Abstract
Background
Intraneural ganglion cysts of the peroneal nerve are rare, and there is lack of evidence for the surgical management of this entity. We performed this study to evaluate the imaging, diagnosis, treatment and outcome of seven patients with intraneural ganglion cysts of the peroneal nerve.
Materials and methods
We retrospectively studied the files of seven patients with intraneural ganglion cysts of the peroneal nerve, diagnosed and treated from 2016 to 2019. Diagnostic approach included clinical examination of the leg and foot, magnetic resonance imaging, nerve conduction studies, surgical excision of the cyst and histological examination. The mean follow-up was 2 years (range 1–3.5 years). We evaluated the time and methods for surgical treatment, and the clinical outcomes of the patients.
Results
All patients presented symptoms of peripheral compression neuropathy; three patients presented with foot drop. The intraneural ganglion cysts were excised in all cases in addition to knee articular nerve branch transection to avoid cysts recurrence. Postoperatively, all patients experienced complete neurological recovery without clinical evidence of intraneural ganglion cysts recurrences.
Conclusion
The treating physicians should be aware of intraneural ganglion cysts of the peroneal nerve in patients presenting with limb weakness, sensory deficits at the lateral and anterior side of the leg and foot, paresis or paralysis of the foot and ankle. MR imaging is the imaging modality of choice for a clear and accurate preoperative diagnosis to avoid misdiagnosis and wrong treatment. In case of doubt, these patients should be managed in an orthopedic oncology setting with microsurgery facilities available for complete excision of the intraneural ganglion cyst.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
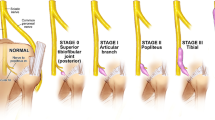
Intraneural ganglion cysts are benign cystic formations in the epineurium of nerves that usually contain a clear, jelly-like fluid [1]. Most commonly they involve the common peroneal nerve and rarely the ulnar and radial nerves [2, 3]. The common peroneal nerve (L4-S2 nerve roots origin) arises at the superior angle of the popliteal fossa and extends to the lateral angle of the popliteal fossa, along the medial border of the biceps femoris muscle. Entering the lateral compartment of the leg, it winds around the neck of the fibula to pierce the peroneal longus muscle and divides into terminal branches of superficial fibular nerve and deep fibular nerve [4]. At this point, intraneural ganglion cysts may occur [3, 5, 6].
The pathogenesis of peroneal intraneural ganglion cysts is unknown. Recently, evidence mainly supports the synovial theory, according to which intraneural ganglion cysts occur by a retrograde flow of synovial fluid of the knee joint, through a capsular defect, into the epineurium of an articular branch of the peroneal nerve and then into the common peroneal nerve [5]. Peroneal intraneural ganglion cysts typically lead to signs and symptoms of compressive peripheral neuropathy such as pain, sensory disorders and weakness or paralysis of the muscles supplied by the peroneal nerve. The diagnosis is obtained with magnetic resonance (MR) imaging. Τhe treatment of choice is surgical excision of the lesion, with optimal postoperative results. The local recurrence rate after excision is high if the cyst is not removed completely, and/or if the articular branch to the knee joint is not transected intraoperatively [6].
To enhance the literature, this article presents a series of seven patients who underwent successful surgical excision of intraneural ganglion cysts of the peroneal nerve. The aim is to discuss the clinical presentation, imaging diagnosis of the lesions and surgical treatment of the patients, as well as to increase the awareness of the treating physicians for the possible diagnosis of intraneural ganglion cysts in patients with neurological symptoms in the foot.
Patients and methods
We retrospectively studied the files of seven patients who were admitted and treated at the authors’ institutions with intraneural ganglion cysts of the peroneal nerve from May 2016 to October 2019. There were four women and three men, with a mean age of 52.5 years (range 29–68 years). Four patients presented with paresis and three patients presented with paralysis of the ankle and foot dorsi-flexors (tibialis anterior, extensor digitorum longus and extensor hallucis longus) and foot evertors (peronei); all patients experienced hypoesthesia in the anterolateral side of the affected leg. No patient experienced a palpable mass at the head/neck area of the fibula, and no patient reported any previous history of trauma to the region. The mean time from initiation of neurological symptoms to presentation and diagnosis was 2.5 months. The mean follow-up was 2 years (range 1–3.5 years). No patient was lost to follow-up. All patients gave written informed consent for their data to be included in this study.
