Abstract
We investigated cardiac function in 67 fetuses of gestational diabetic mothers (FGDMs) and 122 fetuses of healthy mothers between 24 and 36 weeks of gestation. Cardiac functions were evaluated by M-mode, pulsed-wave, and tissue Doppler echocardiography. Fetal echocardiograms were performed at 24, 28, 32, and 36 weeks of gestation. Glycated hemoglobin (HbA1c) levels were obtained from all pregnant women at 24 weeks of gestation. The mean age of diabetic pregnant women was significantly greater than that of controls. Serum HbA1c values of both groups were within normal limits, but they were significantly greater in the diabetic group (p = 0.003). The increase in peak aortic and pulmonary artery velocities were greater in FGDM (p < 0.001). No pathological interventricular septal (IVS) hypertrophy was observed. There was a significant increase in IVS thickness in FGDM compared with controls, which was more prominent at the end of the third trimester (p < 0.001). During the course of pregnancy, mitral E-wave (p < 0.001), A-wave (p = 0.007), tricuspid E-wave (p < 0.001) and A-wave (p = 0.002) velocities were greater in FGDM. The increases in mitral E/A and tricuspid E/A ratios were lower in FGDM with advancing gestation. The E a-wave (p = 0.02), A a-wave (p = 0.04), and S a-wave (p < 0.001) velocities of the right-ventricular (RV) free wall and the E a (p = 0.02) and A a (p = 0.01) velocities of the left-ventricle (LV) posterior wall were greater in FGDM during the course of pregnancy. The E a/A a ratio of the RV posterior wall was greater in FGDM with advancing gestation (p < 0.03). LV and RV E/E a ratios were similar in both groups. The LV myocardial performance index measured by pulsed-wave Doppler was greater in FGDM (p < 0.001). We detected diastolic dysfunction in FGDM. The data suggest that gestational diabetes mellitus may impair ventricular diastolic functions without causing pathological fetal myocardial hypertrophy. We detected subclinical diastolic dysfunction using both pulsed-wave and tissue Doppler imaging in FGDM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gestational diabetes mellitus (GDM) is the most common metabolic disorder in pregnancy, with an overall prevalence of 3–7 % during pregnancy [18]. Although the exact mechanism of its effect on the fetal heart has not been defined, it is considered to be multifactorial. High levels of glycated hemoglobin (HbA1c) are particularly associated with increased risk of malformation [12]. The presence of hyperglycemia influences biochemical transformation processes in the fetus [3, 11]. In addition, maternal diabetes induces placental genes related to chronic stress and inflammation, and recent data suggest the potential role of inflammation for embryopathy related to maternal diabetes [5]. The myocardial tissue is the most likely structure affected by hyperglycemia. The ventricular free walls are less affected by hypertrophy compared with the interventricular septum (IVS) [7].
Results of recent studies suggest that pre-GDM leads to fetal cardiomyopathy and fetal diastolic dysfunction after a decrease of ventricular compliance [22]. However, current studies on GDM are insufficient, and the effects of GDM on the fetus remain unclear. Thus, the aim of the present study was to investigate detailed cardiac function in fetuses of gestational diabetic mothers (FGDMs).
Materials and Methods
Patient Population
One hundred eighty-nine pregnant women who were admitted to the Pediatric Cardiology Outpatient Clinics of Turkey Yüksek Ihtisas Training and Research Hospital between November 2009 and January 2012 were included in the study. All patients signed a written informed consent. This study was approved by the local Ethics Committee. The fetal age of the pregnant women at follow-up was determined by obstetric ultrasound. All fetuses were evaluated for growth, and amniotic fluid volume was assessed. Fetal biometric measurements, including biparietal diameter, abdominal circumference, femur length, and fetal weight, were estimated. Intrauterine growth restriction (IUGR) was defined as an estimated fetal weight below the 10th percentile with decreased amniotic fluid volume. Fetal echocardiogram was performed at 24, 28, 32 and 36 weeks of gestation to assess function. In this prospective cohort study, the study group consisted of 67 pregnant women with GDM, and the control group consisted of 122 healthy pregnant women.
