Abstract
Pericardial effusion (PE) may require readmission after cardiac surgery and has been associated with postoperative morbidity and mortality. We sought to identify the prevalence and risk factors for postoperative PE requiring readmission in children. A retrospective analysis of the Pediatric Health Information System database was performed between January 1, 2003, and September 30, 2014. All patients ≤18 years old who underwent cardiac surgery were identified by ICD-9 codes. Those readmitted within 1 year with an ICD-9 code for PE were identified. Logistic regression analysis was performed to determine risk factors for PE readmissions. Of the 142,633 surgical admissions, 1535 (1.1%) were readmitted with PE. In multivariable analysis, older age at the initial surgical admission [odds ratio (OR) 1.17, p < 0.001], trisomy 21 (OR 1.24, p = 0.015), geographic region (OR 1.33–1.48, p ≤ 0.001), and specific surgical procedures [heart transplant (OR 1.82, p < 0.001), systemic-pulmonary artery shunt (OR 2.23, p < 0.001), and atrial septal defect surgical repair (OR 1.34, p < 0.001)] were independent risk factors for readmission with PE. Of readmitted patients, 44.2% underwent an interventional PE procedure. Factors associated with interventions included shorter length of stay (LOS) for the initial surgical admission (OR 0.85, p = 0.008), longer LOS for the readmission (OR 1.37, p < 0.001), and atrial septal defect surgery (OR 1.40, p = 0.005). In this administrative database of children undergoing cardiac surgery, readmissions for PE occurred after 1.1% of cardiac surgery admissions. The risk factors identified for readmissions and interventions may allow for improved risk stratification, family counseling, and earlier recognition of PE for children undergoing cardiac surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pericardial effusion (PE) is a well-known morbidity after cardiac surgery. PE is often a component of postpericardiotomy syndrome (PPS), defined as the occurrence of at least two of the following criteria: fever beyond the first postoperative week without infection, pleuritic chest pain, friction rub, new or worsening pleural effusion, or new or worsening PE [1]. PPS was first introduced as a clinical entity in the 1950s after surgical repair of mitral stenosis secondary to rheumatic heart disease [2]. This syndrome was subsequently identified in patients without rheumatic heart disease, and reports later suggested that the potential etiology of PPS was anti-heart antibodies [3]. The most common current theory of PPS and postoperative PE is an immune-mediated inflammatory process involving the pericardium. PPS typically occurs in the first postoperative weeks, but may occur months after cardiac surgery. While the severity of disease varies and may be mild, patients can develop life-threatening cardiac tamponade.
Conflicting reports exist for both the prevalence and risk factors for PPS and PE after cardiac surgery. Most recent studies have documented PPS in 3–43% of patients [4–10]. PE, either alone or as a component of PPS, has been reported across a wide range of patients from 1 to 85% [11–20] with tamponade occurring in 1–2% [11, 13, 17]. Numerous risk factors have been identified, but these studies have frequently been limited to reports from single institutions with relatively small number of patients. The primary objective of the current study is to determine the prevalence and risk factors for readmissions secondary to PE in children after cardiac surgery through the use of a large multi-institutional database. The secondary objective is to determine the risk factors associated with PE interventions during the readmission. Addressing these objectives through a large database allows for the study of relatively rare outcomes through a large cohort and the ability to examine varying practice patterns, as opposed to the potential biases from single-institution reports.
Materials and Methods
Study Design
Data for this study were obtained from the Pediatric Health Information System (PHIS), an administrative database that contains inpatient, emergency department, ambulatory surgery, and observation encounter-level data from 45 not-for-profit, tertiary care pediatric hospitals in the USA. These hospitals are affiliated with the Children’s Hospital Association (Overland Park, KS). Data quality and reliability are assured through a joint effort between the Children’s Hospital Association and participating hospitals. Portions of the data submission and data quality processes for the PHIS database are managed by Truven Health Analytics (Ann Arbor, MI). For the purposes of external benchmarking, participating hospitals provide discharge/encounter data including demographics, diagnoses, and procedures. Nearly all of these hospitals also submit resource utilization data (e.g., pharmaceuticals, imaging, and laboratory) into PHIS. Data are de-identified at the time of data submission, and data are subjected to a number of reliability and validity checks before being included in the database. Unique patients were identified by medical record numbers and unique admissions by identification numbers.