Anteroposterior and lateral radiographs of the knee were normal in all cases. Nerve conduction studies showed that the common peroneal nerve was affected at the fibular neck level in all cases, with a mean motor nerve conduction velocity (NCV) tibial of 41.35 m/s and a mean motor NCV peroneal of 35.3 m/s (Table 1). The Medical Research Council muscle (MRC) scale for muscle power assessment showed a mean grade 1–2/5 of dorsiflexion in all patients and variable eversion deficit in three patients. MR imaging showed a mean of 4.25 cm in maximum diameter cystic lesion at the point where the common peroneal nerve divides into the superficial peroneal nerve and the deep peroneal nerve in all patients (Fig. 1a–c).
A 54-year-old man with paralysis of the left common peroneal nerve (Table 1; Patient 1). T2-weighted a axial, b sagittal and c coronal MRI of the left knee show a cystic fluid-filled mass in close proximity to the common peroneal nerve. d Through a direct approach over the course of the peroneal nerve centered 2 cm posterior to the fibular head, e the nerve was identified and dissected, and f using microsurgical technique the ganglion cyst was g excised. Due to hourglass compression of the peroneal nerve (arrows), h external neurolysis followed by i longitudinal epineurotomy and limited internal neurolysis to release the fascicles was done. The patient experienced complete recovery of his neurological symptoms 9 months postoperatively.
All patients were operated under general anesthesia in the supine position. The procedure was performed using high thigh tourniquet. The skin incision was done along the posterior border of the fibular head and extended proximally along the lateral border of biceps femoris tendon (Fig. 1d). Using microsurgical dissection with 3 × binocular loupes magnification, the common peroneal nerve was identified and released from adhered fibers of the long peroneal muscle and its fascia (Fig. 1e). With careful dissection, the entire ganglion cysts that infiltrated the common peroneal nerve were completely excised (Fig. 1f, g), and sent for pathology in all cases. The articular nerve branch of the common peroneal nerve was transected in all cases. Due to presence of hourglass compression of the nerve, under loupes magnification, external neurolysis was done aiming for complete nerve decompression (Fig. 1h–i).
Results
Macroscopic (Figs. 2a–d , 3a–c) and microscopic examination of the lesions showed ganglion cysts in all patients. The cysts had a smooth lining and a wall thickness ranging from 1 to 5 mm. Microscopically, the wall of the cysts was formed by hyalinized paucicellular connective tissue.
A 29-year-old man with paralysis of the right common peroneal nerve (Table 1; Patient 2). T2-weighted a axial and b sagittal MR imaging of the right knee showed a cystic fluid-filled mass in proximity to the right common peroneal nerve. c Intraoperatively, an intraneural ganglion cyst was observed (arrows). d The cyst was excised after rupture its sheath. The patient experienced complete recovery of his neurological symptoms 7 months postoperatively.
A 68-year-old woman with paresis of the left common peroneal nerve (Table 1; Patient 3). a T2-weighted MR imaging of the left knee showed a cystic fluid-like mass in close proximity to the common peroneal nerve. b The ganglion cyst was carefully dissected and c completely excised. The patient experienced complete recovery of her neurological symptoms 3 months postoperatively.
Postoperatively, the neurological status improved in all patients at an average time to achieve MRC grade 4–5/5 of dorsiflexion of 6 months. Muscle weakness and loss of sensation persisted the first few weeks after the operation but recovered completely in all patients gradually, within 3 months to 9 months (mean, 5 months). No clinical evidence of ganglion cysts recurrence (palpable mass or neurological deficits) was reported until the period of this study. No medical therapies associated with the surgical operation were administered postoperatively to any of the patients in this series; an ankle and foot orthosis was used until neurological recovery in the three patients with paralysis of the ankle and foot dorsi-flexors. No imaging or nerve conduction studies were done in any of the patients postoperatively because of the lack of clinical findings at follow-up; in case of clinical findings (palpable mass) and recurrent neurological deficits, an MR imaging study would have been performed.
