Abstract
Paediatric radiology requires dedicated equipment, specific precautions related to ionising radiation, and specialist knowledge. Developing countries face difficulties in providing adequate imaging services for children. In many African countries, children represent an increasing proportion of the population, and additional challenges follow from extreme living conditions, poverty, lack of parental care, and exposure to tuberculosis, HIV, pneumonia, diarrhoea and violent trauma. Imaging plays a critical role in the treatment of these children, but is expensive and difficult to provide. The World Health Organisation initiatives, of which the World Health Imaging System for Radiography (WHIS-RAD) unit is one result, needs to expand into other areas such as the provision of maintenance servicing. New initiatives by groups such as Rotary and the World Health Imaging Alliance to install WHIS-RAD units in developing countries and provide digital solutions, need support. Paediatric radiologists are needed to offer their services for reporting, consultation and quality assurance for free by way of teleradiology. Societies for paediatric radiology are needed to focus on providing a volunteer teleradiology reporting group, information on child safety for basic imaging, guidelines for investigations specific to the disease spectrum, and solutions for optimising imaging in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Developing countries, and in particular those in sub-Saharan Africa, present radiologists and clinicians with substantial challenges when trying to offer paediatric imaging services. Difficulties include cost, patient difficulty in accessing care, a massive disease burden, climate, geographical extremes, poor infrastructure, human resource shortages, and political factors such as instability and migration. Technical solutions have been developed to help overcome some of these challenges, often as a result of collaborative efforts by developing country clinicians, the World Health Organisation (WHO) and non-governmental organisations (NGOs). New technology, often considered too high-tech for resource-limited settings, may in fact provide simplified solutions; an obvious example is digital imaging, which obviates film developing, and allows transfer of images over large distances so that remote experts may offer advice and diagnosis. Radiologists and radiographers can also help overcome the lack of specialised staff by “task shifting” certain skills to non-radiologists/radiographers who may perform radiographs and interpret them where there is a need. Equipment vendors have a responsibility for making cheap and robust equipment available to those countries that cannot afford to pay Western prices and to offer technical assistance in maintenance and repair to less skilled personnel. Governments of developed nations and NGOs can assist, not only financially, but also by investing in human resource development. This paper highlights some of the most important challenges for offering a paediatric imaging service in developing countries, and offers a roundup of new technology and ideas for training that may contribute to resolving some existing issues.
Poverty and access to health
More than 80% of the world’s population live on less than $10 (U.S.) per day [1]. As a result, almost one-third of children in developing countries are malnourished or stunted, with the bulk of affected children living in sub-Saharan Africa and South-East Asia. [2]. Of some 1.9 billion children living in the developing world, more than one-third have inadequate access to shelter, about one in five have no access to safe water, and one in seven have no access to health services [3].
Mortality in Africa
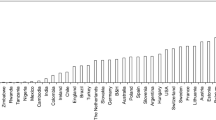
Worldwide, in 2004, 2.6 million deaths occurred in young people between the ages of 10 and 24 years. Of these, 97% were in the developing world [4]. The countries with the top 30 infant mortality rates in the world are all in Africa. Nevertheless, there are stark disparities among countries. Nearly half (44%) of the population of Mozambique is younger than 14 years of age [5], and the mortality rate in children younger than 5 years old is 138/1,000 live births [6]. This contrasts with neighbouring South Africa, a relatively well developed sub-Saharan country, where the corresponding rate is 69/1,000 [6], and only 29% of the population is younger than 14 years of age.
Despite the greater expenditure on healthcare in South Africa compared to Mozambique, the gains in life expectancy and healthy life expectancy have been disappointing [7]. However, the one area where there is a marked difference is in paediatric healthcare and infant mortality. In South Africa, the infant mortality rate is 44/1,000 compared to 106/1,000 in Mozambique. Compounding a higher overall burden of paediatric disease, the HIV epidemic has significantly changed the population pyramids of many African countries, with a dramatic loss of middle-aged individuals who traditionally support both the younger and older subpopulations. HIV has also caused a significant increase in mother-and-child mortality [7].
Disease burden
In 2000–2003, almost three-quarters of the 10.6 million annual deaths in children younger than 5 years were attributable to just six causes: pneumonia (19%), diarrhoea (18%), malaria (8%), neonatal pneumonia or sepsis (10%), preterm delivery (10%), and birth asphyxia (8%). Thus, four communicable diseases accounted for more than half of all child deaths. This pattern was comparable in all regions defined by the WHO, except for malaria, for which almost all childhood deaths occurred in Africa. Under-nutrition was an underlying cause in 53% of all deaths in children younger than of 5 years [8].
In African children, respiratory illness is the most important cause of mortality and morbidity. Pneumonia alone is responsible for approximately 21% of deaths in African children younger than 5 years of age each year. As a result of the HIV epidemic in sub-Saharan Africa, HIV-associated acute and chronic respiratory disease has emerged as a major factor in the epidemiology of childhood respiratory illness, and has increased the incidence, severity and mortality of pneumonia in African children [9].
HIV
According to the WHO AIDS Epidemic Update, in 2008, there were 2.1 million children younger than of 15 years living with HIV worldwide, and 430,000 new infections. In children younger than 15 years of age, 280,000 deaths were attributable to HIV or AIDS. Two-thirds of all HIV infections occurred in sub-Saharan Africa, and 91% of newly infected children were born in Africa. Furthermore, 14 million children in sub-Saharan Africa have lost at least one parent to AIDS. While substantial progress has been made in improving access to antiretroviral therapy, children remain under-served: 44% of the total HIV population has access to antiretroviral therapy, but only 15% of children do [10]. Swaziland has the highest worldwide adult prevalence of HIV at 27%, while South Africa has the largest worldwide population living with HIV at 5.7 million. In South Africa, 29% of females accessing antenatal care are HIV-positive [11], which has an impact on child health by means of vertical (mother-to-child) transmission, and as a result of increased maternal mortality.