The diagnosis of GDM was made according to the guidelines of the American Diabetes Association [1] and the World Health Organization. In addition, HbA1c levels were assessed in all patients. Only four of the pregnant women were on insulin therapy, whereas the rest of the pregnant women were on diet alone. Fetuses with congenital heart disease, rhythm disorder, or IUGR were not included in the study. Exclusion criteria for all women were pre-GDM, -eclampsia, -existing hypertension treated with anti-hypertension drugs, renal disease, liver disease or hematologic disease.
Fetal Echocardiography
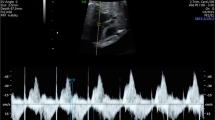
All ultrasound examinations were performed with a commercially available echocardiographic machine (Vivid 7 Dimension System; Vingmed-General Electric, Horten, Norway). The examinations were performed using a 4-MHz convex probe and a large-scale segmental analysis. Cardiac structural assessment was performed using segmental sequential analysis. The IVS septum, left-ventricular (LV), and right-ventricular (RV) end-diastolic diameters were measured using M-mode echocardiography. IVS thickness was measured at end-diastole in M-mode echocardiography. Interventricular hypertrophy was defined as an IVS septum thickness >2 SDs according to gestational age [6]. In the four-chamber view of the fetal heart, the cursor was placed perpendicular to the IVS, just below the tips of the atrioventricular valves. The end-diastolic dimension (EDD) and the end-systolic dimension (ESD) of the LV and RV were measured by M-mode. LV and the RV shortening fractions were calculated as (EDD − ESD)/EDD. Diameters of the aortic and pulmonary annulus were measured three times in frozen real-time images during systole using the leading edge-to-leading-edge method, and their mean value was used for further analysis.
Mitral and tricuspid inflow velocities were measured in apical four-chamber view using pulsed-wave Doppler at the leaflet tips of the mitral and tricuspid valves. Peak systolic velocity waveforms from the ascending aorta were obtained from the five-chamber view. Peak systolic velocity waveforms from the pulmonary artery were obtained from the short-axis view. In both vessels, the Doppler sample volume was placed immediately distal to the semilunar valves.
The fetal cardiac tissue Doppler imaging (TDI) was performed in four-chamber view. The imaging was performed when fetal body movements paused after the mother was asked to hold her breath. Particular attention was also paid to keep the angle of insonation <20° while the tissue Doppler and pulsed-wave velocities were obtained. No angle correction of the Doppler signal was applied. In the TDI and the pulsed-wave Doppler measurements, the average of three successive pulses was taken. Right and left myocardial velocities were obtained from the apical four-chamber view. The sample volume was placed at three basal myocardial positions: the LV posterior wall, the IVS, and the RV free wall. The sample volume width measured approximately 1 mm. The Nyquist limit was adjusted to 15–20 cm/s. The mean peak values of three early diastolic waves (E a) and of three late diastolic or atrial filling waves (A a) were registered, and the mean ratio of the peak velocities of the E a and A a waves in each position (E a/A a ratio) was determined. The mean peak values of three systolic waves (S a) were registered. LV E/E a ratios were also calculated.
In the measurement of the LV myocardial performance index (MPI), the E/A waveform was always kept positive, whereas the angle of insonation was always kept at <20° [10]. The four-chamber view was taken, and the apical view of the heart was obtained. To measure the MPI, the Doppler cursor was placed on the lateral wall of the ascending aorta just below the aortic valve and next to the mitral valve. The waves reflecting systole and diastole were obtained in combination. At the beginning and the end of the aortic valve wave forms, a clear echo was formed in the Doppler tracing corresponding to the opening and closing of the two valves. Measurements at three time intervals were performed using pulsed-wave Doppler. These intervals were the isovolumetric contraction time (IVCT [time interval from the closure of the mitral valve to the opening of the aortic valve]), the ejection time (ET [time interval between the opening and the closure of the aortic valve]), and the isovolumetric relaxation time (IVRT [time interval from the closure of the aortic valve to the opening of the mitral valve]). The MPI was calculated by the following formula: (IVCT + IVRT)/ET. All studies were recorded on videotape and as hard copies. Measurements were performed by a single operator who was blinded to hypothesis and patients’ clinic status.
