Abstract
Background
Understanding acetabular pathomorphology is necessary to correctly treat patients with hip complaints. Existing radiographic parameters classify acetabular coverage as deficient, normal, or excessive but fail to quantify contributions of anterior and posterior wall coverage. A simple, reproducible, and valid measurement of anterior and posterior wall coverage in patients with hip pain would be a clinically useful tool.
Questions/Purposes
We (1) introduce the anterior wall index (AWI) and posterior wall index (PWI), (2) report the intra- and interobserver reliability of these measurements, and (3) validate these measurements against an established computer model.
Methods
We retrospectively reviewed 87 hips (63 patients) with symptomatic hip disease. A validated computer model was used to determine total anterior and posterior acetabular coverage (TAC and TPC) on an AP pelvis radiograph. Two independent observers measured the AWI and PWI on each film, and the intraclass correlation coefficient (ICC) was calculated. Pearson correlation was used to determine the strength of linear dependence between our measurements and the computer model.
Results
Intra- and interobserver ICCs were 0.94 and 0.99 for the AWI and 0.81 and 0.97 for the PWI. For validation against the computer model, Pearson r values were 0.837 (AWI versus TAC) and 0.895 (PWI versus TPC). Mean AWI and PWI were 0.28 and 0.81 for dysplastic hips, 0.41 and 0.91 for normal hips, 0.61 and 1.15 for hips with a deep acetabulum.
Conclusions
Our data suggest these measures will be helpful in evaluating anterior and posterior coverage before and after surgery but need to be evaluated in asymptomatic individuals without hip abnormalities to establish normal ranges.
Level of Evidence
Level III, diagnostic study. See Instructions for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recent research has led to the recognition of acetabular overcoverage as the pathomechanism of pincer-type impingement of the hip [5]. Anterior segmental head overcoverage is thought to be a pathomechanical cause for pincer-type impingement in hips with acetabular retroversion [5, 14, 22]. Acetabular retroversion can be identified by two radiographic signs, the crossover sign of the acetabular rims and the posterior wall sign [14, 23]. The crossover sign describes only the relative relationship between the anterior and posterior walls and does not answer the question of whether the anterior or posterior walls provide excessive, normal, or deficient coverage. A positive posterior wall sign suggests deficient coverage but does not provide a quantitative value or range for values for deficient, normal, or excessive coverage [14].
Analysis of acetabular pathomorphology is necessary to appropriately treat patients with complaints related to the hip. There is increasing concern that failure to recognize abnormalities of acetabular morphology leads to inadequate or inappropriate treatment of hip disease [7, 11–14, 16]. Consequently, the question arises whether normal coverage of the femoral head can be defined on an AP pelvis radiograph. The lateral center-edge (LCE) angle is widely accepted to define the amount of lateral coverage of the femoral head [22, 24]. However, simple parameters for quantifying anterior and posterior head coverage on an AP pelvis radiograph have not been developed. Tannast et al. [20] recently reported a computerized measurement method on AP pelvis radiographs and subsequently reported [19] differences in the amount of anterior and posterior coverage between normal-appearing acetabula, dysplastic acetabula, and hips with a deep socket. The question arose whether a simple radiographic parameter on an AP pelvis radiograph could identify the same differences in anterior and posterior coverage. We therefore developed simple radiographic parameters to quantify anterior and posterior coverage: the anterior wall index (AWI) and the posterior wall index (PWI). These parameters measure the length of the covered head portion along the head-neck axis and divide this measurement by the radius of the femoral head.
Our purposes in this study are to (1) introduce these new measurements, (2) provide analysis of the intra- and interobserver reliability of these measurements, and (3) validate these measurements against an established computer analysis model.
Patients and Methods
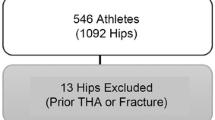
We retrospectively reviewed 109 patients (155 hips) treated surgically for various hip disorders between January 2003 and December 2003 to measure the parameters. We excluded 46 patients (68 hips) from evaluation if they had undergone previous surgical intervention, were treated for fracture or severe proximal femoral deformity (eg, Legg-Calvé-Perthes, proximal femoral focal deficiency), if no appropriate preoperative radiograph was available, or if the hip exhibited Grade 2 or higher osteoarthritis according to the Tönnis classification [22]. This left us with 63 patients (87 hips) included in the analysis (Table 1). A standardized radiographic technique was performed for all reviewed AP pelvis radiographs. A film focus distance of 1.2 m was used with the beam centered between the pubic symphysis and a line connecting the anterior superior iliac spine with the pelvis in neutral rotation [14]. The longitudinal rotation of the pelvis was verified as correct when the tip of the coccyx was in line with pubic symphysis. Any rotation of the tip of the coccyx from the symphyseal line by more than 1 cm was considered unacceptable for measurement purposes. Images were not specifically corrected for tilt.