Tuberculosis
More than 90% of children with tuberculosis (TB) live in the developing world. Where HIV is prevalent, a dangerous synergy ensues. HIV co-infection has been associated with less successful treatment of TB in children, partly due to social factors (parent illness or death), partly to immuno-compromise [12]. The estimated incidence of TB in sub-Saharan Africa is nearly twice that in South-East Asia, at nearly 350/100,000. Globally, about 1.6 million people died of TB in 2005, with the highest number of deaths and the highest mortality rate in Africa. The TB epidemic in Africa spread rapidly during the 1990s, but has been slowing each year, and the incidence now appears to have stabilised or even decreased in many regions [6]. South Africa has the highest rate of TB in the world at 948/100,000, closely followed by Zimbabwe at 782/100,000. HIV/TB co-infection is common in countries with a high prevalence of HIV, with South Africa, Zimbabwe, Malawi and Botswana all reporting an HIV prevalence >50% in people infected with TB. The global number of HIV-positive patients with TB in 2005 was 1.39 million with over three-quarters (79%) of these living in Africa and almost one-third (31%) of these African cases being reported in South Africa [13].
Trauma
In Africa, trauma is the third commonest cause of death. In children, trauma is less common than infection, infestation and malnutrition. There is a 7.5% mortality rate from trauma, which is almost entirely accounted for by burns (75%) and road traffic accidents (25%). The commonest injuries are fractures due to falls (45%), and burns (32%) [14]. Other common mechanisms of injury are pedestrian motor vehicle accidents (34%) and inhalation burns (36%) [15]. Investment in trauma prevention is disproportionately low. For example, in 2006–2007, the WHO allocated less than 1% of its annual budget to work-related to injuries and physical violence (worldwide) [16].
Barriers to radiology in developing countries and some solutions
One-fifth of the world’s population does not have access to water, with the majority concentrated in the developing world [17]. For example, in Mozambique, only 57% of the population has access to water services, and in rural areas only 25% of the population receives water at home [18]. Water is a basic requirement for hospitals, and it is important in film development and processing in radiology services. Water is a key component in developer solutions (manual and automatic) as it acts as a solvent and forms an important component of processing tanks (Fig. 1). A good water supply and drain is therefore essential for any darkroom [19]. With many areas in developing countries having an inadequate water supply, a method of instantaneous drying processing seems a reasonable alternative [19, 20], and computed (CR) or digital radiography (DR) installations may present the best modern solutions.
Access to electricity is fundamental to hospital infrastructure. Many rural hospitals have an unreliable supply of electricity [19]. For example, hospitals may only have access to electricity for brief periods in the evenings because of the cost of fuel [19, 21]. In radiology, electrical power is normally used to operate the X-ray unit and X-ray processing tank refrigeration units [22]. The WHO has recommended X-ray equipment with an independent power source [19, 23]. Two X-ray units, the WHO Basic Radiological System (WHO-BRS) and the World Health Imaging System for Radiography (WHIS-RAD), were developed as battery-operated units to overcome this problem [19, 24]. Electricity supply is also often prone to power surges and variations in voltage. Surge protectors and voltage stabilisers should therefore be included to protect radiological equipment [25]. Overloading systems using custom-made equipment is a recurrent problem that runs the risk of complications, such as equipment meltdown and fire (Fig. 2).
The lack of water and electricity is generally coupled with a lack of public infrastructure such as roads and railway links [26]. These are important in any health infrastructure as they allow access to hospitals, transport of equipment and consumables and, in the case of imaging, access for companies that provide maintenance of radiological equipment. Embedded service contracts exist where equipment is designed specifically for regular servicing [26]. Accessibility to rural areas that do not have public infrastructure may prove too costly for suppliers of sophisticated equipment. The WHO-BRS was designed to meet criteria of low maintenance, easy operability and cost-effectiveness [27]; the only parts that require maintenance on the WHIS-RAD are the X-ray tube, the generator, and the light-beam collimator [28]. Some CR readers have been built purposely to be light and can be sent for repairs by freight as complete units.
Developing countries also experience extremes of climate, which may affect equipment. The average temperature in Mozambique is 23°C, with the temperature reaching 30°C in summer. The average annual relative humidity is 63% [29]. This is important because, in high temperatures, algae can build up in processors and cause malfunction [25]. When not properly controlled, temperature and humidity will have adverse effects on the film and the worker. Humidity should be maintained at 40–50% and temperature at 19–28°C for film to remain usable [22]. High temperatures damage the emulsion, causing fogging and loss of contrast. Sealed containers can protect film from moisture to a degree. Processing solutions must also be kept at an optimum temperature of 20°C. Compensation for temperature variations is by increasing or decreasing the time of development. Temperatures below 16°C inhibit the reducing agent activity, and high temperatures produce underdeveloped, fogged radiographs, emphasising the need for adequate ventilation [22].
Access to radiology and hospital services
Only 220 million people in the developing world have access to a basic radiological service. The WHO recommends a three-tiered imaging service pyramid consisting of basic radiological services (BRS) providing uncomplicated examinations, general purpose radiological service (GPRS) providing a backup service for BRS, and a specialised radiological service (SRS) that provides specialised procedures [30]. However, this model does not currently exist in many developing countries.