Statistical Analysis
All analyses were performed using SPSS version 15.0 (SPSS, Chicago, IL) statistical software. The intergroup comparisons in terms of the changes related to advancing gestation were performed by the general linear model repeated-measures analyses of variance. Student t test was performed in the assessment of the groups in the same week of gestation, and p < 0.05 was considered to be statistically significant.
Results
Both groups were similar in terms of gravidity and parity (Table 1). The mean age at the time of admission of the diabetic pregnant women (31.57 ± 5.9 years) was significantly greater than that in the control group (27.95 ± 5.8 years). Mean HbA1c in the diabetic group (5.79 %) was significantly greater than that in the control group (5.02 %) (p = 0.003); its level at >6.5 % indicate pathological blood glucose concentrations. The mean infant birth weight of diabetic mothers (3,145 ± 300.4 g) was similar to that in the control group (3,051 ± 303.4 g). We did not detect any pathologic hypertrophy in the IVS.
The following alterations were observed in the fetal echocardiography according to the gestational week.
Week 24 of Gestation
The MPI value was significantly greater in infants from diabetic mothers compared with those in the control group (Table 5).
Week 28 of Gestation
The values of aortic velocity, IVS thickness, mitral E, mitral A, tricuspid E, tricuspid A, RV E a, RV E a/A a, septum E a/A a, IVRT, and MPI were significantly greater, whereas the LV E/E a value was significantly lower, in the FGDM group compared with the control group (Tables 2, 3, 4, 5).
Week 32 of Gestation
The values of the pulmonary artery and aortic velocities, IVS thickness, mitral E, mitral A, tricuspid E, RV E a, RV E a/A a, LV E a/A a, septum E a/A a, IVRT, and MPI were significantly greater in the FGDM group compared with the control group (Tables 2, 3, 4, 5).
Week 36 of Gestation
The values of pulmonary artery and aortic velocity, IVS thickness, mitral E, mitral A, tricuspid E, tricuspid A, RV E a, RV S a, RV E a/A a, LV E a, IVRT, and MPI were significantly greater, whereas the LV E/E a value was significantly lower, in the FGDM group compared with the control group (Tables 2, 3, 4, 5).
During the course of pregnancy, although the rates of increases in the diameters of the aortic and pulmonary annuli were similar, the pulmonary artery and aortic velocities were significantly greater in the FGDM group compared with the control group (Table 2). There were no differences in LV and RV shortening fractions during the course of pregnancy (approximately 34 % for both groups). Mitral E, A and tricuspid E- and A-wave velocities were significantly greater in the FGDM group compared with the control group (Table 2), whereas mitral E/A and tricuspid E/A ratios were significantly lower in FGDM with advancing gestation (Table 2). The E/E a ratio gradually decreased in both the RV and LVs with no differences between the groups (Tables 3, 4).
Concordant to the myocardial development during the course of pregnancy, all myocardial velocities obtained from all levels increased. The increase of myocardial velocity was greater in the RV, whereas the velocities of the RV free walls were greater than the LV velocities, which in turn were greater than those of the septum. Although the E a-wave velocities obtained from all levels were always lower than the A a-wave velocities, the E a/A a ratio was increased because the increase of E a velocity was greater than the A a velocity during pregnancy. The RV E a-, A a-, and S a-wave velocities, as well as the LV E a- and S a-wave velocities, were significantly greater in the FGDM group compared with the control group. Furthermore, the RV E a/A a ratio was significantly greater in the FGDM group compared with the control group (Table 4).