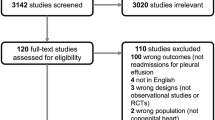
This study was a retrospective cohort study. The patient cohort consisted of all patients who underwent cardiac surgery from January 1, 2003, through September 30, 2014, across the hospitals in the PHIS database. A query of the PHIS database was performed to identify all patients 18 years old or younger during this time period with an international classification of diseases, ninth revision (ICD-9) diagnosis code of heart disease and procedure code for cardiac surgery. From this cohort, to review all patients readmitted with a PE, the database was queried for patients readmitted within 1 year with either an ICD-9 diagnosis code for PE or an ICD-9 procedure code for a pericardial intervention, primarily pericardiocentesis (Table 1). For the readmission, each patient was counted only once, and only the most recent surgical admission prior to readmission was analyzed.
Measurements
Data collected from the initial surgical admission for the entire cohort included gender, age, length of stay (LOS), region of country, and type of cardiac surgery. The presence of the following genetic syndromes was collected as well: trisomy 21, 22q11 syndrome, and Turner syndrome. The PHIS database often assigns a risk adjustment for congenital heart surgery (RACHS) score to each surgery on the basis of complexity, which was collected for each admission when available [21]. Patients with several operations and RACHS scores during the same admission were assigned the highest RACHS score during the admission for the analysis. Data collected during the readmission included age at readmission, time from surgery to readmission, time from discharge to readmission, LOS of readmission, mortality, interventions, and medications.
Data Analysis
Standard descriptive statistics were used to summarize the data and were expressed as mean ± standard deviation for normally distributed continuous variables, median [interquartile range (IQR)] for skewed continuous variables, and frequency with percentage for categorical variables. Univariable analysis via logistic regression was performed to determine the association between risk factors and the prevalence of readmissions with PE and PE interventions. Log-transformed values were used for skewed continuous variables (age, LOS, time from surgery to readmission, time from discharge to readmission). A multivariable logistic regression model was created to determine the influence of each of the risk factors after adjustment for significant covariates. All covariates with a p value ≤0.20 were considered for inclusion in the multivariable model. Highly collinear covariates (variance inflation factor >10) were not included together in the final multivariable model. In the event of two highly collinear variables, the variable that performed best in the post hoc goodness-of-fit testing (by Akaike information criteria) was ultimately included. In multivariable analysis, age at surgery was excluded due to collinearity with age at admission. RACHS scores were not included in the multivariable model as they were highly collinear with the list of surgical procedures. Since the goal was to determine which specific surgeries resulted in PE readmissions, the surgical procedure groupings were preferred over RACHS scores for the multivariable model. Odds ratios with 95% confidence intervals were reported. Final p values <0.05 were considered significant. All analyses were performed with STATA software (version 13.1, StataCorp, College Station, Texas).
Results
Total Patient Cohort
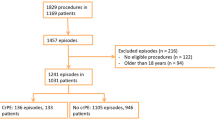
From January 1, 2003, through September 30, 2014, there were 142,633 admissions involving cardiac surgery in children (Table 2). Of this cohort, there were 1535 (1.1%) readmissions within 1 year with a PE. Out of the entire 142,633 admission cohort, the majority (54.7%) were male with a median age at initial surgical admission of 6.3 (IQR 0.56–46.5) months. The median age at surgery was 6.4 (IQR 1.1–46.6) months with an average LOS of 8 (IQR 4–21) days. Of the genetic diagnoses coded, trisomy 21 occurred most frequently (8.2%), followed by 22q11 syndrome (2.5%) and Turner syndrome (0.44%). Among the documented RACHS scores, a RACHS score of 3 (28.9%) was most common. The patients’ primary surgical interventions were condensed into fourteen categories, categorized for the purpose of this study (Fig. 1). Patients may have had multiple surgeries per admission and/or multiple ICD-9 procedure codes per surgery, so the number of surgeries exceeds the number of patients. Aortic arch intervention, including patent ductus arteriosus (PDA) surgery, was most common (41.5%), followed by atrial septal defect (ASD) surgical closure (23.5%), valve operations (19.4%), and ventricular septal defect (VSD) surgical closure (16.5%). Regions of the country were divided into Midwest, Northeast, South, and West, with the South having the most patients (33.4%) in this cohort.