In many instances, the private sector will have state-of-the-art hospitals and specialised imaging equipment serving only a small percentage of the population [26]. South Africa’s healthcare system is an example of such technological inequalities. South Africa has an under-resourced and overused public sector that delivers services to 80% of the population, as well as a highly developed private sector that serves the health needs of 20% of the population. There are currently 200 private hospitals in urban South Africa that are equipped with state-of-the-art radiological equipment [31].
Modern nephrology is an example of a clinical paediatric service that has become highly dependent on radiology for diagnosis and therapy. Nephrologists’ requirements for diagnostic modalities, range from BRS to advanced SRS, as summarised in table 1 [32].
Human resources
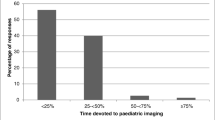
As expected, countries with well-established and functional training and examination centres, such as South Africa (eight training centres including the University of Cape Town and the University of the Witwatersrand training complexes) and Kenya (notably the Aga Khan University Teaching Hospitals), have the most radiologists. South Africa is the best-staffed country in sub-Saharan Africa, with 497 registered radiologists and 685 radiographers, a strong and active radiological society (RSSA), a strong radiographic society (SORSA), and an independent examining body (the College of Radiologists). In 2008, Kenya had 248 radiologists. There are established training programs for radiologists in East Africa (Cameroon, Ghana, Nigeria, Sierra Leone), East Africa (Kenya, Tanzania, Uganda) and Southern and Central Africa (South Africa, Zimbabwe, Mauritius, Mozambique) [33]. However, 14 African countries have no radiologist and most have fewer than 30. For example, Malawi has only one radiologist serving a population of more than 15 million. According to one review, the ratios of radiologists-to-population in African countries are: Tanzania 1:1.5 million; Uganda 1:1 million; Kenya 1:400,000; South Africa 1:100,000 [35]. In comparison, in the United States, Europe and Canada, the ratio is approximately 1:50,000.
In settings with few practitioners and a massive disease burden, the radiological workload is staggering. Table 2 summarises and compares the workload in two African countries with those in the United Kingdom, the United States and New Zealand. The figures suggest that South Africa is over staffed. These data, however, do not take into account the massive discrepancies between the public and private sector staffing [31]. For example, in a survey of the Western Cape of South Africa in 2008, the public service had 36 consultants (excluding registrars) for 607,671 patients imaged (1:16,879 per year), and private practice had 76 consultants for 590,835 patients (1:7,774 per year) [36]. Only 10 of the 36 public hospitals in the Western Cape had consultants available on the premises; 26 hospitals had no experts available at all, and examinations were either interpreted by the referring clinician, or referred for expert opinion at larger or academic hospitals. Private radiology practices had more than double the number of consultants per hospital compared to the public sector (2.6 versus 1.1), although government services handle the majority of investigations [36]. The number of radiographers, however, was relatively evenly distributed between the private and public sectors (7.2 per public hospital; 8.2 per private hospital), with an even workload [36]. This supports the idea of capacitating radiographers as much as possible as principal providers of radiological services.
Equipment
The WHO recommends that small hospitals with one doctor should have basic imaging equipment [24]. This includes simple radiographic and US equipment that should be available at least to all sick and injured children [24].
Since the 1960s, the WHO has tried to overcome imaging problems in developing countries by developing a basic radiological system, which evolved into the WHO-BRS [37]. This consisted of a reliable X-ray machine and three manuals covering radiographic technique, film processing and image interpretation [19, 37]. The machine comprises a generator, X-ray tube, high-quality focused grid and a “C-arm” type tube stand for use in areas with poor electricity supply and poor access to technical services [37].
The WHO-BRS was replaced by the WHIS-RAD in 1995 complying with specifications as set out by the WHO. The WHIS-RAD has the highest possible radiation safety and is thus suitable for use in children [24]. It can be operated on batteries, capacitors or solar cells and has a simple maintenance plan [38] (Figs. 3 and 4). A digital version of WHIS-RAD is available using digital technology and may be a future solution for many countries, enabling instant reporting via teleradiology services and eliminating the need for film development and processing (Fig. 5).
Mobile radiography is a tantalising alternative because of low price and mobility. These units are designed for use in patients who cannot be moved from their hospital beds, such as in intensive care units [39]. Numerous NGOs working in developing countries (including the World Health Imaging Alliance, WHIA) do not support the use of mobile units as they depend on expert users (trained radiographers) owing to the variety of adjustments that need to be made. Some mobile units are cheap, making them attractive to developing countries, but these are often underpowered and restricted to performing appendicular skeletal radiographs.
The cost of technology is a major barrier to obtaining quality equipment [21]. An assessment of equipment prices in Kenya in 2008 showed that low-end US scanners cost approximately (in U.S. dollars) $20,000, compared to $150,000 for a high-end unit; low-end radiography units, $40,000, high-end, $250,000; and CT, $200,000 [34]. The major disadvantage of the WHIS-RAD machine is that it remains expensive [38]. Preferentially priced WHIS-RAD units have been made available to NGOs at approximately $36,000 in 2009 without inclusion of an accompanying digital system (additional $36,000; personal communication, Médecins sans Frontières).
It is also noted that well-intended donations of old pieces of equipment from developed-world hospitals often arrive in African institutions without a repair manual, no maintenance contract, no staff training, and no reagents. When these units break down, they are left unused.
