Abstract
Background
Patellofemoral instability is one of the most common causes of cartilage damage in teenagers.
Objective
To quantitatively evaluate the patellar cartilage in patients with patellofemoral instability using T2 relaxation time maps (T2 maps), compare the values to those in patients without patellofemoral instability and correlate them with morphological grades in patients with patellofemoral instability.
Materials and methods
Fifty-three patients with patellofemoral instability (mean age: 15.9 ± 2.4 years) and 53 age- and gender-matched patients without patellofemoral instability were included. Knee MR with axial T2 map was performed. Mean T2 relaxation times were obtained at the medial, central and lateral zones of the patellar cartilage and compared between the two groups. In the patellofemoral instability group, morphological grading of the patellar cartilage (0-4) was performed and correlated with T2 relaxation times.
Results
Mean T2 relaxation times were significantly longer in the group with patellofemoral instability as compared to those of the control group across the patellar cartilage (Student’s t-test, P<0.05) with the longest time at the central area. Positive correlation was seen between mean T2 relaxation time and morphological grading (Pearson correlation coefficiency, P<0.001). T2 increased with severity of morphological grading from 0 to 3 (mixed model, P<0.001), but no statistical difference was seen between grades 3 and 4.
Conclusion
In patellofemoral instability, patellar cartilage damage occurs across the entire cartilage with the highest T2 values at the apex. T2 relaxation times directly reflect the severity in low-grade cartilage damage, which implies an important role for T2 maps in differentiating between normal and low-grade cartilage damage.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Patellofemoral instability encompasses a wide spectrum of diseases, from mild patellofemoral maltracking/malalignment issues to complete dislocation of the patella impacting the lateral femoral condyle. Patellofemoral instability is a leading cause of cartilage damage in the pediatric population, particularly in physically active children [1]. Most patients are affected during the second decade of life and half of them suffer from recurrent dislocation and/or subsequent instability of the patellofemoral joint [2].
Plain radiographs are the first imaging exam in patients with clinical suspicion of patellofemoral instability or with nonspecific anterior knee pain; however, they are not diagnostic in general [3] and, ultimately, MR imaging is pursued in most cases. MR findings of patellofemoral instability are very characteristic; MR findings of acute patellar dislocation include cartilage damage of the medial facet of the patella, bone marrow edema of the lateral femoral condyle and medial stabilizer injuries [3–9]. Patellofemoral maltracking, besides acute dislocation, refers to the dynamic abnormality of patellofemoral joint. Patellofemoral maltracking is evaluated with static as well as with kinematic techniques [10]. Variable degrees of patellar cartilage damage occur in patellofemoral instability and the medial facet of the patella is known to be the most vulnerable spot in patellofemoral instability [3–9]. Conventional MR imaging has played a pivotal role in diagnosis and morphological grading of cartilage damage [10]. However, morphological grading as roughly estimated on conventional MR imaging tends to be subjective; furthermore, diagnostic accuracy is significantly limited, especially for low-grade cartilage damage [11].
Quantitative MR using T2 relaxation time mapping (T2 map) is a biochemical imaging technique that enables investigation of the microstructural changes of the cartilage [12–15]. The T2 map is highly sensitive to the orientation of the collagen fibers and to water content within the cartilage. For the diagnosis of early cartilage degeneration, the superiority of T2 maps to conventional MR has been proven in adults with osteoarthritis [16, 17]. However, the role of T2 maps in cartilage imaging in children is still uncertain. In contrast to senescent changes of the cartilage in adults with osteoarthritis where T2 relaxation times significantly increase with age, growing children have a significant decrease in T2 relaxation times during skeletal maturation [18].
Our study aims to validate the role of T2 maps in imaging patellar cartilage in children, in whom concurrent developmental and pathological changes coexist. The purpose of this study is to evaluate the patellar cartilage in patients with patellofemoral instability using T2 maps and to compare their T2 maps with T2 maps of age- and gender-matched subjects without patellofemoral instability. Furthermore, T2 relaxation times in the patellofemoral instability group will be correlated with morphological grading of the cartilage damage obtained from conventional MR.
