Abstract
Fetuses of diabetic mothers may have structural or functional cardiac abnormalities which increase morbidity and mortality. Isolated functional abnormalities have been identified in the third trimester. The aim of the present study was to assess fetal cardiac function (systolic, diastolic, and global myocardial performance) in the second trimester in mothers with gestational diabetes, and also to relate cardiac function with glycemic control. Mothers with gestational diabetes mellitus referred for fetal cardiac evaluation in the second trimester (between 19 and 24 weeks) from March 2015 to February 2016 were enrolled as case subjects in this study. Non-diabetic mothers who had a fetal echocardiogram done between 19 and 24 weeks for other indications were enrolled as controls. Functional cardiac variables showed a statistically significant difference in isovolumetric relaxation and contraction times and the myocardial performance index and mitral E/A ratios in the gestational diabetic group (p = 0.003). Mitral annular plane systolic excursion was significantly less in the diabetic group (p = 0.01). The only functional cardiac variable found abnormal in mothers with poor glycemic control was the prolonged isovolumetric relaxation time. Functional cardiac abnormalities can be detected in the second trimester in fetuses of gestational diabetic mothers and timely intervention can improve postnatal outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maternal diabetes mellitus is known to affect fetal growth and development. Uncontrolled diabetes mellitus in early gestation has a teratogenic effect causing defects in cardiogenesis, the reported incidence of malformations being five times greater than the general population [1–3]. The most frequently associated cardiac disorders are hypertrophic cardiomyopathy (70%) pericardial effusion (15%), intermittent or persistent bradycardia (15%), and structural heart defects. Structural heart defects are related to the neural crest cells, namely ventricular septal and endocardial cushion defects, tetralogy of Fallot, and persistent truncus arteriosus.
Diabetic pregnancies can be divided into two categories: pregestational diabetes (diagnosed before the present pregnancy) and gestational diabetes (glucose intolerance detected in the present pregnancy) [4, 5]. Pregestational diabetes occurs in around 0.5% of pregnancies worldwide [6]. Prevalence of gestational diabetes is much higher ranging from 4 to 10%. In Pakistan, these incidences are 3.5 and 6%, respectively [4, 7]. Incidence of fetal congenital heart disease is the same in mothers with pregestational and gestational diabetes [5]. Effective treatment of pregestational and gestational diabetes improves short- and long-term fetal outcomes [4].
In the absence of structural heart defects, fetuses of diabetic mothers may have functional cardiac abnormalities [8–10], which have recently gained importance and may be found despite good glycemic control. It has been previously reported that interventricular septal hypertrophy develops in late third trimester of pregnancy [11] and diastolic functional abnormalities develop with it. Russell et al. have shown functional cardiac impairment in fetuses of mothers with type 1 diabetes mellitus as early as 13 weeks of gestation [6]. In fetuses of mothers with gestational diabetes, functional abnormalities without septal hypertrophy have been observed in the third trimester [12]. However, functional status of the fetal heart in the second trimester has not been well described. Alterations in fetal cardiac function from early developmental stages may predispose to increased risk of cardiovascular diseases in adulthood [6].
The present study was undertaken to assess fetal cardiac function (systolic, diastolic, and global myocardial performance) in the second trimester in mothers with gestational diabetes, and also to relate cardiac function with glycemic control. The hypothesis is that functional abnormalities may be present and detectable as early as in the second trimester in this cohort.
Patients and Methods
Mothers with gestational diabetes mellitus referred for fetal cardiac evaluation in the second trimester (between 19 and 24 weeks) from March 2015 to February 2016 were enrolled as case subjects in this study. Non-diabetic mothers who had a fetal echocardiogram done between 19 and 24 weeks for other indications were enrolled as controls. Exclusion criteria were pregestational diabetes, the presence of structural heart disease, twin pregnancies, hypertension (pregnancy induced or essential), intrauterine growth retardation (defined as weight for gestation less than 5th percentile [13]), and polyhydramnios. Ethical principles of the institution were followed and the material in question was obtained, with the subjects understanding that it might be published. Details of history, maternal and gestational ages, glycemic control (HbA1c and/or oral glucose tolerance test), medications, and non-cardiac anomalies detected on routine obstetric ultrasound scans were noted.
