Abstract
To explore whether oral rehydration salts (ORS) is effective in the treatment of children with vasovagal syncope (VVS). One hundred and sixty-six consecutive patients with recurrent syncope and positive head-up tilt testing (HUTT) were recruited, randomly divided to conventional therapy (health education and tilt training) plus ORS (with 500 ml of water) group (Group I, 87 patients) and conventional therapy group (Group II, 79 patients). Therapeutic effect was evaluated by changes of syncopal episode and reperformed HUTT response. At the end of 6-month follow-up, syncopal episode did not reoccur in 49 (56.3 %) patients, decreased in 34 (39.1 %) patients, and had no obvious change or increased in four (4.6 %) patients in Group I, and the results were 31 (39.2 %), 37 (46.8 %), and 11 (14 %) in Group II, respectively. The difference was significant (χ 2 = 7.074, P < 0.05). When HUTT was reperformed, 57 (65.5 %) and 28 (35.4 %) patients had negative response and 30 (34.5 %) and 51 (64.6 %) patients had positive response, respectively, in Group I and Group II. The difference was also significant (χ 2 = 13.808, P < 0.01). In Group I, the two aspects had no difference between vasodepressor type and mixed type; however, syncopal episode had a significant difference between children aged ≤12 and >12 years (χ 2 = 6.371, P < 0.05); there was no difference in reperformed HUTT response. ORS with 500 ml of water is an effective therapy for VVS. It can be recommended as one of non- pharmacological treatment measures in children with VVS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Syncope is a transient loss of consciousness which is characterized by intermittent, reflex vasodilatation, and bradycardia that results in transient failure of blood pressure control and diminished cerebral perfusion [10, 14]. It may occur at all ages, especially in children and adolescents. Some studies indicated that 15 % of the population experienced at least one episode of syncope before adulthood [16]. Other studies estimated a higher rate that is up to 47 % of adolescent girls and 24 % of adolescent boys [7, 19]. Vasovagal syncope (VVS) is the most common form of syncope [17]. This condition may produce a wide variety of symptoms that include, but are not limited to, fatigue, dizziness, abdominal discomfort, muscle or joint pain, decreased mental concentration, and syncope. Although it is a functional cardiovascular disorder and has benign prognosis, it is emerging as a significant and potentially disabling condition for many children and adolescents. It may cause a great deal of missing of school work and social activities owing to incapacitating symptoms [12, 15, 20]. Therefore, the intervention of this common disorder is necessary.
The first-line intervention measures used in the management of VVS are non- pharmacological approaches, consisting of patient education, increased fluid and salt intake, physical counter pressure maneuvers, and so on [17, 23]. The most common way of increasing fluid and salt intake is increased dietary salt intake on a daily basis. But liberal addition of salt to meals has its shortcomings, such as that the quantity added is not easy to control and excessive salt intake may increase the risk of hypertension. Oral rehydration salts (ORS) as an easily feasible choice that is being used in the treatment of neurally mediated syncope instead of increased dietary salt intake [24, 26]. But the reports about the therapeutic effect of ORS were rare. In present study, we evaluated the therapeutic effect of ORS in children with VVS by the changes of syncopal episode and reperformed head-up tilt test (HUTT).
Patients and Methods
Patients
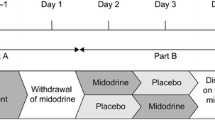
Two hundred consecutive patients with unexplained syncope were recruited, who saw a doctor at children syncope specialist outpatient unit of the Second Xiangya Hospital of Central South University between March 2009 and October 2013, and were randomized (1:1) to conventional therapy (health education and tilt training) plus ORS (dissolved in 500 ml of water) group (Group I) and conventional therapy group (Group II). Finally, 166 patients were included meeting the following criteria: (1) Experiencing syncope at least twice in the past 6 months. (2) Other diseases were ruled out on the basis of clinical history, physical examination, neurologic evaluation, routine laboratory tests, 12-lead electrocardiography, electroencephalogram, computed tomography, or magnetic resonance imaging of the brain. (3) Highly suspected VVS and referred to the tilt test room. The original HUTT was a positive response and indicated VVS. Underwent reperformed HUTT at the end of six-month follow-up.
The patients were 7 to 17 years old and were divided into ≤12-year group and >12-year group. The weight was from 20 to 56 kg. The detail demographic characteristics were described in Table 1. The reported duration of syncopal episode was from 1 week to 10 years, and the median time was 4 months. The number of syncopal episode was from 2 to more than 20 times.
This study was approved by the hospital ethical committee and conducted with the patients and their parents’ informed consent.