The MPI value increased during pregnancy, particularly in the third trimester, which was mainly driven by the significant increase in IVRT (Table 4). The changes in IVCT and ET during pregnancy were similar between the groups (Table 5).
Discussion
Cardiomyopathy associated with hypertrophy of the IVS in children of diabetic mothers is the most common cause of diastolic function disorder in childhood. The diastolic phase includes two components: ventricular relaxation and atrial systole. Ventricular relaxation is a process that occurs during isovolemic relaxation and then during early rapid filling of the ventricle. Using conventional Doppler imaging, diastolic dysfunction is diagnosed when at least two of the following parameters are identified: (1) abnormal E/A ratio through mitral or tricuspid valve inflow and (2) increased duration of IVRT. Cardiac dysfunction secondary to severe intrauterine myocardial hypertrophic changes, particularly in FGDM, has been frequently reported [4]. Furthermore, increased myocardial mass and LV hypertrophy in the fetal heart was suggested to cause greater preload than seen in normal controls [21]. No pathological IVS hypertrophy was observed in our study, although we found evidence of subclinical diastolic dysfunction in FGDM.
An HbA1c level <6.5 % is considered normal in pregnancy [8]. In our study, the average HbA1c levels were <6.5 % in both groups, although they were significantly greater in diabetic pregnant women compared with the healthy controls. Interventricular hypertrophy is defined as an IVS thickness >2 SDs according to gestational age. Rizzo et al. [15] reported an increase in interventricular thickness during the second and third trimesters of gestation as well as an inverse correlation between the E/A ratio and IVS thickness. They advocated that ventricular compliance was impaired by the thickening of the IVS. In contrast, Russell et al. [17] did not observe disproportionate hypertrophy in the diabetic group and suggested that this was related to the generalized hypertrophy. In our study, the observation of diastolic dysfunction in the absence of a pathological hypertrophy supported that the diastolic dysfunction was not related to the hypertrophy alone.
In our study, aortic and pulmonary artery flow velocities were greater in FGDM compared with the control group. Rizzo et al. [15] suggested that the greater levels of peak flow velocities in FGDM were related to increased fetal cardiac output resulting from increased somatic growth of the fetus during pregnancy. In our study, although the flow velocities of FGDM were greater than those in the control group, there were no differences between the two groups in terms of birth weight. Thus, changes in flow velocities in FGDM may be related to alterations in myocardial compliance.
LV and RV shortening fractions were approximately 34 % in both the FGDM and control groups. Ren et al. [14] observed that compared with the control group, the LV ejection fraction in patients with gestational diabetes followed an increasing course that was independent from glycemic control. Gandhi et al. [7] also reported increased ventricular diameters and contractility in FGDM. In our study, there we no differences in ventricular diameters and shortening fraction between the FGDM group and the control group.
Rizzo et al. [16] found lower rates of increase in E/A in FGDM during pregnancy. In contrast, Wong et al. [21] reported similar rates of E/A of the mitral and tricuspid valves in control-group fetuses versus fetuses of mothers with impaired glucose tolerance. With progressing gestation, the greater rate of increase of E wave compared with A wave indicates increased activity and passive ventricular filling. In a study by Flores et al., normal cardiac functions and normal morphological alterations were observed in FGDM, whereas Weiner et al. [20] reported lower E/A rates in fetuses of pre-gestational diabetic mothers. In our study, mitral and tricuspid E/A ratios were also significantly lower in FGDM compared with the control group during the course of pregnancy, which likely indicates diastolic dysfunction secondary to developmental retardation of ventricular maturation.
