Abstract
Purpose
While CT/MR enteroclysis provides excellent anatomical details, it fails to provide information on metabolic activity of the inflammatory lesions of the intestine. We conceptualized a fusion of metabolic imaging techniques such as PET and an anatomical imaging modality such as CT enteroclysis to derive information both on morphological details and functional activity of lesions at the same time.
Patients and methods
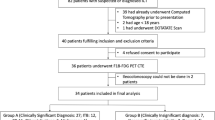
In a prospective study, we included 17 adult patients with newly diagnosed inflammatory diseases of the intestine. Low dose whole body PET-CT scan was obtained first, which began at approximately 60 min after injection of 10 mCi of 18fluoro-deoxyglucose (FDG). Subsequently, PET-CT enteroclysis of the abdomen was performed after infusion of 2 l of 0.5% methylcellulose through a naso-jejunal catheter.
Results
Fourteen patients had abnormal and three had normal PET-CT enteroclysis studies. Twenty-three segments of small intestine and 27 segments of large intestine showed increased FDG uptake. The detection rate of PET-CT enteroclysis was significantly higher (total =50 segments, 23 segments of small intestine and 27 segments of large intestine) as compared with barium studies (16 segments of small intestine) and colonoscopy (17 segments of large intestine) combined together (total =33 segments). In addition PET-CT enteroclysis showed extra-luminal FDG uptake (lymph nodes in two, sacroilitis in two, and mesenteric fat proliferation in five).
Conclusions
As a single investigation, PET-CT enteroclysis detects a significantly higher number of lesions both in the small and large intestine in comparison to that detected by conventional barium and colonoscopy combined together. This technique is non-invasive, feasible and very promising.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Information on the intestinal lumen, intestinal wall and the surrounding structures including lymph nodes is required for a complete evaluation of the intestine. One also needs to know about the length, site, multiplicity and activity of the stricture(s), if present. The assessment of the intestinal lumen has traditionally been done by conventional barium studies including barium meal follow through and small-bowel enteroclysis [1]. While enteroclysis provides information on the size and site of intestinal strictures, it fails to provide information on the activity of the strictures and surrounding structures. Much interest has been focused on computerized tomography (CT) enteroclysis and magnetic resonance (MR) enteroclysis in recent times to overcome the individual deficiencies of CT/MRI (no distention of the small intestine) and conventional enteroclysis (no extraluminal information) [1]. Both the CT enteroclysis and MR enteroclysis are reported to be highly accurate in depicting mucosal abnormalities and extraintestinal complications in patients with inflammatory diseases of the intestine [1]. Although these techniques provide excellent anatomical information, they fail to show the metabolic status of the disease activity. Small intestinal endoscopic techniques such as capsule endoscopy and double balloon enteroscopy hold a lot of promise for evaluation of the intestinal lumen; however, they fail to provide information on the intestinal wall and surrounding structures. Therefore, they are combined with a cross-sectional imaging technique such as CT enteroclysis or more often MR enteroclysis [2]. Therefore, we conceptualized a fusion of a metabolic imaging technique like positron emission tomography (PET) and an anatomical imaging modality like CT enteroclysis to derive information both on the morphological details and the functional activity of the lesions at the same time.
PET is now a well-established functional imaging technique and is widely used in the management of various cancers [3–5]. Fusion of PET with CT (PET-CT) provides morphological localization of the metabolically active focus/foci. This technique exploits the property of viable malignant cells, which have higher uptake and metabolism of glucose [6]. Increase in the glucose utilization is not specific for cancer cells; various cytokines and growth factors increase the affinity of glucose transporters for deoxy-glucose in inflammatory conditions also [6]. PET has been used for assessment of various inflammatory disorders and has shown encouraging results [7–9]. The interpretation of abdominal PET images is often difficult due to physiologic uptake of FDG in a variety of abdominal/pelvic organs, which makes it difficult to distinguish normal from abnormal uptake. As the intestine remains in a collapsed state, the resolution of the intestine remains very poor on PET-CT. Therefore, distension of the intestine is required for better resolution on imaging [10]. Combining PET with CT enteroclysis, we proposed to evaluate the intestine after its inflation with negative contrast, a technique we call PET-CT enteroclysis. In this pilot study including 17 patients with inflammatory diseases of the intestine, we assessed the feasibility and diagnostic yield of PET-CT enteroclysis.
