Abstract
The purpose of this study was to evaluate the diagnostic accuracy of multidetector-CT enteroclysis (MDCT-E) versus barium enteroclysis with methylcellulose (BE) in clinically selected patients with suspected small bowel disease. We prospectively studied 52 patients who underwent unenhanced and contrast-enhanced multidetector CT (16 rows) after administration of 2–2.5 l of methylcellulose by naso-jejunal tube. BE was performed after administration of barium 60% w/v (200–250 ml) and methylcellulose (1–2 l). Patients with radiological signs of Crohn’s disease were classified into the following subtypes: active, fibrostenotic, fistulising/perforating, reparative or regenerative subtypes. Twenty-eight patients also underwent endoscopy. The radiological prevalent subtype was the active subtype. The sensitivity, specificity and diagnostic accuracy of MDCT-E versus BE was 83%, 100% and 89%, respectively. BE showed five false negative CT cases due to early Crohn’s disease; endoscopy confirmed positive cases of the CT and the BE, but showed one false negative case of the BE. Together, MDCT enteroclysis and BE permitted the diagnosis of Crohn’s disease in 30 patients, adhesions in one patient, lymphoma in two patients and carcinoid tumours in two patients. In conclusion, MDCT-E permits good representation of pathological patterns. Early stages of Crohn’s disease are better evaluated by BE.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
CT has become a routine examination in the evaluation of gastrointestinal disorders, both for its rapid execution and its accuracy with axial images and multiplanar reconstructions in the other spatial planes. Spiral single slice and multidetector CT have improved image quality and have reduced scan times.
However, the technique should be very precise, and the primary requirements of CT imaging of the small bowel should be pursued, namely: visualisation of the entire small bowel; adequate visceral distension; elimination of respiratory motion and of peristalsis; i.v. administration of iodinated contrast agent to evaluate the extent and pattern of wall enhancement [1].
In CT enteroclysis (CT-E) contrast material is infused through a naso-jejunal tube and contiguous axial images are obtained after total opacification of the small intestine. CT enteroclysis was introduced to overcome the individual deficiencies of CT and barium enteroclysis with methylcellulose (BE) and to combine the advantages of both into one technique. CT enteroclysis has a unique theoretical advantage in its ability to show, simultaneously, intraluminal, mural and extra-intestinal complications of small bowel Crohn’s disease [2].
The purpose of this study was to evaluate the diagnostic accuracy of multidetector CT enteroclysis (MDCT-E) versus barium enteroclysis with methylcellulose in a symptomatic patient population with clinical suspicion or previous diagnosis of small bowel disease.
Materials and methods
We prospectively examined 52 patients (30 men, 22 women; age range: 25–75 years, mean 45 years). The selection criteria were: diarrhoea, abdominal pain or bleeding pertinent to the small bowel, known or suspected Crohn’s disease.
Exclusion criteria included pregnancy, renal insufficiency, intestinal obstruction, previous intestinal resection, documented reaction to iodinated contrast material. Oral informed consent was obtained from all patients.
Technique
Before examination, all patients underwent an intestinal preparation according to the following plan: 2 days before, a light diet free of fruit and vegetables; the day before, 150 mg of a mixture in equal parts of sennosides A and B with a cup of sugared tea at 8:00 a.m.; at 1:00 p.m., a semi-liquid diet; at 5:00 p.m., 15 g of magnesium sulphate in three-quarters of a glass of lukewarm water followed by the consumption of 3 l of water during the following 4–5 h; at 9:00 p.m., a cup of hot soup; fasting from 9:00 p.m.
All patients underwent fluoroscopic placement of a 12–16 F naso-jejunal tube. Then, the patient was brought into the CT room. Contrast material (1,500–2,500 ml of 0.5% methylcellulose) was manually infused, using 60 ml syringes. We aimed to have a constant and continuous injection, approximately two syringes per minute. An anticholinergic compound (N-butyl-hyoscine bromide) was administered intravenously to avoid spasms, to obtain homogeneous small bowel distension and to reduce the patient’s abdominal discomfort. We administered 10 mg when the patient complained of abdominal discomfort and 10 mg just before a CT scan.