Despite the lower tissue Doppler velocity of the E a wave compared with the A a wave during pregnancy, the E a/A a ratio increased toward term age, suggesting an improvement in myocardial compliance and relaxation. In our study, there was a similar pattern of change of tissue Doppler velocities with advancing gestation, although the velocities of the RV E a, A a and S a, and LV E a waves were greater in FGDM compared with the control group. We also found a greater RV E a/A a ratio in FGDM compared with the control group during the course of pregnancy. These data suggest that compliance and relaxation of the RV were more likely affected than that for the LV. Decreased compliance in the presence of maternal diabetes leads to a high level of myocardial acceleration, particularly in the RV [9]. A greater RV E a/A a ratio in FGDM was considered the result of an adaptation process to the present situation rather than a pathological process. Furthermore, Ren et al. [14] reported lower rates of E a/A a in FGDM with respect to gestational age.
In a study of fetuses of pre-gestational diabetic mothers performed by Nii et al. [13], the E/E a ratio was decreased due to greater rates of increased E a values during the course of pregnancy. This accelerated increase in E a values is related to increased ventricular compliance. The greater levels of MPI in the first trimester in mothers having type 1 diabetes mellitus was also assessed as a response of the fetal heart to hyperglycemia, suggesting that the fetal heart was more sensitive to hyperglycemia during the initial periods of pregnancy. Rizzo et al. [16] reported lower ratios of E/A in fetuses of pre-gestational diabetic pregnant women between 16 and 20 weeks compared with those of healthy mothers. The afterload decreases with advancing gestational age in a normal pregnancy. In the present study, we found a decreasing E/E a ratio, especially in the diabetic group, during the course of pregnancy, which was likely a result of the greater myocardial velocities at the mitral and tricuspid annulus due to GDM. However, there were no differences in LV and RV E/E a ratios between the groups.
Although MPI is a global indicator of cardiac function, it is also used for the assessment of fetal ventricular function. Indeed, MPI has been suggested to be a potential follow-up criterion in complicated pregnancies, cases of intrauterine development retardation associated with fetal cardiac adaptive alterations, fetuses of pre-eclamptic mothers, cases of hydrops fetalis, and cases of fetal Rh isoimmunization. Increased MPI is an indicator of globally impaired ventricular function in FGDM during the intermediate and late periods of pregnancy. Although MPI has been shown to increase in pathological situations, such as hypervolemia and increased cardiac afterload, a study by Api et al. [2] in pre-eclamptic babies reported no significant alteration in MPI values despite increased afterload. Tsutsumi et al. [19] defined increased MPI as an indicator of global worsening of ventricular function between 27 and 33 weeks of pregnancy. Increased IVRT and increased E/A ratio are also indicators of improvement of ventricular diastolic function associated with the progression of pregnancy. Russell et al. [17] reported that increasing MPI during pregnancy was associated with increasing IVRT in FGDM. In our study, we also found increased MPI related to significantly increased IVRT in FGDM, particularly at the end of the second trimester and at the third trimester.
Conclusion
Although FGDM included in our study were asymptomatic, we detected subclinical diastolic dysfunction and increased left MPI that may be related to alterations in myocardial compliance. Thus, GDM may impair ventricular diastolic functions without causing pathological fetal myocardial hypertrophy. Tissue Doppler and pulsed-wave Doppler play an important role in showing diastolic dysfunction.
