Abstract
Borderline acetabular dysplasia refers to mildly sub-normal patterns of acetabular shape and coverage that might predispose children to mechanical dysfunction and instability. Borderline dysplasia generally includes children with a lateral center edge angle (CEA) of 18–24°. Some children with borderline radiographic measurements have normal joint mechanics and function while others benefit from acetabular reorienting surgery. Although radiographic findings of borderline dysplasia might suggest instability, the ultimate diagnosis is based on history and physical exam in addition to imaging. Children with borderline acetabular dysplasia sometimes benefit from other cross-sectional imaging studies such as MR imaging to evaluate for secondary evidence of instability, including damage along the acetabular rim, or labral degeneration and hypertrophy. CT is also helpful for depiction of 3-D acetabular morphology for preoperative assessment and planning. Pediatric radiologists are often the first to identify borderline or mild dysplasia on radiographs. It is imperative that pediatric radiologists serve as effective consultants and offer appropriate recommendations as part of a cohesive multidisciplinary approach to this complex patient population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Developmental hip dysplasia (DDH) is one of the most important and most common pediatric musculoskeletal conditions. While as many as 80% of cases are present at birth, many remain undiagnosed. When present in infancy, DDH might be detected on the basis of physical examination findings (i.e. Barlow and Ortolani maneuvers) and static and dynamic ultrasound features originally described by Graf [1, 2]. The long-term implications of DDH are significant because the condition leads to development of osteoarthritis in 25–50% of patients by the age of 50 years [3]. The reduced size and the increased obliquity of the acetabular weight-bearing surface create shearing forces on the articular cartilage and cause chronic overloading of the anterior and anterolateral acetabular rim [4]. This mechanical dysfunction, if uncorrected, leads in adulthood to pain, abductor fatigue and often symptoms of instability, culminating in gradual failure of the cartilage and leading to progressive osteoarthritis.
Treatment strategies depend on the mechanical stability of the hip and the type and degree of bony deformity. In infants with mild DDH, capsular laxity and mild acetabular dysplasia are the issues, and simple positioning of the hips in abduction and flexion in a protective brace or Pavlik harness usually leads to tightening of the capsule and resolution of the dysplasia. In children with full congenital dislocations, particularly if diagnosed after infancy, a formal manipulative reduction might be required, with spica casting for several months. At any age, treatment is focused on reducing and maintaining the femoral head to a concentric position within the acetabulum. If bony malalignment is present in the older child with DDH, realignment surgery is often needed to restore stability. Infants and children with developmental hip dysplasia might be treated to cure by virtue of these early strategies, or they might have persistent subluxation that requires further surgery later in adolescence or young adulthood.
Dysplasia in adolescents
Adolescents and young adults who had been asymptomatic with respect to the hip might also have mild forms of acetabular dysplasia detected on radiographs based on criteria originally defined by Wiberg (Figs. 1 and 2) [5]. In many children the indication for radiographs is hip pain, though for some children radiographs are performed for other indications. In the absence of a dedicated examination by a hip specialist who can assess for signs or symptoms of instability, it is not known whether mild or subtle radiographic abnormalities are the source of the child’s symptoms. Radiographic measurements of femoral head coverage and position might suggest the possibility of mechanical dysfunction of the hip, though it is the mechanics that define the underlying disease, not the radiographs. In contrast to infantile DDH, adolescent dysplasia has a higher male predominance and is more often bilateral [6]. The difference in demographics between groups has prompted many to question whether adolescent and infantile hip dysplasias are two distinct entities.