At the end of the infusion of the methylcellulose, the patients underwent multidetector 16-row CT (MDCT) (Light Speed Pro 16, GE Medical Systems, Milwaukee, USA), with the following scanning parameters: collimation (in millimetres) 1.25, table speed (in millimetres per rotation), 13.75; pitch 1.375; rotation time 0.6 s, tube potential 120kV, tube current 500 MAs. Unenhanced and contrast-enhanced CT was performed with the patient in the supine position from the diaphragm to the perineum during a single breath hold. A further 200–250 ml of methylcellulose was given after the unenhanced scans in the case of inadequate small bowel distension. Contrast-enhanced CT images were acquired 40 s after i.v. injection of 130–150 ml contrast agent at a rate of 3 ml/s (Ultravist 370, Schering AG, Berlin, Germany).
Image 2D processing was performed with a computer workstation (Advantage Windows, GE Medical Systems).
The patients were then brought into their rooms, where they stayed for 6 h without removal of the naso-jejunal tube. After 6 h the patients underwent fluoroscopic barium enteroclysis with methylcellulose. We administered 200–250 ml 60% wt/vol suspension of 60% barium sulphate, followed by 1,000–2,000 ml (mean 1,200 ml) 0.5% methylcellulose infusion. The contrast flow and progress through the small bowel was fluoroscopically controlled to avoid possible gastric reflux and overloading of the intestine. Postero-anterior and oblique film radiographs were taken with the patient in the supine and prone position; the examination was completed with compression spot views for adequate demonstration of the distal ileum and possible abnormal findings.
Finally, we also evaluated patient discomfort.
Analysis of images
Two gastrointestinal radiologists reviewed all images in consensus. MDCT-E images were interpreted first, in random order; images from the barium enteroclysis with methylcellulose were interpreted next, also in random order. Then, the results of MDCT-E and BE were compared and were classified as normal, Crohn’s disease, other disease. Barium enteroclysis with methylcellulose was performed in all patients.
In CT, after iodinated contrast medium injection, the normal wall of the distended loop (normal parietal thickness <3 mm) shows a linear and homogeneous hyperdense appearance between endoluminal low-density solution and extraparietal hypodensity of the peritoneal fat.
The CT criteria for the diagnosis of small bowel disease was the parietal thickening. We analysed density (in Hounsfield units), grade (in millimetres), symmetry and extent (in millimetres) of the parietal thickening, and presence of associated extraluminal anomalies to perform a differential diagnosis between several small bowel diseases (tumours, inflammatory disease, others).
Crohn’s disease was diagnosed when the parietal thickening was present in association with at least one extraparietal inflammatory involvement (comb sign, lymphadenopathies, abscesses, fistulae).
We looked for small bowel distension. The distension of each small bowel segment was classified in a four-point scale (0=absent, 1=incomplete, 2=partial, 3=complete).
Moreover, we evaluated whether coronal and sagittal 2D reformations added information compared to axial images.
All the barium enteroclysis with methylcellulose images were examined for the following findings: oedematous folds, aphthoid and linear ulcerations, cobblestoning, micronodules, sinus tract, fistulae, stenosis, pre-stenotic dilation, other signs (e.g. adhesions, filling defects).
In patients with Crohn’s disease we classified radiological signs according to the classification of Maglinte et al. [3], as indicated in Table 1.
MDCT-E examinations and BE were compared with endoscopic and surgical results of patients who had undergone ileoscopy (28 patients) or surgery (five patients).
The comparable statistic evaluations were carried out by χ2 testing. A value of P< 0.05 was considered statistically significant. This was a pilot study made in order to obtain the data with which a formal calculation can be made on a sample target group of the necessary size. Therefore, every statistical test performed has purely explorative significance.
Results
The different degrees of distension of the loops (classified by a four-point scale) are summarised in Table 2. Complete distension was observed in 40/52 (77%) patients in the proximal jejunum, in 42/52 (81%) in the distal jejunum, in 46/52 (88%) in the proximal ileum, in 48/52 (92%) in the distal ileum, and in 46/52 (88%) in the last ileal loop.
A further 200–250 ml of methylcellulose was given after the unenhanced scans for the inadequate small bowel distension in 10/52 (19%) patients.