Discussion
Peroneal nerve palsy is one of the most common peripheral neuropathies of the lower extremity [3, 4, 7,8,9]. Previous studies have reported that multiple causes are responsible for this condition that often leads to motor and sensory deficits of the limb. External compression is the most common cause, but other causes such as trauma, tight casts, systematic metabolic diseases and prolonged bed rest may also exist [8, 9]. Additionally, not only a direct trauma can cause peroneal palsy, but also and indirect trauma such as an ankle sprain may lead to peroneal nerve neurapraxia from stretch injury [7,8,9]. Intraneural ganglion cysts are rare causes of peripheral neuropathy and can affect any peripheral nerve. Usually, these cysts affect the common peroneal nerve and secondarily the ulnar and the radial nerve. The incidence of intraneural ganglion cysts is lower in children and adolescents [10,11,12]. Intraneural ganglion cysts are non-neoplastic cysts that occur within the epineurium of the nerve. The main difference between intraneural ganglion cysts and other types of ganglion cysts is their relation to the nerves [13]. Conservative treatment is not recommended due to poor results; surgical treatment is successful in all cases with restoration of the nerve function, and limb mobility and sensation [3, 5, 10, 11]. However, to avoid iatrogenic nerve injury, careful nerve dissection and decompression using a microsurgical technique are recommended [10, 11, 14]. Additionally, to prevent recurrence of the cyst, excision of the knee articular branch has been recommended [14].
Studies regarding intraneural ganglion cysts are limited [2, 3, 5,6,7, 10, 13,14,15,16,17,18]. In a retrospective study of 65 patients who underwent surgical excision of intraneural ganglion cysts of the peroneal nerve [3], the motor and sensory outcomes were excellent postoperatively and poor postoperative results were related only to the time from onset of symptoms to surgical treatment. Although the optimal time of surgical excision is unclear, early surgery is recommended to avoid permanent nerve damage from nerve compression [15]. The size of the intraneural ganglion cyst and the age of the patients do not seem to be related to a poor prognosis. Imaging evidence of intraneural ganglion cysts recurrence was 9%, but symptomatic clinical recurrence rate was 6% [16]. Preservation of the knee articular branch of the peroneal nerve has been related to higher local recurrence rates of recurrence because of its anatomical position; therefore, excision or cauterization of the nerve branch has been recommended [3]. Degeneration of the proximal tibiofibular joint is an additional factor for local recurrence of intraneural ganglion cysts of the peroneal nerve after adequate surgical excision [6, 14,15,16,17]. Preservation of the proximal tibiofibular joint’s synovium that is responsible for the production of joint fluid is closely related to high risk of recurrence [6, 14,15,16,17]. For this reason, complete superior tibiofibular joint excision has been recommended to minimize the risk of intraneural ganglion cysts recurrence; excision of the joint has not been associated with joint instability provided that the lateral collateral ligament that is the main stabilizer of this joint has been preserved during exposure of the superior tibiofibular joint [6, 14, 17]. In the present series, in line with the literature (Table 2), we performed complete intraneural ganglion cysts excision and decompression of the peroneal nerve with careful external neurolysis, and transection of the knee articular branch in all patients to avoid recurrences.
In conclusion, intraneural ganglion cysts of the peroneal nerve are often misdiagnosed due to the rarity of this entity and the non-specific clinical presentation. The treating physicians should be aware of this entity in patients presenting with limb weakness, sensory deficits at the lateral and anterior side of the leg and foot, paresis or paralysis of the foot and ankle. MR imaging is the imaging modality of choice for a clear and accurate preoperative diagnosis to avoid misdiagnosis and wrong treatment (whoops surgery). In case of doubt these patients should be managed in an orthopedic oncology setting with microsurgery facilities available for complete excision of the intraneural ganglion cyst. If performed early, complete recovery of nerve deficits is the rule.