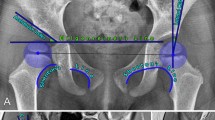
Radiographs of the hip in a 16-year-old girl demonstrate measurement technique for lateral center edge angle (CEA), acetabular index, and anterior CEA. a Three points are marked for subsequent measurements: Point 1 at the center of the femoral head, Point 2 at the medial edge of the sourcil, Point 3 at the lateral edge of the sourcil. b Anteroposterior pelvic radiograph coned down to the right hip demonstrates technique for measuring lateral CEA. The lateral CEA is the angle formed between the line connecting Point 1 to Point 3 and a vertical line (normal 25–40°). c Acetabular index is determined by the angle formed between a line connecting Point 2 to Point 3 and a horizontal line (normal 0–10°). d False profile view of the right hip demonstrates measurement technique for determining anterior CEA. Anterior CEA is determined by the angle between a line from Point 1 to Point 4 (at the anterior margin of the sourcil) and a vertical line (normal 25–40°)
Severe bilateral hip dysplasia in a 19-year-old woman. a Anteroposterior radiograph of the pelvis demonstrates a lateral center edge angle (CEA) of the right hip of 5° and (b) acetabular index of 16°. The left hip is similarly dysplastic. c False profile radiograph of the right hip demonstrates anterior center edge angle of 8°
The standing anteroposterior (AP) radiograph of the pelvis remains the gold standard of imaging for adolescent hip dysplasia, supplemented by other views including the false profile radiograph [4]. A number of radiographic measurements have been described that define the dysplastic hip, the three most fundamental including the lateral center edge angle (CEA), the acetabular index and the anterior CEA [7]. The lateral CEA and the acetabular index are both measured on a properly positioned standing AP radiograph of the pelvis, whereas the anterior CEA is measured on the false profile radiograph (Figs. 1 and 2). In 1939 Wiberg [5] defined a normal lateral CEA as being over 25°, an abnormal angle as less than 20° (Fig. 2) and everything in between as uncertain. These ranges were validated in subsequent investigations [8, 9]. Similar criteria exist for the anterior CEA as measured on a false profile radiograph, where this angle is considered normal above 25°, borderline at 20–24° and deficient below 20° (Fig. 2) [10]. In certain children the anterior acetabular roof insufficiency is more severe than the lateral roof insufficiency, and the false profile view might help to identify these children, with the caveat that the anterior CEA is the most dependent on radiographic technique [11]. The acetabular index is considered normal at 0–10° [7], though some have suggested that angles up to 13° are normal [8]. Values above this are considered indicative of dysplasia.
Borderline measurements
While florid acetabular dysplasia is incontrovertible when identified radiographically (Fig. 2), the correct diagnosis becomes more difficult when the measurement angles are only mildly out of the normal range, leading to the creation of an “uncertain” or “borderline” category (Figs. 3 and 4). These children remain a source of confusion and controversy among radiologists and hip specialists. Ultimately, a child falling into an uncertain category has either a healthy or an unhealthy hip, and this distinction depends on a variety of factors unique to each child that go beyond a simple radiographic measurement. The label “borderline dysplasia” has been adopted to define a group that falls into an uncertain measurement category with lateral CEA of 18–24° [12,13,14], in whom further evaluation is necessary before a diagnosis can be made.
Borderline lateral center edge angle (CEA) in a 16-year-old girl with right hip pain. a Anteroposterior (AP) pelvis radiograph reveals borderline lateral CEA of 19°. The left hip is normal. b False profile radiograph of the same girl reveals anterior CEA of 19°. c Coronal T1 map from delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) examination reveals normal cartilage. The girl did not have signs of instability, was treated for psoas strain, and symptoms improved without surgery. Because psoas strain could still be related to underlying microinstability, the girl was under long-term observation under care of a hip surgeon
Left hip pain in an 11-year-old female soccer player with a family history of hip dysplasia. a Anteroposterior (AP) radiograph interpreted as normal. b Girl now is age 13 years, still with left hip pain. Bilateral hips were considered shallow, with lateral center edge angle (CEA) measured at 16° on the left and 23° on the right. Acetabular index on the left was also considered elevated at 13°. Positive apprehension test reflected instability of the left hip on physical examination, with no instability noted on the right. c False profile radiograph reveals adequate anterior coverage, with anterior CEA of 27°. d AP pelvis radiograph status post left-side periacetabular osteotomy demonstrates improved lateral coverage. The girl reported improved symptoms. e AP pelvis radiograph 1 year later, after relief of symptoms and return to normal activity. She had mild intermittent pain on the right and was being monitored periodically for symptoms
Given the mechanical basis for the joint damage in acetabular dysplasia, it is a reasonable assertion that hips with slightly diminished coverage are predisposed to joint damage related to increased wear on the acetabular rim. Children with mild dysplasia are known to have evidence of labral and cartilage damage at hip arthroscopy [15]. This does not mean that all children with a lateral CEA of 18–24° develop osteoarthritis. Early studies evaluating the relationship between center edge angle and dysplasia focused primarily on hip function rather than specific evidence of joint damage [16], though it is likely that normally functional hips might over time also have labral tears and cartilage lesions.
Delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) measurements
Delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) was developed to identify hips with early biomechanical damage to the cartilage matrix in advance of morphologic cartilage loss [17]. When introduced via intravenous or intraarticular injection, an anionic molecule such as gadopentetate−2 (Gd-DTPA−2) distributes over time in cartilage inversely to the concentration of negatively charged glycosaminoglycans. The concentration of Gd-DTPA−2 can be indirectly determined with measurements of T1 and is expected to be lower in normal cartilage compared to degraded cartilage with loss of glycosaminoglycans. This measurement is referred to as the “dGEMRIC index” (Fig. 3). Evaluation of the dGEMRIC index in people with no or mild dysplasia revealed that the dGEMRIC index of mildly dysplastic hips did not differ significantly from that of normal hips [17]. It should be noted that in this study people with mild dysplasia were defined by a lateral CEA >15°, which is lower than what would now be considered the threshold of mild dysplasia. These data suggest that children with mild or borderline dysplasia might not be at increased risk of developing end-stage osteoarthritis, though because these people were not followed longitudinally over time it is unknown whether cartilage degeneration evolved over time. The dGEMRIC index also does not address whether children have signs or symptoms of instability, which might be what brings them to medical attention.
Radiographic landmarks
Measurements obtained from conventional radiographs rely on identification of precise landmarks, including the center of the femoral head, the medial margin of the acetabular sourcil, and the lateral margin of the acetabular sourcil (Fig. 1). The sourcil is not always well-defined, especially in children younger than 15 years. In younger children it is uncommon for the lateral margin of the sourcil to also be the lateral margin of the acetabulum, prompting some investigators to develop a “modified lateral CEA” that includes only the sclerotic portion of the acetabular sourcil. This is in contrast to the traditional CEA, which is measured to the lateral acetabular margin [18]. The range of normal depends on technique because the modified angle has a lower standard range (15–20°) compared to the traditional angle. Without strict attention to radiographic landmarks the variability between measurements can be extreme [19,20,21]. The most reliable method is to automate the process with computer-aided software, either by incorporating a computerized measurement program [22] or by standardizing the projection of the radiograph [23]. Unless rigorous criteria are being used for measurement, a mildly abnormal measurement should not be considered a mark of disease unless there are other compelling imaging and clinical findings. An ad hoc measurement performed by “eyeballing” the radiograph is unlikely to be accurate. It is best to measure multiple times, especially in the absence of computer-aided systems.
Normal variants
Crossover sign
Radiologists are wise to proceed cautiously around the hip, given the frequency with which previously reported radiographic measurements or findings have been subsequently determined to represent normal variants. An example of this is the crossover sign on the AP pelvis radiographs. In 2007 it was demonstrated that the presence of a crossover sign was a highly reliable indicator of cranial (superior acetabular) anteversion of less than 4° [24]. For reference, the superior aspect of the acetabulum is anteverted approximately 10–14°. At angles less than 0°, the anterior wall is lateral to the posterior wall, leading to the crossover sign on radiographs where the two walls overlap. It became standard for radiologists and hip specialists to comment on the presence of a crossover sign on AP radiographs of the pelvis as suggestive of acetabular retroversion. In clinical practice, however, these children did not always have signs or symptoms of retroversion, nor did cross-sectional imaging confirm retroversion. Over time, the literature refuted an association between crossover sign and clinically confirmed acetabular retroversion. Even asymptomatic children without hip disease or symptomatology demonstrated a crossover sign on a well-positioned radiograph, reflecting variations in patient positioning as well as the variable morphology of the anterior inferior iliac spine [25, 26].