Prevalence of surgical procedures and effusions per surgery. Fourteen groupings of surgical procedures with (1) the percentage of each surgery within the entire patient cohort (red bars) and (2) the percentage of each surgery among those patients who had PE readmission (blue bars). PDA patent ductus arteriosus, ASD atrial septal defect, VSD ventricular septal defect, EP electrophysiology, ToF tetralogy of Fallot, AVC atrioventricular canal, TGA transposition of the great arteries, TAPVR total anomalous pulmonary venous return
Comparison of Pericardial Effusion and No Effusion
The 141,098 surgical admissions that did not result in PE admission were compared to the 1535 resulting in readmissions. In a univariable analysis (Table 3), there were several variables associated with increased likelihood of readmission with PE: older age at initial cardiac surgical admission, shorter LOS of initial cardiac surgical admission, older age at surgery, and specific surgical procedures (heart transplantation, Glenn/Fontan, ASD, and valve procedures). Additionally, there were several variables associated with decreased likelihood of readmission with PE: RACHS scores 2 and 4 in comparison with RACHS score of 1 (which includes ASD surgery), surgery in the Midwest region, and specific surgical procedures (transposition of the great arteries, aortic arch and/or PDA, truncus arteriosus, VSD, conduit, and electrophysiology (EP) surgical procedures).
In multivariable analysis (Fig. 2), older age (odds ratio [OR] 1.17 per month, p < 0.001), trisomy 21 (OR 1.24, p = 0.015), geographic region (OR 1.33–1.48, p ≤ 0.001 for all regions in comparison with Midwest region), and specific surgical procedures [heart transplant (OR 1.82, p < 0.001), systemic-pulmonary artery shunt (OR 2.23, p < 0.001), and ASD surgical repair (OR 1.34, p < 0.001)] were identified as independent risk factors for readmission with PE, whereas aorta/PDA (OR 0.85, p = 0.013), VSD (OR 0.84, p = 0.024), conduit (OR 0.60, p < 0.001), and EP surgical procedures (OR 0.52, p < 0.001) were associated with decreased likelihood of PE readmission. The absolute risk of readmission for each of the above factors is shown in Table 4.
Readmission Cohort
For those subjects who were readmitted with PE, the median age at readmission was 25.6 (IQR 5.9–96.9) months (Table 2). The median time from surgery to readmission was 20 (IQR 13–42) days, and the time from discharge to readmission was 12 (IQR 6–29) days. The median LOS of the readmission was 5 (IQR 2–10) days, and the mortality rate was 0.65%. Accurate analysis of the cause of death could not be determined through the database. The most commonly used medications included diuretics (90.2%), anti-inflammatory medications (71.7%), and steroids (34.7%). Interventional procedures were performed in 44.2% of patients, most commonly pericardiocentesis (72.6%), followed by pericardiotomy (26.1%) and pericardiectomy (1.3%).
Comparison of Interventional and Medical Management
The 678 patients who required interventional management during the readmission were compared to the 857 who did not undergo an intervention (Table 5). In univariable analysis, longer time from discharge to readmission, longer LOS of the readmission, and ASD surgery were associated with PE intervention, while conduit surgery was associated with decreased likelihood of PE intervention. In multivariable analysis, factors independently associated with PE interventions included shorter LOS for the initial surgical admission (OR 0.85 per day, p = 0.008), longer LOS for the readmission (OR 1.37 per day, p < 0.001), and ASD surgery (OR 1.40, p = 0.005), while conduit surgery remained a factor associated with decreased likelihood of PE intervention (OR 0.55, p = 0.04).
Discussion
In this PHIS database study of children undergoing cardiac surgery, the prevalence of readmissions for PE was 1.1%, significantly less than previously published studies. For example, a prospective analysis of 336 children undergoing open heart surgery who underwent serial echocardiograms demonstrated PE in 23% of patients with 13% having moderate to large PE [12]. This discrepancy may be due to the fact that for a readmission with PE to be included in our study, the patients must have been readmitted to a PHIS-reporting hospital. As there likely were readmissions from our cohort to non-PHIS institutions, the 1.1% PE prevalence may be an underestimated value. Our study also only included patients who required readmission for PE, potentially selecting for patients with the most clinically significant PE. Lehto et al. similarly identified a lower prevalence of 2.5% in adults when analyzing readmissions but focused on PPS rather than specifically PE [22].