Acetabula were stratified into one of the three morphologic groups based on preoperative AP pelvis radiographs: (1) dysplastic, (2) normal, and (3) deep. A dysplastic acetabulum was defined as an LCE angle of less than 20°. A deep acetabulum was defined as meeting one of the following criteria: (1) an LCE angle of greater than 39° [23] or (2) projection of the acetabular fossa or medial femoral head medial to the ilioischial line. Each acetabulum was also evaluated at the time of surgical intervention and intraoperative findings were used to correlate with preoperative diagnosis. Preoperative radiographs were analyzed for total anterior acetabular coverage (TAC) and total posterior acetabular coverage (TPC) with Hip2Norm (University of Bern, Bern, Switzerland), a validated computer program for measuring acetabular morphology [20]. The Hip2Norm computer analysis model validation included an external comparison (comparison with CT scan data) and internal comparison (analysis of multiple radiographs on the same cadaver pelvis with tilt and rotation systematically altered), as well as analysis of inter- and intraobserver reliability [20, 21, 25]. Hip2Norm has the ability to correct radiographs for tilt and rotation; however, we did not use this function for this study.
Two individuals performed the wall index measurements, an orthopaedic surgeon experienced in viewing and interpreting AP pelvis radiographs (JMS) and a medical student with no prior experience interpreting AP pelvis radiographs (LK). Both observers were trained in the method on a single radiograph before recording their measurements. Each observer performed two measurements on each radiograph, with an interval of at least 5 days between the first and second readings.
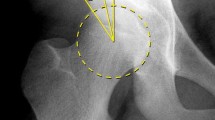
The measurement was performed for each hip as follows (Fig. 1). A circle was placed over the femoral head that best approximated the femoral head shape and center of rotation. In cases of proximal femoral morphologic abnormality, the major diameter of the head was used to fit the circle. The radius of the circle was then determined. A line was drawn down the axis of the neck, intersecting the circle through its center. The distance along this line between the medial intersection of the circle and the intersection of the anterior wall (a) was recorded. Then, the distance between the medial intersection of the circle and the intersection of the posterior wall (p) was recorded. If either wall fell medial to the circle (as in the case of a severely dysplastic hip), a negative value was assigned to the a or p distance. The AWI and PWI were then calculated by dividing the a and p lines, respectively, by the radius of the circle. Sample AWI measurements are shown for a dysplastic hip (Fig. 2A), normal hip (Fig. 2B), and a hip with a deep acetabulum (Fig. 2C).
(A) This is an example of the AWI calculated in a normal hip. The calculated AWI is 1.1 cm/2.7 cm = 0.41. (B) This is an example of the AWI calculated in a dysplastic hip. The calculated AWI is 0.8 cm/2.4 cm = 0.33. (C) This is an example of the AWI calculated in a hip with a deep acetabulum. The calculated AWI is 2.7 cm/2.9 cm = 0.93.
We used the intraclass correlation coefficient (ICC) [10] to calculate level of agreement among two or more continuous variables. We then evaluated our AWI and PWI measurements to determine association with the TAC and TPC measurements specified by Hip2Norm. Standard linear regression analysis was used to determine whether a linear relationship existed between those measurement sets, and the Pearson correlation coefficient was used to determine the strength of that linear relationship. Normal distribution was determined with the Kolmogorov-Smirnov test. Homoscedasticity was determined with the Fligner-Killeen test of homogeneity of variances. All statistical analyses were performed using R Version 2.14.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
The mean intraobserver ICC was 0.94 (95% CI, 0.91–0.97) for the AWI and 0.81 (95% CI, 0.72–0.87) for the PWI (Table 2). The mean interobserver ICC was 0.99 (95% CI, 0.98–0.99) for the AWI and 0.97 (95% CI, 0.95–0.98) for the PWI.
The mean AWI and PWI were 0.28 and 0.81, respectively, for dysplastic hips; 0.41 and 0.91, respectively, for normal hips; 0.61 and 1.15, respectively, for hips with a deep acetabulum (Table 3). The quantification of the linear relationship between our measurements and the Hip2Norm values (Table 3) showed an r of 0.837 (p < 0.001) for the AWI versus TAC (Fig. 3A) and an r of 0.895 (p < 0.001) for the PWI versus TPC (Fig. 3B).