Coxa profunda
In similar fashion, the term “coxa profunda” fell in and out of favor almost as quickly. Coxa profunda is defined as present if the floor of the acetabular fossa lies medial to the ilioischial line. It is considered an indirect sign of acetabular over-coverage of the femoral head and was proposed as an imaging feature of pincer-type femoroacetabular impingement in 2007 [27]. With this awareness, radiologists readily offered this imaging finding as evidence of an underlying condition: acetabular over-coverage. Over time, coxa profunda was claimed to be a normal radiographic finding that does not support a diagnosis of pincer impingement [28,29,30].
Cam deformity
Finally, the definition of “cam” deformity in children with femoroacetabular impingement has been a subject of interest and debate for many years. Cam lesions are bony protuberances along the femoral head/neck junction that impinge against the acetabular rim in hip flexion. The most objective means of measuring the size of a cam deformity is the alpha angle, an angle formed by a line connecting the center of the femoral head to the center of the femoral neck, and a line from the center of the femoral head to the point at which the femoral neck falls outside a best-fit circle around the head. In the early 2000s it was accepted that children with an alpha angle in the range of 50° likely had cam-type femoroacetabular impingement (FAI) [31,32,33,34]. Over the last decade there has been increasing awareness that some previously defined cam lesions in people with FAI might be present in asymptomatic populations with no hip disease [35,36,37,38]. Moreover a positive impingement test, often associated with the presence of anterior FAI, has been demonstrated in healthy young adults who might not have FAI [39], making this an unreliable indicator of disease in isolation of other evidence.
Radiographic technique
Given that our interest in identifying and treating painful and debilitating disease in children might outpace our understanding of normal anatomical variation, radiologists need guidelines for interpreting radiographs that reveal an uncertain degree of femoral head coverage. A cautious approach would be to suggest the possibility of borderline hip dysplasia and recommend referral to a hip specialist. This recommendation should be performed when the imaging findings have been deemed reliable, which requires strict adherence to proper imaging technique. The following should be assessed on every AP radiograph of the pelvis:
-
(1)
Is the pelvis tilted or rotated? As a guideline, the distance between the superior edge of the pubic symphysis and the coccyx should be 1–3 cm [40].
-
(2)
How well defined are the measurement landmarks? If there is doubt as to where the landmarks are located, the measurements are likely to be inaccurate.
-
(3)
Are measurements performed using electronic calipers or with a validated computer-assisted program? If performed by hand, have the initial measurements been validated with a repeat attempt?
-
(4)
Is the patient older than 15 years, and if not is the modified lateral CEA standard being employed rather than the classic lateral CEA?
The answers to these questions have a great impact on the reported measures. If the imaging technique is adequate and the child still falls into an indeterminate category of the borderline dysplastic (a lateral CEA that falls between 18° and 24°), this is still only the first step in a complex diagnostic process. Our understanding of hip disease has evolved considerably over the last decade. It is impossible to accurately characterize all of the different patterns of instability and under-coverage with 2-D radiographic views. Relying solely on the lateral CEA to determine normal versus deficient coverage assumes all dysplasia is global, or primarily involves the superior acetabulum. We now know that at least three distinct patterns of acetabular deficiency exist: anterosuperior, global, and posterosuperior insufficiency [41], and AP radiographs are not designed to detect a focal anterior or posterior deficiency. The presence of borderline dysplasia on radiographs also does not confirm the presence of instability, which is ultimately what leads to symptoms and joint damage. The presence or absence of instability or impingement must be determined through careful history and physical exam, as well as from static and possibly dynamic imaging. The femoro-epiphyseal acetabular roof (FEAR) index has been proposed as a useful radiographic marker of instability (Fig. 5) [42]. Another helpful radiographic clue to the presence of instability is the upsloping lateral sourcil margin [43]. All of these observations, however, require further validation before they can be considered reliable markers of disease.