References
American Diabetes Association (2002) Preconception care of women with diabetes. Diabetes Care 28:82–84
Api O, Emeksiz MB, Api M, Ugurel V, Unal O (2009) Modified myocardial performance index for evaluation of fetal cardiac function in pre-eclampsia. Ultrasound Obstet Gynecol 33:51–57
Corrigan N, Brazil DP, McAuliffe F (2009) Fetal cardiac effects of maternal hyperglycemia during pregnancy. Birth Defects Res A 85:523–530
Dawid G, Węgrzynowski J, Kwiatek M, Biczysko-Mokosa A, Petriczko E, Horodnicka-Józwa A (2010) A fetal dilated and hypertrophic cardiomyopathy associated with maternal gestational diabetes a case report. Pediatr Endocrinol Diabetes Metab 16:123–125
Desoye G, Shafrir E (1996) The human placenta in diabetic pregnancy. Diabetes Rev 4:70–89
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I et al (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57:450–458
Gandhi JA, Zhang XY, Maidman JE (1995) Fetal cardiac hypertrophy and cardiac function in diabetic pregnancies. Am J Obstet Gynecol 173:1132–1136
Garcia-Flores J, Jañez M, Gonzalez MC, Martinez N, Espada M, Gonzalez A (2011) Fetal myocardial morphological and functional changes associated with well-controlled gestational diabetes. Eur J Obstet Gynecol Reprod Biol 154:24–26
Hatém MA, Zielinsky P, Hatém DM, Nicoloso LH, Manica JL, Piccoli AL et al (2008) Assessment of diastolic ventricular function in fetuses of diabetic mothers using tissue Doppler. Cardiol Young 18:297–302
Hernandez-Andrade E, López-Tenorio J, Figueroa-Diesel H, Sanin-Blair J, Carreras E, Cabero L et al (2005) A modified myocardial performance (Tei) index based on the use of valve clicks improves reproducibility of fetal left cardiac function assessment. Ultrasound Obstet Gynecol 26:227–232
Langer O, Conway DL (2000) Level of glycemia and perinatal outcome in pregestational diabetes. J Matern Fetal Med 9:35–41
Macklon NS, Hop WCJ, Wladimiroff JW (1998) Fetal cardiac function and septal thickness in diabetic pregnancy: a controlled observational and reproducibility study. Br J Obstet Gynaecol 105:661–666
Nii M, Roman KS, Kingdom J, Redington AN, Jaeggi ET (2006) Assessment of the evolution of normal fetal diastolic function during mid and late gestation by spectral Doppler tissue echocardiography. J Am Soc Echocardiogr 19:1431–1437
Ren Y, Zhou Q, Yan Y, Chu C, Gui Y, Li X (2011) Characterization of fetal cardiac structure and function detected by echocardiography in women with normal pregnancy and gestational diabetes mellitus. Prenat Diagn 31:459–465
Rizzo G, Arduini D, Romanini C (1992) Accelerated cardiac growth and abnormal cardiac flow in fetuses of type I diabetic mothers. Obstet Gynecol 80:369–376
Rizzo G, Arduini D, Capponi A, Romanini C (1995) Cardiac and venous blood flow in fetuses of insulin-dependent diabetic mothers: evidence of abnormal hemodynamics in early gestation. Am J Obstet Gynecol 173:1775–1781
Russell NE, Foley M, Kinsley BT, Firth RG, Coffey M, McAuliffe FM (2008) Effect of pregestational diabetes mellitus on fetal cardiac function and structure. Am J Obstet Gynecol 199:312
Schafer G, Veter K (1999) Diabetes and pregnancy. Ther Umsch 56:572–576
Tsutsumi T, Ishii M, Eto G, Hota M, Kato H (1999) Serial evaluation for myocardial performance in fetuses and neonates using a new Doppler index. Pediatr Int 41:722–727
Weiner Z, Zloczower M, Lerner A, Zimmer E, Itskovitz-Eldor J (1999) Cardiac compliance in fetuses of diabetic women. Obstet Gynecol 93:948–951
Wong ML, Wong WH, Cheung YF (2007) Fetal myocardial performance in pregnancies complicated by gestational impaired glucose tolerance. Ultrasound Obstet Gynecol 29:395–400
Zielinsky P, Nicoloso LH, Firpo C, Marcantonio S, Scheid M, Gus EI et al (2004) Alternative parameters for echocardiographic assessment of fetal diastolic function. Braz J Med Biol Res 37:31–36
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Balli, S., Pac, F.A., Ece, İ. et al. Assessment of Cardiac Functions in Fetuses of Gestational Diabetic Mothers. Pediatr Cardiol 35, 30–37 (2014). https://doi.org/10.1007/s00246-013-0734-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-013-0734-0