Materials and methods
In this prospective study, we evaluated 17 patients (10 men; mean age 33.7 years; age range, 15–60 years) who were suspected to have inflammatory diseases of the intestine. All of them were evaluated clinically, biochemically and radiologically as per the standard patient care. For evaluation of the intestine, they underwent barium meal follow through, and/or enteroclysis, and colonoscopy for diagnosis, extent and disease activity. Esophago-gastro-duodenoscopy and ileo-colonoscopy was performed in all the patients using video-endoscopes. Endoscopic examination of the jejunum and ileum was not done in any patient. The colonoscopy examination was done in all patients. For all except two, the examination was complete till ileo-caecal valve. However, in two patients the right colon could not be seen due to stricture at the hepatic flexure. Before the colonoscopy, the colon was prepared with two packets of polyethylene glycol (Peglec, Tablets India, each packet containing 137.5 g of polyethylene glycol) dissolved in 4 l of water. The lesions were classified as minor (erythema, aphthous ulcerations) and major (ulcerations, nodularity, strictures, and cobblestoning) lesions. Based on endoscopic and radiological investigations, the intestine was divided into various segments: stomach (S), duodenum (D), jejunum (J), ileum (I), ileocecal valve (ICV), cecum (C), ascending colon (AC), hepatic flexure (HF), transverse colon (TC), splenic flexure (SF), descending colon (DC), sigmoid colon and rectum (R). Then the lesions were noted according to the segments of involvement. Multiple endoscopic biopsies were obtained from these lesions.
The diagnosis of Crohn’s disease was made on the basis of a combination of clinical, endoscopic, radiological and histological features. The diagnosis of intestinal tuberculosis was made on the basis of clinical presentation (constitutional symptoms, intestinal obstruction), endoscopic features (ulcerations, nodularity, and strictures), histological findings and presence of acid fast bacilli (AFB) on the smear examination or demonstration of mycobacterial DNA by polymerase chain reaction (PCR). The extent and behavior of Crohn’s disease were classified according to the Montreal classification [11]. The activity of Crohn’s disease was assessed using the Crohn’s disease activity index (CDAI) [12].
All the patients underwent PET-CT enteroclysis. The ethics committee of our institution approved this work, and an informed consent was taken from all the participants.
PET-CT imaging
Image acquisition
All 17 patients were evaluated during a symptomatic stage of their disease using PET-CT enteroclysis. All of them underwent both a low dose whole body PET-CT followed by PET-CT enteroclysis. For intestinal preparation, all of them were asked to ingest one packet of polyethylene glycol (Peglec, Tablets India, Pondicherry, India; each packet containing 137.5 g of polyethylene glycol), dissolved in 2 l of water in the evening prior to the procedure. All of them were asked to report to the fluoroscopy room in the fasting state. A jejunal catheter (Frekka, 12 French, 120 cm) was passed trans-nasally after application of lidocaine hydrochloride 2% gel (Xylocaine, AstraZeneca). No sedation was given to any patient for the procedure. The tip of the catheter was positioned just distal to duodeno-jejunal flexure under fluoroscopic guidance. Patients were then transferred to the PET-CT suite.
All of them were asked to rest in a quiet room after intravenous injection of 10 mCi of 18fluoro-deoxyglucose (FDG). Sixty minutes after radiotracer injection, a low dose whole body PET-CT scan was acquired on a Biograph scanner (Siemens, Germany) using the following parameters: 5-mm collimation, 10-mm table speed, and a reconstruction increment of 2 mm and slice thickness of 3 mm. After completion of the whole body PET-CT scan, 2 l of 0.5% methylcellulose, prepared at room temperature, was infused into the jejunum through the naso-jejunal catheter. A 50 ml handheld syringe was used for administration of methylcellulose to provide adequate and uniform small intestine distention. After complete instillation of 1.5 l of methylcellulose in the jejunum, injection Hyoscine n-butyl bromide (Buscopan, Boehringer Ingelheim, Germany), 20 mg was administered intravenously to reduce peristalsis and to improve the distensibility of the intestine. Additional volume of methylcellulose fluid was infused till the patient complained of abdominal discomfort due to abdominal distension or had a desire to pass stool. After achieving adequate small intestinal distension, PET-CT of only the abdomen and pelvis (PET-CT enteroclysis) was performed using the same PET-CT parameters. In both imaging sessions, no intravenous contrast medium was used.