Pericardial Effusion Readmission
Potential risk factors for PE, or PPS in general, reported in the literature include predischarge PE [7], female gender [6, 12], warfarin use [12], pleural incision [6], Ross procedure [14], ASD surgery [20, 23], valve surgery [3], Fontan surgery [12, 15], atrioventricular canal surgery [15], winter months [14], summer months [5], lower platelet count [5], higher lymphocyte count [5], increased chest tube drainage [15], red blood cell transfusions [1], and renal insufficiency [1]. In the current larger study, several risk factors were found to be associated with PE readmissions. Despite the high degree of statistical difference detected in this large dataset, the absolute differences in risk are small.
Older age of patients at the initial cardiac surgical admission was a significant risk factor for PE readmission. There have been conflicting reports of the effects of age on PE in the literature. In adult studies, younger age was associated with increased risk of PPS [1] and increased risk of PE intervention [24]. Other studies have not found age to be a significant factor [7, 9]. In one pediatric study of ASD surgical repair, however, the risk of PE or PPS in children older than 5 years old was more than twice the risk of children younger than 5 years old [4]. We speculate that older children may be more likely to mount an immunologic response and therefore develop a significant PE. Moreover, PE that does not lead to tamponade may be more easily recognized in older children who are more likely to express symptoms and potentially be brought to medical attention.
Trisomy 21 was also identified as an independent risk factor for PE readmission with 1.3% developing PE. To our knowledge, trisomy 21 has not previously been identified as a risk factor for postoperative PE. Concolino et al. [25] performed a prospective analysis of children with trisomy 21 without cardiac disease with serial echocardiograms over 2 years. Patients with trisomy 21 were significantly more likely to develop a PE compared to healthy controls (28 vs. 2%). These findings have been replicated in other studies; hypothyroidism and abnormal myelopoiesis have been proposed as features of trisomy 21 subjecting them to higher risk of PE in general [26]. If these children in general have a greater propensity to develop PE, cardiac surgery and possibly the resulting inflammatory process may provide the trigger to develop a significant postoperative PE requiring readmission.
There was a statistically higher prevalence of PE readmissions in all geographic regions in comparison with the Midwest, where 0.82% were readmitted with a PE. It is quite possible that in the Midwest, patients may be readmitted to their local hospitals with PE, not necessarily a PHIS-reporting hospital. There would accordingly be fewer PE reports among Midwest PHIS hospitals. There may also be a different threshold for admission with varying management approaches.
Pericardial Effusion Readmission: Surgical Procedures
Heart transplantation was a significant risk factor for PE readmission with 2.3% developing PE. There have been a few reports of PE after heart transplantation in adults. Risk factors for postoperative PE have included a larger weight difference between the recipient and the donor, lack of previous median sternotomy, and longer duration and number of acute rejection episodes [27, 28]. The one pediatric study examining PPS and heart transplantation identified PPS in 7 out of 15 patients with lower cyclosporine levels and increased levels of activated helper T cells and cytotoxic T cells, suggestive of a role for cell-mediated immunity in the pathogenesis of PE [29].
An unexpected independent risk factor for PE admission was surgery that included a systemic-pulmonary shunt, such as the Blalock–Taussig (BT) shunt, with 1.2% developing PE. This finding is in contrast to Dalili et al. [15], who prospectively followed 486 children after various surgical procedures for congenital heart disease. The highest risk was after Fontan and atrioventricular canal defect repairs (29% for each), and out of 80 patients with a modified BT shunt, only one patient developed an effusion. It was surprising that the placement of a shunt in the current study was associated with a higher likelihood of postoperative PE, but many of the patients who underwent a BT shunt likely underwent other cardiac procedures during the same admission or same surgery, such as a Norwood procedure. We also surmise that manipulation of the heart and pericardium during the shunt procedure may be enough of a trigger for PE development. Additionally, there have been several studies describing the complication of seroma formation around BT shunts which are composed of polytetrafluoroethylene, presumably from the leakage of fluid through the graft wall [30]. In fact, there is a report of a patient who developed cardiac tamponade after placement of a systemic-pulmonary artery shunt secondary to serous leakage through the walls of the graft [31].