Femoro-epiphyseal acetabular roof (FEAR) index. a Anteroposterior (AP) radiograph of the hip in the same 16-year-old girl as in Fig. 1. The FEAR index is the angle formed between a line connecting Point 2 and Point 3 along the acetabular roof (black lines), and a line drawn along the central third of the femoral physeal scar (white line). A positive FEAR index is defined by a laterally directed angle with the apex pointing medially. The FEAR index in this girl is less than 5°. A FEAR index >5° has a greater correlation with instability compared to FEAR index <5°. b AP radiograph of the hip in a 13-year-old girl with mild left acetabular sourcil demonstrates a mildly upturned lateral sourcil (arrow). c Normal AP radiograph of the left hip in a 13-year-old boy with right hip pain demonstrates a normal lateral sourcil for comparison. The black line indicates the acetabular roof and the white line indicates the central third of the physeal scar. The FEAR index is demonstrated in this normal hip to illustrate a negative FEAR index with the apex of the angle directed laterally
Wiberg [5] laid the important groundwork with his seminal article describing the “normal” lateral coverage of the femoral head, and for many decades those assertions have not been disproved; subsequent investigations have only substantiated his original findings [44,45,46], though the lower end of the normal threshold has shifted more toward the dysplastic end of the spectrum. Larger population-based studies have recently suggested that these ranges are gender-specific and that male and female patients should not be measured against the same standard. Updated reference standards proposed by Laborie et al. [39] suggested that cutoff values for male patients should be 21° compared to 20° in female patients. Updated upper threshold values for acetabular index according to this study were 15° for males and 16° for females, compared to previous published threshold of 10° for both groups. According to these new criteria, many patients who had previously been characterized as mildly or borderline dysplastic might now be considered normal. Additionally, age, gender, height and body mass index (BMI) have been found to be factors in what are considered to be normal ranges of acetabular coverage, shifting the lower range of normal coverage further into the dysplastic range for certain populations [47].
Advancing investigation
The term “borderline dysplasia” is also falling out of favor. Advanced imaging modalities have revealed patterns of dysplasia that are not apparent on radiographs. Focal anterior and posterior dysplasia groups have a normal lateral CEA on the AP radiograph [9]. Refined and updated radiographic measurements have been proposed that would enable better identification of children with focal dysplasia, such as the anterior wall index and posterior wall index [48]. Early studies demonstrated differences in the anterior and posterior wall indices in symptomatic dysplastic patients compared to those with a normal acetabulum [48]. Subsequent investigation revealed that even asymptomatic people have radiographic anterior and posterior wall index measurements that overlap those of people with dysplasia [49]. This indicates that some degree of variation in the 3-D morphology of the acetabulum is normal. Further validation of these indices with cross-sectional imaging and longitudinal follow-up is necessary before these new reference standards can be considered reliable indicators of disease.
In the presence of instability related to acetabular dysplasia, there is often overgrowth of soft-tissue structures that compensates for the deficient bony support. This includes enlargement of the acetabular labrum [50, 51], even in the absence of labral tear or degeneration. Focal muscle enlargement has also been noted in unstable patients, specifically the iliocapsularis muscle [52]. MRI might be useful in identifying these secondary signs of instability. Still, no clearly positive findings confirm the presence of instability. Femoral version is also a key component in determining hip stability, as an anteverted femur is be more anteriorly uncovered than a neutral femur [53]. Overt features of acetabular rim damage also support the diagnosis of dysplasia, including labral degeneration and tearing and cartilage loss, though adolescents who have borderline dysplasia might not yet have visible manifestations of osteoarthritis, even if instability is the pain generator.