Kenya has a relatively well-developed health system with both private and public sectors, and with radiologist training schemes. As expected, there is more radiological equipment in private than in public facilities, and more in the capital Nairobi than in rural areas. On average, there are two X-ray and two US systems per public hospital in Nairobi; four X-ray and three US units per hospital in the private sector. In the outer districts, there is only one US and one X-ray unit for three hospitals in public hospitals, compared with at least one US and one X-ray unit per private hospital. A survey in Kenya found that six out of ten hospitals had a single-slice CT scanner and only five had multi-detector row scanners [34].
Malawi, one of the poorest countries in southern Africa, has only two CT scanners (one in the public sector) in the entire country. An MRI scanner has recently been installed for research purposes but also serves private and public patients.
Safety and other minimum requirements of the X-ray room
Even where resources are restricted, safety should be a primary concern. The WHIS-RAD system developed by the WHO is self-shielding and may not require complete room preparation. In all situations however (except possibly with slit beam technology), X-ray units should be housed in a dedicated room, ideally situated on the ground floor and designed so that access is exclusively for those performing the procedure, and for referred patients. There should be internationally understandable warning signs and a warning light outside to prevent unauthorised or inadvertent entry. An engineer should plan the room by performing calculations of the radiation dose that will be received by bystanders outside the room according to workload and occupancy.
Options for the structure of the walls include either solid 23-cm thick clay brick or, in the case of other brick types and dry walls, the addition of 2-mm lead sheeting. In developing countries, a cheaper alternative to lead-lining is barium plaster of 6-mm thickness (1 part barium plaster, 1 part barium sulphate, 1 part concrete). The lead lining (or alternative) must rise 2.2 m from the floor. The floor partitions must be made of concrete >15 cm thick. The door should preferably be a sliding door with 10-cm overlap, positioned away from the X-ray unit, and lined by a lead sheet of 2 mm. Protective barriers must be designed to be effective and must contain a lead-lined glass window to allow the radiographer to watch the patient’s position, immobilisation and inspiration. Even these simple building requirements may be unachievable in remote resource-deprived locations.
Patients in developing countries are not usually educated about the risks of ionising radiation to themselves, their children, or their unborn children. Radiographers are often not formally trained and therefore lack knowledge in physics and safety. It is therefore paramount that all staff members are made aware of such risks, and in particular about the increased risk in children.
Staff monitoring proves to be a challenge in developing countries. While film badges are relatively robust and cheap, remote areas lack the facilities for reading these, and they have to be sent off for reading. Ensuring that monitoring devices are used and worn appropriately is also a challenge for primary care facilities with no trained radiation supervisors. Thermoluminescent dosimeters are currently expensive and too fragile for use in extreme environments, but may be an option as on-site reading is possible. Visits to imaging sites by a biomedical engineer, a superintendent radiographer or a radiologist can ensure that radiation safety practices remain in place and are diligently adhered to.
Teleradiology
While teleradiology is flourishing in the developed world, few teleradiological links have been made to the developing world. Barriers to the implementation of radiology services in general also complicate setting up reliable links [40]. Examples of simple, low-cost solutions have been employed by the Swinfen Charitable Trust and by AED-SATELLIFE. Swinfen gives healthcare personnel in remote places, Internet access and a digital camera, and facilitates a low-cost telemedicine service linking doctors at hospitals in the developing world with medical and surgical consultants who give advice at no cost. Local doctors can send clinical photos, medical histories and any other relevant material (such as radiographs). Currently, the Swinfen group allows doctors in 181 remote hospitals immediate access to 458 consultants covering all medical and surgical specialties [41]. However, only a minority of the work done by the Swinfen group would be classed as teleradiology. AED-SATELLIFE (formally known as SATELLIFE) was the first non-profit organisation to own and use a low earth-orbit satellite [42]. AED-SATELLIFE makes use of mobile computing devices such as handheld computers and mobile phones for data communication. Again, teleradiology is only a small part of the work done by this group.
More complex solutions are also beginning to emerge. A tele-US system for real-time imaging in resource-limited settings is now possible [43]. Using open-source software and commercial off-the-shelf hardware, a remote US technician can be connected to a radiologist. Another recent initiative has been Téléradiologie sans Frontières (TSF; Teleradiology without Borders), a Luxembourg-based enterprise involving expert radiologists and high-end technology based on a Power Server PACS system developed and donated by RamSoft [44]. Using a standard computer, users log on to WEB-PACS over the Internet. Images are transmitted to the data centre at the push of a button, and radiologists interpret images sent to them. Everything is stored centrally, and available online. If a computer is lost or damaged, it is easy to recover the images with any other computer using a web browser. Thanks to TSF’s WEB-PACS, large files need no longer be split. The PACS enables the smooth transmission of large files that upload in the background, often while readers are completing their normal workload. This also helps to avoid the disadvantages of hardcopy storage and retrieval, which is time- and space-consuming (Fig. 6). Plain radiographs can also be photographed and recreated in JPEG (Joint Photographic Experts Group) format [45, 46]. JPEG images can then be converted into DICOM (Digital Imaging and Communication in Medicine) format; a PACS conversion facility is essential to the process. There is no charge for the remote reading service, which is currently available in parts of Francophone Africa. Established private teleradiology practices such as Nighthawks are also involved in pilot programs with NGOs reporting radiographs from rural health centres, free of charge [47].