Image interpretation
All the acquired data were transferred to a work station for processing and interpretation. PET-CT and PET-CT enteroclysis images were analyzed in a random fashion. The CT part of the images of PET-CT enteroclysis images were seen and interpreted by two experienced gastrointestinal radiologists (RS and CD) separately and then a consensus was made if there was discordance with PET-CT findings. The PET images of all the patients were seen separately by a nuclear medicine expert (RKP). Evaluation of all the images was done in both axial and coronal planes. Both the radiologists and the nuclear medicine experts were blinded to the clinical details and the previously done radiological imaging. After the separate evaluation, all the images were again seen together by the radiologists, nuclear medicine expert and the clinician together for the final reporting.
After reconstruction of the images in axial and coronal planes using Syngo software (Siemens, Germany), the image analysis was performed qualitatively (visually) and semi-quantitatively (uptake quantification). For semi-quantitative analysis, a region of interest (ROI) was drawn around the site of abnormal FDG uptake in the intestine. The slice with a maximal FDG uptake in the ROI was chosen on the first time point scan for quantitative measurement of metabolic activity of the tracer in terms of standard uptake value (SUV). From these ROIs, the SUV were calculated according to the formula described below:
Whereas, ‘MBq’ = a mega-Becquerel, and ‘g’ = grams.
Criteria for qualitative analysis
The interpretation included a review of both uncorrected and attenuation-corrected scans. Special attention was given to FDG uptake in the intestine. The SUVs for normal intestine are low (2.95±1.25) and slightly lower than that of the liver (3.2±0.79) [13]. PET findings were interpreted as positive if the FDG uptake of the intestinal segment was greater than or equal to that of the liver. PET findings were interpreted as negative if the FDG uptake of the intestinal segment was less than that of the liver. In cases of disagreement, a final decision was made by consensus. On the basis of past experience, we have noted that visual assessment of suspected lesions may be just as effective in differentiating active from inactive disease as is semi-quantitative analysis using the SUV [14]. Therefore, the SUV was not used to differentiate a normal and abnormal intestinal uptake. Furthermore, it was often difficult to generate a region of interest over some intestinal segments due to overlapping.
Data analysis
The conventional barium studies, endoscopic features and PET-CT enteroclysis data were specifically analyzed for the findings listed in Table 1. The involvement of the small and large intestine was analyzed segment wise. Mucosal abnormalities, such as thickening of mucosal folds and erosive or aphthous lesions on enteroclysis and intestinal wall thickening on CT enteroclysis, were rated as mucosal changes [1, 15]. Wall thickening was diagnosed when the small intestinal wall measured at least 3 mm on an adequately distended intestinal loop [16, 17]. Stenosis was characterized as a lack of intestinal loop distention below a minimum diameter of 1.5 cm, and the criterion for the diagnosis of prestenotic dilatation was a diameter exceeding 2.5 cm or the presence of segments wider than more proximal intestinal loops. Additional abnormalities included fatty proliferation, mesenteric vascular proliferation (Comb’s sign), mesenteric lymphadenopathy and conglomeration of intestinal loops due to transmural inflammatory changes. Both PET-CT and PET-CT enteroclysis were compared with the conventional barium studies and endoscopic findings with regard to the assessment of disease extent and distribution. Standard descriptive statistics, a binominal analysis, and a McNemar test were used to analyze the data.
Results
Placement of the naso-jejunal tube was successful in all the patients. The mean fluoroscopy time for placing the naso-jejunal tube was 4.18±2.02 min. The mean radiation dose delivered to the patient during placement of the naso-jejunal catheter as measured by dose area product meter was 12,936±3,951 mGycm2.
Results of conventional barium studies and colonoscopic examination
Conventional barium studies (BMFT-12 or enteroclysis-5) were performed in 17 patients (Table 1). On conventional barium study, in total, 16 segments of small intestine (D-2, J-2, IL-9, and ICJ-3) were seen involved in 14 patients, whereas 3 patients had normal barium studies. Six patients had strictures in the small intestine with proximal dilatation (three in proximal ileum, two in ICJ, and one in the jejunum); three patients had contracted and pulled up cecum. Of the three patients who had ulcerations in the terminal ileum, one had an ulcer in the anti-mesenteric border and another had a nodular terminal ileum. One patient had diffuse mucosal fold thickening involving whole of the small intestine. One patient each had thickening of duodenal and jejunal folds. None of the patients had an intestinal fistula.
