Abstract
Objective
The aim of this study is to exploit the normal nature of peroneal nerve anatomy to identify constant magnetic resonance imaging (MRI) patterns in peroneal intraneural ganglia.
Design
This study is designed as a retrospective clinical study.
Materials and methods
MR images of 25 patients with peroneal intraneural ganglia were analyzed and were compared to those of 25 patients with extraneural ganglia and 25 individuals with normal knees. All specimens were interpreted as left-sided. Using conventional axial images, the position of the common peroneal nerve and either intraneural or extraneural cyst was determined relative to the proximal fibula and the superior tibiofibular joint using a symbolic clock face. In all patients, the common peroneal nerve could be seen between the 4 and 5 o’clock position at the mid-portion of the fibular head. In patients with intraneural ganglia, a single axial image could reproducibly and reliably demonstrate both cyst within the common peroneal nerve at the mid-portion of the fibular head (signet ring sign) between 4 and 5 o’clock and within the articular branch at the superior tibiofibular joint connection (tail sign) between 11 and 12 o’clock; in addition, cyst within the transverse limb of the articular branch (transverse limb sign) was seen at the mid-portion of the fibular neck between the 12 and 2 o’clock positions on serial images. Extraneural ganglia typically arose from more superior joint connections with the epicenter of the cyst varying around the entire clock face without a consistent pattern. There was no significant difference between the visual and template assessment of clock face position for all three groups (intraneural, extraneural, and controls). We believe that the normal anatomic and pathologic relationships of the common peroneal nerve in the vicinity of the fibular neck/head region can be established readily and reliably on single axial images. This technique can provide radiologists and surgeons with rapid and reproducible information for diagnosis and treatment planning.
Conclusions
By using conventional bony anatomy as reference points (namely fibular neck and mid-portion of fibular head), standard axial images can be used to interpret key features of peroneal intraneural ganglia and to establish their accurate diagnosis (rather than extraneural ganglia) and pathogenesis from an articular origin (rather than from de novo formation), a fact that has important therapeutic implications. Because of the relative rarity of peroneal intraneural cysts and physicians’ (radiologists and surgeons) inexperience with them and the complexity of their findings, they are frequently misdiagnosed and joint communications are not appreciated preoperatively or intraoperatively. As a result, outcomes are suboptimal and recurrences are common.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The pathogenesis of peroneal intraneural ganglia, long a source of controversy, is becoming clear. Typical pathoanatomic features have been substantiated to support a joint origin for these cysts [the unifying articular (synovial) theory] [1, 2]. Predictable magnetic resonance imaging (MRI) findings can predictably demonstrate the consistent anatomic findings and help identify the type of cyst (intraneural or extraneural) and a joint connection [3]. MRI therefore can clarify the pathogenesis of these cysts. Central to our understanding of the propagation of these peroneal intraneural cysts is their u- or j-shaped articular branch that serve as a conduit for cyst fluid to dissect from the superior tibiofibular joint and dependent upon intra-articular pressures ascend preferentially up the common peroneal nerve (and at times into the sciatic nerve) rather than descend down the terminal branches of the peroneal nerve [4].
Recently, introduced were three two-dimensional MRI signs that could be utilized to diagnose peroneal intraneural ganglia at the fibular head and neck region and to establish their articular connection to the superior tibiofibular joint (Fig. 1a and b): The “tail sign” described the cystic articular branch–joint connection; the “transverse limb” sign, cyst within the articular branch as it crossed over the anterior surface of the fibular neck; and the “signet ring” sign, eccentric cyst within the outer epineurium of the common peroneal nerve [3]. The tail sign is non-specific, as current MRI resolution does not allow differentiation of a neural from a non-neural pedicle in intraneural versus extraneural cysts. The transverse limb sign was determined to be pathognomonic because of its constant anatomic relation to a bony reference point (i.e., the fibular neck) and its presence even in cysts with limited proximal extension but was not widely appreciated previously. The signet ring sign, which perhaps is the most commonly depicted because the cyst is expanded, may be absent in the occasional case in which proximal extension was limited.