Discussion
Quantification of anterior and posterior acetabular coverage is necessary for appropriate treatment of both dysplastic hips and hips exhibiting impingement due to acetabular overcoverage. We therefore developed two new measurements to quantify anterior and posterior acetabular coverage using a single AP pelvis radiograph: the AWI and the PWI. Our purposes were to (1) introduce these measurements, (2) provide analysis of the intra- and interobserver reliability of these measurements, and (3) validate these measurements against an established computer analysis model.
The study has several limitations. First, these indexes have not been evaluated or validated in asymptomatic individuals. Therefore, we can only say that these findings apply to patients with symptomatic hip disease and currently cannot be used to identify normal from abnormal acetabular coverage in asymptomatic patients. Further validation of these measurements in asymptomatic patients would help expand their use in determining normal from abnormal hips. Second, rotational malalignment of the pelvis during acquisition of the radiographs will have an influence on the amount of anterior and posterior wall coverage [21]. This may give rise to measurement errors. However, our radiographs were taken with a standardized technique that is reproducible and minimizes malalignment [15]. Furthermore, we did not use Hip2Norm to correct for rotation or tilt, as most clinicians do not have software available to perform this function; therefore, manual measurements and computer modeling were performed at the same pelvic orientation. This allowed for the greatest consistency in measurements between the two techniques. Third, measurement of head coverage at one single point along the head-neck axis ignores the curved variations in the shapes of the anterior rim to a certain degree [8]. Even though our measurement was taken only at a single point along the rim, in our patient cohort, it showed high correlation with the area-based measurement obtained from Hip2Norm. Fourth, our cohort of normal-appearing acetabula contained a considerably higher percentage of males (78.9%) than either the dysplastic (20.6%) or deep (8.8%) acetabulum cohorts (Table 1). All patients in our study were being treated for symptomatic hip pain, and this distribution reflects the higher prevalence of purely femoral-sided pathology in males and, conversely, the higher prevalence of acetabular pathomorphology in females [1, 18]. Finally, these indexes are not suitable for markedly aspherical femoral heads such as occur in Legg-Calvé-Perthes disease. Difficulty in determining a radius of curvature of grossly deformed heads will affect the AWI and PWI even though no acetabular pathomorphology may be present.
The AWI and PWI correlated with previously performed anterior and posterior wall coverage measurements based on a computer model analysis of AP pelvis radiographs [20]. Average values and ranges for the AWIs have been provided for normal acetabula, which will help to distinguish between insufficient and excessive coverage (Table 3, Fig. 2). The intra- and interobserver reliabilities for both indexes indicate these measurements are highly reproducible.
When comparing the performance of our new measurements with the data collected from our computer model, Pearson’s r values of 0.837 for the AWI and 0.895 for the PWI indicate strong correlation with the area-based values obtained from Hip2Norm. These correlations suggest the AWI and PWI are acceptable alternatives to computer modeling when determining anterior and posterior acetabular wall coverage.
Anterior and posterior head coverage can be quantified with the aid of CT scans, computer model analysis, and plastic templates on AP pelvis radiographs [2, 3, 6, 8]. Typically, the craniocaudal projection of the head coverage is used to calculate the coverage of the anterior and posterior hemispheres. Although these measurements seem to provide accurate data on coverage, these techniques have the disadvantage that they require a CT scan or specialized computer software [2, 4, 9]. In addition, they cannot be used for intraoperative assessment. A more simple method for measuring the contact area with a template has been proposed by Hefti [6], who primarily designed the method to analyze the contact surfaces and the resulting transmitted forces. However, Hefti’s calculations of anterior and posterior head coverage in individual examples with normal morphology of hips are consistent with the findings of the computerized analysis (Hip2Norm) by Tannast et al. [19]. They found, in normal acetabula, the anterior wall and posterior wall cover 15% to 26% and 27% to 32% of the head sphere, respectively. Systematic analysis in normal, dysplastic, and deep acetabula showed a normal distribution of values with a difference of anterior and posterior wall coverage among all three groups [19]. The decreased anterior and posterior head coverage in dysplastic hips was confirmed independently with the same computerized method in a different patient group before undergoing periacetabular reorientation for development hip dysplasia [17].
Our findings also raise questions about the utility of the posterior wall sign as described by Reynolds et al. [14]. From our data, it would appear, in hips with normal acetabular morphology, the line of the posterior wall would be very slightly medial to the true center of the femoral head. Since the normal PWI encompasses a range from medial to the center of the femoral head to just lateral to it, we would caution the reader not to use the posterior wall sign alone to make determinations on acetabular morphology.
