Abstract
Background
India had a population of 1,259,271,000 in 2012, with 31% of its population composed of children younger than 15 years. In comparison, children younger than 15 compose 20% of the population in the United States and 16% in Canada. Despite the differences in this demographic, little emphasis is placed on pediatric radiology in India.
Objective
To conduct a needs assessment evaluating the adequacy of pediatric radiology in India and to establish a pediatric radiology education program in India.
Materials and methods
We developed a questionnaire to assess radiologists’ perspective on the quality of training in pediatric radiology. Responses were obtained from attendees at a pediatric radiology education program in Mumbai. These data were used to obtain funding and implement a program to increase awareness and stimulate pediatric radiology training at select institutions across India.
Results
Out of 86 respondents, 82% indicated that their academic institutions did not place emphasis on dedicated pediatric radiology training, and 63% indicated they received less than 2 weeks of dedicated training. Of the respondents, 77% said their institutions practiced pediatric radiology with inadequate standard of care and 75% of respondents said pediatric radiology would gain increasing importance in the future. Outcomes of the implemented program included increased awareness of pediatric radiology and establishment of a pediatric radiology fellowship program in India.
Conclusion
Education and training in pediatric radiology in India is inadequate. Focused initiatives have the potential to improve the standards set for pediatric radiology in India. Similar initiatives could help develop pediatric radiology in other developing countries.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
India is one of the most populous countries in the world with 1,259,271,000 people, and a significant portion of its population comprises young children [1]. According to population statistics from 2012, 31% of India’s population was comprised of children younger than 15 years, a percentage higher than that of the United States (20%) and almost double that of Canada (16%) [2]. With such a large pediatric population in India, the importance of providing quality health care to children is critical. Although the mortality rate for children younger than 5 years in India has been reduced by approximately 3% per year since 1990, 24% of the world’s total deaths in children younger than 5 occur in India [3], leading all nations. Thirty percent of neonatal deaths worldwide occur in India. For children younger than 15 years, India is also the global leader in estimated total deaths secondary to malignant neoplasms [4].
Until recently, little emphasis had been placed on pediatric radiology subspecialization within India. The subspecialty has not generated sufficient interest among post-residency graduates; there were no post-graduate pediatric radiology fellowship programs in India until 2012, according to courses listed on the Medical Council of India website [5]. An editorial published in the Indian Journal of Radiology and Imaging (IJRI) shed light on clinician and trainee perspectives regarding the current state of pediatric radiology in India, suggesting that a lack of subspecialty training is a cause of sub-optimal care provided to children requiring medical imaging [6]. Further, qualitative feedback from various conferences and Indian radiologists also suggested that pediatric radiology receives much less attention in radiology residency programs when compared against other subspecialties in radiology. Although previous research offers some insight into the state of pediatric radiology in India, there has not been a formal report elucidating the current status of this subspecialty in India or in other developing countries. Efforts are being made to improve pediatric radiology training and skills even from within India. India has a handful of fellowship-trained pediatric radiologists from overseas. Additionally, the Indian Society of Paediatric Radiology (ISPR) was established in 2003 and has been gaining influence in the last few years. It has approximately 330 life members and had 356 registered delegates at the last annual conference in 2012 [7].
Our study had two main objectives: (1) to conduct a needs assessment, elucidating the current status of pediatric radiology in India, and (2) to initiate a pediatric radiology educational training program in India. Highlights of the outcome of our needs assessment and initiatives taken to expand upon and improve pediatric radiology in India are also discussed.
Materials and methods
Educational training program
A 2-day interactive teaching program was introduced to train radiologists and radiology residents (n = 156) in India on topics including ultrasound of the neonatal brain, cervical spine trauma management, common pediatric abdominal conditions, radiation dosing and risks, and bone tumors in children (Table 1). The program was conducted Nov. 7-8, 2009, at King Edward Memorial Hospital, a government-funded public medical college in Mumbai, and program registration fees were 2,000 rupees ($34 CAD) for radiologists and 1,000 rupees ($17 CAD) for radiology residents. The program was hosted locally by the Radiology Education Foundation (REF) and designed and organized in collaboration with the tertiary-care Hospital for Sick Children, Toronto, Canada. It was initially funded by a seed grant through the Global Child Health program of SickKids International.