References
Kokkalis ZT, Stavropoulos NA, Mavrogenis AF, Panagopoulos A, Soucacos PN (2019) Benign peripheral nerve tumors. Injury 50(Suppl 5):S77–S83. https://doi.org/10.1016/j.injury.2019.10.054
Spinner RJ, Mikami Y, Desy NM, Amrami KK, Berger RA (2018) Superficial radial intraneural ganglion cysts at the wrist. Acta Neurochir 160(12):2479–2484. https://doi.org/10.1007/s00701-018-3715-5
Wilson TJ, Mauermann ML, Rock MG, Spinner RJ (2018) Outcomes following surgery for peroneal intraneural ganglion cysts. Muscle Nerve 57(6):989–993. https://doi.org/10.1002/mus.26062
Drake Richard A, Vogl W, Mitchell Adam WM (2014) Gray’s anatomy for student’s. Churchill Livingstone, Toronto, Ontario, Canada, p 1192
Spinner RJ, Atkinson JL, Scheithauer BW, Rock MG, Birch R, Kim TA, Kliot M, Kline DG, Tiel RL (2003) Peroneal intraneural ganglia: the importance of the articular branch. Clin Ser J Neurosurg 99(2):319–329. https://doi.org/10.3171/jns.2003.99.2.0319
Wu P, Xu S, Cheng B, Chen L, Xue C, Ge H, Yu C (2019) Surgical treatment of intraneural ganglion cysts of the ulnar nerve at the elbow: long-term follow-up of 9 cases. Neurosurgery 85(6):E1068–E1075. https://doi.org/10.1093/neuros/nyz239
Spinner RJ, Crnkovich F, Ahmed M, Kobeal I, Amrami KK (2012) Can trauma cause tibial intraneural ganglion cysts at the superior tibiofibular joint? Clin Anat 25(6):785–787. https://doi.org/10.1002/ca.22079
Mitsiokapa E, Mavrogenis AF, Drakopoulos D, Mauffrey C, Scarlat M (2017) Peroneal nerve palsy after ankle sprain: an update. Eur J Orthop Surg Traumatol 27(1):53–60. https://doi.org/10.1007/s00590-016-1845-0
Mitsiokapa EA, Mavrogenis AF, Antonopoulos D, Tzanos G, Papagelopoulos PJ (2012) Common peroneal nerve palsy after grade I inversion ankle sprain. J Surg Orthop Adv 21(4):261–265. https://doi.org/10.3113/jsoa.2012.0261
Apel PJ, Zielinski JA, Grider DJ, Brown RD, Orfield NJ (2020) Intraneural peroneal ganglion cyst excision in a pediatric patient: a case report. JBJS Case Connect 10(1):e0272. https://doi.org/10.2106/JBJS.CC.19.00272
Desy NM, Wang H, Elshiekh MA, Tanaka S, Choi TW, Howe BM et al (2016) Intraneural ganglion cysts: a systematic review and reinterpretation of the world’s literature. J Neurosurg 125:615–630. https://doi.org/10.3171/2015.9.JNS141368
Desy NM, Spinner RJ (2016) Pediatric intraneural ganglia: the value of a systematic review for “Orphan” conditions. World Neurosurg 91:658–659. https://doi.org/10.1016/j.wneu.2015.11.024
Lisovski V, Minderis M (2019) Intraneural ganglion cyst: a case report and a review of the literature. Acta Med Litu 26(2):147–151. https://doi.org/10.6001/actamedica.v26i2.4036
Spinner RJ, Desy NM, Rock MG, Amrami KK (2007) Peroneal intraneural ganglia. Part II. Lessons learned and pitfalls to avoid for successful diagnosis and treatment. Neurosurg Focus 22:E27
Keser N, Akpinar P, Is M, Aktas I (2018) Irreversible footdrop as a consequence of neglected knee pain in an adolescent with a peroneal intraneural ganglion cyst. World Neurosurg 111:307–310. https://doi.org/10.1016/j.wneu.2017.12.168
Lucattelli E, Menichini G, Brogi M, Roselli G, Innocenti M (2019) Long-Term functional outcome after surgical treatment of peroneal intraneural ganglion cyst. World Neurosurg 132:e217–e222. https://doi.org/10.1016/j.wneu.2019.08.195
Wilson TJ, Stone JJ, Howe BM, Rock MG, Spinner RJ (2020) Joint outcomes following surgery for superior tibiofibular joint-associated peroneal intraneural ganglion cysts. Neurosurgery 86(3):383–390. https://doi.org/10.1093/neuros/nyz205
Akcakaya MO, Shapira Y, Rochkind S (2013) Peroneal and tibial intraneural ganglion cysts in children. Pediatr Neurosurg 49(6):347–352. https://doi.org/10.1159/000368838
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kokkalis, Z.T., Kalavrytinos, D., Kokkineli, S. et al. Intraneural ganglion cysts of the peroneal nerve. Eur J Orthop Surg Traumatol 31, 1639–1645 (2021). https://doi.org/10.1007/s00590-021-02903-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-02903-7