On ileo-colonoscopy, 12 patients showed colonic disease involving 17 segments (R = 2, SC = 2, DC = 2, HF = 3, TC = 1, AC = 3 and C = 4), whereas five patients had normal colonoscopic examination. (Table 1) In two patients the scope could not be passed beyond the hepatic flexure because of stricture at the hepatic flexure. The most common findings at colonoscopy were aphthous ulcers (n=8), longitudinal and deep ulcerations (n=3), nodular and deformed cecum with contracted IC junction (n=2) and patchy erythema (n=2). Three patients had hemorrhoids with anal fissure.
Based on clinical, radiological, endoscopic and histological characteristics, a diagnosis of Crohn’s disease was made in nine patients, intestinal tuberculosis in five, tropical sprue in two, immunoproliferative small intestinal disease and celiac disease in one each.
Results of PET- CT enteroclysis
All the 17 patients were evaluated completely by PET-CT enteroclysis. The intestinal loops were distended well in all the patients (Table 1). Twenty-three segments of small intestine (D = 2, J = 2, IL = 11, ICJ = 8) and 27 segments of large intestine (R = 4, S = 4, DC = 3, HF = 2, TC = 6,AC = 5,C = 3) showed an increase in FDG uptake in 14 patients, whereas in 3 patients PET-CT enteroclysis was unremarkable. Intestinal wall thickening was seen in 14 patients (IL = 7, D = 1, J = 2, AC = 2, TC = 1, DC = 1). PET-CT enteroclysis showed conglomerate intestinal loops (inseparable intestinal loops despite an attempt to dilate them with fluid) in two patients. One patient with clinical suspicion of inflammatory bowel disease showed diffuse uptake in the entire small intestine starting from the duodenum till the IC junction on PET-CT enteroclysis (Fig. 1). The full thickness intestinal biopsy showed features of immuno-proliferative small intestinal disease (IPSID). None of these patients had any demonstrable enteric fistula. In patients with intestinal tuberculosis, the PET-CT enteroclysis showed FDG uptake mostly in the ileocecal region (Fig. 2), whereas the FDG uptake was multifocal in those with Crohn’s disease (Fig. 3).
Coronal CT (a), PET (b) and fused PET-CT (c) images with out luminal distention obtained 60 min after intravenous injection of F18-FDG demonstrate diffuse intestinal uptake of FDG in the small intestine (upper row). Coronal CT (d), PET (e) and fused PET-CT (f) images after luminal distention demonstrate diffuse intestinal uptake of FDG, but prominent and better delineated in the small intestine (lower row)
Coronal CT (a), PET (b) and fused PET-CT (c) images without luminal distention obtained 60 min after intravenous injection of F18-FDG demonstrate focal areas of increased FDG uptake at ileocecal junction (upper row). Coronal CT (d), PET (e) and fused PET-CT (f) images after luminal distention demonstrate distended intestinal loops and focal areas of increased FDG uptake at the ileocecal junction (lower row). Note the diminished background activity after intestinal distention
Coronal CT (a), PET (b) and fused PET-CT (c) images without luminal distention obtained 60 min after intravenous injection of F18-FDG demonstrate diffuse bowel uptake of FDG in small and large intestine (upper row). Coronal CT (d), PET (e) and fused PET-CT (f) images after luminal distention demonstrate diffuse intestinal uptake of FDG, but prominent and better delineated in small and large intestine (lower row). Note the disappearance of patchy FDG uptake after intestinal distention (arrow)
The extra-luminal findings seen on PET-CT enteroclysis were abdominal lymphadenopathy with high FDG uptake in three patients (mesenteric lymph nodes in two and para-aortic lymph nodes in one), mesenteric and pericolic fatty proliferation in five patients, bilateral sacroilitis in two, renal stone in two and bilateral hydronephrosis in one patient. Neither of these abnormalities could be identified with conventional tests. Three patients with histologically confirmed diagnosis of celiac disease (1) and tropical sprue (2) had normal PET-CT enteroclysis findings.