Materials and methods
This study was approved by the institutional review board (IRB) and was Health Insurance Portability and Accountability Act (HIPAA) compliant. T2 relaxation time was performed as part of routine knee MR imaging, which is approved by the Food and Drug Administration and one of the widely accepted quantitative cartilage imaging techniques. The requirement for informed consent was waived for this retrospective study.
Subjects
Using the Picture Archiving and Communication System (Merge PACS; Merge Healthcare, Chicago, IL), we retrospectively reviewed 1,224 consecutive knee MRI exams, which were performed because of clinical request at our institution (Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA) during a 14-month period from January 2011 to March 2012. The MR images and reports were reviewed by H.K.K. (musculoskeletal radiology and pediatric radiology fellowship training with 12 years’ experience in MR imaging). Study subjects were then chosen to comprise a group with patellofemoral instability and a group without patellofemoral instability. Inclusion criteria for both groups were: 1) imaging performed at our institution using 1.5-T imager (HDxt; GE Medical Systems, Milwaukee, WI), and 2) MR exams included at least an axial fast spin echo T2-weighted sequence with fat suppression and axial T2 maps.
Additional inclusion criteria for the patellofemoral instability group included: 1) age range from 5 to 22 years, and 2) either a history of lateral patellar dislocation, subluxation or general patellar instability in one or both knees, or persistent anterior knee pain with clinical findings supporting patellofemoral instability, such as increased Q angle and positive apprehension patellar tilt tests [19, 20]. The subjects, who had patellofemoral instability associated with a developmental condition or syndrome, such as Down syndrome, cerebral palsy or Ehlers-Danlos syndrome, were excluded. A total of 53 patients with patellofemoral instability were included: 15 male, 38 female, mean age: 15.9 years (range: 8 to 21 years, standard deviation: 2.4 years).
Additional inclusion criteria for the group without patellofemoral instability included: 1) no known previous history of anterior knee pain, patellar dislocation, subluxation or malalignment; 2) no MRI findings of patellar cartilage abnormality, bone marrow edema of the patella, or ligament injury possibly affecting the patellar cartilage, such as complete anterior cruciate ligament tear; 3) no abnormalities involving or extending to the patella, such as neoplasm, inflammation, infection or fracture, and 4) no conditions affecting the congruency of the patellofemoral joint, such as congenital structural anomalies, developmental delay, non-weight bearing condition or underlying diagnosis of any kind of syndrome. Two hundred sixty-eight subjects met the criteria for the control group. For the matched pair design, 53 age- and gender-matched subjects were randomly chosen from among the 268 subjects. The matched pair design based on age and gender was performed because the T2 relaxation times of the patellar cartilage are age and gender dependent in growing children [18].
MR imaging and interpretation
MR imaging, which included conventional MR and T2 maps, was performed using the same protocol across all subjects in the groups with and without patellofemoral instability. Interpretation of MR imaging was performed by the two reviewers (C.H.K., with musculoskeletal radiology fellowship training with 18 years of experience in MR, and C.A., with pediatric radiology fellowship training with 15 years of experience in MR) consistently. Time interval between the recognition of the symptom and MR imaging was variable: Most cases of acute patellar dislocation underwent MR imaging within 2 weeks. However, the cases of recurrent dislocation or malalignment issues had a wide range of duration between the first symptomatic presentation and imaging performance. All the patients in the group with patellofemoral instability had less than 5 years of history of pain of the patellofemoral joint.