NGOs and outreach programs
The care for patients in remote, underdeveloped, and sometimes dangerous, regions is often left to NGOs, who have the will and means to assist those in need without any personal gain. Médecins sans Frontières (MSF; Doctors without Borders) is an international humanitarian aid organisation that provides medical assistance to populations in need in more than 70 countries, 36 of these in Africa [48]. While the initial focus of MSF was emergency response to natural and man-made disasters, armed conflict and epidemics, medical activities have expanded to include long-term care for children with malnutrition, TB, HIV, and a variety of endemic diseases. Radiography has become an increasingly important component of the medical care that MSF provides, supporting TB and surgical (in particular orthopaedic) programmes, and obstetric care [48].
Traditionally, MSF relied on local ministries of health or private hospitals and clinics to provide imaging services (Fig. 7). As the organisation’s ambitions evolved to provide increasingly complex health interventions, MSF has funded radiographic and US equipment for individual programs depending on need. In 2009, MSF owned 20 X-ray units and used a further 30 belonging to ministries of health world-wide. In addition, it owned 24 US units and used a further 12 worldwide with two consultant radiologists offering teleradiology consultation and visits to individual projects on request. The WHIS-RAD unit and the accompanying manuals have been adopted by MSF as the radiography system of choice. The world-wide availability of the internet makes teleradiology consultation a realistic possibility. For MSF facilities, computed radiography systems are therefore recommended over the use of film-screen radiography to take advantage of opportunities for teleradiology consultation. At MSF facilities that have access to only film screen radiography, films are photographed with digital cameras for use in teleradiology [45, 46].
The MSF experience in Liberia is a good example of the use of digital radiography in paediatric care. In response to 14 years of civil war, MSF has provided medical aid in Liberia for more than 20 years in several locations including hospitals and clinics for adults, children, and obstetric care. In support of a TB program for children run by MSF, the Island Paediatric Hospital in Monrovia served as the site of the first installation of a fully digital X-ray unit based on the design and specifications of the WHIS-RAD. The protracted conflict in Liberia led to the emigration of many healthcare professionals, including physicians, nurses, and radiographers, from the country. With no experienced radiographers to choose from, MSF hired two highly motivated young men with twelfth-grade education, limited experience with computers, and no medical training, to serve as radiographers. With the simplified design of the WHIS-RAD and use of the well-illustrated WHO manual on positioning, projections and technique, both became highly competent. The prototype fully digital unit produces a high-quality diagnostic image on the computer monitor within 5 s of the exposure.
Interpretations were initially provided by the MSF expatriate and national physicians, physician assistants, and nurses caring for the patient. In December 2008, a trial teleradiology consultation service was begun between the Island Hospital site and a University of Virginia radiologist in the United States (W.E.B.). The digital X-ray unit allowed the easy download of radiographic images in JPEG (or a variety of other) image formats. A slow internet connection was available at the MSF office across the road but was not available in the hospital itself. MSF healthcare providers would download images in compressed JPEG format to a portable hard drive, walk across the road, access a computer, and send the images as an email attachment to the radiologist in the United States. The email would contain brief clinical and laboratory information, and the working diagnosis. The image attachments were 200–300 kilobytes, easily transmitted even with very slow internet connections. The radiologist usually received the images within 1–4 h of the exposure. The image quality was judged to be diagnostic in almost every case. The radiologist’s findings, interpretation, and diagnosis were returned to the sender by email usually within 2–6 h, maximum 12 h, of the exposure. During the 17-month trial period, over 250 teleradiology consultations were provided to a total of 13 healthcare providers at the MSF Island Hospital site. A brief survey of seven of the MSF expatriate physicians involved in the teleradiology project found that teleradiology consultation routinely strengthened their clinical diagnosis and often significantly changed the clinical diagnosis and treatment. An illustrative case example is provided (Fig. 8). In the spring of 2010, MSF turned over the last of its hospitals in Liberia to the Ministry of Health, donating much of its remaining equipment including the installed radiographic unit at Island Hospital.
Primary tuberculosis. An 18-month-old Liberian boy presented with malnutrition, weight loss and cough. The chest radiograph shows consolidation of the left upper lung. Distinct narrowing of the left bronchus (arrow) strongly suggests peribronchial lymphadenopathy in primary tuberculosis. The patient improved significantly after 2 months of anti-tuberculous treatment
In South Africa, MSF offers dedicated imaging services to children with drug-resistant TB with attending specialists’ services. Other NGOs, such as the Baylor School of Health, offer paediatric services in rural parts of developing countries. One such program in Swaziland attends to paediatric patients, particularly those with HIV and TB [49] (Fig. 9).
Another excellent example of an NGO focusing on supplying WHIS-RAD equipment coupled with computed radiography and teleradiology for remote and poverty affected areas, is the WHIA. The WHIA promotes the use of WHIS-RAD X-ray systems with digital technology. It partners itself with the Rotary, which raises funds for qualifying clinics [50]. At Crossroads clinic in the Western Cape of South Africa, WHIA collaborates with the University of Cape Town and the University of Virginia to develop a digital solution for WHIS-RAD in developing countries.
Other NGOs also provide varying levels of education, equipment, and maintenance support in Africa. The Radiological Society of North America (RSNA), through its Committee on International Relations and Education (CIRE), has for many years sponsored long- and short-term visits to African countries by international visiting professors specifically chosen for their expertise. Host countries invite requests from visiting professors with specialised skills such as paediatric radiology. The CIRE then matches volunteer professors’ expertise to the expressed needs of the host country. The professors may visit and teach for periods of from 2–3 weeks to up to 6 months, or even a year.