Hypotheses for this study. a The reproducible anatomy of the common peroneal nerve (CPN) and its terminal branches can be seen. The articular branch (AB) arises from the deep peroneal nerve (DPN). A branch to the tibialis anterior (TA) arises from the AB. The arrow shows the ascending limb of the articular branch as it heads toward the superior tibiofibular joint. SPN superficial peroneal nerve, F fibular head. b Locations for previously described imaging signs have been superimposed on a. The tail sign (green circle) identifies cyst at the superior tibiofibular joint connection; the transverse limb sign (yellow circle) demonstrates cyst within the transverse limb of the articular branch as it crosses the anterior portion of the fibular neck; the signet ring sign (blue circle) demonstrates cyst within the common peroneal nerve. The dashed arrow demonstrates the path of proximal intraneural cyst extension from the superior tibiofibular joint along the articular branch to the common peroneal nerve (or more proximally), characteristic of the u or J sign. c Our predictions for this study were that the anatomical configuration of the u- or J- shaped (inset) intraneural cyst and the location of these signs could allow us to identify reproducible imaging parameters. A transverse section through the fibular head should show both the tail and signet ring signs in one axial image. A transverse section through the fibular neck should show the transverse limb sign (with permission, Mayo Foundation, 2008)
Our familiarity with the normal and affected cross-sectional anatomy, specifically the pathologic j- or u-shaped articular branch, suggested to us that specific single axial images obtained from conventional knee MRIs could be predicted three-dimensionally to demonstrate these signs based on knowledge of standard bony coordinates (Fig. 1a and b). We predicted that a single axial image could be determined which would intersect the “J” in two defined loci, allowing visualization of both the joint connection (tail sign) and the intraneural cyst (signet ring sign) against fixed bony anatomy at once (Fig. 1c). Such a technique would facilitate the easy and reproducible diagnosis (i.e., the nature of the cyst) and the joint connection (i.e., the origin). This could provide radiologists and surgeons with a simple and reliable recipe for success. Such a technique would prevent misdiagnosis and would help end the controversy that joint connections do not exist in intraneural ganglia. In so doing, it could improve outcomes by decreasing unrecognized joint connections that when untreated frequently lead to recurrences.
Materials and methods
Routine MRIs done at our institution and referring facilities of 25 consecutive cases of intraoperatively and histologically confirmed peroneal intraneural ganglia treated over the past decade were retrospectively analyzed. These sets of MR images were compared to 25 consecutive cases of extraneural ganglia and 25 consecutive routine knee MRIs obtained for other indications such as internal derangement (which served as controls for this study). All of the cases included (intraneural, extraneural, and controls) were of skeletally mature adults. All of the MR images were analyzed both visually and with a specially created template to define the position of the common peroneal nerve and cyst to established bony landmarks. The vast majority of the peroneal intraneural ganglia were scanned on 1.5 T imagers. The earliest MR examinations were done at 0.5 T, while the more recently treated pathological cases and all normal knees were imaged at 3 T. Fast spin echo (FSE) T2-weighted axial images, usually with fat suppression, were analyzed due to the consistent identification of the common peroneal nerve and its branches relative to the fibular head and neck, and because this sequence is included on all standard knee imaging at our institution. When available, T1-weighted axial images were also reviewed. This study was completed with the approval of our Institutional Review Board. Many of the patients included in the intraneural ganglia cohort were published in a previous paper introducing the aforementioned MRI signs [3].
For this study, all MR examinations were interpreted as left-sided as a convention. The position of the nerve and the cyst was first assessed relative to the proximal fibula and to the superior tibiofibular joint. In the pathologic cases, the presence of the tail sign and the signet ring sign as seen on a single image was assessed in the pathologic group. The position of the transverse limb sign by itself was determined. In the cases of extraneural ganglia, the position of the cyst relative to the peroneal nerve and the fibular head as well as the location of the joint connection was determined. The position of the nerve/cyst was evaluated relative to a 12-h clock face using hour and half-hour increments. The bony level of this combination of MRI signs was recorded. The configuration and the dimensions of the proximal fibula were assessed at the selected cross-sectional point. The fibular head was divided into thirds visually, with the middle third having the largest cross sectional area. In the control group, the position of the common peroneal nerve and its terminal branches and their relationship to the fibular neck/head region were also identified. Section thickness was noted for each case.