PET-CT enteroclysis has detected involvement of a significantly higher number of intestinal segments (total = 50, 23 small intestine and 27 large intestine) (p<0.01) as compared with barium studies (16 segments of small intestine) and colonoscopy (17 segments of large intestine) together. All the 12 patients with positive colonoscopic findings had abnormal PET-CT enteroclysis. Moreover, two patients with normal colonoscopic examination showed FDG uptake on PET-CT enteroclysis in the transverse colon in one (patient no. 10) and diffuse uptake in whole of the colon in another (patient no. 13).
Complications of PET-CT enteroclysis
Most patients complained of nasal discomfort during placement of the naso-jejunal catheter. Three patients complained of mild epigastric discomfort for approximately 15 min after the introduction of the catheter. All patients had mild abdominal discomfort after instillation of fluid for distention the of intestine. Five patients had large volume evacuation of the bowel following the procedure, which resolved without any medication.
Discussion
In this study, PET-CT enteroclysis as a single test showed significantly more lesions in the intestine in comparison to those seen by conventional barium studies and colonoscopic examination in combination. In addition, this technique showed extra-intestinal abnormalities such as lymphadenopathy, mesenteric fat proliferation and sacroilitis. In this study, we report the feasibility of PET-CT enteroclysis.
The feasibility and accuracy of CT enteroclysis in patients with Crohn’s disease has been well documented in the literature [1]. CT enteroclysis enables detailed morphologic characterization of inflamed intestinal segments and reveals mural and extramural manifestations. PET-CT enteroclysis is a simple extension of CT enteroclysis and provides information on morphological details as well as the metabolic activity of the lesion(s). PET-CT is used extensively in evaluation of various extra-abdominal and abdominal malignancies; however, this technique has been used sparingly in patients with small intestinal tumors. PET-CT has also been used for staging of colorectal cancer [4, 5]. The major limitation of its use in small intestinal lesions is because of poor resolution of intestine due to undistended and overlapping intestinal loops and intestinal motility-related artifacts.
PET-CT has also been used in the evaluation and follow-up of patients with various inflammatory diseases including systemic lupus erythematosus and rheumatoid arthritis [19]. At times, it may be difficult to differentiate malignant lesions from inflammatory diseases based on the activity seen on PET-CT. For such a differentiation, using dual-point FDG-PET imaging, Zhuang et al. [19] observed that the SUVs of delayed images increased significantly over time in malignant lesions, whereas the SUV of inflammatory lesions decreased significantly over time.
A normal small intestine, supposedly due to its peristalsis (smooth muscle contraction), shows radiotracer uptake on PET scan. The FDG uptake in the normal intestine is lower than that of the liver. The normally calculated SUVs for normal intra-abdominal organs are 2.58±0.58 for spleen, 2.84±1.06 for stomach, 2.95±1.25 for intestine, and 3.2±0.79 for the liver [13]. The patterns of physiologic uptake in the small intestine vary from diffuse low-level uptake to heterogeneous and multifocal uptake [20]. The small intestine typically demonstrates heterogeneous low-level FDG uptake; however, this uptake can appear more focally intense in the pelvis where intestinal loops overlap each other [21]. Therefore, interpretation of FDG uptake in undistended small intestine is difficult. Gastro-intestinal stromal tumors typically show high avidity for FDG and can be imaged using PET scans where they appear as focal lesions. Lymphomatous lesions of the small intestine also show marked FDG avidity and long segment involvement as seen in one of our patients with immunoproliferative small intestinal disease. Metastatic involvement of the small intestine has been described most frequently in patients with melanoma, which typically shows high FDG avidity [22, 23]. PET-CT has been shown to help in detecting unsuspected intestinal metastases [24, 25]. FDG uptake in the colon is heterogeneous and can vary in distribution from mild focal to diffuse uptake. The cecum and right colon often show higher uptake of FDG, presumably due to the higher concentration of lymphocytes in them [20]. Segmental pattern of FDG uptake has been reported in patients with proctitis, infectious colitis, lymphocytic colitis and hemorrhagic colitis, whereas a nodular focal or multifocal pattern is seen in polyps, adenoma, and colonic cancer [26, 27]. Diffusely increased FDG uptake has been described in patients with inflammatory enterocolitis [7, 28]. FDG-PET has even detected in histologically confirmed mildly inflamed lesions in patients with Crohn’s disease where colonoscopic examination appeared normal [7, 9, 28].
