Abstract
This review is a bird’s eye view of the practice of pediatric radiology in India. The key focus of this article is training, certification and employment opportunities for radiologists aspiring to specialise in pediatric radiology. Further, we have traced the growth in academic and research opportunities over the past two decades, as well as given a peep into the future trajectory of this speciality. An understanding of these concepts is key to the expansion of pediatric radiologists not just within India, but across the globe.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pediatric radiology is a rapidly growing speciality in most parts of the world. This has been facilitated primarily by a growing realisation of the adage ‘children are not small adults’, among both radiologists and physicians. The stages of normal physiological development lend themselves to unique imaging manifestations in children, which are often challenging to interpret for those not well versed with pediatric imaging. Similarly, pediatric diseases/disorders can have imaging manifestations that pose difficulties for general radiologists who may not be familiar with these conditions. These include congenital, metabolic and genetic disorders; malignancies; as well as structural malformations. Many of these conditions are rare, at best, and often general radiologists spend an entire career having encountered only a handful of these in their practice.
As per the 2011 census of India, 36.7% of the population was below 18 years, which amounts to approximately 444 million children. The projected number of children in the year 2016 had risen to 448 million children [1]. This further highlights the need for sub-speciality trained pediatric radiologists, in order to cater to the needs to this burgeoning population of children.
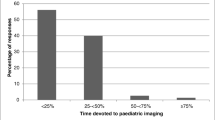
Training
In India, the undergraduate medical degree is offered at 706 colleges, with an annual intake of over 109,000 students. Following this, students typically undergo 3 years of training in radiology, the MD (doctor of medicine) or the DNB (diplomate of national board) programme. The MD programme is available at 221 institutes across the country, while the DNB programme is offered at 186 institutes, which form a total annual intake of nearly 2200 students. During this period, residents are exposed to a multi-speciality spectrum, of which pediatrics forms a small part, limited mostly to common entities such as spinal dysraphism, genitourinary and anorectal malformations, and common malignancies such neuroblastoma, Wilms tumor, hematological disorders and bone tumors of childhood. In addition, bulk of the daily case interpretation focusses on infections, particularly tuberculosis, and thus students are trained in pattern-based reporting of both pre- and post-treatment imaging findings of tuberculosis. It is noteworthy that there is significant variation across institutes in training residents in pediatric radiology, based on footfall, referral base as well as experience of faculty members. Further, as per National Medical Council (NMC) guidelines, only the months to be spent in each modality have been stipulated, but not in each subspeciality. There is also a description of curriculum based on anatomical organ systems, among which common pediatric conditions feature, but dedicated pediatric radiology training has not been listed in the curriculum. In a study conducted by Sidhu et al. nearly a decade ago, 63% of respondents had less than 2 weeks of dedicated pediatric radiology training during their residency [2]. Therakathu et al. followed up this work a few years later, and found that among delegates of a pediatric radiology conference in India, perceived inadequacy of training in pediatrics during the MD Radiology programme was still reported by 61.7% of the respondents [3].
This reported lacuna has been addressed to a large extent by the boom in online education seen during the years 2020–2021, which was initially tailored to address the interruption in training during the COVID-19 pandemic. The Indian College of Radiology and Imaging (ICRI) has since then formalised various modules for resident education which are available in an on-demand format and updated weekly [4]. Most subspecialities, including pediatrics have been included, which include essential resources for exam preparation and daily clinical practice. ICRI in conjunction with the Indian Society of Pediatric Radiology (ISPR), conducted a full-day pediatric radiology workshop on the 4th of February 2024, which was attended by 335 delegates. However, it must be borne in mind that online webinars do not provide a substitute to clinical radiology training as in a pediatric radiology rotation, and thus effort must be made to increase the time residents spend in pediatric radiology.
For those seeking to specialise further in this field, the options are currently limited to fellowships in pediatric radiology, which train fellows in diagnostic radiology, interventional procedures or a combination of both, based on the centre’s expertise and experience. While some institute allow candidates to apply immediately post MD/DNB, others require a mandatory period of senior residency (post MD training) which may range from 1 to 3 years. Since these fellowships are only a recent addition to the radiology education spectrum, most radiologists until now have relied on informal training and clinical experience acquired over years of sub-speciality practice. In addition, many private centres follow a modality-based specialization, for instance, the radiologist who has specialised in ultrasonography would be performing all pediatric sonography as part of the routine workflow, and thus would have developed a reasonable level of expertise in this.