Three observers, who evaluated the images first independently and then with agreement by consensus, retrospectively analyzed all images (intraneural, extraneural, and control) for all measurements. The observers included a neurosurgeon and a musculoskeletal radiologist, both experienced in the diagnosis and treatment of periarticular ganglia, and a second-year medical student who was trained in the basic anatomy of the peroneal nerve and knee joint but who had no other radiology experience. The radiologist and student were blinded to the surgical findings. A template (a transparency with circles of different diameters subdivided into times to simulate more exactly the “hour hands” on the clock face) was used and superimposed on images to maintain consistency and reproducibility in addition to separate, visual assessment of clock face position. The leg position (neutral, or internally or externally rotated) was accounted for by using the tibial tuberosity as the guide to a true, neutral anterior position, and the template was applied accordingly.
Statistical differences among the groups were analyzed using chi square analysis. P value less than 0.05 was considered statistically significant. JMP 6.0 (SAS, North Carolina) was used to compute statistical significance. The first analysis looked at differences in the location of the common peroneal nerve (i.e. between 4:30 and 5:00 o’clock) in the axial plane among all three groups (controls, intraneural, and extraneural). The second analysis looked at differences among all three groups in the location of the common peroneal nerve (at 4:30) in reference to the superior tibiofibular joint in the axial plane. The third analysis looked for differences in the joint connection in relation to the fibular head (i.e. superior, middle, or inferior) among the intraneural and extraneural groups.
Results
The relevant anatomy could be seen in all cases independent of acquisition techniques. The fibular head was roughly round at its mid-portion, and the fibular neck was oval or rectangular. There was 100% concordance between slices selected by the observers and the estimation of clock face position within 1 h, both visually and using the template individually. Slice thickness ranged from 2.5–8 mm. The articular branch of the nerve was seen on average within 4 mm of the mid-portion of the fibular head when it was visible (with intraneural cyst or on 3-T control examinations). All observers were able to distinguish intraneural versus extraneural cysts with 100% accuracy.
Intraneural ganglia
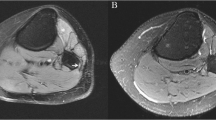
For the intraneural ganglia, the joint connection (tail sign) and intraneural cyst (signet ring sign), as well as the transverse limb sign could be seen on serial axial images through the fibular head and neck. On these left-side images, the signet ring sign (intraneural cyst) was consistently seen between 4 and 5 o’clock together with the tail sign (connection to the superior tibiofibular joint) at the 11–12 o’clock on one axial image, always at the mid-portion of the fibular head (Figs. 2 and 3a). The transverse limb sign was seen within one to two slices of the mid-portion of the fibular head (defined as its largest dimension). The 12–2 o’clock position best showed the transverse limb in its entirety at the mid-portion of the fibular neck in all cases (Figs. 2 and 3b). Further refinement of this concept allowed identification of cyst within both a portion of the transverse limb adjacent to the joint and the peroneal nerve at 12 and 3 o’clock, respectively, at the level of the junction of the head and neck of the proximal fibula. In some cases, nearly the entire extent of cyst within the articular branch could be seen on a single axial image. In several cases of peroneal intraneural ganglia, the transverse limb and tail signs could be seen on a single image, which included the mid-portion of the fibular head and the head–neck junction of the proximal fibula. In most of these instances, cyst could also be seen extending proximally toward the common peroneal nerve (Fig. 4). The intraneural cysts had the typical, previously described consistent tubular configuration extending along the common peroneal nerve and its branches.