Needs assessment
A questionnaire was administered to attendees of the teaching program. The questionnaire was developed by the authors of this study, who drew on their backgrounds in both psychometrics and radiology education. A hard-copy format of the questionnaire was provided in all quiz and lecture sessions during the program and responses were anonymous. Its purpose was to gather feedback from the attendees regarding their training and clinical experiences, competencies and attitudes and perceptions toward the subspecialty of pediatric radiology in India.
The questionnaire consisted of 18 questions: 15 questions were presented on a Likert equidistant 5-point scale and the remaining 3 questions were presented in multiple-choice format (Appendix 1). In exchange for their participation, attendees had the opportunity to win pediatric radiology textbooks through a lottery-like drawing conducted at the end of the program. The data from this needs assessment were used to apply for the N. Thorne Griscom Award for education by the Society for Pediatric Radiology (Fig. 1).
Analysis
The results were tabulated showing the proportion of respondents (compared to the total number of overall respondents) and their respective answers (Table 2).
Results
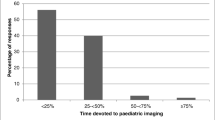
Completed questionnaires were obtained from 86 out of the 156 attendees; 76% of the respondents were radiology residents; 80% of the respondents indicated that pediatric radiology is a very important part of their practice, and 52% of respondents indicated that 20–40% of their current patients are classified as pediatric (Fig. 2). With regard to respondents’ training experiences, nearly two-thirds (63%) indicated that they had received less than 2 weeks of dedicated pediatric radiology training (Fig. 3), with 82% indicating a belief that their institutions did not place any importance on dedicated pediatric radiology training. With regard to training, 45% indicated that it was not important to have adequate training in pediatric radiology; 23% were equivocal. Greater than half (57%) agreed that their training was inadequate and 17% were equivocal. When asked whether respondents believed their institutions practiced pediatric radiology at an adequate standard of care, 77% did not think so. With regard to respondents’ perceptions about their competencies in handling children, 47% were equivocal, 30% thought they were not competent and 22% though they were competent in handling pediatric patients. Perhaps most important, 75% of respondents thought pediatric radiology would gain increasing importance in the near future (Fig. 4).
Funding obtained was used to implement a pediatric radiology education program in select cities and institutions. This has led to a variety of outcomes, including the establishment of the first pediatric radiology fellowship in India, a national debate on pediatric radiology subspecialization at the 10th Annual Conference of the ISPR (Sept. 29, 2012) and an overall heightened awareness of the increasing importance of this subspecialization in select medical teaching institutions. This is reflected in an oration as an extension of the editorial published in IJRI [6], which further outlines the challenges of pediatric radiology, perceptions in the field and potential solutions to increase pediatric radiology subspecialization in India.
Discussion
Our needs assessment demonstrated respondents’ lack of training and confidence in their pediatric radiology practices despite a general consensus of the importance of pediatric radiology. Furthermore, the issue of sub-optimal pediatric radiology practices affecting health care institutions in India was acknowledged by the majority of program attendees as an ongoing concern in need of remediation.
These results should be interpreted with caution, however, because educational endeavors based on resident- or trainee-identified needs might be limited to the perceived needs as unperceived needs go unrepresented and hence unaddressed. For this reason, we gathered perspectives from radiologists, as well, who were able to draw on their more extensive experiences in educational and clinical settings. Further caution should be taken, because our particular needs assessment demonstrated a 56% response rate among program attendees. Whether this translates proportionally to the remaining population of radiologists in India is unknown and warrants further investigation. It is possible that our sampling group is not representative of the overall population of Indian radiologists because it was based on a non-random sample of the population. Likewise, given that India is such a vast and populous country it is plausible that we do not have information or clinicians’ opinions from other centers of excellence regarding pediatric radiology subspecialization. Conversely, however, the current inadequacies in pediatric radiology training in India might also be underestimated by our results given the local sample of the population.