In summary, normal, excessive, and deficient anterior and posterior wall coverage can be identified on a plain AP pelvis radiograph with the simple parameters (AWI, PWI) we describe. Furthermore, our parameters are highly reproducible and strongly correlate with area-based measurements from a validated computer analysis model. We believe these two indexes should be included in future radiographic analysis of the hip, especially in patients amenable to hip-preserving surgeries, as it is our experience that too much surgical trimming of the anterior rim in femoroacetabular impingement may lead to rapid progression of osteoarthritis. We acknowledge these measurements have only been validated in patients with symptomatic hip disease, and further validation in asymptomatic patients would be required to broaden their use. These measurements should help to identify adequate anterior and posterior coverage to achieve the optimal balance after surgical intervention.
References
Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018.
Chosa E, Tajima N, Nagatsuru Y. Evaluation of acetabular coverage of the femoral head with anteroposterior and false profile radiographs of hip joint. J Orthop Sci. 1997;2:378–390.
Dutoit M, Zambelli PY. Simplified 3D-evaluation of periacetabular osteotomy. Acta Orthop Belg. 1999;65:288–294.
Ecker TM, Tannast M, Puls M, Siebenrock KA, Murphy SB. Pathomorphologic alterations predict presence or absence of hip osteoarthrosis. Clin Orthop Relat Res. 2007;465:46–52.
Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:263–269.
Hefti F. Spherical assessment of the hip on standard AP radiographs: a simple method for the measurement of the contact area between acetabulum and femoral head and of acetabular orientation. J Pediatr Orthop. 1995;15:797–805.
Köhnlein W, Ganz R, Impellizzeri FM, Leunig M. Acetabular morphology: implications for joint-preserving surgery. Clin Orthop Relat Res. 2009;467:682–691.
Konishi N, Mieno T. Determination of acetabular coverage of the femoral head with use of a single anteroposterior radiograph: a new computerized technique. J Bone Joint Surg Am. 1993;75:1318–1333.
Kubiak-Langer M, Tannast M, Murphy SB, Siebenrock KA, Langlotz F. Range of motion in anterior femoroacetabular impingement. Clin Orthop Relat Res. 2007;458:117–124.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174.
Mast JW, Brunner RL, Zebrack J. Recognizing acetabular version in the radiographic presentation of hip dysplasia. Clin Orthop Relat Res. 2004;418:48–53.
Perreira AC, Hunter JC, Laird T, Jamali AA. Multilevel measurement of acetabular version using 3-D CT-generated models: implications for hip preservation surgery. Clin Orthop Relat Res. 2011;469:552–561.
Peters CL, Anderson LA, Erickson JA, Anderson AE, Weiss JA. An algorithmic approach to surgical decision making in acetabular retroversion. Orthopedics. 2011;34:10.
Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288.
Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248.
Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion: treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286.
Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644.
Stulberg S. Acetabular dysplasia: development of osteoarthritis of the hip. In: Harris W, ed. The Hip: Proceedings of the Second Open Scientific Session of the Hip Society. St Louis, MO: CV Mosby; 1974:82–93.
Tannast M, Albers CE, Steppacher SD, Siebenrock KA. Hip pain in the young adult. In: Bentley G, ed. European Instructional Lectures. Berlin, Germany: Springer-Verlag; 2011:141–154.
Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G. Radiographic analysis of femoroacetabular impingement with Hip2Norm—reliable and validated. J Orthop Res. 2008;26:1199–1205.
Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190.
Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin, Germany: Springer-Verlag; 1987.
Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770.
Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand. 1939;83(suppl 58):7–38.
Zheng G, Tannast M, Anderegg C, Siebenrock KA, Langlotz F. Hip2Norm: an object-oriented cross-platform program for 3D analysis of hip joint morphology using 2D pelvic radiographs. Comput Methods Programs Biomed. 2007;87:36–45.
Author information
Authors and Affiliations
Corresponding author
Additional information
One of the authors (JMS) certifies that he, or a member of his immediate family, has received or may receive, during the study period, fellowship funding from the Maurice E. Müller Foundation of North America. Each author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Siebenrock, K.A., Kistler, L., Schwab, J.M. et al. The Acetabular Wall Index for Assessing Anteroposterior Femoral Head Coverage in Symptomatic Patients. Clin Orthop Relat Res 470, 3355–3360 (2012). https://doi.org/10.1007/s11999-012-2477-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2477-2