Clock face. Drawing (left) of the common peroneal nerve and its terminal branches (corresponding to the anatomy seen in Fig. 1 a). Drawing (center) demonstrating the transverse planes through the regions of the mid-fibular head where the tail and signet ring signs were seen and the mid-fibular neck where the transverse ring sign was observed (as described in Fig. 1 b). At the mid-portion of the fibular head (upper right panel), its diameter is maximal. At this level, the fibular head appears circular and the proximal tibia, triangular. With a left clock face, the signet ring sign is between the 4 and 5 o’clock position and the tail sign at the 11 o’clock (shown here) and 12 o’clock position. At the fibular neck (lower right panel), the transverse limb sign is between 12 and 2 o’clock position. The orientation of these two MR images has been corrected for the external rotation present in the source images. The artist drawing (right central panel) is a three-dimensional representation from a posterior to anterior vantage point of the u-shaped intraneural cyst with the transverse planes through the described imaging signs (with permission, Mayo Foundation, 2008)
Peroneal intraneural cyst (same source images as in Fig. 2). a T2-weighted FSE axial image with fat suppression (TR = 3,000/TE = 49 ms) at the level of the mid-fibular head shows intraneural cyst within the common peroneal nerve at the 4:30 o’clock position (asterisk). The connection to the anterior portion of the superior tibiofibular joint is seen at the 12:00 o’clock position (arrow). Note the classic denervation changes in the anterior compartment muscles. b T2-weighted FSE axial image with fat suppression (TR = 3,000/TE = 49 ms) inferior to a, at the level of the mid-fibular neck, shows cyst within the transverse limb of the articular branch of the nerve (arrowhead) between 12:00 and 2:00 o’clock
Peroneal intraneural cyst. Axial T2-weighted FSE image (TR = 4,800/TE = 84 ms) with fat suppression at the level of the head–neck junction of the proximal fibula demonstrates the joint connection of the intraneural cyst at 12:00 (arrow), cyst within the transverse limb of the articular branch extending from 12:00–3:00 (arrowhead), and intraneural cyst extending proximally toward the common peroneal nerve (asterisk), representing the tail and transverse limb signs, respectively
Extraneural ganglia
The common peroneal nerve was identified in all cases between 4 and 5 o’clock for the cases of extraneural ganglia. The joint connection was more variable, ranging from around the clock face, depending on the location of the capsular defect. The joint connection was also more superiorly located compared with the intraneural ganglia. Similar to the group with intraneural ganglia, the fluid within the superior tibiofibular joint could be best seen at the mid-portion of the fibular head, but the joint connection itself was more superiorly located. The epicenter of the cyst varied considerably with dissection along tissue planes as well as intramuscular, intraosseous, and subcutaneous extension. In all cases, the nerve could be easily distinguished from the cyst. In a single case, the cyst extended laterally from the joint to abut the nerve at the 4 o’clock position of the mid-fibular head on a single image, but the nerve fascicles themselves were unaffected, and the fat plane surrounding the common peroneal nerve was preserved (Fig. 5) and was in fact remote from the nerve on the remainder of the images in the series. The extraneural cysts were more variable in shape than the intraneural ganglia, ranging in shape from oval to round with loculations that could extend along fascial planes.
Extraneural cyst, pseudo-signet ring sign. a Axial T2-weighted FSE with fat suppression (TR = 3,700/TE =45 ms) at the level of the mid-fibular head shows an extraneural cyst arising from the superior tibiofibular joint. The cyst (asterisk) extends posteriorly to abut the common peroneal nerve (arrowhead) simulating the appearance of an intraneural signet ring sign. There is a small amount of fluid within the joint capsule at 11:00 o’clock position (arrow) that could be mistaken for the joint connection of an intraneural cyst. The nerve itself is normal and the fat plane between the nerve and the cyst is preserved, confirming its extraneural location. b Axial T2-weighted FSE image with fat suppression (TR =3,700/TE =45 ms) 5 mm above a at the upper fibular head and superior aspect of the superior tibiofibular joint shows the joint connection (arrow) to the extraneural cyst (asterisk)
Control group
In the normal group, the position of the common peroneal nerve relative to the fibular head could be seen on each study regardless of acquisition technique. The common peroneal nerve was seen consistently at the 4–5 o’clock position at the level of the mid-portion of the fibular head (Fig. 6a). On serial axial images, the peroneal nerve remained intimately associated with the fibular head at the 4–5 o’clock position over several cuts (a distance of 1–2 cm). The transverse limb of the articular branch could be reliably seen in the control group (Fig. 6b) between the junction of the fibular head/neck and the mid-fibular neck. The deep and superficial branches of the peroneal nerve could be seen in all cases at the 3 and 4 o’clock positions at the fibular neck at and just below the level of the articular branch at its junction with the common peroneal nerve.