Centres training pediatric radiologists in India
Fellowship programmes or post-doctoral certificate courses (PDCC) were initially offered only at institutes of national eminence, operating under the government of India, including All India Institute of Medical Sciences (AIIMS) New Delhi, Christian Medical College (CMC) Vellore and Postgraduate Institute of Medical Education & Research (PGIMER) Chandigarh. Recent additions to these have been the the All India Institutes of Medical Sciences at Jodhpur (Rajasthan) and Rishikesh (Uttarakhand). Further, there has been introduction of these courses at few other smaller institutes in cities such as Bangalore (Karnataka), Chennai (Tamil Nadu) and Pune (Maharashtra), spearheaded by experienced pediatric radiologists with established practice at these centres. However, the intake of these courses ranges from only one or two trainees per year, which means the total output of trained radiologists is 5–7 per year. This is the reason that fellowship trained pediatric radiologists remain a small group in the present scenario. There is no accreditation information of these courses in either the NMC or the National Board of Examinations (NBE) database.
While the curriculum across all programmes is similar in terms of cumulative exposure to imaging modalities such as computed tomography (CT), magnetic resonance imaging (MRI), ultrasonography and fluoroscopy, the training schedule is not standardized and varies between institutions. For instance, while some prefer to have a daily rotation of fellows among imaging modalities, others would follow a monthly or two-monthly rotation.
The issue of pediatric ultrasonography training among pediatric radiology fellows has been raised in the past by Back and colleagues in their study conducted in the USA [5]. They reported that only 23.3% fellows had undertaken ultrasonography scanning without a sonographer during their fellowship, despite 58.6% programme directors reporting a dedicated US curriculum in the programme. In India, on the other hand, all ultrasound scans are performed by radiologists. There is a focus on specialised pediatric ultrasonography performed by fellows, which are often under direct supervision of faculty. In fact, based on the authors’ experience from institutes they have worked at, a number of physicians rely exclusively on reports issued by pediatric radiologists, either fellows or faculty, and often request for re-scanning in case scans have been performed by non-pediatric radiologists.
Further, the range of interventional procedures also differs based on institutional organisation. While some have a diagnostic radiology focussed approach, others provide a wide spectrum of interventional radiology procedures. For instance, at the authors’ institution, there is a myriad of interventional procedures including vascular malformation embolisation, esophageal dilatation, embolisation and stenting in congenital portal venous anomalies as well as urological procedures such as percutaneous nephrostomies and ureteric stenting. It must be kept in mind that the requirement for guided biopsies, drainages and vascular access lines is universal, across all centres.
Another crucial aspect of the pediatric radiologist’s training is understanding the clinician’s perspective and learning to be an integral part of multidisciplinary teams (MDT) with improved diagnosis and patient management. Since most of these institutes have sub-speciality based training in clinical pediatrics and pediatric surgery, a system of weekly MDT discussions has evolved that allows residents and consultants of multiple specialities to interact, exchange information and improve patient outcomes. These are currently functional in disciplines such as pediatric surgery, pediatric pulmonology, pediatric oncology and pediatric neurology.
Employment opportunities
There is no stipulated number or percentage of work hours for designation of a speciality radiologist in India. Radiologists working at pediatric hospitals or child care centres, or those in multi-speciality institutes who devote a significant proportion of time to work in the pediatric domain are designated pediatric radiologists. Based on the ISPR membership, nearly 500 radiologists identify as either part-time or full-time pediatric radiologists in India. As previously mentioned, since the pediatric radiology fellowship programme is a recent addition which is available only at select institutes, fellowship trained radiologists are only 40–50 in number and make up < 10% of the pediatric radiology workforce. The major proportion of pediatric radiology work is therefore undertaken by general radiologists who have gained expertise by virtue of experience in the speciality.