The standard knee MRI protocol at our institution included fast spin echo (FSE) proton-density-weighted sagittal image (repetition time [TR]/echo time [TE] 1,700-2,000/11-12 ms, field of view [FOV] 14-16 cm, matrix 320 × 224, slice thickness 3 mm, slice gap 1 mm, echo train length [ETL] 8, number of excitations [NEX] 2) , fat-saturated FSE T2-weighted axial, sagittal and coronal images (TR/TE 3,000/60 ms, FOV 14-16 cm, matrix 256 × 192, slice thickness 3-4 mm, slice gap 1 mm, ETL 8, NEX 2), coronal T1-weighted image (TR/TE 350/10-15 ms, FOV 16 cm, matrix 256 × 192, slice thickness 3 mm, slice gap 1 mm, ETL 6, NEX 1), and optional 3-D gradient echo sequences (TR/TE 50/6-7 ms, flip 60, FOV 13-16 cm, matrix 256 × 128, slice thickness 2 mm, 45 slices, NEX 1, imaging time 3 min 35 s).
Morphological grading of patellar cartilage damage was assessed in the group with patellofemoral instability on axial T2 fat suppression images and/or 3-D gradient echo sequences. Three-dimensional gradient echo sequences were performed in 42 subjects out of 53 in the group of patellofemoral instability. MR images were evaluated by two radiologists (C.H.K. and C.A.) with consensus. On conventional MR images, the patellar cartilage lesions were classified into four grades according to the signal intensity, surface description and diameter (Fig. 1): 0, normal; 1, intracartilaginous high T2 signal; 2, superficial fissuring and cracks or partial-thickness defect extending down to <50% of the cartilage depth; 3, fissuring to the level of calcified layer or a large defect extending down to >50% of the cartilage depth (down to calcified layer but not through the subchondral plate); and 4, full-thickness defect penetrating subchondral bone. The patellar cartilage in the patients in the group without patellofemoral instability was considered grade 0, which was assessed at the time of inclusion in the control group.
Axial fat-saturated T2-weighted images (left) and T2 maps (right) for morphological grades of the cartilage lesions. Grade 1, a 20-year-old woman: Focal intracartilaginous high signal (arrowhead) in the lateral patellar facet (C2 to L2) is evident on the T2-weighted images, which correlates well with the color-coded map. Grade 2, a 12-year-old girl: A superficial patellar cartilage crack (arrowhead) in the central zone is observed on T2-weighted images. In addition, there is diffuse intracartilaginous change on both T2-weighted images and T2 maps. Grade 3, an 18-year-old girl: A minimally displaced cartilage fragment (arrows) involving more than 50% of the cartilage thickness is visible in the apex on the T2-weighted images, and the surrounding color change is well appreciated on the T2 map. Note that the color-coded map does not demonstrate the full extent of the cartilage abnormality in this case of grade 3 damage, compared with the above grade 2 lesion. Grade 4, a 17-year-old girl: Noncontiguous full-thickness defects (arrows) are visualized on the T2-weighted images. Patellar bone marrow and surrounding soft-tissue edema and medial patellofemoral ligament rupture as well as cartilage defect are seen in the M1 location, which would be the most common result of acute patellar dislocation
An axial T2 map of the patellar cartilage was performed with the following MR imaging parameters: TR=1,500 ms, TE=9,18, 27, 36, 45, 54, 63, 72, 81, 90 and 99 ms, number of echoes=11, matrix: 256 × 160, slice thickness: 3-4 mm, slice gap: 1 mm, FOV: 14 cm. Each exam had 8-26 slices. The acquisition time of the T2 mapping series was about 5 min. Our institutional imaging process software (Interactive Data Language; ISS, Boulder, CO) was used to generate gray-scale T2 maps and color-coded images. The pixel-by-pixel based analysis of the cartilage was performed using a linear least square curve fitting algorithm [18].
The mean T2 relaxation time was automatically calculated by placing a region of interest (ROI). The patellar cartilage was manually segmented by S.S. (medical graduate student with 1 year of experience in MR research) under the supervision of H.K.K. with 6 years of experience in T2 maps. The first and last images were excluded to eliminate the volume average effect. Mean T2 values of the patellar cartilage were calculated from the remaining slices of the patella and were obtained in a consistent manner in the groups with and without patellofemoral instability. The patellar cartilage was traced to include the entire cartilage, including the circumferential physis, the unossified cartilage and the articular cartilage in the group in which the physis is open; in the group with the physis closed or closing, only articular cartilage was included for analysis. This method was described and utilized in our previous publications [18, 21].