MRI at 3 T obtained in an symptomatic volunteer. a Axial T1-weighted FSE image (TR =650/TE =18 ms) obtained at the level of the mid-fibular head shows the common peroneal nerve at the 4:30 position (arrow) adjacent to the fibular head. b Axial T1-weighted FSE image (TR =650/TE =18 ms) obtained 8 mm inferior to a shows the terminal branches of the peroneal nerve at the level of the fibular neck. A portion of the transverse limb of the articular branch can be seen between 1:00 and 2:00 o’clock (upper thin arrow). More laterally, one can see the take-off of the trifurcation of the terminal branches: The lower thin arrow shows the more proximal portion of the articular branch, the big arrow shows superficial peroneal branch, and the arrowhead indicates the deep branch of the peroneal nerve
Statistical analysis
For the first analysis, there was no statistical significant difference among all three groups for the location of the nerve between 4:30 and 5:00 (p = 0.99). For the second analysis defining the nerve at 4:30 in reference to the superior tibiofibular joint, there was no statistical difference between all three groups (p = 0.235). For the third analysis between the intraneural and extraneural groups, there was a statistically significant difference in the location of the joint connection (i.e. tail sign) in relation to the fibular head (p < 0.001).
For the intraneural ganglia, the position of the joint connection was 100% of the time at the 11–12 o’clock position on the fibular head and in 100% in the mid location to the superior tibiofibular joint. The extraneural ganglia had wider variation, ranging from 1–12 o’clock (mean, 8.4 ± 3.5), with only 7% located at the mid location in reference to the superior tibiofibular joint.
Discussion
As was recently reported, intraneural ganglia share a joint origin with dissection along an articular branch within the epineurium [1, 2]. This feature has been especially important in the analysis of the prototype peroneal intraneural ganglia but also for rarer sites for intraneural ganglia. This has allowed a thorough understanding of a previously controversial pathogenesis, as misdiagnosis and misinterpretation that before have led to misinformation and mistreatment can be eliminated. Intraneural ganglia are rare (approximately 350 reported cases), and the peroneal nerve is, by far, their most common location. Peroneal intraneural ganglia are nearly always symptomatic with pain and/or neuropathy (i.e., preferentially deep peroneal nerve lesions) and appear tubular. Extraneural ganglia are relatively prevalent in the normal population [5], and when symptomatic, present with pain more so than with neuropathy; they tend to appear globular. Useful imaging signs have been described to identify the joint origin and to classify cysts as intraneural and extraneural. Treatments differ, and this distinction is important. The optimal management of intraneural and extraneural ganglia is unknown. For intraneural ganglia, we perform decompression of the cyst through a limited epineurotomy (and purposefully do not attempt to resect the entire cyst or cyst wall) along with disconnection of the articular branch (to eliminate intraneural recurrences). In extraneural ganglia, we resect the cyst from the soft tissues. To prevent extraneural recurrences, we also resect the superior tibiofibular joint in patients with either intraneural or extraneural ganglia, as we believe that the synovium represents the primary pathology [6, 7]. Furthermore, in some cases, both intraneural and extraneural cysts may coexist, highlighting the need for accurate diagnosis and targeted treatment. In any of these cases, the articular nature is important.
The anatomic understanding of this process has revealed a reproducible pattern that makes for MRI appeal. Previously, we have focused largely on using special techniques with specialized high-resolution studies and advanced imaging (multiplanar, vastly undersampled isotropic projection imaging [VIPR] [8], three-dimensional rendering [9], or MR arthrography [10]) to identify, verify, and corroborate our unified articular theory. As was previously reported, signs can be identified which by themselves were obtained using standard MR images of lower technical quality but demanded complex appreciation, knowledge, and experience to identify joint connections or characterize cyst patterns [3]. The consistency of the anatomy of the peroneal nerve and its branches, shown in this paper to be independent of pathology, can be exploited to reliably diagnose and indeed predict the relationship of cyst to nerve.