ASD surgical repair has classically been associated with increased risk of postoperative PE and PPS [20, 23], but there have been conflicting reports in more recent literature [15]. ASD surgical repair was indeed a significant risk factor in the current study with 1.3% developing PE. It has been previously proposed that chronic volume overload of the right atrium, as commonly seen in patients with ASDs, may allow for altered mechanics of PE production [32]. We surmise that the inflammatory reaction secondary to the pericardiotomy and right atriotomy combined with this chronic volume overload may have a role in PE production.
There were several surgical procedures associated with lesser risk of PE readmission, including EP surgical procedures (0.77% PE), aorta/PDA surgery (0.78% PE), VSD surgery (0.93% PE), and conduit surgery (0.70% PE). EP surgical procedures, such as pacemaker placement, may involve very small manipulations of the pericardium compared to larger surgical procedures. Many of the aortic arch and PDA surgical repairs involve a thoracotomy only and no pericardiotomy, and conduit surgery may potentially have limited intracardiac involvement, aside from the ventriculotomy for conduit insertion. VSD surgery may be approached similarly to an ASD repair, but the lack of right-sided volume overload may play a role in the lack of PE.
Pericardial Effusion Interventions
In multivariable analysis, factors independently associated with PE interventions included shorter LOS for the initial surgical admission, longer LOS for the readmission, and ASD surgery, with conduit surgery remaining as a factor associated with decreased likelihood of PE intervention. Nearly half of patients required intervention, primarily pericardiocentesis. This large number is consistent with the methodology of the current study to identify only those PE that were considered significant enough to warrant readmission. In regard to short LOS as a risk factor, for those patients with a shorter original LOS, the PE likely would have developed after discharge, thereby requiring readmission for intervention. For patients with a longer original LOS, however, the PE may have developed while still inpatient. Longer LOS of the readmission is likely related to the time associated with assessing the results of medical management, the pericardial intervention itself, and then evaluating the results prior to discharge. Longer LOS may just be a consequence of the PE intervention itself, rather than a true risk factor. Similar to the risk of PE readmissions, ASD surgery was a risk factor for PE intervention. We surmise that PE from ASD surgery may be less responsive to medical management than other surgical procedures. It is also possible that practitioners are more inclined to intervene for a PE after ASD surgery due to its well-described association with PPS and PE.
There have been numerous studies attempting either to prevent or to treat PPS and PE with a variety of medications. While some studies have advocated the effectiveness of prophylactic administration of nonsteroidal anti-inflammatory drugs (NSAIDs) [8], colchicine [11], or steroids [19], others have found no effect of these medications on the development of PPS and PE [9, 33]. NSAIDs, colchicine, and steroids have been advocated as effective treatments for PPS, along with the use of diuretics [20, 34, 35]. Indeed, this study identified diuretics, NSAIDs, and steroids as the most commonly used medications after readmission. Colchicine was used in only 1.8% of readmissions.
There are several limitations to this study, primarily due to the use of an administrative database. The database is reliant on the correct documentation of patient diagnostic and procedural codes. Additionally, for PE, there is not a single ICD-9 code. Several ICD-9 codes had to be used to determine the total number of patients who were diagnosed with pericardial disease and possible effusion. Readmissions were documented only at PHIS-reporting hospitals, and information about readmissions to non-PHIS hospitals was not available. Due to these factors, there was potential error in the estimated prevalence of PE readmissions. The severity of the PE could not be assessed, and trivial and severe effusions would be documented similarly. It was assumed that trivial PE would not be coded frequently as a diagnosis during an admission. There were frequently multiple diagnoses per admission, and it was not possible to determine if the PE was the primary cause of the readmission after surgery, only that a PE was present.