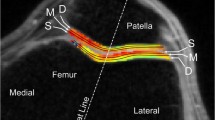
Morphological grading of cartilage damage and mean T2 relaxation times were obtained at the same locations of the patellar cartilage (Fig. 1). A total of six locations in three zones (lateral, central and medial) were evaluated in each subject (Fig. 2): M1, medial one-third of the medial facet; M2, middle one-third of the medial facet; C1, lateral one-third of the medial facet; C2, medial one-third of the lateral facet; L2, middle one-third of the lateral facet; and L1, lateral one-third of the lateral facet. To minimize memory bias, the morphological grading of the cartilage damage (C.H.K., C.A.) and mean T2 relaxation times were evaluated by different reviewers (H.K.K., S.S.) independently who were blinded to T2 relaxation time measurements and morphological grading.
T2 relaxation time mapping in a 17-year-old girl. On the gray-scale map (a) and color-coded map (b), the patellar cartilage was divided into three zones (medial, central and lateral) and six locations: M1, medial one-third of the medial facet; M2, middle one-third of the medial facet; C1, lateral one-third of the medial facet; C2, medial one-third of the lateral facet; L2, middle one-third of the lateral facet; and L1, lateral one-third of the lateral facet
Statistical analysis
Student’s t-test was used to compare mean T2 relaxation times of the patellar cartilage between the two groups. In addition, the Wilcoxon rank-sum test was used to see if there were any substantive differences. The two methods were in good agreement in every case so that only the Student’s t-test results are reported. In the group with patellofemoral instability, morphological grading was correlated with mean T2 relaxation times from the corresponding locations using the Pearson correlation coefficient. In addition, the Spearman rank correlation was also derived. The two correlations were in good agreement in every case so that only the Pearson results are reported. Lastly, a linear mixed model was examined where the response was the T2 relaxation time and the fixed effects were the morphological grade and the location. The random effects were subject ID and the subject by region interaction. The adjusted mean T2 relaxation times, the least squares means, were compared for each pair of adjacent morphological grades of cartilage damage, i.e. 0 vs. 1, 1 vs. 2, etc. These differences were considered statistically significant (different from zero) if the adjusted P-values were less than 0.05. The adjustment used was based on the false discovery rate in order to account for the multiple comparisons [22].
All statistical analyses were performed with SAS® version 9.3 software packages (SAS Institute, Cary, NC).
Results
Morphological grading was performed at all six locations in all subjects in the patellofemoral instability group. Mean T2 relaxation times were not measurable at M1 and M2 in one subject in the patellofemoral instability group who had high-grade cartilage damage at the medial facet. The mean T2 relaxation times from all 6 locations were obtained in the other 52 subjects in the patellofemoral instability group. Therefore, 318 morphological grades and 316 numeric values of the mean T2 relaxation times were obtained in the group with patellofemoral instability. The morphological grades were: 150 normal (47.1%, 150/318), 112 grade 1 (35.2%, 112/318), 26 grade 2 (8.1%, 26/318), 14 grade 3 (4.4%, 14/318) and 16 grade 4 (5.0%, 16/318). Of the 53 patellofemoral instability knees, 52 (98.1%) had articular cartilage lesions of the patella in at least one location on the basis of the morphological grading, and only 1 knee had no cartilage abnormality, i.e. grade 0 in all 6 locations, and 20 had the highest grade of 1, 13 had the highest grade of 2, 8 had the highest grade of 3 and 11 had the highest grade of 4. The grade 4 of cartilage damage most commonly occurred at the far medial facet (M1) of the patella, which was seen in 7 patients with patellofemoral instability.