Concerning the use of N-butyl-hyoscine bromide (Buscopan), the first dose was usually administered intravenously before 1–1.5 l of methylcellulose; no patients had any contraindications to the drug (glaucoma, prostatic hypertrophy, tachyarrhythmia), and no side effects were observed.
The abnormal loops showed wall thickening ranging between 4 mm and 12 mm (mean 7 mm), loop diameters ranging between 11 mm and 30 mm (mean 22 mm), luminal diameter between 2 mm and 18 mm (mean 8 mm), longitudinal extent between 10 cm and 30 cm (mean 15 cm). Unenhanced CT depicted density values of involved segments ranging between 20 HU and 57 HU and the degree of their contrast enhancement ranged between 75 HU and 208 HU.
In total, MDCT found 55 small bowel thickened loops that presented signs referring to Crohn’s disease. Barium enteroclysis with methylcellulose found 60 altered small bowel loops; ulcerations and cobblestoning were prevalent signs. According to the radiological classification, we have indicated in Table 3 the radiological signs identified in our study.
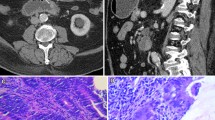
The prevalent subtype was active inflammatory subtype. In particular, target sign was present in 15 patients (Figs. 1 and 2), comb sign in five patients (Fig. 3). Fistulae were evident in six patients studied by CT enteroclysis and in four patients studied by barium enteroclysis with methylcellulose (Fig. 4). Abscesses were present only in two patients (Fig. 5).
Comparing loop to loop between MDCT-E and BE, all loops identified as abnormal on CT examination were also abnormal on BE. The most frequently involved sites were the distal ileum and the last ileal loop (Table 4).
Barium enteroclysis with methylcellulose permitted the identification of five false negative CT cases. They were carried out on early disease with nodular thickened folds or aphthoid lesions without accompanying oedema or wall thickening (Fig. 6). In one patient the false negative case was due to inadequate distension of the loop that did not permit the relief of a pathological pattern.
In total, MDCT-E suspected Crohn’s disease in 25 patients and BE suspected Crohn’s disease in 30 patients. Seventeen patients were free of disease by both techniques. If the BE is considered as the gold standard, the sensitivity, specificity and diagnostic accuracy of the CT is 83%, 100% and 89%, respectively (Table 5).
Thirty-three patients underwent ileoscopy. The ileoscopy failed in five patients; in those patients, in fact, the distal ileal loops were not visualised by endoscopy because there were some stenoses in the colon. Imaging results were compared with ileoscopy in 28 patients; the mean time between MDCT-E and ileoscopy was 6 days. In Table 6 we have indicated the values of negative and positive false cases, negative and positive true cases, sensitivity, specificity and diagnostic accuracy of the barium enteroclysis with methylcellulose and the MDCT-E in comparison with endoscopy.
The cases positive in the endoscopy and negative in the MDCT-E were due to early disease (erosions and aphthoid ulcers).
The cases positive in the MDCT-E and negative in the endoscopy were due to proximal and/or extraluminal small bowel involvement.
Sensitivity, specificity and diagnostic accuracy of MDCT-E versus endoscopy was 78%, 100% and 82%, respectively, while sensitivity, specificity and diagnostic accuracy of the BE was 96%, 100% and 96% respectively (Table 6).
Other diseases were: lymphoma in two patients, carcinoid tumours in two patients, and adhesions in one patient. The lymphomas were a form associated with coeliac disease, which appeared before a diagnosis of coeliac disease; in the MDCT-E this appeared as significant small bowel thickening, homogeneous in attenuation; contrast enhancement was minimal (Fig. 7). In the patients with carcinoid tumours the MDCT-E showed a small intraluminal mass; contrast enhancement was intense (Fig. 8). In all five patients the diagnoses were confirmed by surgery; the mean time between MDCT-E and surgery was 25 days.
Moreover, we noted in all patients that multiplanar reformations (MPRs) did not give further information, compared with axial images, even if they have increased the capacity for non-radiologist–medical doctors to recognise the disease.
Finally, all patients complained of abdominal discomfort (nausea and/or abdominal pain); vomiting occurred in 6/52 (11.5%) patients.