Conclusion
In this large administrative database of children undergoing cardiac surgery, readmissions for postoperative PE occurred after 1.1% of cardiac surgery admissions. The risk factors identified for PE readmissions, particularly the newly described risk factor of trisomy 21, may allow for improved risk stratification, family counseling, and earlier recognition of PE for children undergoing cardiac surgery.
Abbreviations
- PE:
-
Pericardial effusion
- PPS:
-
Postpericardiotomy syndrome
- PHIS:
-
Pediatric Health Information System
- ICD-9:
-
International classification of diseases, ninth revision
- LOS:
-
Length of stay
- RACHS:
-
Risk adjustment for congenital heart surgery
- IQR:
-
Interquartile range
- PDA:
-
Patent ductus arteriosus
- ASD:
-
Atrial septal defect
- VSD:
-
Ventricular septal defect
- EP:
-
Electrophysiology
- OR:
-
Odds ratio
- BT:
-
Blalock–Taussig
- ToF:
-
Tetralogy of Fallot
- AVC:
-
Atrioventricular canal
- TGA:
-
Transposition of the great arteries
- TAPVR:
-
Total anomalous pulmonary venous return
- M:
-
Months
- D:
-
Days
References
Lehto J, Gunn J, Karjalainen P, Airaksinen J, Kiviniemi T (2015) Incidence and risk factors of postpericardiotomy syndrome requiring medical attention: the Finland postpericardiotomy syndrome study. J Thorac Cardiovasc Surg 149:1324–1329
Soloff LA, Zatuchui J, Janton OH et al (1953) Reactivation of rheumatic fever following mitral commissurotomy. Circulation 8:481–493
DeScheerder I, Wulfrank D, Van Renterghem L et al (1984) Association of anti-heart antibodies and circulating immune complexes in the postpericardiotomy syndrome. Clin Exp Immunol 57:423–428
Jones DA, Radford DJ, Pohlner PG (2001) Outcome following surgical closure of a secundum atrial septal defect. J Paediatr Child Health 37:274–277
Miller RH, Horneffer PJ, Gardner TJ et al (1998) The epidemiology of the postpericardiotomy syndrome: a common complication of cardiac surgery. Am Heart J 116:1323–1329
Imazio M, Brucato A, Rovere ME et al (2011) Contemporary features, risk factors, and prognosis of the postpericardiotomy syndrome. Am J Cardiol 108:1183–1187
Heching HJ, Bacha EA, Liberman L (2015) Post-pericardiotomy syndrome in pediatric patients following surgical closure of secundum atrial septal defects: incidence and risk factors. Pediatr Cardiol 36:498–502
Sevuk U, Baysal E, Altindag R et al (2015) Role of diclofenac in the prevention of postpericardiotomy syndrome after cardiac surgery. Vasc Health Risk Manag 11:373–378
Gill PJ, Forbes K, Coe JY (2009) The effect of short-term prophylactic acetylsalicylic acid on the incidence of postpericardiotomy syndrome after surgical closure of atrial septal defects. Pediatr Cardiol 30:1061–1067
Finkelstein Y, Shemesh J, Mahlab K et al (2002) Colchicine for the prevention of postpericardiotomy syndrome. Herz 27:791–794
Imazio M, Brucato A, Rovere ME et al (2011) Colchicine prevents early postoperative pericardial and pleural effusions. Am Heart J 162:527–532
Cheung EW, Sa Ho, Tang KK et al (2003) Pericardial effusion after open heart surgery for congenital heart disease. Heart 89:780–783
Yip SB, Chau MC, Chow WH et al (1997) Pericardial effusion in adults undergoing surgical repair of atrial septal defects. Am J Cardiol 79:1706–1708
Prabhu AS, Ross RD, Heinert MR, Walters HL, Hakimi M (1996) Decreased incidence of postoperative pericardial effusions after cardiac surgery for congenital heart disease. Am J Cardiol 77(9):774–776
Dalili M, Zamani H, Aarabi-Moghaddam M (2012) Pericardial effusion after pediatric cardiac surgeries: a single center observation. Res Cardiovasc Med 1:28–32
Weitzman LB, Tinker WP, Kronzon I, Cohen ML, Glassman E, Spencer RC (1984) The incidence and natural history of pericardial effusion after cardiac surgery—an echocardiographic study. Circulation 69:506–511