Head-up Tilt Test
After given informed parental consent, patient underwent HUTT. The test was performed in the morning in a quiet room after overnight fasting, in the condition of patient under continuous monitoring. Blood pressure, heart rate, and rhythm were continuously monitored. A three-lead electrocardiogram was continuously traced throughout the test. Blood pressure and electrocardiogram were recorded every 2 min or continuously if symptoms developed. Rescue equipment and first-aid drugs were available at all times in the test room, and an experienced nurse, who was blinded to which treatment group the subjects were in, executed the test.
HUTT was performed after an initial observation with patient in the supine position for 10 min. The test consisted of two consecutive phases. The first phase was baseline head-up tilt test (BHUT). The patient was tilted at 60° for 45 min without medication in accordance with the Westminster drug-free protocol [11]. If syncope did not develop, the patient underwent sublingual nitroglycerin-provocated head-up tilt test (SNHUT) keeping the same position for a further 20 min after given a sublingual nitroglycerin 4–6 μg/kg (maximum ≤0.3 mg). The end points of the test were positive response or completion of the protocol. If syncope occurred during the test, the tilt table was rapidly lowered to the supine position and the test was terminated.
The test was considered positive if syncope or pre-syncope that was associated with hypotension, bradycardia or both occurred. Syncope was defined as sudden transient loss of consciousness with inability to maintain postural tone and with spontaneous recovery. Pre-syncope was defined as the complex of premonitory signs and symptoms of imminent syncope (e.g., severe light-headedness, severe weakness, graying of vision, or hearing loss) with difficulty in maintaining postural tone. The estimation of the positive responses was according to our previous report [4] :(1) Systolic blood pressure <80 mmHg and/or diastolic blood pressure <50 mmHg. (2) Bradycardia: heart rate <75 beats per minute (bpm) for 4- to 6-year-old children, <65 bpm for 7- to 8-year-old children, <60 bpm for 8-year-old or older children, or sinus arrest >3 s. (3) Second-degree or higher atrioventricular block. (4) Atrioventricular junctional rhythm, including escape rhythm and accelerated idiorhythm. Three types of positive response were defined according to the changes in blood pressure and heart rate: (1) Mixed type: a blood pressure fall with a heart rate decreased or an abnormal rhythm. (2) Cardioinhibitory type: a rapid decrease in heart rate presenting as bradycardia or an abnormal rhythm. (3) Vasodepressor type: just a rapid decrease in blood pressure.
Health Education, Tilt Training, and Oral Rehydration Salts Treatment
All the patients accepted the health education and tilt training. The health education mainly focused on the etiology, benign prognosis of VVS and how to avoid potential triggers, such as prolonged standing, exposure to high temperatures, dehydration, coughing, physical pain, sudden onset of extreme emotions. At children syncope specialist outpatient unit, all patients and their parents were instructed to perform the tilt training by standing against a wall (with the united ankles 15 cm from the wall). Then, the patients performed maneuver at home twice a day for a planned duration of up to 30 min. The training was performed in a comfortable and safe environment to avoid the risk of physical trauma and was completed under the supervision of a family member. In addition, all 87 patients were given oral rehydration salts I in Group I. One package of ORS consisted of 11 g Glucose, 1.75 g NaCl, 0.75 g KCl, 1.25 g NaHCO3 (Manufacturer: Chinese Fuzhou Haiwang Pharmaceutical Co., Ltd; Approval number: H35021107). Dosage and Administration: one package was dissolved in 500 ml boiled water, drunk up in a day. ORS treatment was terminated at the end of 6-month follow-up. All 166 patients and their parents were instructed to record in detail any recurrent syncopal episode and required to visit the doctor once a month.
Evaluation of Therapeutic Effect
Therapeutic effect was evaluated according to the changes of recurrent syncopal episode and the result of reperformed HUTT. If the episode did not reoccur or decreased, it was thought to have an improvement of clinical symptoms and the therapy was effective. If the episode had no obvious reduction or increased, it was thought to have no improvement and the therapy was ineffective. All patients underwent the reperformed HUTT at the end of 6-month follow-up. If HUTT changed from the original BHUT positive to negative or SNHUT positive, or the original SNHUT positive to negative, it was thought to have an improvement of HUTT and the therapy was effective.
Statistical Analysis
The SPSS 17.0 software was used for statistical analysis. Continuous variables were expressed as mean ± SD, and differences between groups were compared by the method of T test. Categorical variables were presented as numbers and percentages and were compared by use of the Chi-square test. A P value of <0.05 was used to determine statistical significance.
