS. Automatic quantitation of regional myocardial wall motion and thickening from gated technetium—99m sestamibi myocardial perfusion single-photon emission computed tomography. J Am Coll Cardiol 1997;30:1360-7.
Milavetz JJ, Giebel DW, Christian TF, Schwartz RS, Holmes DR, Gibbons RJ. Time to therapy and salvage in myocardial infarction. J Am Coll Cardiol 1998;31:1246-51.
Candell-Riera J, Pereztol-Valdes O, Aguade-Bruix S, Castell-Conesa J, Oiler-Martinez G, Simo M, et al. Regional wall motion and wall thickening visual scores from gated SPECT in anterior and infero-lateral myocardial infarctions. Nucl Med Commun 2004;25:201-6.
Pennell D. Myocardial salvage: retrospection, resolution, and radio waves. Circulation 2006;113:1821-3.
Ndrepepa G, Mehilli J, Schwaiger M, Schuhlen H, Nekolla S, Martinoff S, et al. Prognostic value of myocardial salvage achieved by reperfusion therapy in patients with acute myocardial infarction. J Nucl Med 2004;45:725-9.
Mochizuki T, Murase K, Higashino H, Miyagawa M, Sugawara Y, Kikuchi T, et al. Ischemic “memory image” in acute myocardial infarction of 123I-BMIPP after reperfusion therapy: a comparison with 99mTc-pyrophosphate and 201Tl dual-isotope SPECT. Ann Nucl Med 2002;16:563-8.
Di Carli MF, Prcevski P, Singh TP, Janisse J, Ager J, Muzik O, et al. Myocardial blood flow, function, and metabolism in repetitive stunning. J Nucl Med 2000;41:1227-34.
Main ML, Magalski A, Chee NK, Coen MM, Skolnick DG, Good TH. Full-motion pulse inversion power Doppler contrast echocardiography differentiates stunning from necrosis and predicts recovery of left ventricular function after acute myocardial infarction. J Am Coll Cardiol 2001;38:1390-4.
Aletras AH, Tilak GS, Natanzon A, Hsu LY, Gonzalez FM, Hoyt RF, et al. Retrospective determination of the area at risk for reperfused acute myocardial infarction with T2-weighted cardiac magnetic resonance imaging: histopathological and displacement encoding with stimulated echoes (DENSE) functional validations. Circulation 2006;113:1865-70.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sotgia, B., Sciagrà, R., Parodi, G. et al. Estimate of myocardial salvage in late presentation acute myocardial infarction by comparing functional and perfusion abnormalities in predischarge gated SPECT. Eur J Nucl Med Mol Imaging 35, 906–911 (2008). https://doi.org/10.1007/s00259-007-0663-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-007-0663-3