Kuvin JT, Harati NA, Pandian NG, Bojar RM, Khabbaz KR (2002) Postoperative cardiac tamponade in the modern surgical era. Ann Thorac Surg 74:1148–1153
Clapp SK, Garson A Jr, Gutgesell HP, Cooley DA, McNamara DG (1980) Postoperative pericardial effusion and its relation to postpericardiotomy syndrome. Pediatrics 66:585–588
Sevuk U, Baysal E, Altindag R et al (2016) Role of methylprednisolone in the prevention of postpericardiotomy syndrome after cardiac surgery. Eur Rev Med Pharmacol Sci 20:514–519
Cantinotti M, Spadoni I, Assanta N et al (2014) Controversies in the prophylaxis and treatment of postsurgical pericardial syndromes: a critical review with a special emphasis on paediatric age. J Cardiovasc Med 15(12):847–854
Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI (2002) Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg 123:110–118
Lehto J, Kiviniemi TO, Gunn J et al (2016) Occurrence of postpericardiotomy syndrome admissions: a population-based registry study. Ann Med 48:28–33
Timmis GC, Gordon S, Ramos RG (1971) Recurrent postpericardiotomy syndrome. Its protracted nature and association with atrial septal defects. Mich Med 70:539–542
Alraies MC, Jaroudi WA, Shabrang C, Yarmohammadi H, Klein AL, Tamarappoo BK (2014) Clinical features associated with adverse events in patients with postpericardiotomy syndrome following cardiac surgery. Am J Cardiol 114(9):1426–1430
Concolino D, Pascuzzi A, Pietragalla E, Lia R, Strisciuglio P, Canepa S (2005) High prevalence of isolated pericardial effusion in Down Syndrome. Am J Med Genet 132A:331–332
Hirashima C, Eguchi Y, Kohmura Y, Minakami H, Sato I (2000) Isolated pericardial effusion and transient abnormal myelopoiesis in a fetus with Down’s Syndrome. J Obstet Gynaecol Res 26:303–306
Cilberto GR, Anjos MC, Gronda E et al (1995) Significance of pericardial effusion after heart transplantation. Am J Cardiol 76:297–300
Hauptman PJ, Couper GS, Aranki SF, Kartashov A, Mudge GH, Loh E (1994) Pericardial effusions after cardiac transplantation. J Am Coll Cardiol 23:1625–1629
Cabalka AK, Rosenblatt HM, Towbin JA et al (1995) Postpericardiotomy syndrome in pediatric heart transplant recipients. Immunologic characteristics. Tex Heart Inst J 22(2):170–176
Dogan OF, Duman U, Karagoz T, Ozkutlu S, Ersoy U (2005) Diagnosis of perigraft seroma formation by use of echocardiography after modified Blalock–Taussig shunt. Eur J Echocardiogr 6:385–387
Garcia-Guerata L, Burgueros M, Borches D, Gonzalez V, Jimenez J (1997) Cardiac tamponade after a systemic-pulmonary shunt complicated by serous leakage. Ann Thorac Surg 63:248–250
Just H, Mattingly TW (1968) Interatrial septal defect and pericardial disease: coincidence or causal relationship? Am Heart J 76(2):157–167
Mott AR, Fraser CD, Kusnoor AV et al (2001) The effect of short-term prophylactic methylprednisolone on the incidence and severity of postpericardiotomy syndrome in children undergoing cardiac surgery with cardiopulmonary bypass. J Am Coll Cardiol 37:1700–1706
Wilson NJ, Webber SA, Pettersen MW et al (1994) Double-blind placebo-controlled trial of corticosteroids in children with postpericardiotomy syndrome. Pediatr Cardiol 15:62–65
Hofneffer PJ, Miller RH, Pearson TA et al (1990) The effective treatment of postpericardiotomy syndrome after cardiac operations. A randomized placebo-controlled trial. J Thorac Cardiovasc Surg 100:292–296
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Elias, M.D., Glatz, A.C., O’Connor, M.J. et al. Prevalence and Risk Factors for Pericardial Effusions Requiring Readmission After Pediatric Cardiac Surgery. Pediatr Cardiol 38, 484–494 (2017). https://doi.org/10.1007/s00246-016-1540-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-016-1540-2