In the analysis conducted by Therakathu et al. in 2017, 56% of respondents showed interest in pursuing pediatric radiology as a career [3]. While this may represent a significant bias considering the survey was conducted at a conference dedicated to pediatric radiology, it still represents an encouraging metric for promotion of pediatric radiology as an independent subspeciality. It is interesting however that the pressing issues reported in this paper that hinder radiologists from opting for pediatric radiology as opposed to other subspecialities, or even versus no specialisation have still not been fully addressed. There is a lack of jobs for trained pediatric radiologists in both the public and the private sector. While large academic institutions do employ radiologists for sub-speciality practice and training, the number of such institutions is small and thus, the turnover of vacancies for subspeciality trained radiologists is also low. There are ~ 20 eminent national institutes in India, among which only half offer dedicated pediatric radiology services and employ speciality radiologists. Further, another 4–5 teaching institutes in the private sector also run pediatric radiology services.
A persistent concern among hospitals other than quaternary care centres has been the challenge of imaging children, including the need to arrange adequate sedation or anesthesia. The lack of adequate technical wherewithal in these hospitals and imaging centres, including anesthesia equipment, pediatric sized resuscitation equipment, dedicated pediatric anesthesia team as well as apprehension regarding potential complications of sedation, prevents them from increasing the workload.
A heartening trend in the recent ~ 7–8 years has been the emergence of private healthcare providers with multiple branches dedicated to childcare, and it is postulated that their growth may provide gainful employment for those trained in the imaging of infants and children. However, this appears to be an intermediate to long term goal rather than a short term outcome. Another positive has been the growth of molecular diagnostics including genomic sequencing and mutation analysis in the last decade. This has led to rapid leaps in the management of children with inherited genetic and metabolic disorders, translating into better care and improved survival. In this setting, physicians face an increasing need for sub-speciality radiologists to correlate imaging with genomic diagnosis, accurately define extent and offer meticulous follow up including monitoring of treatment related complications unique to this population.
Educational activities
The ISPR was constituted in 2003, with the aim of bringing together radiologists across the country practising pediatric radiology to foster educational opportunities and growth of the speciality [6].
The society conducts an annual national conference, along with several continuing medical education (CME) events throughout the year at various locations, aimed both towards resident education and updating practising radiologists. These meetings also provide networking opportunities for radiologists working in geographically diverse locations and set the foundation for multi-centre collaborations. The ISPR has also collaborated with international societies such as the Asian Oceanian Society for Pediatric Radiology (AOSPR) [7] for their annual national meeting. Further, members of the ISPR also participate in events of the Society for Pediatric Radiology (SPR) [8] and the European Society of Paediatric Radiology (ESPR) [9]; and seek to learn from the experience of their international colleagues via efforts such as co-authoring publications or inviting them for scientific symposia. The ISPR is also a member of the World Federation of Pediatric Imaging (WFPI) and a signatory to the Image Gently pledge.
The challenge being faced by radiologists in search of specialist employment opportunities is a ‘turf war’ with subspecialists of clinical branches, who have 3-year training programmes in their subspecialities, which follows the 3-year MD/DNB programme in pediatrics. Due to this long training period, they are very well versed with the imaging manifestations of disorders frequently presenting to their clinics. This is particularly rampant in pediatrics, since pediatric radiology is arguably the vastest subspeciality, including multiple organ systems as well as a host of developmental variations, translating into an enormous spectrum to be mastered by a pediatric radiologist. As opposed to this, specialist physicians may only focus on a single organ system, such as pediatric nephrology or neurology. In this scenario, it is of paramount importance that radiologists be on ‘top of their game’, continuously learning and enhancing their knowledge, to stay updated with the latest guidelines, new research and emerging knowledge across the world, so they remain relevant in the diagnostic algorithm. In this regard, development of structured reporting formats, disease specific, or indication specific, can go a long way in ensuring high quality reports and harnessing the advantages of each modality. Several of these are currently in use, such as for CT and MRI of the temporal bone, cardiac CT, US in children with neonatal jaundice, US of pediatric kidney, ureter and bladder (KUB).