This study shows that routinely obtained axial T2-weighted MR images performed over the past decade (even with 0.5 T) on commercially accessible scanners can supply an abundance of information to facilitate characterizing the nature of these complex cystic lesions arising from the anterior portion of the superior tibiofibular joint. Axial images were selected, as they are the most frequent series obtained and easiest to be interpreted for cross-sectional anatomy. These studies of consecutive patients with different imaging parameters from clinically acquired studies of different sized peroneal intraneural ganglia performed without formal protocols with different technicians could be generalized universally. We identified a system using a 12-h clock face for the mid-fibular head and neck with all images analyzed as a left side by convention specifically for peroneal intraneural ganglia. By identifying these individual signs and their consistent anatomic locations, even inexperienced observers should be able to characterize these cysts as intra- or extraneural and to define the extent of cyst extension within the articular branch and common peroneal nerve for intraneural ganglia. Regardless of slice thickness and overall anatomic differences, two single axial images could identify critical features of peroneal intraneural ganglia. One image at the mid-fibular head could demonstrate the presence of cyst within the common peroneal nerve at 4–5 o'clock (signet ring sign), combined with the identification of a joint connection at 11–12 o’clock (tail sign). Another image at the mid-fibular neck could reveal cyst within the transverse limb of the articular branch (transverse limb sign). In addition, in several instances, a single axial image could demonstrate these two signs, i.e.., tail and transverse limb signs, with cyst extension to the common peroneal nerve also visible. Seeing these two signs on a single slice together with the cyst extension towards the common peroneal nerve may be explained by slight obliquity in the image, thicker slice sections, prominent transverse limb cyst dimensions, or even a very small patient with a short fibular head and neck. In all cases, the three signs (tail, transverse limb and signet ring signs) could be seen on consecutive images. Because of the consistency of the anatomy, small differences in the plane of acquisition (i.e., axial to slightly oblique axial) are not confounding and the studies may be analyzed either with a clock face template or by visual assessment with equally robust results.
A rare but notable exception for the combination of these two signs (tail sign at 11–12 o’clock and signet ring sign at 4–5 o’clock) is the case where there is intraneural cyst extension into the articular branch that does not reach the common peroneal nerve at the level of the fibular head. In this case, the joint connection would be seen as usual, but cyst would not be present in the common peroneal nerve but would be seen in the transverse limb of the articular branch. This presentation is the exception rather than the rule; consistently looking for all three signs will identify these rare cases where the joint connection is in the expected location and cyst is present within the articular branch at the fibular neck. Even in the rare case where there is intraneural cyst within the articular branch but no obvious signet ring sign within the common peroneal nerve, there is still subtle evidence of more proximal cyst extension, but this may be difficult to identify without the benefit of high-field, high-resolution examinations.
Another unusual situation may arise when an extraneural cyst is close to and causes mass effect on the common peroneal nerve, creating the so-called pseudo-signet ring sign. Close inspection of the nerve will show the fat plane always seen between the cyst and the nerve (and which is absent in intraneural cysts) and no cyst within the articular branch of the nerve irrespective of the location of the joint connection. Because the cyst itself may closely approximate the nerve, it is critical to identify cyst within and not just near the nerve in order to correctly distinguish intraneural from extraneural ganglia in this location. Even in this unusual instance, careful application of the diagnostic criteria presented in this paper will allow confident distinction of extrinsic mass effect on a nerve from an extraneural cyst and true, primary neural involvement from an intraneural ganglion cyst. Para-articular cysts arising from the posterior aspect of the superior tibiofibular joint may lead to tibial intraneural ganglia [11] but these are easily distinguished from and are rarer than peroneal intraneural ganglia.