The lack of confidence and training in pediatric radiology practices expressed by the program attendees can be attributed to the underdevelopment of pediatric radiology as a subspecialty in India. India has a shortage of pediatric radiologists and inadequate training in this subspecialization [6]. In developed countries a lack of interest in pediatric radiology as a subspecialization also exists [8–10] and stems from fellows’ perceptions that the field of pediatric radiology is too broad to master sufficiently, growing fears of being overworked because of the shortage of staff pediatric radiologists, a perceived lack of time and teaching resources for faculty to adequately train their fellows and residents, perceived difficulties of handling small and delicate patients, and lower financial compensation when compared to other radiology subspecializations [11]. By developing curricula to mitigate these concerns, we might succeed at advancing interest in the field and improving the condition of this subspecialty in India.
It is interesting to note that pediatric radiology in India has not shown the same trend as other pediatric specialties (e.g., pediatrics, pediatric surgery). In India, these specialties have grown both academically and with regard to patient care, which is a change that has not occurred within pediatric radiology (S. V. Gibikote & S. N. Keshava, Christian Medical College, personal communication).
Despite the minimality of the pediatric radiology subspecialization in India, qualitative feedback received and fervent audience interaction during the 2-day program suggested an interest in future educational seminars focused on teaching pediatric radiology in greater depth with expert instruction [6], which could lead to improvement in pediatric radiology services and awareness in India, thus improving health care for children.
Outcomes
Based on the results of our needs assessment and funding available from the Society for Pediatric Radiology and the University of Toronto, a number of steps have been taken to improve pediatric radiology education in India. Initial steps involved the induction of a program to develop and implement a sustainable, appropriately designed pediatric radiology teaching program for radiology residents in India. The program was initiated to address the aforementioned inadequacies of pediatric radiology in India and follows the Royal College of Physicians and Surgeons of Canada (CanMEDS) Physician Competency Framework as its basis. The aim of the program was to fortify the clinical skills of resident and consultant radiologists in the field of pediatric radiology in India. The curriculum included detailed, interactive teaching seminars covering topics including how to interact with a child in a radiology suite, safe sedation practices, principles of the Image Gently campaign [12] and administering reduced and optimized radiation doses to pediatric patients, among other topics. Teaching seminars were designed to further develop the role of the medical expert in pediatric radiology by seeking consultations with specialists (e.g., child life specialists and pediatric anesthesiologists).
Funding has also enabled radiologists from the Hospital for Sick Children, a tertiary-care children’s hospital in Toronto, to lead structured education programs about safe radiation practices and imaging techniques in various parts of India (Fig. 5). Additionally, opportunities were made available for trainees and junior radiologists from India to pursue visiting fellowships offered at the Hospital for Sick Children in Toronto, enabling these clinicians to transfer skills and knowledge acquired during their fellowship to their native institutions.
Outcomes of needs assessment in India. Site visits and respective pediatric radiology conferences. Two site visits were made at the Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, Punjab (1). PGIMER directors hope to start a pediatric radiology fellowship program in 2014. The Dr. Sampurnanand Medical College, Jodhpur, Rajasthan (2) conducted a pediatric radiology conference and a pediatric CT radiation dose meeting and hosted one site visit. The Radiology Education Foundation hosted our pilot training program at King Edward Memorial Hospital, Mumbai, Maharashtra (3). One site visit was made to Seven Hills Hospital, Mumbai, Maharashtra (4), where a pediatric radiology symposium and CT radiation dose meeting were also conducted. The Christian Medical College (CMC), Vellore, Tamil Nadu (5), inaugurated pediatric radiology fellowship training in India. Multiple site visits and teaching seminars have been conducted at CMC, and it is to host another pediatric radiology conference in September 2014. The Sree Chitra Tirunal Institute for Medical Sciences and Technology, Thiruvananthapuram, Kerala (6), has conducted a pediatric neuroradiology conference
Moreover pediatric radiology is starting to gain importance in India as a result of the Indian Society of Paediatric Radiology, local pediatric radiology leaders and our pediatric radiology education program. For example, the Post-Graduate Institute of Medical Education & Research (PGIMER) in India announced two new seats to the pediatric radiology fellowship program in September 2012 [13]. Institution leaders are optimistic that they will be able to recruit candidates by early 2014. Furthermore, Christian Medical College (CMC), Vellore, is one of the first hospitals to offer a pediatric radiology fellowship program in India, and it had a fellow in training as of March 2013. Funding for this program has allowed seven radiologists with an interest in pediatric radiology subspecialization, under full or partial sponsorship, to complete visiting fellowships of 2–12 weeks at the Hospital for Sick Children in Toronto.