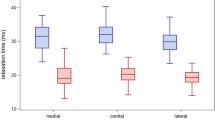
In the patellofemoral instability group, the mean T2 relaxation time was 37.7 ms, whereas the mean T2 relaxation time in the group without patellofemoral instability was 30.0 ms, which was significantly lower (P<0.001). The mean T2 relaxation time in the patellofemoral instability group was significantly longer than that of the group without patellofemoral instability across all locations of the patellar cartilage including the medial, central and lateral facets (P<0.001). Among the 6 locations, the largest difference between the two groups was seen at C1 (lateral one-third of the medial facet, 8.9 ms difference) and C2 (medial one-third of the lateral facet, 8.6 ms difference). The longest mean T2 relaxation times were seen at C1 (39.6 ms) followed by C2 (39.5 ms).
For the patellofemoral instability group, the distribution of morphological grading and mean T2 relaxation times at the six locations are summarized in Tables 1 and 2.
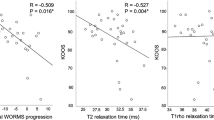
Statistically significant positive correlation was seen between overall mean T2 relaxation times and morphological grading in each location (P<0.001, r=0.58).
Lastly, a linear mixed model was examined where the response was T2 relaxation time and the fixed effects were morphological grade, region and location nested within region. The random effects were subject and subject-by-region interaction. The least squares means are estimates of the means that are adjusted for the other variables in the mixed model. These were derived for each morphological grade. The least squares means T2 relaxation times for cartilages classified as grades 0, 1, 2, 3 and 4 were 33.7 ± 0.7 ms, 38.0 ± 0.8 ms, 41.9 ± 1.4 ms, 46.7 ± 1.7 ms, and 50.7 ± 1.7 ms, respectively (Fig. 3). There was a statistically significant difference between the least squares means T2 relaxation time and each morphological grade from grades 0 to 3 even after adjusting for multiple testing using a false discovery rate and an alpha level equal to 0.05. Specifically, the false discovery rate-adjusted P-values between morphological grades 0 vs. 1, 1 vs. 2 and 2 vs. 3 were 0.004, 0.0116 and 0.020, respectively. There was a directional difference for morphological grades 3 vs. 4 with an false discovery rate-adjusted P=0.086.
Mean T2 relaxation times for cartilage classified as grades 0, 1, 2, 3 and 4 using MRI morphological sequences. Bars are standard deviations. Mean T2 relaxation times for cartilage classified as grades 1, 2 and 3 were significantly longer than for those classified as grades 0, 1 and 2, respectively (P<0.05). However, there were no significant differences between the mean T2 relaxation time of cartilage classified as grade 3 and that classified as grade 4
Discussion
Patellofemoral instability is a consequence of incongruence between the patella and the femoral trochlear groove. Abnormal patellofemoral congruence can result in acute episodes of patellar dislocation resulting in patellar cartilage damage. Patellofemoral incongruence also results in altered biomechanics of the patellofemoral joint and generates excessive contact stress and significant shearing forces [23] with early cartilage degeneration [24].
Patellofemoral instability is a leading cause of cartilage damage in physically active children and adolescents [1]. The overall incidence of cartilage damage in patellofemoral instability has been reported in adults and is variable depending on the chronicity of patellofemoral instability and modalities utilized in evaluating the cartilage damage. An arthroscopic study showed that more than half of patients with patellofemoral instability had patellar cartilage damage [25]. A higher incidence of cartilage damage was reported in a conventional MR imaging study, which documented a rate of cartilage damage ranging from 71% in patients with a single episode of dislocation to 97% in those with multiple episodes [26]. In our study, which did not subclassify the patellofemoral instability group based on chronicity, all patients with patellofemoral instability except one demonstrated patellar cartilage damage on morphological grading with conventional MR. Patellofemoral instability has a progressive nature and a tendency toward worsening of cartilage damage in both extent and severity, which directly correlates with duration of disease in adults [22]. It is worth noting that our patient cohort is younger than in previous studies but showed a higher incidence of cartilage damage.