In the assessment of patients with inflammatory bowel disease (IBD), cross-sectional imaging such as CT and MRI provides information on the extent, activity, location and complications of the disease. Conventional tracers like radiolabelled leukocytes have been well-established non-invasive scintigraphy techniques and are still widely used for evaluation of the extent and activity of the disease in patients with IBD [29, 30]. Leukocyte scintigraphy demonstrated sensitivity of 80% to 98% and specificity of 90% to 100% for the detection of IBD in untreated patients [29–31]. However, leukocyte scintigraphy suffers from substantial shortcomings of the tedious, time-consuming cell labeling procedure. In addition, this technique has false-positive results in patients with mesenteric ischemia, carcinoma of the colon and intestinal bleeding. PET-CT utilizes the advantages of the high sensitivity of FDG-PET with the increased resolution of CT in evaluation of patients with IBD. A combination of typical patterns of intestinal wall enhancement as seen at contrast-enhanced CT and a diffuse FDG uptake within the small intestine at PET suggests the presence of an inflammatory or an infectious disease with greater certainty [18]. PET has been used in the evaluation and monitoring of children patients with IBD in whom a colonoscopic examination is difficult to carry out. In a study including 38 patients with Crohn’s disease (17 ileal, 12 ileo-colic, 5 pan-colonic, 3 left-sided disease, 1 right-sided disease) and 17 with ulcerative colitis (15 pan-colitis, 2 left-sided colitis), Lemberg et al. [32] assessed the value of PET in identifying active intestinal inflammation and compared the results with those seen on conventional endoscopic and radiological studies. PET correctly identified active inflammatory diseases in 80% of children with IBD (81.5% with Crohn’s disease, 76.4% with ulcerative colitis) and correctly showed no evidence of inflammation in children with recurrent abdominal pain. FDG accumulation corresponded with sites of active disease at colonoscopy in 83.8% and with small bowel follow-through with pneumo-colon in 75% of patients. In a retrospective study, Loffler et al. [33] using histology as the standard of reference, reported a sensitivity, specificity and accuracy of 98%, 68% 83% with PET-CT as compared that with endoscopic examination (90%, 75%, 82%). For small intestinal lesions, FDG-PET was more reliable. In the evaluation of inflammation in the colon and terminal ileum in patients with Crohn’s disease, Neurath et al. [34] reported a sensitivity of 85%, 67% and 41%, respectively, and specificity of 89%, 93% and 100%, respectively, of PET, hydro-MRI and granulocyte scintigraphy with labeled antibodies in a comparative study. In another preliminary study, FDG-PET was able to detect colitis at an early clinical stage when morphologic imaging was equivocal particularly in early stages of collagenous or eosinophilic colitis [28]. Pio and colleagues [35] reported a good correlation between the intensity of activity as quantified by FDG-labelled WBCs PET and histo-pathologic grading of the degree of inflammation.
One of the main advantages of PET-CT enteroclysis in the evaluation of intestine is the ability to acquire CT enteroclysis scans during the same scanning session as PET scans. It is a non-invasive test that can evaluate both small and large intestine in the same sitting. This test has a potential to differentiate the active form of disease from the fibrostenotic form, especially in Crohn’s disease, and therefore can guide treatment. This technique can also detect extra-intestinal manifestations such as sacroilitis as seen in two of our patients. PET-CT enteroclysis may serve as a one-stop shop investigation for evaluation and especially follow-up of patients with intestinal inflammatory diseases. There is a need of comparative evaluation of this technique using an endoscopic examination (double balloon or capsule enteroscopy) as a gold standard.
One major issue with the use of PET-CT enteroclysis is radiation exposure where patients are subjected to the ionizing radiation of the CT scan along with the radioactivity of FDG. However, radiation exposure to a patient undergoing complete intestinal evaluation (BMFT/enteroclysis and CT scan of the abdomen) is 12–15 mSV (BMFT/enteroclysis 3 mSV and CT abdomen 10 mSV), which is more than that given by PET-CT enteroclysis alone [36, 37].
The major limitation of this study is the lack of an endoscopic evaluation of the small intestine for comparison. There was however a correlation between the lesions seen at colonoscopy and PET-CT enteroclysis. Secondly, there is a lack of follow-up in this study.
In conclusion, as a single investigation, PET-CT enteroclysis detects a significantly higher number of lesions both in small and large intestine in comparison to that detected by conventional barium and colonoscopy combined together. This technique is non-invasive, feasible and very promising.