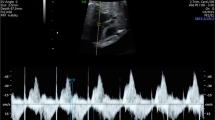
Fetal echocardiogram was done using the echocardiographic machine GE Vivid E9 Ultrasound System, (GE Healthcare Life Sciences, Pittsburg, USA) with the curvilinear 4C probe and standard fetal software for analysis. 2D, M-mode, color flow mapping, pulsed Doppler were used to analyze the fetal cardiac structure and function. The study was performed by a Pediatric Cardiologist by standard method [14], after obtaining good views and near parallel Doppler alignment with either ventricular wall or inter ventricular septum, with an incidence angle of less than 25°. No correction for angle was done. Dimension of cardiac structures, M-mode of tricuspid, and mitral annular plane systolic excursion (TAPSE and MAPSE in mm) were noted, and tricuspid and mitral inflow velocities were noted as E and A waves depicting passive and active ventricular filling, respectively. Pulsed Doppler interrogation of atrioventricular valves was done in the standard apical 4 chamber view with sampling volume from just distal to valve tips. The mean peak value of three early diastolic waves (E) and of three late diastolic or atrial filling waves (A) was recorded, and the mean ratio between the peak velocities of the E and A waves in each position (E/A ratio) was determined at the mitral and tricuspid valves.
Aortic and pulmonary valve diameters were measured in systole and tricuspid and mitral valve diameter in diastole. Systolic function was calculated as ejection fraction on 2-D measurements and when possible with M-mode measurements. Diastolic function was assessed by pulsed Doppler measuring the E/A ratios, isovolumetric relaxation time (IVRT, interval of time between aortic valve closure and opening of mitral valve in ms) isovolumetric contraction time (IVCT, interval of time between mitral valve closure and opening of aortic valve in ms), ejection time (ET, time interval from opening to closure of aortic valve, in ms), and myocardial performance index (MPI or Tei index) calculated by the formula IVCT + IVRT/ET. MAPSE and TAPSE were recorded in all fetuses. These measurements were made by standard techniques described earlier [13, 14].
Statistical Analysis
Data were collected on the statistical package SPSS version 20.5 (SPSS Inc., Chicago, IL, USA) and used for data analysis. The data were normally distributed as determined by the Shapiro–Wilk normality test. Hence quantitative analyses were reported as mean and standard deviation. Analysis of variance (ANOVA) was used for each variable. Chi-square test of the observed frequencies was used for qualitative analysis, and p < 0.05 was considered to be statistically significant.
Results
A total of 128 mothers were enrolled, 64 were in the gestational diabetic group, and 64 were in the non-diabetic control group. In the diabetic group, 44 mothers were on diet control and 20 were on oral anti-diabetics, none received insulin. The non-diabetic group was heterogeneous, with previous miscarriages, previous child with a cardiac or non-cardiac defect, echogenic focus found on routine ultrasound examination, increased nuchal translucency, advanced maternal age, and artificial reproductive technology. The mean age of mothers was 31 ± 4.9 years (median 29 years), and the mean gestational age at the time of first examination was 23 ± 3.4 weeks (median 22 weeks). Glycemic control was classified as good if the HbA1c was <6 gm/dl or the glucose tolerance test showed serum glucose levels of <160 mg/dl. 20% of mothers on diet therapy and 8% on oral anti-diabetic medications had inadequate control of diabetes.