Research
In the past decade, there has been a steady growth in research quality, time devoted to research as well as the publication output of Indian pediatric radiologists. Further, there has also been an increase in research work undertaken in the field of pediatrics by MD radiology residents, no doubt due to mentorship by senior pediatric radiologists at educational institutions. This was documented at the ISPR annual conference in 2019, where nearly 150 abstracts were selected for presentation, ~ 90% of which were submitted by residents or fellows. This number saw a dip during the COVID-19 pandemic; however, the recent annual meeting in 2023 showed a revival of research interest, with nearly a hundred submitted abstracts, an overwhelming majority again by residents and fellows.
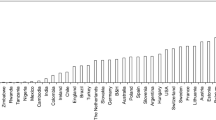
The positive trend in India’s contribution to international pediatric radiology research has also been reflected in the work by editors of Pediatric Radiology journal, who analysed the percentage of publications from low income (LIC) and lower-middle income countries (LMIC) from 2019 to 2022. India’s share was consistently the highest among all the countries compared, and showed an increase from 1.7 to 4.3% in the span of these 4 years itself [10]. As the authors rightly pointed out, the share of submitted papers may have been even greater, and it is likely that the rejection rate was higher. It was documented that the rate of acceptance of manuscripts by authors from upper middle income countries (UMIC) was seven times that of manuscripts by authors from LMICs. In this regard, the commitment by the Pediatric Radiology editors [11] to increase the representation of LIC and LMICS in the journal, by initiatives such as mentoring of authors as well as reviewers from these countries, will definitely encourage young researchers from India, seeking to conduct high quality research with international reach.
Future directions
To foster the growth of pediatric radiology as a speciality in India, a three-pronged strategy must be applied. The first would be creation of awareness regarding training programmes, their nature, availability, and a well-structured curriculum. In a study conducted by Lu et al. on pediatric radiology fellowship content in the USA and Canada, they found that of the 45 Accreditation Council for Graduate Medical Education (ACGME) approved programmes in the USA, 43 had active websites [12]. Similarly, among the 9 Canadian programmes, 8 had active websites. Further, a list of running fellowship programmes was available at a centralised electronic database in each country. Individual programme websites also contained details on the structure including clinical training and research opportunities, expected remuneration, and the application process. Such a centralised database must be compiled in India as well, with the collaborative effort of programme directors of fellowship programmes at various institutes, as well as the ISPR. An effort has been made in this regard by Café Roentgen [13]. The website documents open positions in various fellowships as well as carries detailed reviews from previous students. However, the information is not comprehensive, and also is rather subjective since the curriculum information is in the form of an opinion and not posted by an official source such as university in-charge or programme director. Further, formal accreditation of these fellowships via the National Medical Council (NMC) must be sought. It is a practice among residents nearing completion of the MD programme to look for further educational opportunities, and in fact, in the study by Therakathu et al., 97.5% respondents voted for an increase in the number of pediatric radiology fellowships in the country [3]. However, knowledge about existing programmes and their specific advantages was dismally low, and thus such a centralised repository is the need of the hour.
The other aspect of this would be exploration of developing imaging techniques and tailoring a ‘child-sized’ approach among each. Imaging equipment is a radiologist’s eyes and ears, and therefore, we must make a concerted effort to embrace new technology, and offer state of the art imaging, so patients as well as physicians may truly understand our capability in diagnosis. The world of pediatric radiology is currently changing with the advent of photon counting CT. A study by Siegel et al. comparing radiation dose of photon counting CT with energy integrating detector (EID) CT in pediatric high resolution CT chest showed a significant difference in the radiation dose, the reduction was nearly 45% [14]. Based on discussions at the recent annual SPR meetings, as well as online content, it appears as if institutes acquainted with this technology have shifted their approach from ‘No CT’ to ‘Do CT’, due to its capacity for high quality imaging with significant dose reduction. With administrative financial support, we must attempt to offer the same to our patients as well. Similarly, other technology such as contrast enhanced ultrasonography, which have the ability to alter the challenging logistics of cross-sectional imaging at centres without adequate anaesthesia support, must be sought and utilised.
The last, but not the least, would be the expansion of interventional radiology into the realm of pediatrics. Children have a host of unique requirements for procedures, including pain and anxiety alleviation, weight-based dosage of drugs such as local anaesthetics, anticoagulants, sclerosants as well as sizing of instruments such as vascular access lines and catheters. A pediatric radiologist’s knowledge of these aspects, as well as comfort and precision when performing procedures in children, is invaluable for ensuring robust and safe procedures without unexpected complications. Rohilla et al. in their study among individuals practising pediatric interventional radiology in North America identified that more than 60% had completed a pediatric radiology fellowship [15]. We must attempt to replicate a similar trend in India as well. The article by Young et al. is an excellent resource for radiologists attempting to begin IR services as part of their pediatric radiology practice [16].