Discussion
The conventional techniques for small bowel study (small bowel follow-through examination, small bowel barium enteroclysis with methylcellulose) visualise the gastrointestinal tract from inside; therefore, normal characteristics and mucosal–luminal alterations are accurately depicted.
Now, direct visualisation of the entire small bowel is possible with wireless capsule endoscopy (CE) in which the patient ingests a small capsule that transmits small bowel intraluminal images to an external recorder. CE has been shown to be superior to both small bowel barium enteroclysis with methylcellulose [4] and small bowel follow-through examination [5] to find ulcerative lesions in patients with gastrointestinal bleeding.
However, these techniques only provide indirect information on the intestinal wall and adjacent extra-intestinal structures, unlike CT, which is able to assess mural and extramural findings [1, 5]. In addition, CE was not performed in patients with a stricture found at the small bowel follow-through examination or at the small bowel barium enteroclysis with methylcellulose [5].
The role of CT in small bowel studies has only recently been defined, owing to the relatively rare occurrence of small bowel disease, and, consequently, there is less interest in the development and updating of this imaging procedure. Sensitivity of CT studies in inflammatory small bowel disease is not known and relies on the quality of the examination, the severity of inflammation and on the presence of mesenteric or intraperitoneal abnormalities. The development of faster machines and the rapid increase in spatial resolution with the introduction of multidetector CT and multiplanar reconstructions have modified the approach to small bowel diagnostic imaging.
The use of CT in small bowel disease is aimed at the visualisation of the entire organ and adequate distension, the elimination of respiratory and peristaltic motion artefacts, and the i.v. administration of contrast agents to evaluate the pattern and extent of wall enhancement. Accurate intestinal cleansing is required, as in conventional radiology [1].
Independent of the CT technique used, it is essential to have a fluid-distended loop, because mural wall thickening is the hallmark of intestinal disease. A comparison between BE and abdominal CT in Crohn’s disease shows that BE obtains a better bowel distension, while CT better shows transmural and extra-intestinal spreading [6].
In CT the normal thickness of the intestinal wall is barely perceptible in a wall-distended segment and should be no greater than 2 mm to 3 mm thick; during the i.v. administration of the contrast-agent bolus, there is a normal perceptible enhancement of the bowel wall. Inadequate contrast opacification of the intestinal lumen and incomplete luminal distension account for the vast majority of errors.
There are different modalities of administration and different types of contrast agents used to obtain the distension of the small bowel [1]. The small bowel can be opacified with positive contrast agents (1–2% barium sulphate suspension or a 2–3% water-soluble iodinated solution) or negative contrast agents (oral water, oral oil emulsions or methylcellulose by naso-duodenal tube) [1].
Orally administered contrast agents have the disadvantage of an inadequate non-uniform distension of all small bowel loops, particularly of jejunal loops; the problem is overcome at the cost of higher invasiveness, time and costs with CT enteroclysis. CT enteroclysis combines the advantages of CT and barium enteroclysis with methylcellulose into one technique [2]; in 1992 Klöppel et al. [7] made the first study on CT enteroclysis in inflammatory small bowel disease, pointing out the diagnostic accuracy of this technique in the evaluation of mucosal abnormalities, bowel wall thickening, fistulae and extra-intestinal complications.
Hypodense contrast medium ensures better definition of the internal aspect of the small bowel, especially to evaluate the degree of parietal contrast enhancement after intravenous infusion contrast bolus [8]. This explains why we have used a hypodense contrast agent such as methylcellulose in our study; it is a well-known, safe, non-toxic medium that has long been used for conventional enteroclysis, it is not absorbable, thus avoiding the risk of haemodilution. It has almost the same density as water, thus providing a good difference between the bowel content and the contrast-enhanced intestinal wall.