Given these areas of investigation and uncertainty, the borderline dysplastic hip has attracted well-deserved attention in the literature. Specific concerns have been raised around whether the term “borderline dysplasia” is an adequate label and whether this is a single condition. It is more likely that children with a borderline lateral CEA of 18–24° consist of clusters of patients, some of whom might have cam impingement, and some of whom have focal acetabular deficiency [13]. Specific patterns of acetabular deficiency and femoral morphology are best characterized with cross-sectional imaging examinations, such as MRI or CT, which might also detect other causes for hip pain. It is recommended that any child in whom there is concern for dysplasia undergo an MRI as part of a complete evaluation because there might be another finding that explains the child’s symptoms (Fig. 6), or evidence of intra-articular damage that supports rim loading. MRI is well suited for detecting cartilage and labral abnormalities as well as marrow lesions that are present in the setting of altered biomechanics and early osteoarthritis [8]. Low-dose pelvic CT is also valuable for preoperative assessment of the hip morphology with precise characterization of the bony deficiencies in three dimensions. It is crucial that these children are directed to an experienced hip specialist who is able to contextualize the imaging findings with a comprehensive physical exam and an appropriate history. These children should be interrogated with respect to the nature and location of their pain with specific questions around instability. A comprehensive physical exam should follow, including attention to the child’s gait, pelvic position and rotational profile.
Imaging in an 18-year-old female track athlete with right hip pain. a Anteroposterior (AP) pelvis radiograph reported as borderline right acetabular dysplasia and normal left hip. b AP pelvis status post right periacetabular osteotomy demonstrates increased lateral coverage, though the woman had reported worsening symptoms. c Sagittal proton-density fat-suppressed MR image of the right hip performed preoperatively (retrospectively) reveals an osteoid osteoma within the anterior acetabulum (arrow). The woman’s symptoms resolved after radiofrequency ablation
Conclusion
The term “borderline dysplasia” refers to patterns of acetabular coverage that might predispose children to instability. Some children with borderline radiographic measurements have normal joint mechanics and function (Fig. 1 Should say Figure 3), while others benefit from acetabular reorienting surgery (Fig. 2 Should say Figure 4) [11]. It is important that radiologists reflect this uncertainty in their reports with appropriate management recommendations. Instability might be suggested by radiographs, but ultimate diagnosis is confirmed on the basis of history and physical exam assessing for instability. These children should undergo high-resolution MR imaging of the hip to evaluate for joint damage, and CT might be helpful for better 3-D characterization of the bony shape and contour. Dynamic ultrasonography has been validated as a helpful adjunct in the determination of instability by measuring anterior femoral head translation with dynamic maneuvers replicating the apprehension test [54]. As pediatric radiologists, we are often the first to identify borderline or mild dysplasia on the basis of radiographs. It is imperative that we serve as effective consultants and offer appropriate recommendations as part of a cohesive multidisciplinary approach to this complex patient population.
References
Graf R (1984) Classification of hip joint dysplasia by means of sonography. Arch Orthop Trauma Surg 102:248–255
Graf R (1984) Fundamentals of sonographic diagnosis of infant hip dysplasia. J Pediatr Orthop 4:735–740
Gala L, Clohisy JC, Beaule PE (2016) Hip dysplasia in the young adult. J Bone Joint Surg Am 98:63–73
Millis MB, Kim YJ (2002) Rationale of osteotomy and related procedures for hip preservation: a review. Clin Orthop Relat Res 405:108–121
Wiberg G (1939) Studies on dysplastic acetabula and congenital subluxation of the hip joint. With special references to the complication of osteoarthritis. Acta Chir Scand 83:28–38
