Abstract
Giant cavernous malformations are rare. There are 17 cases reported in the literature, eight of them in children. Although cavernous malformations have typical imaging findings, the diagnosis of giant cavernous malformation can be challenging because of its large size and varied appearance. It can be more challenging when imaging reveals multilobular involvement and a focal infiltrative pattern mimicking malignancy. We report a case of a giant cavernous malformation with multilobular involvement and a focal infiltrative pattern.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cavernous malformations of the central nervous system are clinically and angiographically occult vascular lesions. They are usually asymptomatic but can cause neurological symptoms such as seizures. Their behavior can be dynamic, with change in size and the appearance of new lesions [1]. The imaging findings of a cavernous malformation typically include a well-circumscribed lobulated mass with a central reticulated core caused by hemorrhage of various ages. Giant cavernous malformations (GCM) are rare, and because of their large size and varied imaging findings, the diagnosis can be challenging, particularly when they show multilobular involvement and a focal infiltrative pattern. We report a 14-year-old boy who had a GCM with a focal infiltrative pattern.
Case report
A 14-year-old boy presented with numbness and involuntary tremor of the right hand. For 4 months he had had one or two seizures a day, with loss of consciousness. Neurological examinations were normal, with intact sensory and motor functions and full GCS scores (6M 5V 4E) on admission. There were no abnormal laboratory findings.
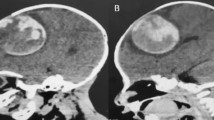
On brain CT images there was a huge well-defined solid and multicystic mass in the temporoparietooccipital lobe, measuring about 13.8 cm in the AP plane, 7.8 cm in the transverse plane, and 8.3 cm in the craniocaudal plane. Most of the solid portion was covered with dense nodular calcifications, and the remaining portions revealed heterogeneous isoattenuation to moderate/high attenuation. On images after administration of contrast agent, minimal enhancement was noted. There was calvarial remodelling on the ipsilateral side of the mass revealed as thinning of the calvaria (Fig. 1). Brain MRI also displayed a huge solid and cystic mass in the temporoparietooccipital lobe. The solid portion showed heterogeneous signal intensity with dark and high-signal dots on T2-weighted (T2-W) images. A dark signal intensity rim surrounding the lesion was noted on T2-W images. T1-weighted (T1-W) images showed a signal isointense to the gray matter with a minimal heterogeneous enhancement pattern after gadolinium injection. On coronal T2-W images, the mass appeared to have infiltrated the lateral ventricle with perilesional edema (Fig. 2).
CT images of the brain. a Image before contrast agent administration reveals a huge mixed solid and cystic mass in the temporoparietooccipital lobe with dense nodular calcifications in the solid portion. b Image after contrast agent administration shows minimal enhancement. c Thinning of the ipsilateral calvaria caused by the huge mass (arrows) is seen
MR images. a T2-W axial image shows a mixed solid and cystic mass with heterogeneous signal intensity of the solid portion. There are punctate and serpentine high- and low-signal intensity structures within the mass and a dark-signal hemosiderin rim surrounding it. There is little mass effect despite its large size. b T1-W image at the same level shows a heterogeneous mass with high- and low-signal intensity areas. c Gadolinium enhanced T1-W image shows minimal enhancement of the solid portion. d On the T2-W coronal image the mass appears to have infiltrated the lateral ventricle (arrows) and perilesional edema
The lesion was suspected to be a huge supratentorial tumor such as ependymoma. Vascular malformations such as AVM and GCM were included in the differential diagnoses.
A left parietal craniotomy was performed and the mass was partially resected. At surgery the mass was multilobular and gray in color with cystic cavities containing yellowish fluid. Blood was oozing from the surface. On cross-section, the mass was solid and was a mixture of gray–white and yellow–brown to dark-brown in color with diffuse punctate calcifications and dilated blood vessels. A histopathological specimen revealed lesions composed of large ectatic fibrous-walled vessels that were devoid of intervening brain parenchyma. Histopathological diagnosis was a GCM (Fig. 3).
Two weeks after surgery, brain CT was performed. There were no unusual postoperative findings other than the residual cavernous malformation in the left temporal lobe (not shown). After surgery, the patient’s symptoms improved and he had no neurological deficits.