References
Sailer J, Peloschek P, Schober E, Schima W, Reinisch W, Vogelsang H, et al. Diagnostic value of CT enteroclysis compared with conventional enteroclysis in patients with Crohn’s disease. Am J Roentgenol 2005;185:1575–81.
Mackalski BA, Bernstein CN. New diagnostic imaging tools for inflammatory bowel disease. Gut 2006;55:733–41.
Abdel-Nabi H, Doerr RJ, Lamonica DM, Cronin VR, Galantowicz PJ, Carbone GM, et al. Staging of primary colorectal carcinomas with fluorine-18 fluorodeoxyglucose whole-body PET: correlation with histopathologic and CT findings. Radiology 1998;206:755–60.
Kim JH, Czernin J, Allen-Auerbach MS, Halpern BS, Fueger BJ, Hecht JR, et al. Comparison between 18F-FDG PET, in-line PET/CT, and software fusion for restaging of recurrent colorectal cancer. J Nucl Med 2005;46:587–95.
Larson SM, Schoder H, Yeung H. Positron emission tomography/computerized tomography functional imaging of esophageal and colorectal cancer. Cancer J 2004;10:243–50.
Zhuang H, Alavi A. 18-fluorodeoxyglucose positron emission tomographic imaging in the detection and monitoring of infection and inflammation. Semin Nucl Med 2002;32:47–59.
Kresnik E, Mikosch P, Gallowitsch HJ, Heinisch M, Lind P. F-18 fluorodeoxyglucose positron emission tomography in the diagnosis of inflammatory bowel disease. Clin Nucl Med 2001;26:867.
Skehan SJ, Issenman R, Mernagh J, Nahmias C, Jacobson K. 18F-fluorodeoxyglucose positron tomography in diagnosis of paediatric inflammatory bowel disease. Lancet 1999;354:36–837.
Bicik I, Bauerfeind P, Breitbach T, von Schulthess GK, Fried M. Inflammatory bowel disease activity measured by positron-emission tomography. Lancet 1997;350:262.
Prabhakar HB, Sahani DV, Fischman AJ, Mueller PR, Blake MA. Bowel hot spots at PET-CT. Radiographics 2007;27:145–59.
Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut 2006;55:749–53.
Yoshida EM. The Crohn’s Disease Activity Index, its derivatives and the Inflammatory Bowel Disease Questionnaire: a review of instruments to assess Crohn’s disease. Can J Gastroenterol 1999;13:65–73.
Bischofdelaloye A, Wahl RL. How high level of FDG abdominal activity is considered normal? (abstract). J Nucl Med 1995;36 Suppl:106P
Kumar R, Xiu Y, Yu JQ, Takalkar A, El-Haddad G, Potenta S, et al. F18-FDG-PET in evaluation of adrenal lesions in patients with lung cancer. J Nucl Med 2004;45:2058–62.
Minordi LM, Vecchioli A, Guidi L, Mirk P, Fiorentini L, Bonomo L. Multidetector CT enteroclysis versus barium enteroclysis with methylcellulose in patients with suspected small bowel disease. Eur Radiol 2006;16:1527–36.
Goldberg HI, Gore RM, Margulis AR, Moss AA, Baker EL. Computed tomography in the evaluation of Crohn’s disease. Am J Roentgenol 1983;140:277–82.
Gore RM, Balthazar EJ, Ghahremani GG, Miller FH. CT features of ulcerative colitis and Crohn’s disease. Am J Roentgenol 1996;167:3–15.
Wittenberg J, Harisinghani MG, Jhaveri K, Varghese J, Mueller PR. Algorithmic approach to CT diagnosis of the abnormal bowel wall. RadioGraphics 2002;22:1093–1109.
Zhuang H, Pourdehnad M, Lambright ES, Yamamoto AJ, Lanuti M, Li P, et al. Dual time point 18F-FDG PET imaging for differentiating malignant from inflammatory processes. J Nucl Med 2001;42:1412–17.
Abouzied MM, Crawford ES, Nabi HA. 18FFDG imaging: pitfalls and artifacts. J Nucl Med Technol 2005;33:145–55.
Subhas N, Patel PV, Pannu HK, Jacene HA, Fishman EK, Wahl RL. Imaging of pelvic malignancies with in-line FDG PET-CT: case examples and common pitfalls of FDG PET. RadioGraphics 2005;25:1031–43.