Because we did not have an infusion pump, we manually administered the methylcellulose, and we aimed to have a constant and continuous injection. CT was performed at the end of the injection of the methylcellulose; if unenhanced scans showed bad distension of the loops, we administered a further dose of methylcellulose (approximately 200–250 ml). Moreover, we used a hypotonic agent to obtain homogeneous distension and to avoid abdominal discomfort of the patient; unlike other authors [9, 10], we preferred to administer, intravenously, two doses of 10 mg, the first when the patient complained of abdominal discomfort (usually after 1–1.5 l of methylcellulose), the last just before the CT examination. The first dose permitted the patient to tolerate the methylcellulose administration and permitted us to administer up to 2.5 l of methylcellulose. Following this procedure, we obtained a complete distension in 40/52 (77%) patients in the proximal jejunum, in 42/52 (81%) in the distal jejunum, in 46/52 (88%) in the proximal ileum, in 48/52 (92%) in the distal ileum, and in 46/52 (88%) in the last ileal loop. Manual infusion is limiting because the distension is better when a peristaltic pump is used [9, 10], even if its use does not always permit one to obtain optimal distension of all the loops; Turetschek [10], for example, did not recognise a jejunal stenosis, because of unsatisfactory distension, and misinterpreted it as a spasm. Wold et al. [11] did not use a peristaltic pump to perform enteroclysis CT and did not find significant difference in the adequacy of luminal distension between peroral water CT enterography and CT enteroclysis. In our study we also obtained a good distension for both jejunal and ileal loops.
We used a balloon to avoid methylcellulose reflux into the stomach, which can cause patient vomiting and consequently retrograde emptying of jejunal loops. Even so, vomiting occurred in 6/52 (11.5%) of our patients.
Intravenous injection of contrast medium is an indispensable technical support in the CT evaluation of Crohn’s disease. Usually, the amount of contrast medium and the infusion velocity are 150 ml at 3 ml/s. Not all authors agree on the scan delay after i.v. administration of contrast agent: some prefer an early arterial phase at 25 s [10] or a late arterial phase at 40 s [9, 12, 13]; others prefer a single portal phase at 60–70 s [14]. Horton et al. [15] carried out a bi-phasic study with spiral CT and did not encounter any significant differences in terms of contrast enhancement between the two phases, even if the mural contrast enhancement was bigger in the arterial phase than the portal phase. Maglinte et al. advise a bi-phasic study at 25 s and 60 s or a single phase one at 40 s [16]. We decided to make a single phase study at 40 s of scan delay because we chose to have a better contrast enhancement of the abnormal loops.
Concerning radiological signs, we used the radiological classification presented in 2003 by Maglinte [3]. Classification of subtypes requires accurate information about the presence of ulcerations, oedema, spasms, stenosis, fistulae and mesenteric inflammatory mass. An imaging-based classification system of Crohn’s disease can help to plan appropriate therapy. More than one subtype may be noted in a segment or in multiple segments in the same patients [3]. In our study the prevalent subtype was the active type. In this type the prevalent sign was the mural thickening, with the target sign as alternating rings of high and low density in which the intermediate low-density ring represented submucosal oedema or fat, while the inner ring of mucosa and outer ring of muscle layer and serosa showed intense enhancement [1, 17 ]. The target sign was originally reported in Crohn’s disease, but it is now known to be a non-specific finding; the differential diagnosis included Crohn’s disease, ischaemia, infectious enteritis, radiation enteritis, vasculitis and graft-versus-host-disease [1]. Target sign was observed in 15 patients of our study (Figs. 1 and 3).
Besides its ability to identify bowel wall thickening, spiral CT has the added capacity of demonstrating alterations of the vascular pattern near the bowel wall. The so-called comb sign is manifested by hypervascularity of the involved mesentery manifesting as mesenteric arterial dilation, tortuosity, prominence and wide spacing, and dilation of the vasa recta [17]. The comb sign was present in five patients of our study (Fig. 3).
According to previous work, CT is superior in the evaluation of extra-luminal extension of the inflammatory disease [17]. CT identified abscesses, phlegmons, fistulae and enlarged mesenteric nodes.
CT is the procedure of choice for detection of an intra-abdominal or pelvic abscess. Fistulae were present in six patients of our study (Fig. 4), and abscesses in two patients (Fig. 5). When one is performing abdominal CT it is important to include the entire perineum, as CT may demonstrate peri-anal or peri-rectal abscesses or fistulae [17]. Even though we studied the entire perineum, no cases of abscesses or fistulae were present in this site. In the literature, authors have reported that MDCT better defines disease extension and entero-enteric fistulae because it improves the quality of multiplanar reconstructions (MPRs) [16]. In our study MPRs did not show any abnormality that had not already been detected in axial images, even though they improved our confidence in the interpretation of images and let us better evaluate the extension of intestinal involvement as reported by other authors [18, 19]; coronal images were particularly appreciated by clinicians and surgeons, because they were more familiar with them. However, a recent study [20] shows that the axial slices are superior to coronal reconstructions because of better sensitivity in the most common pathological patterns and higher interobserver agreement in most of them.