Long-term outcomes of implementing such changes include improvements in training, knowledge and competencies among radiology residents and licensed radiologists in India. This is likely to help advance diagnostic and interventional pediatric radiology through the development of trainees who are confident in their imaging skills and knowledge, thereby allowing for these radiologists to provide safe and effective care to children.
We believe the shortage of well-established pediatric radiology fellowship programs and the associated challenges also affect other developing countries. We hope these initiatives can be used to evaluate inadequacies in pediatric radiology across other jurisdictions and provide a framework to improve training and knowledge and promote learning within this specialty. This could be done using a multipronged approach. For example in urban areas with large academic or advanced health care institutions, the large population of children would be well served with sub-specialized pediatric radiologists, whereas in smaller health centers or smaller towns children would benefit from improved pediatric radiology training of general radiologists. Currently, 26% of the world’s population comprises children younger than 15 years; however this number is typically higher for less developed countries [1, 2], where population statistics might not be completely representative. Coupled with projections indicating that developing countries will make up 86% of the global population in 2050 [1], it is imperative that well-trained and knowledgeable pediatric radiologists are available to improve care in the developing world.
Conclusion
Pediatric radiology education and training in residency programs in India are inadequate, according to feedback from radiology residents and staff radiologists in the country. Developing countries might have similar deficiencies in pediatric radiology. Structured and formal education programs can allow for the development of well-trained pediatric radiologists and improved care for children in the developing world.
References
Population Reference Bureau. 2012 World Population Data Sheet. http://www.prb.org/pdf12/2012-population-data-sheet_eng.pdf. Cited 22 July 2013
Population Reference Bureau. Population < 15. http://www.prb.org/DataFinder/Topic/Rankings.aspx?ind=10. Cited 22 July 2013
Liu L, Johnson HL, Cousens S et al (2012) Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 379:2151–2161
World Health Organization (2011) Mortality and burden of disease estimates for WHO member states in 2008. World Health Organization, Geneva. http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/. Cited 30 Oct 2012
Medical Council of India (2010) http://www.mciindia.org/InformationDesk/ForStudents/ListofCollegesTeachingPGCourses.aspx. Cited 23 Sept 2011
Jankharia B (2010) The subspecialization conundrum. Indian J Radiol Imaging 20:1
Indian Society of Paediatric Radiology. http://ispronline.com. Accessed 11 Aug 2013
Bramson RT, Taylor GA (2005) SOS: can we save pediatric radiology? Radiology 235:719–722
Bramson RT, Taylor GA, Blinder R (2005) PEDRAP: a new training alternative for pediatric radiologists. Pediatr Radiol 35:454–455
Merewitz L, Sunshine JH (2006) A portrait of pediatric radiologists in the United States. AJR Am J Roentgenol 186:12–22
Gunderman RB (2004) Strategies for attracting residents to understaffed radiologic specialties: the case of pediatric radiology. J Am Coll Radiol 1:800–803
The Alliance for Radiation Safety in Pediatric Imaging (2013) Image Gently. http://www.pedrad.org/associations/5364/ig/?page=364. Cited 13 Aug 2013
The Indian Express (2012) PGI set to introduce paediatric radiology course from next year. http://www.indianexpress.com/news/pgi-set-to-introduce-paediatric-radiology-course-from-next-year/1009409/. Cited 25 June 2013
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Appendix 1. Needs assessment questionnaire from the pediatric radiology pilot education program
Appendix 1. Needs assessment questionnaire from the pediatric radiology pilot education program


Rights and permissions
About this article
Cite this article
Sidhu, A., Sheikh, N., Chavhan, G. et al. Improving pediatric radiology in India. Pediatr Radiol 44, 657–665 (2014). https://doi.org/10.1007/s00247-013-2868-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-013-2868-x