Comparison of variables between fetuses of diabetic and non-diabetic mothers is shown in Table 1. There was no statistical difference in maternal or gestational ages, and most of the dimensional variables. However, functional variables showed that isovolumetric relaxation and contraction times were significantly prolonged in fetuses of diabetic mothers (p = 0.001 and 0.01, respectively). Myocardial performance index was significantly abnormal in the diabetic group (p < 0.001). The mitral E/A ratios were significantly low in the diabetic group (p = 0.003). Mitral annular plane systolic excursion (MAPSE) was significantly less in the diabetic group (p = 0.01), whereas, although tricuspid annular plane systolic excursion (TAPSE) was also less, it did not reach statistical significance.
Variables were also compared between mothers with diabetes with good and poor glycemic control (Table 2). The only statistically significant difference found was in isovolumetric relaxation time and thickness of interventricular septum in the poor glycemic control group. Rest of the parameters did not differ in fetuses examined at an average gestational age of 23 weeks.
Discussion
Fetuses of mothers with gestational diabetes are at a high risk of cardiac anomalies (structural and functional), cardiac failure, and sudden cardiac death [6, 15]. Uncontrolled diabetes mellitus with altered metabolism, as well as fluctuating glucose levels in early gestation, have a teratogenic effect causing defects in cardiogenesis and cardiac function. This may be related to fetal hyperinsulinemia but is most likely multifactorial [15, 16]. The wide range of cardiac abnormalities found may suggest a complex pathogenesis in these fetuses. This not only has been well described in pregestational diabetes, but is also documented in gestational diabetes, latter being 8–20 times more prevalent.
Functional fetal cardiac assessment is a crucial part of evaluation of all high-risk fetuses including those of diabetic pregnancies [10, 13]. Ventricular diastolic dysfunction can be present in the absence of septal hypertrophy [12, 17]. Recognition of early and subtle changes may be help in management and improve outcome.
Mitral and tricuspid valve inflow patterns, denoting preload characteristics, have been widely studied and are known to change with gestational age. E wave velocity, which depicts passive ventricular filling, increases with gestational age. A wave, which denotes active ventricular filling due to atrial contraction, remains static throughout pregnancy [11, 14]. The increasing E/A wave ratio demonstrate a maturational improvement in ventricular compliance with increasing gestational age leading to a gradual change in filling pressures [11, 18, 19]. IVCT reflects systolic contraction times with longer time consistent with poorer contraction [20], while IVRT reflects diastolic or relaxation function [1], slow relaxation reflecting poor compliance. MPI therefore represents global function. Normal ranges for these are described elsewhere [13, 21].
Pregestational diabetes with poor control has been shown to have a greater association with cardiac functional defects [6]. With improved insight into fetal cardio-circulatory dynamics, in the absence of structural anomalies, functional cardiac abnormalities, particularly left ventricular relaxation, filling, and compliance, are commonly found with gestational diabetes as well and may be unrelated to glycemic control [22]. IVRT is an important indicator of calcium uptake by the myocardium and therefore of myocardial relaxation [23]. Several workers have also shown no relationship of MPI with either heart rate or gestational age [21, 22].
In our study, we have found significant functional abnormalities in the gestational diabetic group compared to the controls in the second trimester. Ventricular filling pressures in the form of E/A ratio showed a less compliant left ventricle than the right ventricle in the gestational diabetic group. Another parameter of left ventricular compliance is the MAPSE which was also significantly less in the study group. TAPSE reflecting right ventricular function was also less but did not reach statistical significance. IVRT, IVCT, and myocardial performance index (MPI) were also significantly deranged in the study group.