Lee CB, Mata-Fink A, Millis MB, Kim YJ (2013) Demographic differences in adolescent-diagnosed and adult-diagnosed acetabular dysplasia compared with infantile developmental dysplasia of the hip. J Pediatr Orthop 33:107–111
Delaunay D, Dussault RG, Kaplan PA, Alford BA (1997) Radiographic measurements of dysplastic adult hips. Skelet Radiol 26:75–81
Beltran LS, Rosenberg ZS, Mayo JD et al (2013) Imaging evaluation of developmental hip dysplasia in the young adult. AJR Am J Roentgenol 200:1077–1088
Wilkin GP, Ibrahim MM, Smit KM, Beaule PE (2017) A contemporary definition of hip dysplasia and structural instability: toward a comprehensive classification for acetabular dysplasia. J Arthroplast 32:S20–S27
Lequesne M (2002) The false profile view of the hip: role, interest, economic considerations. Joint Bone Spine 69:109–113
Putnam SM, Clohisy JC, Nepple JJ (2019) Do changes in pelvic rotation and tilt affect measurement of the anterior center edge angle on false profile radiographs? A cadaveric study. Clin Orthop Relat Res 477:1066–1072
Wyatt MC, Beck M (2018) The management of the painful borderline dysplastic hip. J Hip Preserv Surg 5:105–112
McClincy MP, Wylie JD, Kim YJ et al (2018) Periacetabular osteotomy improves pain and function in patients with lateral center-edge angle between 18° and 25°, but are these hips really borderline dysplastic? Clin Orthop Relat Res 477:1145–1153
McClincy MP, Wylie JD, Yen YM, Novais EN (2019) Mild or borderline hip dysplasia: are we characterizing hips with a lateral center-edge angle between 18 and 25 degrees appropriately? Am J Sports Med 47:112–122
McCarthy JC, Lee JA (2002) Acetabular dysplasia: a paradigm of arthroscopic examination of chondral injuries. Clin Orthop Rel Res 405:122–128
Murphy SB, Ganz R, Muller ME (1995) The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am 77:985–989
Kim YJ, Jaramillo D, Millis MB et al (2003) Assessment of early osteoarthritis in hip dysplasia with delayed gadolinium-enhanced magnetic resonance imaging of cartilage. J Bone Joint Surg Am 85:1987–1992
Omeroglu H, Biçmoglu A, Agus H, Tümer Y (2002) Measurement of center-edge angle in developmental dysplasia of the hip: a comparison of two methods in patients under 20 years of age. Skelet Radiol 31:25–29
Carlisle JC, Zebala LP, Shia DS et al (2011) Reliability of various observers in determining common radiographic parameters of adult hip structural anatomy. Iowa Orthop J 31:52–58
Clohisy JC, Carlisle JC, Trousdale R et al (2009) Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res 467:666–675
Bensler S, Dietrich TJ, Zubler V et al (2018) Pincer-type MRI morphology seen in over a third of asymptomatic healthy volunteers without femoroacetabular impingement. J Magn Reson Imaging 49:1296–1303
Nepple JJ, Martell JM, Kim YJ et al (2014) Interobserver and intraobserver reliability of the radiographic analysis of femoroacetabular impingement and dysplasia using computer-assisted measurements. Am J Sports Med 42:2393–2401
Tannast M, Mistry S, Steppacher SD et al (2008) Radiographic analysis of femoroacetabular impingement with Hip2Norm — reliable and validated. J Orthop Res 26:1199–1205
Jamali AA, Mladenov K, Meyer DC et al (2007) Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res 25:758–765
Zaltz I, Kelly BT, Hetsroni I, Bedi A (2013) The crossover sign overestimates acetabular retroversion. Clin Orthop Relat Res 471:2463–2470
Larson CM, Moreau-Gaudry A, Kelly BT et al (2015) Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res 473:1247–1254
Tannast M, Siebenrock KA, Anderson SE (2007) Femoroacetabular impingement: radiographic diagnosis — what the radiologist should know. AJR Am J Roentgenol 188:1540–1552
Nepple JJ, Lehmann CL, Ross JR et al (2013) Coxa profunda is not a useful radiographic parameter for diagnosing pincer-type femoroacetabular impingement. J Bone Joint Surg Am 95:417–423
Anderson LA, Kapron AL, Aoki SK, Peters CL (2012) Coxa profunda: is the deep acetabulum overcovered? Clin Orthop Relat Res 470:3375–3382
Diesel CV, Ribeiro TA, Coussirat C et al (2015) Coxa profunda in the diagnosis of pincer-type femoroacetabular impingement and its prevalence in asymptomatic subjects. Bone Joint J 97-B:478–483