Discussion
GCMs are rare. In the cases previously reported in the literature, they were in different locations: cerebral, intraventricular and in the brainstem. The age of the patients varied from 16 months [2] to 56 years [3], and the patients included eight children.
Unlike giant aneurysms that are defined as having a diameter of at least 25 mm, no threshold dimension has been accepted for GCM. Some authors suggest that a useful definition of GCM would be a threshold diameter of 6 cm [2]. In our patient, the imaging findings revealed a giant mass measuring 13.8×7.8×8.3 cm. Only three of the previously reported GCMs were larger than 13 cm [2]. The mechanism by which they enlarge is probably recurrent bleeding, followed by organization of the clot, pseudocapsule formation, and secondary expansion [3, 4]. In our patient, the histopathological findings did not differ from those of the usual cavernous malformation. We presume that recurrent bleeding produced both the enlargement and the multicystic appearance in our patient. However, it has also been reported that cavernous malformations can show expansile growth without any evidence of a hemorrhagic event, mimicking a neoplasm [2, 5].
According to the cases in the literature, GCMs have variable imaging appearances, some manifesting as heterogeneous solid lesions with a peripheral hemosiderin rim, showing no significant contrast enhancement or mass effect [3] and others being completely cystic lesions [6]. GCMs have also been reported that resembled neoplasms with marked contrast enhancement and marked peritumoral edema [7]. The presence of a hemosiderin rim and blood breakdown products within the lesion and the absence of significant contrast enhancement and a mass effect might be clues to the correct diagnosis despite the large size of the lesion [3]. In our patient, the imaging findings revealed a giant mass with a hemosiderin rim, blood breakdown products and calcifications. The mass showed minimal heterogeneous enhancement on MRI. These findings were an admixture of some cases reported previously, sharing the imaging findings of the typical cavernous malformation [3–5]. However, some portions of the mass appeared to have infiltrated the occipital horn of the lateral ventricle, and this finding, as well as its large size, perilesional edema and multilobular location, made it difficult to exclude malignancy.
In cavernous malformations, large or small, the perfusion is very slow, and thus they show minimal or no contrast enhancement on CT and MR images. Some authors have reported delayed MR imaging after contrast agent injection, which might be useful in demonstrating the slow uptake of contrast agent by the cavernous malformation [8].
GCMs can mimic neoplasms, particularly those that are large in size and show multilobular involvement with perilesional edema. Therefore, histopathological evaluation of the specimen should be performed for the correct diagnosis, especially in cases that show a focal infiltrative pattern.
References
Clatterbuck RE, Moriarity JL, Elmaci I et al (2000) Dynamic nature of cavernous malformations: a prospective magnetic resonance imaging study with volumetric analysis. J Neurosurg 93:981–986
Lawton MT, Vates GE, Quinones-Hinojosa A et al (2004) Giant infiltrative cavernous malformation: clinical presentation, intervention, and genetic analysis: case report. Neurosurgery 55:988–995
Gelal F, Feran H, Rezanko T et al (2005) Giant cavernous angioma of the temporal lobe: a case report and review of the literature. Acta Radiol 46:310–313
Chicani CF, Miller NR, Tamargo RJ (2003) Giant cavernous malformation of the occipital lobe. J Neuroophthalmol 23:151–153
Siddiqui AA, Jooma R (2001) Neoplastic growth of cerebral cavernous malformation presenting with impending cerebral herniation: a case report and review of the literature on de novo growth of cavernomas. Surg Neurol 56:42–45
Khosla VK, Banerjee AK, Mathuriya SN et al (1984) Giant cystic cavernoma in a child. J Neurosurg 60:1297–1299
van Lindert EJ, Tan TC, Grotenhuis JA et al (2007) Giant cavernous hemangiomas: report of three cases. Neurosurg Rev 30:83–92
Thiex R, Kruger R, Friese S et al (2003) Giant cavernoma of the brain stem: value of delayed MR imaging after contrast injection. Eur Radiol 13:219–225
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, Y.J., Kim, JE., Kim, N.R. et al. Imaging findings of giant cavernous malformation with a focal infiltrative pattern. Pediatr Radiol 37, 1039–1042 (2007). https://doi.org/10.1007/s00247-007-0553-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-007-0553-7