Hypertrophic cardiomyopathy typically observed in infants of the pregestational diabetic mother is characterized by hypertrophy of the interventricular septum, and to a lesser extent the ventricular free walls [11, 18]. This pathology, in association with fetal hyperinsulinemia and increased somatic growth in maternal diabetes, is found mostly in the third trimester [23]. This is less frequently observed in the fetuses of gestational diabetic mothers [12]. In this study, septal thickness was significantly more even in the second trimester with poor diabetic control. Good glycemic control may delay and perhaps reduce functional cardiac impairment [24]. Reller et al. found that early careful management of diabetes in the first trimester compared to late entries had better right ventricular function and less postnatal respiratory distress [25]. The present study showed the poor glycemic control group to have significantly prolonged IVRT. However, no difference was found in most of other cardiac functional parameters between the good and poor glycemic control group of patients, as has been demonstrated by other workers previously. Therefore, IVRT may be a significantly sensitive parameter to detect early cardiac functional abnormalities in pregnancies with poor diabetic control. We do not have a complete postnatal follow-up of these fetuses. A further study design including postnatal follow-up would throw more light on the significance of glycemic control on fetal cardiorespiratory status.
Conclusion
Gestational diabetes is a common obstetric morbidity and puts the fetus at risk of structural and functional cardiac abnormalities. Functional cardiac abnormalities have complex pathogenesis and maybe diagnosed even in the second trimester, despite good glycemic control.
References
Fouda UM, El Kassen MMA, Hefny SM, Fouda RM, Hashem AT (2013) Role of fetal echocardiography in the evaluation of structure and function of fetal heart in diabetic pregnancies. J Maternal-Fetal Neonatal Med 26(6):571–575
Nashaat EH, Mansour GM (2010) Uncontrolled diabetes mellitus and fetal heart. Researcher 2(5):47–55
Akhter J, Qureshi R, Rahim F, Khan MA (1996) Diabetes in pregnancy in Pakistani women: Prevalence and complications in an indigenous south Asian community. Diabetic Med 13(2):189–191
To WWK (2011) Applications of doppler studies for fetal surveillance in diabetic pregnancies. In: Radenkovic M (ed) Gestational Diabetes, Chap. 15. InTech, Rijeka, p 264–276. ISBN: 978-953-307-581-5. http://www.intechopen.com/books/gestational-diabetes/applications-of-doppler-studies-for-fetal-surveillance-indiabetic-pregnancies
Hunter LE, Sharland GK (2015) Maternal gestational diabetes and fetal congenital heart disease: an observational study. J Preg Child Health 2:132. doi:10.4172/2376-127X.1000132
Russell NE, Foley M, Kinsley BT, Firth RG, Coffey M, McAuliffe FM (2008) Effect of pregestational diabetes mellitus on fetal cardiac function and structure. Am J Obstet Gynecol 199(3):312.e1-7. doi:10.1016/j.ajog.2008.07.016
Jawad F, Irshaduddin PK (1996) Prevalence of gestational diabetes and pregnancy outcome in Pakistan. East Med Health J 2(2):268–273
Weiner Z, Zloczower M, Lerner A, Zimmer E, Itskovitz-Eldor J (1999) Cardiac compliance in fetuses of diabetic women. Obstet Gynecol 93(6):948–951
Ichizuka K, Matsuoka R, Hasegawa J, Shirato N, Jimbo M, Otsuki K, Sekizawa A, Farina A, Okai T (2005) The Tei index for evaluation of fetal myocardial performance in sick fetuses. Early Hum Dev 81:273–279
Rizzo G, Arduini D, Capponi A, Romanini C (1995) Cardiac and venous blood flow in fetuses of insulin-dependent diabetic mothers: evidence of abnormal hemodynamics in early gestation. Am J Obstet Gynecol 173(6):1775–1781
Miyake T (2001) Doppler echocardiographic studies of diastolic cardiac function in the human fetal heart. Kurume Med J 48(1):59–64