Denervation changes in the anterior compartment musculature of the leg as a secondary sign of intraneural involvement of cyst have been reported [3]. While there may be mild denervation changes in the cases of extraneural ganglia causing extrinsic mass effect on either the peroneal (or even tibial) nerves, this is rare compared with intraneural ganglia, where it is a consistent finding and visible on the same axial images as the cyst itself and its joint connection. The combination of these MRI features, i.e., the signet ring sign, tail sign, and denervation changes in the muscles on a single image, is by itself essentially pathognomonic of an intraneural cyst arising from the superior tibiofibular joint, independent of identification of the transverse limb sign.
The strengths of this study are the reproducibility of the anatomy of the superior tibiofibular joint and proximal fibula relative to the common peroneal nerve, which allows reliable distinction of normal and pathologic anatomy with the ability to subcategorize cyst types easily using this method by both experienced and inexperienced observers. Small variations in the anatomy due to body habitus or relatively gracile bones do not detract from the consistency of the anatomic relationships between bone, nerve, and intraneural cyst. Furthermore, we have shown that this can be assessed on routine imaging of the knee even with some variation in acquisition parameters and exam positioning so that special imaging or techniques are not required. Review of figures from published reports from other groups [12–23] shows the same reproducible findings and anatomic relationships described in this paper, even though not recognized as such, further affirming the wide applicability and lack of dependence on a specific method of image acquisition.
The limitations of this study include the relative small number of cases and the variability of image acquisition techniques, specifically, the variability in spatial resolution and slice thickness. In addition, the basic assumption of this paper made on our clinical experience and our unified theory is that these cysts are joint connected. In our study, all observers easily identified the joint connections on the imaging provided but were not blinded to the purpose of study, creating conditions for image review, which are different from routine image review in a clinical setting. Because of the potential bias of our group due to our experience with this rare entity, we look forward to future studies that will corroborate these findings with other cohorts and blinded observers to affirm the validity and reproducibility of our work.
While a wide variety of clinically acquired images may provide the information necessary for identifying cysts and distinguishing between intraneural and extraneural extension, optimized imaging provides more insight and information into the extent and true character of these lesions, which may be of significant value to surgeons for planning purposes. This involves high-field imaging (3 T) when available as well as the use of dedicated radiofrequency coils and the highest possible spatial resolution. Imaging in other planes and high-resolution, isotropic three-dimensional acquisitions such as VIPR will help to better delineate the cysts and their relationship to other critical structures such as vessels and distal nerve branches. Ideally, images would be acquired at 3 T with a minimum slice thickness of 4 mm for the axial images through the fibular head and neck with an interslice gap of no greater than 1 mm. The field of view should not exceed 12–14 cm. If only 1.5 T imaging is available, the slice thickness should be maintained at 4 mm or less and the field of view may be slightly increased (14 cm) to compensate for the lower signal to noise ratio. We recognize that ongoing refinements in MR imaging will make this achievable in most clinical settings in the near future.
Conclusion
Despite recent advances and contributions to the literature on this topic, there remain many instances where intraneural cysts are not properly treated due to a lack of prospective identification of the joint connection on imaging. The use of a simple formulaic approach using standardized conventional imaging technique and a recognizable symbol, a clock face, to interpret these complex cysts and their joint connections and the nature of ganglia affecting the peroneal nerve is meant to simplify and generalize our findings for use outside of a specialized academic setting. By using this simple technique, investigators should be able to better delineate the joint connections we believe are present in all of these cases for improved treatment and more durable clinical outcomes.
References
Spinner RJ, Atkinson JLD, Tiel RL. Peroneal intraneural ganglia. The importance of the articular branch: a unifying theory. J Neurosurg 2003; 99: 330–343.
Spinner RJ, Amrami KK, Wolanskyj AP, et al. Dynamic phases of peroneal and tibial intraneural ganglia: a new dimension added to the unifying articular theory. J Neurosurg 2007; 107: 296–307.
Spinner RJ, Desy NM, Amrami KK. Cystic transverse limb of the articular branch: a pathognomonic sign for peroneal intraneural ganglia at the superior tibiofibular joint. Neurosurgery 2006; 59: 157–166.