Brian P, Bernard S, Flemming D (2010) Femoroacetabular impingement: screening and definitive imaging. Semin Roentgenol 45:228–237
Beaulé PE, Zaragoza E, Motamedi K et al (2005) Three-dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res 23:1286–1292
Hack K, DiPrimio G, Rakhra K, Beaulé PE (2010) Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am 92:2436–2444
Nötzli HP, Wyss TF, Stoecklin CH et al (2002) The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 84:556–560
Ahn T, Kim CH, Kim TH et al (2016) What is the prevalence of radiographic hip findings associated with femoroacetabular impingement in asymptomatic Asian volunteers. Clin Orthop Relat Res 474:2655–2661
Frank JM, Harris JD, Erickson BJ et al (2015) Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: a systematic review. Arthroscopy 31:1199–1204
Omoumi P, Thiery C, Michoux N et al (2014) Anatomic features associated with femoroacetabular impingement are equally common in hips of old and young asymptomatic individuals without CT signs of osteoarthritis. AJR Am J Roentgenol 202:1078–1086
Bixby SD, Kienle KP, Nasreddine A et al (2013) Reference values for proximal femoral anatomy in adolescents based on sex, physis, and imaging plane. Am J Sports Med 41:2074–2082
Laborie LB, Lehmann TG, Engesaeter IO et al (2013) Is a positive femoroacetabular impingement test a common finding in healthy young adults? Clin Orthop Relat Res 471:2267–2277
Clohisy JC, Carlisle JC, Beaule PE et al (2008) A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am 90:47–66
Nepple JJ, Wells J, Ross JR et al (2017) Three patterns of acetabular deficiency are common in young adult patients with acetabular dysplasia. Clin Orthop Relat Res 475:1037–1044
Wyatt M, Weidner J, Pfluger D, Beck M (2017) The femoro-acetabular roof (FEAR) index: a new measurement associated with instability in borderline hip dysplasia. Clin Orthop Relat Res 475:861–869
Wong TY, Jesse MK, Jensen A et al (2018) Upsloping lateral sourcil: a radiographic finding of hip instability. J Hip Preserv Surg 5:435–442
Fredensdorg N (1976) The CE angle of normal hips. Acta Orthop Scand 47:403–405
Armbruster TG, Guerra J Jr, Resnick D et al (1978) The adult hip: an anatomic study. Part I: the bony landmarks. Radiology 128:1–10
Werner CM, Ramseler LE, Ruckstuhl T et al (2012) Normal values of Wiberg’s lateral center-edge angle and Lequesne’s acetabular index — a coxometric update. Skelet Radiol 41:1273–1278
Fischer CS, Kühn JP, Ittermann T et al (2018) What are the reference values and associated factors for center edge angle and alpha angle? A population-based study. Clin Orthop Relat Res 476:2249–2259
Siebenrock KA, Kistler L, Schwab JM et al (2012) The acetabular wall index for assessing anteroposterior femoral head coverage in symptomatic patients. Clin Orthop Relat Res 470:3355–3360
Anderson LA, Anderson MB, Erickson JA et al (2017) Acetabular wall indices help to distinguish acetabular coverage in asymptomatic adults with varying morphologies. Clin Orthop Relat Res 475:1027–1033
Garabekyan T, Ashwell Z, Chadayammuri V et al (2016) Lateral acetabular coverage predicts the size of the hip labrum. Am J Sports Med 44:1582–1589
Kraeutler MJ, Goodrich JA, Ashwell ZR et al (2019) Combined lateral osteolabral coverage is normal in hips with acetabular dysplasia. Arthroscopy 35:800–806
Babst D, Steppacher SD, Ganz R et al (2011) The iliocapsularis muscle: an important stabilizer in the dysplastic hip. Clin Orthop Relat Res 469:1728–1734
Kraeutler MJ, Garabekyan T, Pascual-Garrido C, Mei-Dan O (2016) Hip instability: a review of hip dysplasia and other contributing factors. Muscles Ligaments Tendons J 6:343–353
d’Hemecourt PA, Sugimoto D, McKee-Proctor M et al (2018) Can dynamic ultrasonography of the hip reliably assess anterior femoral head translation? Clin Orthop Relat Res 477:1086–1098
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bixby, S.D., Millis, M.B. The borderline dysplastic hip: when and how is it abnormal?. Pediatr Radiol 49, 1669–1677 (2019). https://doi.org/10.1007/s00247-019-04468-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-019-04468-4