Concerning the comparison between MDCT-E and BE, in our experience it can still be useful to combine these techniques in patients with suspected Crohn’s disease. BE was performed in all patients, and the results were evaluated in consensus by two radiologists, one with great experience. In these patients the comparison between the results of the MDCT-E and the BE (our gold standard) showed sensitivity, specificity and diagnostic accuracy of, respectively, 83%, 100% and 98% for the CT. Moreover, some patients also underwent endoscopy. In these patients we compared both MDCT-E and BE with ileoscopy, and we found sensitivity, specificity and diagnostic accuracy of, respectively, 78%, 100% and 82% for the CT and of 96%, 100% and 96% for the BE.
The combination of two techniques, MDCT-E and BE, yields a greater diagnostic definition depicting CT false negative cases. In our survey, in fact, five CT false negative cases were due to an initial phase of the disease; these cases were due to nodular thickened folds or aphthoid ulcers without accompanying oedema or wall thickening. In one patient the false negative result was because of inadequate distension of the loop, which did not permit the relief of pathological patterns. The CT difficulty in identifying early disease has been shown by recent work [5]. In our study, moreover, all false negative cases were recognised by BE and then confirmed by endoscopy. In our study endoscopy also showed a BE false negative case, showing the presence of erosions and rare aphthoid ulcers in the last ileal loop; in this patient the BE was limited because endoluminal secretions had diluted the contrast agents. Further, endoscopy has the noted advantage of permitting biopsies. Nevertheless, endoscopy has some limitations: because it is an invasive examination, it was not performed in patients in whom MDCT-E and BE were negative; in those patients, nevertheless, the clinical follow-up did not show persistent symptoms. It is not always possible to reach the distal ileal loops; in fact, in our study, endoscopy failed in five patients because of the stenosis of the colon. Moreover, endoscopy permits visualisation of limited number of loops; then, it is not possible to exclude the presence of lesions in the remaining loops. Finally, endoscopy does not visualise extraluminal disease.
Even if Crohn’s disease has been the most frequent disease, MDCT enteroclysis permitted us to accurately identify other pathological conditions such as lymphoma (Fig. 7), adhesions and carcinoid tumours (Fig. 8). Specific patterns permitted, in many cases, differential diagnosis between benign and malignant lesions and, in some cases, also the identification of the lesion [1, 21]. Sporadic cases of multifocal carcinoid tumours and melanoma have been reported [2].
Finally, the rate of patients’ general discomfort was high, probably due to the long-standing naso-jejunal tube.
In conclusion, we believe that MDCT enteroclysis permits a good representation of pathological patterns in small bowel disease. According to recent studies, in our opinion CT data still need to be combined with conventional imaging or with CE, in particular early stages of Crohn’s disease are better evaluated by BE. CT is superior to CE and conventional imaging in the assessment of mural and extramural findings. Preferably, CT examination should be carried out with a peristaltic pump and methylcellulose infusion even during CT acquisition, so that a more homogeneous distension of the loops can be obtained.
Finally, the performance of CT permits the diagnosis of other small bowel pathological conditions, particularly benign and malignant tumours.