Conclusion
In conclusion, while pediatric radiology in India has grown immensely in the past two decades, there is tremendous potential for further advancement by harnessing the valuable resource of an enthusiastic young workforce of fellowship trained pediatric radiologists coupled with experienced mentors. Efforts are needed at the individual and the national society level to increase awareness, multicentre collaboration and mentoring of smaller institutes.
References
Other Reports. https://www.nipccd.nic.in/other-reports#gsc.tab=0. Accessed 12 May 2024
Sidhu A, Sheikh N, Chavhan G et al (2014) Improving pediatric radiology in India. Pediatr Radiol 44:657–665. https://doi.org/10.1007/s00247-013-2868-x
Therakathu J, Yadav VK, Keshava SN, Gibikote S, Chavan GB, Shroff M (2017) The current status of pediatric radiology in India: A conference-based survey. Indian J Radiol Imaging 27:73–77. https://doi.org/10.4103/0971-3026.202965
ICRI – Indian College of Radiology and Imaging. https://icri.iria.org.in/. Accessed 12 May 2024
Back SJ, Gurian MS, Reid JR, Darge K (2014) How and how well do pediatric radiology fellows learn ultrasound skills? A national survey. Pediatr Radiol 44:1058–1064. https://doi.org/10.1007/s00247-014-2980-6
ISPR | Indian Society of Paediatric Radiology | ispr | paediatric | society |. http://ispronline.in/. Accessed 12 May 2024
AOSPR. https://www.aospr.com/. Accessed 12 May 2024
Society for Pediatric Radiology | SPR. https://www.spr.org/
ESPRESPR. https://www.espr.org/. Accessed 12 May 2024
Offiah AC, Atalabi OM, Epelman M, Khanna G (2024) Disparities in paediatric radiology research publications from low- and lower middle-income countries: a time for change. Pediatr Radiol 54:468–477. https://doi.org/10.1007/s00247-023-05762-y
Offiah AC, Atalabi OM, Epelman M, Khanna G (2024) Disparities in paediatric radiology research publications from low- and lower middle-income countries: Pediatric Radiology editors as advocates. Pediatr Radiol 54:379–380. https://doi.org/10.1007/s00247-023-05784-6
Lu F, Vijayasarathi A, Murray N, Hamid S, Khosa F (2021) Evaluation of Pediatric Radiology Fellowship website content in USA and Canada. Curr Probl Diagn Radiol 50:151–155. https://doi.org/10.1067/j.cpradiol.2020.01.007
Radiology, Fellowships (2024) DMs and Super-Speciality DNBs in India – Cafe Roentgen. https://caferoentgen.com/2020/02/29/radiology-fellowships-dms-and-super-speciality-dnbs-in-india/. Accessed 12 May 2024
Siegel MJ, Bugenhagen SM, Sanchez A, Kim S, Abadia A, Ramirez-Giraldo JC (2023) Comparison of Radiation Dose and Image Quality of Pediatric High-Resolution chest CT between photon-counting detector CT and energy-integrated detector CT: a matched study. AJR Am J Roentgenol 221:363–371. https://doi.org/10.2214/AJR.23.29077
Rohilla M, Wadhwa V, Purushothaman R, Vilanilam GK, Lewis PS, Wong K (2021) Pediatric interventional radiology workforce in North America: a descriptive analysis of demographics, educational backgrounds and scholarly activities. Pediatr Radiol 51:2077–2082. https://doi.org/10.1007/s00247-021-05014-x
Young VA, Thakor AS, Josephs SC (2022) Update on Pediatric Interventional Radiology. Radiographics 42:1580–1597. https://doi.org/10.1148/rg.220019
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhalla, D., Sharma, R. & Jana, M. Current status of pediatric radiology in India: a perspective. Pediatr Radiol (2024). https://doi.org/10.1007/s00247-024-05961-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00247-024-05961-1