Our work demonstrated that the medial facet of the patella in patellofemoral instability was more severely affected on the basis of morphological grading. We observed that high-grade (grade 3 or 4) cartilage damage is most frequent in the far medial aspect of the patella, whereas low-grade (grade 1) damage was distributed throughout all areas of the patellar cartilage with an increasing tendency of occurrence from the medial facet to the lateral facet, except for the far lateral aspect (L1) of the patella. Insall et al. [27] stated that in their large arthroscopic study, patellar cartilage damage was most commonly observed in the central area of the patella extending equally onto the medial and lateral facets. Indeed, variable areas of patellar cartilage lesions are produced by different injury mechanisms. Lateral facet chondral lesions are often related to chronic patellar tilt and excessive lateral pressure syndrome, whereas medial facet chondral lesions are commonly associated with patellar dislocation [28, 29].
Our study using T2 maps, as in other biochemical imaging researches, also provided the detailed information on the cartilage damage distribution [26, 30, 31]. Mean T2 relaxation times were significantly longer in the patellofemoral instability group than in the control group across all areas of the patellar cartilage. Furthermore, elongation of T2 relaxation times was most accentuated at the central areas of the patellar cartilage. These findings suggest that cartilage damage at the apex (C1 and C2) from friction and avulsion from the medial stabilizer (M1) are the main injury mechanisms in our patient group with patellofemoral instability. Given the longer relaxation times at the lateral facet in the group with patellofemoral instability than the group without patellofemoral instability, we believe that chondral injury in patellofemoral instability covers a wider range of the articular surface of the patella than expected, even extending far away from the epicenter of the injury.
Regarding diagnostic performance of imaging techniques, our results support a previous finding that patellar cartilage lesions in patients with anterior knee pain were wider and thicker on T2 maps as compared to what was seen on conventional knee MR imaging [32]. This highlights the fact that conventional MR sequences interpreted with the current most acceptable morphological grading system for cartilage damage do not fully detect microstructural changes or very early degenerative changes; however, these changes were detected on T2 mapping. The advantage of biochemical imaging over conventional MR imaging has been well recognized in cartilage imaging studies in adults, but this is the first study performed in children that documents the advantage of biochemical imaging.
With technical advancements, biochemical imaging has enabled imaging of the cartilage microstructure [15–18, 26–29]. These new biochemical MR techniques include T2 mapping, delayed gadolinium-enhanced MRI of cartilage (dGEMRIC), T1 rho imaging, sodium imaging and diffusion-weighted imaging. T2 mapping is relatively more easily applicable to the routine knee MR than the other biochemical techniques. T2 relaxation times obtained from T2 maps reflect the microstructural integrity of the extracellular matrix of the cartilage, specifically of the collagen network and water content. Prior studies done in adults with osteoarthritis provided good evidence that T2 mapping is useful in the detection of early-stage degeneration (early disruption of the collagen matrix) [30]. In contrast to adults, growing children have dynamic changes within the cartilage during skeletal maturation; T2 relaxation times decrease with chronological age [18] and the most dramatic changes occur at or near the circumferential physis at the base of the unossified cartilage [21]. Given the dynamic range of normal cartilage in growing children, coexisting pathological conditions might be more difficult to identify on conventional MR, if the changes are not accompanied by gross morphological cartilage abnormalities or if signal changes are not obvious. The superiority of biochemical imaging to conventional MR, therefore, could be maximized in cartilage imaging in children and adolescents.
Our study showed positive correlation between overall mean T2 relaxation times and morphological grading of patellar cartilage damage. That is, the higher morphological grade of the cartilage damage, the longer the T2 relaxation time. A statistically significant difference in the mean T2 relaxation times for each grade level was observed from grades 0 to 3. However, in high-grade cartilage damage (between grades 3 and 4), the T2 relaxation time was not significantly different. This study utilizes both conventional MR and biochemical imaging in cartilage evaluation in patients with patellofemoral instability. However, each imaging technique evaluates a different aspect of the cartilage; a dominant factor in determining the severity of morphological grading is the depth of cartilage defect regardless of the actual extent of adjacent cartilage injury. The biochemical MRI technique, unlike morphological sequences, reflects all range of cartilage damage in remaining cartilage.