The American College of Radiology (ACR) has recently developed the ACR Foundation International Volunteer System to provide assistance in developing radiology in countries outside of the United States. The foundation serves to match donors and facilities with their needs and supplies. Services include the exchange of ideas, materials, equipment and time, and financial support. The major goals of the foundation are to improve radiology in developing countries and to promote international and community service participation by member of the ACR.
Image interpretation
Owing to the dire shortage of radiologists in Africa, clinicians generally, despite little training, read their own radiographs and perform their own US scans, especially in district obstetrics clinics.
MSF runs image interpretation courses as part of its HIV training school in South Africa. A paediatric radiologist (S.A.) teaches groups of five to ten clinicians who work in remote HIV clinics across southern Africa. The course is run six to eight times a year and includes lectures on reading a radiograph, diagnosing tuberculosis, and imaging appearances in children with HIV. Other MSF courses are run in the field in makeshift teaching environments (Fig. 10). Radiographers offer a viable solution for interpreting radiographs as they are trained in anatomy and technology. Most importantly, they are on site at the time of producing the radiograph or other imaging. “Red dot” systems have been in practice for some time where radiographers indicate any suspected radiographic abnormality by applying a red sticker onto the hard copy. This has evolved into a radiographer pattern recognition-program with radiographer reporting [51] (Fig. 11). Dedicated CT radiographers without training in CT image interpretation have been tested for their ability to detect CT abnormalities by years-of-experience, and they demonstrated a high accuracy with increasing experience [52].
One radiographer training program comprises a series of three intensive 2-week courses including lectures and small group tutorials along with film-reading assessments. The course was aimed at radiographers who had completed a 3-year diploma in radiography. The course evaluation found that people who were taking X-rays but were not trained radiographers, gained little from the course as they lacked the necessary background knowledge; follow-up visits showed variable use of the new skills, depending on the amount of support graduates received from their local clinicians. The success of the partnership between the radiographer and the (often quite junior) doctor, who could learn together by discussing each case, depended on the personalities involved, but all course graduates were encouraged to start writing reports to develop their skills, and to advertise the service they could provide. An annotated and indexed computer presentation with voiceover has since been prepared, and it contains more than 800 slides with more than 2,000 high-quality illustrations. It will soon be available through the International Society of Radiographers and Radiation Technologists [53]. Of the 22 chapters, 3 are devoted to the chest, the abdomen and the skeletal system in children.
Tick-sheet reporting cards have been created for interpreting paediatric radiographs and have been introduced by MSF and by X-ray readers in the South African TB Vaccine Initiative (SATVI) with some success [54]. These have the advantage of standardising reading and indicating a level of importance for radiographic findings for example in diagnosing primary TB in children (Fig. 12).
Numerous WHO guidelines and other materials are available to assist health workers without any training in performing and interpreting basic radiographs. However, the effectiveness of such approaches has not been evaluated. Available WHO manuals are based on film-screen radiography, and these must be revised with regard to machine settings for computed or digital radiography use. Some of these books, in particular the paediatric examination manual, have proved difficult to obtain (Table 3; Fig. 13).
Political and professional obstacles
The South African experience demonstrates how socio-political factors can be major stumbling blocks for achieving fair access to healthcare in developing countries (Fig. 14). Although South Africa has seen a significant transformation of society and its institutions since the 1994 political turnover, inequalities remain. The pre-1994 South African health system was characterised by racial segregation, where the facilities and services for blacks were vastly inferior to those for whites. This was achieved partly through unequal funding. In 1985, per-capita spending on healthcare was over three times greater for whites (20% of the population) compared to blacks. Even ambulances were segregated; if an ambulance of the “wrong colour” arrived at the scene of an accident, the driver would leave and another ambulance would have to be summoned, sometimes with fatal consequences [55].
A slum in the outskirts of Cape Town, South Africa, which arose due to restrictions of residential areas, has poor access to healthcare for the majority of the population, but there are good roads for access to the nearby city centre, reliable electricity, as well as trained personnel nearby. Persuading radiologists to work in a slum is difficult, making a case for teleradiology. The spectrum of disease in African slums includes tuberculosis, HIV, pneumonia, diarrhoea and traumatic injury
Government policy severely hindered blacks from attending white medical schools and treating white patients. As a result, between 1968 and 1977 only 3% of newly qualified physicians were black [55]. This continues to be a major contributor to inadequate training of healthcare professionals and an obstacle to meeting the needs of the country, particularly the majority rural population. The problems are exacerbated by a continuous brain-drain as a result of active recruitment of South African physicians to meet rural and remote needs of developed countries thus undercutting South Africa’s attempts to solve its own shortage [56].
The South African medical profession itself played a role in perpetuating the racially segregated healthcare. The failings of the medical profession revealed at the Truth and Reconciliation Commission hearings can be divided into two categories: toleration of, or active promotion of, inequities in healthcare and complicity in gross violations of human rights [55, 57]. This included remaining silent about “race-based public policies affecting the medical profession, the restriction of medical school admissions on race, segregation of hospitals and other health facilities and the maintenance of separate waiting rooms by members of the profession” [56]. It should however be noted that the profession has been one of the more active participants in the transformation of South African society during the last decade.
Price [58] argues that these policies could not be adequately explained merely as symptoms of the differential access to political and economic power but that health services were also instruments of the state in achieving apartheid goals, i.e. reproducing the conditions of capitalist accumulation and maintaining white supremacy. In this context, children are always victims, as they neither support nor oppose political ideals or power groups.