Tatlidil R, Mandelkern M. FDG-PET in the detection of gastrointestinal metastases in melanoma. Melanoma Res 2001;11:297–301.
Rohren EM, Turkington TG, Coleman RE. Clinical applications of PET in oncology. Radiology 2004;231:305–32.
Israel O, Yefremov N, Bar-Shalom R, Kagana O, Frenkel A, Keidar Z, et al. PET/CT detection of unexpected gastrointestinal foci of 18F-FDG uptake: incidence, localization patterns, and clinical significance. J Nucl Med 2005;46:758–62.
Pandit-Taskar N, Schoder H, Gonen M, Larson SM, Yeung HW. Clinical significance of unexplained abnormal focal FDG uptake in the abdomen during whole-body PET. Am J Roentgenol 2004;183:1143–7.
Tatlidil R, Jadvar H, Bading JR, Conti PS. Incidental colonic fluorodeoxyglucose uptake: correlation with colonoscopic and histopathologic findings. Radiology 2002;224:783–7.
Gutman F, Alberini JL, Wartski M, Vilain D, Le Stanc E, Sarandi F, et al. Incidental colonic focal lesions detected by FDG PET/CT. Am J Roentgenol 2005;185:495–500.
Kresnik E, Gallowitsch HJ, Mikosch P, Wurtz F, Alberer D, Hebenstreit A, et al. (18)F-FDG positron emission tomography in the early diagnosis of enterocolitis: preliminary results. Eur J Nucl Med Mol Imaging 2002;29:1389–92.
Almer S, Granerus G, Strom M, Olaison G, Bonnet J, Lemann M, et al. Leukocyte scintigraphy compared to intraoperative small bowel enteroscopy and laparotomy findings in Crohn’s disease. Inflamm Bowel Dis 2007;13:164–74.
Lantto E, Jarvi K, Krekela I, Lantto T, Taavitsainen M, Vedenkangas H, et al. Technetium-99m hexamethyl propylene amine oxine leucocytes in the assessment of disease activity in inflammatory bowel disease. Eur J Nucl Med 1992;19:14–18.
Sciarretta G, Furno A, Mazzoni M, Basile C, Malaguti P. Technetium-99m hexamethyl propylene amine oxime granulocyte scintigraphy in Crohn’s disease: diagnostic and clinical relevance. Gut 1993;34:1364–9.
Lemberg DA, Issenman RM, Cawdron R, Green T, Mernagh J, Skehan SJ, et al. Positron emission tomography in the investigation of pediatric inflammatory bowel disease. Inflamm Bowel Dis 2005;11:733–8.
Loffler M, Weckesser M, Franzius C, Schober O, Zimmer KP. High diagnostic value of 18F-FDG-PET in pediatric patients with chronic inflammatory bowel disease. Ann N Y Acad Sci 2006;1072:379–85.
Neurath MF, Vehling D, Schunk K, Holtmann M, Brockmann H, Helisch A, et al. Noninvasive assessment of Crohn’s disease activity: a comparison of 18F-fluorodeoxyglucose positron emission tomography, hydromagnetic resonance imaging, and granulocyte scintigraphy with labeled antibodies. Am J Gastroenterol 2002;97:1978–85.
Pio BS, Byrne FR, Aranda R, Boulay G, Spicher K, Song MH. Noninvasive quantification of bowel inflammation through positron emission tomography imaging of 2-deoxy-2-[18F] fluoro-D-glucose-labeled white blood cells. Mol Imaging Biol 2003;5:271–7.
Nolan DJ. The small intestine. In: Grainger RG, editor. Grainger and Allison’s text book of diagnostic radiology. 4th ed. London: Churchill Livingstone; 2001. pp. 1075–98.
Towson JEC. Radiation protection and dosimetry in PET and PET/CT. In: Valk PE, Bailey DL, Townsend DW, Maisey MN, editors. Positron emission tomography basic science and clinical practice. London: Springer; 2003. pp. 265–82.
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial disclosure:
All the authors of this study declare no conflict of interest and financial obligation.
Rights and permissions
About this article
Cite this article
Das, C.J., Makharia, G., Kumar, R. et al. PET-CT enteroclysis: a new technique for evaluation of inflammatory diseases of the intestine. Eur J Nucl Med Mol Imaging 34, 2106–2114 (2007). https://doi.org/10.1007/s00259-007-0525-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-007-0525-z