Balli S, Pac FA, Ece İ, Oflaz MB, Kibar AE, Kandemir Ö (2014) Assessment of cardiac functions in fetuses of gestational diabetic mothers. Pediatr Cardiol 35(1):30–37. doi:10.1007/s00246-013-0734-0 (Epub 2013 Jun 19)
Parasuraman R, Osmond C, Howe DT (2013) Gestation-specific reference intervals for fetal cardiac Doppler indices from 12 to 40 weeks of gestation. Open J Obstet Gynecol 3:97–104
Hernandez-Andrade E, Benavides-Serralde JA, Cruz-Martinez R, Welsh A, Mancilla-Ramirez J (2012) Evaluation of conventional Doppler fetal cardiac function parameters: E/A ratios, outflow tracts, and myocardial performance index. Fetal Diagn Ther 32:22–29. doi:10.1159/000330792
Reis ZSN, Osanan GC (2011). Congenital cardiopathies screening associated with diabetes mellitus using maternal fructosamine plasma concentration. In: Radenkovic M (ed) Gestational diabetes. InTech, Rijeka. doi:10.5772/21867. http://www.intechopen.com/books/gestational-diabetes/congenital-cardiopathies-screening-associated-with-diabetes-mellitus-using-maternal-fructosamine-plasmaconcentration
Hornberger LK (2006) Maternal diabetes and the fetal heart. Heart 92:1019–1021
Hatém MA, Zielinsky P, Hatém DM, Nicoloso LH, Manica JL, Piccoli AL, Zanettini J, Oliveira V, Scarpa F, Petracco R (2008) Assessment of diastolic ventricular function in fetuses of diabetic mothers using tissue Doppler. Cardiol Young 18(3):297–302. doi:10.1017/S1047951108002138 (Epub 2008 Apr 14)
Wong ML, Wong WHS, Cheung YF (2007) Fetal myocardial performance in pregnancies complicated by gestational impaired glucose tolerance. Ultrasound Obs Gyn 29(4):395–400
Blanchard AC, Fouran JC (1993) Determinants of Doppler flow velocity profile through mitral valve of the human fetus. Br Heart J 70:437–460
Mieghem TV, Hodges R, Jaeggi E, Ryan G (2014) Functional echocardiography in the fetus with non-cardiac disease. Prenat Diagn 34:23–32
Nair A, Radhakrishnan S (2016) Fetal left ventricular myocardial performance index: defining normal values for Indian population and a review of literature. Ann Pediatr Cardiol 9(2):132–136
Rizzo G, Arduini D, Romanini C (1992) Accelerated cardiac growth and abnormal cardiac flow in fetuses of type I diabetic mothers. Obstet Gynecol 80(3):369–376
Reis ZSN, Osanan GC (2011). Congenital cardiopathies screening associated with diabetes mellitus using maternal fructosamine plasma concentration. In: Radenkovic M (ed) Gestational diabetes, Chap. 14. InTech, Rijeka, p 264–276. ISBN: 978-953-307-581-5. http://www.intechopen.com/books/gestational-diabetes/applications-of-doppler-studies-for-fetal-surveillance-indiabetic-pregnancies
Chu C, Gui YH, Ren YY, Shi LY (2012). The impact of maternal gestational diabetes mellitus on fetal hearts. Biomed Environ Sci 25(1):15–22
Reller MD, Tsang RC, Meyer RA, Braun CP (1985) Relationship of prospective diabetes control in pregnenecy to neonatal cardiorespiratory function. J Pediatr 106(1):86–90
Acknowledgements
The authors acknowledge the statistical assistance provided by Mr Iqbal Azam and the echocardiographic technical assistance by Ms Salima Ashiq Ali and Urooj Fatima.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest. The corresponding (first author) has done the study with the technical help of echocardiography staff and would shoulder the responsibility of the overall integrity of the work. The last 3 authors have collectively contributed to the conception, design, collection of data, and critical revision.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Atiq, M., Ikram, A., Hussain, B.M. et al. Assessment of Cardiac Function in Fetuses of Gestational Diabetic Mothers During the Second Trimester. Pediatr Cardiol 38, 941–945 (2017). https://doi.org/10.1007/s00246-017-1600-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-017-1600-2