The history of South Africa’s health system under apartheid serves to highlight the fact that access to essential health services, including radiology, is not just a technical challenge, but that political policies create inequalities that act as barriers to care that may perpetuate for generations.
Conclusion
Many of the problems and solutions discussed in this paper are relevant both for adults and children. However, when considering that paediatric radiology requires dedicated equipment, specific radiation safety considerations, and specialist knowledge, one can see how developing countries with the general difficulties described would be hard-pressed to provide an adequate, if any, children’s imaging service. Population pyramids in Africa show that children are forming the bulk of the population, especially where HIV is creating many orphans who are subject to extreme living conditions, poverty, lack of parental care, and exposure to diseases such as tuberculosis, HIV, pneumonia and diarrhoea, and are subjected to violence and other trauma. Imaging should play a critical role in the medical treatment of these children, but it is expensive, difficult to provide, and challenging to maintain. WHO initiatives such as production of the WHIS-RAD unit are needed to continue into other areas such as the provision of maintenance and servicing, while new efforts by NGOs to install WHIS-RAD units in developing countries and providing modern digital solutions need support. Paediatric radiologists are needed to offer their services for reporting, consultation and quality assurance via teleradiology. This could be offered from the comfort of their practices and homes for free. Those with grander humanitarian aspirations could join groups such as MSF to offer on-site training and support the production of teaching materials that could help form a radiological workforce.
As paediatric radiologists, our focus should be on providing volunteer teleradiology reporting, information on child safety under basic imaging conditions, guidelines for appropriate investigations specific to the disease spectrum of developing nations, and solutions for optimised imaging. Our professional societies need to call out to their members for volunteers, make their societies’ aspirations known to NGOs and other concerned groups, and then organise useful outreach teams to act now.
References
Chen S, Ravallion M. The developing world is poorer than we thought, but no less successful in the fight against poverty, Policy Research Working Paper 4703, World Bank, August 2008. http://econ.worldbank.org/external/default/main?pagePK=64165259&piPK=64165421&theSitePK=469372&menuPK=64216926&entityID=000158349_20100121133109. Accessed 5 October 2010
2007 Human Development Report (HDR), United Nations Development Program, November 27, 2007 / 2008, p.25. http://hdr.undp.org/en/media/HDR_20072008_EN_Complete.pdf. Accessed 5 October 2010
State of the World’s Children, 2005, UNICEF. http://www.unicef.org/sowc05/english/sowc05.pdf. Accessed 5 October 2010
Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM, Bose K, Vos T, Ferguson J, Mathers CD (2009) Global patterns of mortality in young people: a systematic analysis of population health data. Lancet 374:881–892
The World Factbook. https://www.cia.gov/library/publications/the-world-factbook/geos/mz.html. Accessed 5 October 2010
World Health Organisation. http://www.who.int/countries/. Accessed 5 October 2010
Zanoni B (2005) Epidemiology of HIV in Southern Africa. Pediatr Radiol 39:538–540
Bryce J, Boschi-Pinto C, Shibuya K, Black R (2005) WHO Child Health Epidemiology Reference Group. Lancet 365:1147–1152
Zar HJ (2006) Global paediatric pulmonology: out of Africa. Paediatr Respir Rev 7:S226–S228
WHO AIDS epidemic update UNAIDS/09.36E / JC1700E (English original, November 2009). http://data.unaids.org/pub/Report/2009/JC1700_Epi_Update_2009_en.pdf. Accessed 5 October 2010
Women and Children in South Africa. http://www.unicef.org/southafrica/children.html. Accessed 5 October 2010
Adams LV (2004) Childhood tuberculosis in the developing world. Pediatr Ann 33:685–690
WHO Report. Global tuberculosis control. http://www.who.int/tb/publications/global_report/2009/pdf/report_without_annexes.pdf. Accessed 5 October 2010
Ng’ambi TM, Borgstein ES (2005) Epidemiology of paediatric trauma admission at Queen Elizabeth Cebtral Hospital, Blantyre. Malawi Med J 17:5–6
Osinaike B, Amanor-Boadu S. Paediatric trauma admissions in a Nigerian ICU. Internet Journal of Emergency and Intensive Care Medicine. http://www.ispub.com/ostia/index.php?xmlPrinter=true&xmlFilePath=journals/ijeicm/vol9n2/icu.xml. Accessed 5 October 2010
Stuckler D, King L, Robinson H, McKee M (2008) WHO's budgetary allocations and burden of disease: a comparative analysis. Lancet 372:1563–1569
Dept. of Int. devt.(2001) Access to water in developing countries. http://www.parliament.uk/documents/post/pn178.pdf. Accessed 19 December 2009
Mozambique.http://www.citizen.org/cmep/Water/cmep_Water/reports/safrica/. Accessed 19 December 2009
Palmer PES (1985) The WHO basic radiological system. Radiography 53:170–178
Krupinski EA (1996) Clinical Assessment of dry laser-processed film versus traditional wet-processed film with computer tomography, magnetic resonance imaging, and ultrasound. Acad Radiol 3:855–858