We observed the discrepancy in the distribution of the severity of the patellar cartilage injury between T2 mapping and morphological grading; the most severe grade of morphological cartilage damage was seen at the medial facet while the central area of the patella had the longest T2 relaxation time. This discrepancy between the results from two different imaging techniques is again explained by the different natures of the imaging modalities. Therefore, in the evaluation of cartilage in patients with patellofemoral instability, we believe that conventional MR and biochemical imaging could provide complementary information depending on severity of cartilage damage.
Our study has some limitations. Although this is the largest study done in a pediatric population with patellofemoral instability, there may not have been enough cases of high-grade injury (grades 3 and 4) to detect a significant difference. The higher-grade cartilage damage was reported in patients with more episodes of dislocation [25]. However, we did not subclassify the patellofemoral instability group based on the chronicity of disease or mechanism of injury (dislocation vs. malalignment without dislocation). In our efforts to assess cartilage abnormalities in patients with patellofemoral instability, chronicity of the disease might be a significant factor. A future study with a larger sample size and an even number in each subgroup of morphological cartilage damage as well as consideration of the disease chronicity might be needed to identify the different patterns of cartilage damage. Second, this study is limited by the control group. The group without patellofemoral instability was not a true healthy subject cohort because all of them underwent knee MR imaging for a different clinical indication. Another limitation is that we did not take into account the spatial variations of T2 in different layers (superficial vs. deep) of the cartilage. Besides, we admit that it was tricky to exactly draw the ROIs over the cartilage in cases of high-grade cartilage defect. The final limitation is that none of our cases with cartilage damage was correlated with arthroscopic or histological findings.
Conclusion
Patellar cartilage damage in patients with patellofemoral instability occurs across the entire cartilage. T2 relaxation times positively correlate with morphological grades of cartilage lesions, significantly differentiating the severity in low grades, which implies an important role in differentiating normal cartilage and low-grade cartilage damage. Therefore, in clinical practice, biochemical imaging of T2 maps and morphological MR studies complement each other.
References
Heywood AWB (1961) Recurrent dislocation of the patella - a study of its pathology and treatment in 106 knees. J Bone Joint Surg (Br) 43:508–517
Hawkins RJ, Bell RH, Anisette G (1986) Acute patellar dislocations. The natural history. Am J Sports Med 14:117–120
Lance E, Deutsch AL, Mink JH (1993) Prior lateral patellar dislocation: MR imaging findings. Radiology 189:905–907
Elias DA, White LM, Fithian DC (2002) Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology 225:736–743
Guerrero P, Li X, Patel K et al (2009) Medial patellofemoral ligament injury patterns and associated pathology in lateral patella dislocation: an MRI study. Sports Med Arthrosc Rehabil Ther Technol 1:17
Kirsch MD, Fitzgerald SW, Friedman H et al (1993) Transient lateral patellar dislocation: diagnosis with MR imaging. AJR Am J Roentgenol 161:109–113
Nomura E, Horiuchi Y, Inoue M (2002) Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee 9:139–143
Sanders TG, Paruchuri NB, Zlatkin MB (2006) MRI of osteochondral defects of the lateral femoral condyle: incidence and pattern of injury after transient lateral dislocation of the patella. AJR Am J Roentgenol 187:1332–1337
Virolainen H, Visuri T, Kuusela T (1993) Acute dislocation of the patella: MR findings. Radiology 189:243–246
McNally EG, Ostlere SJ, Pal C et al (2000) Assessment of patellar maltracking using combined static and dynamic MRI. Eur Radiol 10:1051–1055