References
Birnbaum BA (1999) Computed tomography of the small bowel. Technique and principles of interpretation. In: Herlinger H, Maglinte DDT, Birnbaum BA (eds) Clinical imaging of the small intestine. Springer, Berlin Heidelberg New York, pp 153–166
Bender GN, Timmons JH, Williard WC, Carter J (1996) Computed tomographic enteroclysis: one methodology. Invest Radiol 31:43–49
Maglinte DD, Gourtsoyiannis N, Rex D, Howard TJ, Kelvin FM (2003) Classification of small bowel Crohn’s subtypes based on multimodality imaging. Radiol Clin North Am 41:285–303
Liangpunsakul S, Chadalawada V, Rex DK, Maglinte D, Lappas J (2003) Wireless capsule endoscopy detects small bowel ulcers in patients with normal results from state of the art enteroclysis. Am J Gastroenterol 98:1295–1298
Hara AK, Leighton JA, Sharma VK, Fleisher DE (2004) Small bowel: preliminary comparison of capsule endoscopy with barium study and CT. Radiology 230:260–265
Maglinte DDT, Hallett RL, Rex D (2001) Imaging of small bowel Crohn’s disease: can abdominal CT replace barium radiography? Emerg Radiol 8:127–133
Klöppel R, Thiele J, Bosse J (1992) The Sellink CT method. Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 156:291–292
Scholten ET, Ziedses des Plantes BG, Falke TH (1995) Computed tomography of the large bowel wall. Choice of slice thickness and intraluminal contrast medium. Invest Radiol 5:275–284
Rollandi GA, Curone PF, Biscaldi E, Nardi F, Bonifacino E, Conzi R, Derchi LE (1999) Spiral CT of the abdomen after distension of small bowel loops with transparent enema in patients with Crohn’s disease. Abdom Imaging 24:544–549
Turetschek K, Schober E, Wunderbaldinger P, Bernhard C, Schima W, Puespoek A, Vogelsang H, Moeschl P, Mostbeck G (2002) Findings at helical CT enteroclysis in symptomatic patients with Crohn disease: correlation with endoscopic and surgical findings. J Comput Assist Tomogr 26:488–492
Wold PB, Fletcher JG, Johnson CD, Sandborn WJ (2003) Assessment of small bowel Crohn disease: noninvasive peroral CT enterography compared with other imaging methods and endoscopy-feasibility study. Radiology 229:275–281
Makò EK, Mester AR, Tarjan Z, Karlinger K, Toth G (2000) Enteroclysis and spiral CT examination in diagnosis and evaluation of small bowel Crohn’s disease. Eur J Radiol 35:168–175
Rust GF, Sackman M, Eisele O, Reiser M (2001) Virtual large intestine imaging with multi-level CT. Pain free coloscopy that works! MMW Fortschr Med 143:32–36
Balthazar EJ (2002) Evaluation of the small intestine by computed tomography. In: Gourtsoyiannis NC (ed) Radiological imaging of the small intestine. Springer, Berlin Heidelberg New York, pp 87–130
Horton KM, Eng J, Fishman EK (2000) Normal enhancement of the small bowel: evaluation with spiral CT. J Comput Assist Tomogr 24:67–71
Maglinte DD, Lappas JC, Heitkamp DE, Bender GN, Kelvin FM (2003) Technical refinements in enteroclysis. Radiol Clin North Am 41:213–229
Kelvin FM, Herlinger H (1999) Crohn’s disease. In: Herlinger H, Maglinte DDT, Birnbaum BA (eds) Clinical imaging of the small intestine. Springer, Berlin Heidelberg New York, pp 259–289
Horton KM, Fishamn EK (2003) The current status of multidetector row CT and three-dimensional imaging of the small bowel. Radiol Clin North Am 41:199–212
Raptopoulos V, Schwatz RK, McNicholas MM, Movson J, Pearlman J, Joffe N (1997) Multiplanar helical CT enterography in patients with Crohn’s disease. AJR Am J Roentgenol 169:1545–1550
Schmidt S, Chevallier P, Charalon M, Bessoud B, Verdun FR, Frascarolo P, Schnyder P, Denys A (2005) Multidetector CT enteroclysis: comparison of the reading performance for axial and coronal views. Eur Radiol 15:238–246
Romano S, De Lutio E, Rollandi GA, Romano L, Grassi R, Maglinte DD (2005) Multidetector computer tomography enteroclysis (MDCT-E) with neutral enteral and IV contrast enhancement in tumor detection. Eur Radiol 15:1178–1183
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Minordi, L.M., Vecchioli, A., Guidi, L. et al. Multidetector CT enteroclysis versus barium enteroclysis with methylcellulose in patients with suspected small bowel disease. Eur Radiol 16, 1527–1536 (2006). https://doi.org/10.1007/s00330-006-0185-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0185-6