Kozilainin, H (2001) Rehabilitation of hospital infrastructure in a developing country. World Hospital Health Serv 37:28–8,34,36
US Army medical department centre and school. X-ray film processing.http://milmed.pmk.ac.th/MD0954%20X-RAY%20FILM%20PROCESSING.pdf. Accessed 3 January 2010
Korolev A I (1990) Equipment for fast radiography with diffusion-transfer photographic materials. (translated from Russian) Meditsinskaya Tekhnika1:25–27
McHugh K (2002) Essential imaging facilities. In: Southall DP, Coulter B, Ronald C, Nicholson S, Parke S (eds) International child health care: a practical manual for hospitals worldwide. Child Advocacy International. BMJ Books, London
Advice on Donating Equipment Overseas. http://idcsig.org/page6.html. Accessed 22 December 2009
Malkin AA (2007) Design of healthcare technologies for the developing world. Annu Rev Biomed Eng 9:567–587
Kitonyi JM (1993) The basic radiological system experience in Kenya. East Afr Med J 70:793–796
The World Health Imaging System for Radiography—WHIS-RAD: simply perfect. World health Organisation, Geneva, 2004
What Is The Climate, Average Temperature/ Weather In Mozambique? http://www.climatetemp.info/mozambique/.Aceesed 21 December 2009
Brederhofs J, Raceveneau (1982) Radiological services throughout the world. Diagn Imaging 51:121–133
Health care in South Africa http://www.southafrica.info/about/health/health.htm Accessed: 3 January 2010
Urinary tract infection in children: diagnosis, treatment and long-term management. NICE clinical guideline 54. http://www.nice.org.uk/nicemedia/pdf/CG54NICEguideline. Accessed 5 October 2010
Frost and Sullivan (2008) Strategic Analysis of the Medical Imaging Market in Kenya. http://www.pharmaceutical-market-research.com/publications/medical_devices/strategic_analysis_medical_imaging_market_kenya.html. Accessed 5 October 2010
Kawooya M (2008) Role Extension for the Radiographer in the New Millennium. http://www.isrrt.org/images/isrrt/09H50%20DR%20M%20KAWOOYA%20RM%201A%20SESSION%201%20FRIDAY.pdf. Accessed 5 October 2010
www.medpages.co.za. Accessed 5 October 2010
Strachan M (2009) Imbalance between public and private radiological services in the Western Cape Of South Africa. Dissertation University of Stellenbosch, South Africa
Hanson GP (1988) Essential X-ray services: the basic radiological system (BRS). Trop Geogr Med 40(4):s576–s578
Health systems http://www.who.int/topics/health_systems/en/.Accessed 5 January 2010
Simpson PD (1998) A study of chest radiography with mobile units. Br J Radiol 71:640–645
Wootton R (2001) Telemedicine and developing countries—successful implementation will require a shared approach. J Telemed Telecare S1:1–6
http://www.swinfencharitabletrust.org/. Accessed 5 October 2010
http://www.healthnet.org/. Accessed 5 October 2010
Pyke J, Hart M, Popov V et al (2007) A tele-ultrasound system for real-time medical imaging in resource limited settings. In: Conference Proceedings of the IEEE 2007:3094–3097
http://www.teleradiologie-sans-frontieres.org/. Accessed 7 October 2010
Szot A, Jacobson FL, Munn S, Jazayeri D, Nardell E, Harrison D, Drosten R, Ohno-Machado L, Smeaton LM, Fraser HS (2004) Diagnostic accuracy of chest X-rays acquired using a digital camera for low-cost teleradiology. Int J Med Inform 73:65–73
Corr P, Couper I, Beningfield SJ, Mars M (2000) A simple telemedicine system using a digital camera. J Telemed Telecare 6:233–236
http://www.nighthawkradiology.net/. Accessed 5 October 2010
http://www.doctorswithoutborders.org/news/article.cfm?id=4157. Accessed 5 October 2010
Baylor College of Medicine. International Paediatric AIDS Initiative. http://www.Bayloraids.org/programs/Swaziland/outreach.php. Accessed 5 October 2010
Rotarians assess need for WHIS-RAD imaging system in Zimbabwe. http://www.auntminnie.com/index.asp?Sec=nws&sub=rad&pag=dis&ItemId=53004Accessed 3 January 2010
Rudd PD (2003) The development of radiographer reporting 1965–1999. Radiography 9:7–12
Brandt A, Andronikou S, Wieselthaler N, Louw B, Kilborn T, Dekker G, Bertelsman J, Dreyer C (2007) Accuracy of radiographer reporting of paediatric brain CT. Pediatr Radiol 37:291–296
Cowan I, Smith T, Nakabea P, Ajibulu O, Hennessy O (2007) WHO/RANZCR/ISRRT. Developing the image interpretation skills of South Pacific radiographers: a joint WHO/RANZCR/ISRRT project. Australas Radiol 51:527–531
Andronikou S, Vanhoenacker FM, De Backer AI (2009) Advances in imaging chest tuberculosis: blurring of differences between children and adults. Clin Chest Med 30:717–744, viii
Williams JR (2000) Ethics and human rights in South African medicine. CMAJ 162:1167–1170
Sullivan P (1999) Canada a prime destination as MDs flee South Africa. CMAJ 160:1615–1616
Truth and Reconciliation Commission of South Africa Report. Cape Town: TRC/Juta; 1998. vol IV, chapt V. p. 120. www.polity.org.za/govdocs/commissions/1998/trc/index.htm. Accessed August 2010
Price M (1986) Health care as an instrument of apartheid policy in South Africa. Health Policy Plan 1:158–170
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Andronikou, S., McHugh, K., Abdurahman, N. et al. Paediatric radiology seen from Africa. Part I: providing diagnostic imaging to a young population. Pediatr Radiol 41, 811–825 (2011). https://doi.org/10.1007/s00247-011-2081-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-011-2081-8