Diederichs G, Issever AS, Scheffler S (2010) MR imaging of patellar instability: injury patterns and assessment of risk factors. Radiographics 30:961–981
Tiderius C, Hori M, Williams A et al (2006) dGEMRIC as a function of BMI. Osteoarthritis Cartilage 14:1091–1097
Urish KL, Keffalas MG, Durkin JR et al (2013) T2 texture index of cartilage can predict early symptomatic OA progression: data from the osteoarthritis initiative. Osteoarthritis Cartilage 21:1550–1557
Mosher TJ, Liu Y, Torok CM (2010) Functional cartilage MRI T2 mapping: evaluating the effect of age and training on knee cartilage response to running. Osteoarthritis Cartilage 18:358–364
Nieminen MT, Nissi MJ, Mattila L et al (2012) Evaluation of chondral repair using quantitative MRI. J Magn Reson Imaging 36:1287–1299
Mosher TJ, Dardzinski BJ (2004) Cartilage MRI T2 relaxation time mapping: overview and applications. Semin Musculoskelet Radiol 8:355–368
Mosher TJ, Dardzinski BJ, Smith MB (2000) Human articular cartilage: influence of aging and early symptomatic degeneration on the spatial variation of T2--preliminary findings at 3 T. Radiology 214:259–266
Kim HK, Shiraj S, Anton CG et al (2014) Age and sex dependency of cartilage T2 relaxation time mapping in MRI of children and adolescents. AJR Am J Roentgenol 202:626–632
Brattstroem H (1964) Shape of the intercondylar groove normally and in recurrent dislocation of patella. A clinical and X-ray-anatomical investigation. Acta Orthop Scand Suppl 68:61–148
Hughston JC (1968) Subluxation of the patella. J Bone Joint Surg Am 50:1003–1026
Shiraj S, Kim HK, Anton C et al (2014) Spatial variation of T2 relaxation times of patellar cartilage and physeal patency: an in vivo study in children and young adults. AJR Am J Roentgenol 202:W292–W297
Shaffer JP (2007) Controlling the false discovery rate with constraints: the Newman-Keuls test revisited. Biom J 49:136–143
del Mar Carrion Martin M, Santiago FR, Calvo RP et al (2010) Patellofemoral morphometry in patients with idiopathic patellofemoral pain syndrome. Eur J Radiol 75:e64–e67
Davis IS, Powers CM (2010) Patellofemoral pain syndrome: proximal, distal, and local factors, an international retreat, April 30-May 2, 2009, Fells Point, Baltimore, MD. J Orthop Sports Phys Ther 40:A1–A16
Franzone JM, Vitale MA, Shubin Stein BE et al (2012) Is there an association between chronicity of patellar instability and patellofemoral cartilage lesions? An arthroscopic assessment of chondral injury. J Knee Surg 25:411–416
Vollnberg B, Koehlitz T, Jung T et al (2012) Prevalence of cartilage lesions and early osteoarthritis in patients with patellar dislocation. Eur Radiol 22:2347–2356
Insall J, Falvo KA, Wise DW (1976) Chondromalacia patellae. A prospective study. J Bone Joint Surg Am 58:1–8
Fulkerson JP, Buuck DA (2004) Disorders of the patellofemoral joint. Lippincott Williams & Wilkins, Philadelphia
Outerbridge RE (1961) The etiology of chondromalacia patellae. J Bone Joint Surg (Br) 43-B:752–757
Watanabe A, Obata T, Ikehira H et al (2009) Degeneration of patellar cartilage in patients with recurrent patellar dislocation following conservative treatment: evaluation with delayed gadolinium-enhanced magnetic resonance imaging of cartilage. Osteoarthritis Cartilage 17:1546–1553
Bengtsson Moström E, Lammentausta E, Finnbogason T et al (2015) Pre- and postcontrast T1 and T2 mapping of patellar cartilage in young adults with recurrent patellar dislocation. Magn Reson Med 74:1363–1369
Hannila I, Nieminen MT, Rauvala E et al (2007) Patellar cartilage lesions: comparison of magnetic resonance imaging and T2 relaxation-time mapping. Acta Radiol 48:444–448
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Kang, C.H., Kim, H.K., Shiraj, S. et al. Patellofemoral instability in children: T2 relaxation times of the patellar cartilage in patients with and without patellofemoral instability and correlation with morphological grading of cartilage damage. Pediatr Radiol 46, 1134–1141 (2016). https://doi.org/10.1007/s00247-016-3574-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-016-3574-2