Spinner RJ, Carmichael SW, Wang H, Parisi TJ, Skinner JA, Amrami KK. Patterns of intraneural ganglion cyst descent. Clin Anat 2008; 21: 233–245.
Ilahi OA, Younas SA, Labbe MR, Edson SB. Prevalence of ganglion cysts originating from the proximal tibiofibular joint: a magnetic resonance imaging study. Arthroscopy 2003; 19: 150–153.
Spinner RJ, Desy NM, Rock MG, Amrami KK. Peroneal intraneural ganglia. Part I. Techniques for successful diagnosis and treatment. Neurosurg Focus 2007; 22(6): E16.
Spinner RJ, Desy NM, Rock MG, Amrami KK. Peroneal intraneural ganglia. Part II. Lessons learned and pitfalls to avoid for successful diagnosis and treatment. Neurosurg Focus 2007; 22(6): E27.
Amrami KK, Desy NM, Stanley DW, et al. The evaluation of ganglion cysts using vastly undersampled isotropic projection imaging (VIPR). J Magn Reson Imaging 2007; 26: 768–772.
Spinner RJ, Edwards PK, Amrami KK. Application of three-dimensional rendering in joint-related ganglia. Clin Anat 2006; 19: 312–322.
Spinner RJ, Amrami KK, Rock MG. The use of MR arthrography to detect occult joint communication in a recurrent peroneal intraneural ganglion. Skeletal Radiol 2006; 35: 172–179.
Spinner RJ, Mokhtarzadeh A, Schiefer TK, Krishnan KG, Kliot M, Amrami KK. The clinico-anatomic explanation for tibial intraneural ganglion cysts arising from the superior tibiofibular joint. Skeletal Radiol 2007; 36: 281–292.
Leon J, Marano G. MRI of peroneal nerve entrapment due to a ganglion cyst. Magn Reson Imaging 1987; 5: 307–309.
Coakley FV, Finlay DB, Harper WM, Allen MJ. Direct and indirect MRI findings in ganglion cysts of the common peroneal nerve. Clin Radiol 1995; 50: 168–169.
Gayet LE, Morand F, Goujon JM, Pries P, Clarac JP. Compression of the peroneal nerve by a cyst in a seven year old child. Rev Chirurg Orthop 1996; 82: 762–766.
Harbaugh KS, Tiel RL, Kline DG. Ganglion cyst involvement of peripheral nerves. J Neurosurg 1997; 87: 403–408.
Yamazaki H, Saitoh S, Seki H, Murakami N, Misawa T, Takaoka K. Peroneal nerve palsy caused by intraneural ganglion. Skeletal Radiol 1999; 28: 52–56.
Coleman SH, Beredjeklian PK, Weiland AJ. Intraneural ganglion cyst of the peroneal nerve accompanied by complete foot drop. Am J Sports Med 2001; 29: 238–241.
Ostlere S. Imaging the knee. Imaging 2003; 15: 217–241.
Rubin DI, Nottmeier E, Blasser KE, Peterson JJ, Kennelly K. Acute onset of a deep peroneal neuropathy during a golf game resulting from a ganglion cyst. J Clin Neuromusc Dis 2004; 6: 49–53.
Iverson DJ. MRI detection of cysts of the knee causing common peroneal neuropathy. Neurology 2005; 65: 1829–1831.
Singh R, McKenzie GJ, Paterson M. Sudden onset foot drop from peroneal ganglia. J Orthop 2006; 3(4): e20.
Park G-Y, Bae J-H, Lee S-Y, Lee S-M, Song K-S. Common peroneal nerve palsy caused by an intraneural ganglion—a case report. J Korean Acad Rehab 2006; 30: 289–293.
Frank DA, Sangimino MJ. Peroneal nerve palsy secondary to ganglion cyst of the proximal tibiofibular joint in a pediatric patient. Orthopedics 2008; 31: 86.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spinner, R.J., Luthra, G., Desy, N.M. et al. The clock face guide to peroneal intraneural ganglia: critical “times” and sites for accurate diagnosis. Skeletal Radiol 37, 1091–1099 (2008). https://doi.org/10.1007/s00256-008-0545-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-008-0545-1