Results
Therapeutic Effect
Syncopal episode did not reoccur in 49 (56.3 %) patients, decreased in 34 (39.1 %) patients, and had no obvious change or increased in four (4.6 %) patients in Group I, and when HUTT was reperformed, 57 (65.5 %) patients had negative response and 30 (34.5 %) patients had positive response. No patients complained of adverse reactions. In Group II, the episode did not reoccur in 31 (39.2 %) patients, decreased in 37 (46.8 %) patients, and had no obvious change or increased in 11 (14 %) patients, and when HUTT was reperformed, 28 (35.4 %) patients had negative response and 51 (64.6 %) patients had positive response. The recurrent syncopal episode was significantly different between the two groups (χ 2 = 7.074, P = 0.029), and the responses of reperformed HUTT also had significant difference (χ 2 = 13.808, P = 0.0002). The data are presented in Table 2.
Therapeutic Effect of Patients with Different Hemodynamic Types
The recurrent syncopal episode and the responses of reperformed HUTT at the end of follow-up both had not significant difference between vasodepressor type and mixed type (χ 2 = 5.919, P = 0.052; χ 2 = 0.422, P = 0.516, respectively). The data are displayed in Table 3.
Therapeutic Effect of Patients of Different Ages
The recurrent syncopal episode was significantly different between children aged ≤12 years group and >12 years group (χ 2 = 7.291, P = 0.026). The responses of repeated HUTT had no significant difference (χ 2 = 0.008, P = 0.929). The data are shown in Table 4.
Discission
Despite the benign course of VVS, it may impose substantial changes in lifestyle and cause profound psychological distress and physical impairment [15, 20]. Thus, the therapy aiming to prevent the recurrence and associated injuries and improve the quality of life is necessary and important.
Increased dietary salt intake was recommended as one of the first-line non-pharmacological treatment measures [17]. However, for liberal addition of salt in the diet, there was the risk of excessive salt intake and hypertension. On the basis of previous research results and the pathogenesis of hypovolemia, decreased orthostatic tolerance and abnormal baroreceptor reflex in the patients with VVS, it was thought that ORS treatment should be a logical approach for VVS. Therefore, ORS as the replacement of increased dietary salt intake was focused and used increasingly in the treatment of autonomous nerve-mediated syncope by the clinician. Xu et al. [24] showed that 96 % (27/28) of patients had improved clinical symptoms and 64 % (18/28) had improved HUTT results after ORS therapy combined with health education in children with neurally mediated syncope. The study of Zhang et al. [26] indicated that ORS treatment for 3 months was effective in 74.4 % (29/39) children patients with postural tachycardia syndrome according to the change of the symptom score. A multicenter study in China [3] proved that ORS was effective for some patients with VVS and postural tachycardia syndrome, but less effective than beta-receptor blocker.
Previous studies indicated that increased dietary salt intake or oral sodium chloride accompanied with water ingestion could treat successfully VVS. El-Sayed and Hainsworth [8] found that 70 % of the patients given salt and 30 % of the placebo group showed increase in plasma and blood volumes and in orthostatic tolerance, and decrease in baroreceptor sensitivity 8 weeks later. The study of Cooper and Hainsworth [5] had showed that salt loading of patients with VVS was likely to result in some subjective and objective signs of improvement. Salt loading caused a small but significant increase in mean pressure and significant increases in orthostatic tolerance and baroreceptor sensitivity. Mtinangi and Hainsworth [18] indicated that the effect of salt loading on orthostatic tolerance could be assessed quickly as an improvement was evident as few as 3 days. Furthermore, nonrandomized studies suggested that extra supplement of fluid and salt were also effective in children and the elderly subjects as well [21, 25].
The role of sodium chloride in the treatment of syncope has been sure. However, ORS also contains potassium chloride, sodium bicarbonate in addition to sodium chloride. Whether other components also play a role in the treatment of VVS is still unknown. He et al. [13] proved that both potassium chloride and potassium bicarbonate significantly improved endothelial function compared with placebo. Other evidence on the effect of potassium supplementation on the vasculature also demonstrated that an increase in potassium intake had beneficial effects on the cardiovascular system by a way of an improvement in endothelial function [9, 22]. So, we speculated that potassium as one of the ion components of ORS maybe also has an effect on cardiovascular function of patients with VVS.
It is widely accepted that the endothelium represents the largest functional organ of vasoregulation in the human body. Acid-base homeostasis is an important physiologic parameter that controls cell function, and change in pH can influence vascular tone by regulating endothelium and vascular smooth muscle cells. Bicarbonate is one of the main materials maintaining acid–base balance in the extracellular space and within the intracellular space [6]. The evidence of Boedtkjer and Aalkjaer [2] implied that disturbed intracellular pH either consequent to disturbed regulation or due to metabolic challenges needs to be taken into consideration as a mechanistic component of artery dysfunction and disturbed blood pressure regulation. It is still a mystery waiting to be disclosed whether the bicarbonate component of ORS influences vascular function by regulating subtly pH of the internal environment of the patients with VVS.
ORS is very easy to get in different levels of hospitals and the cost is low. So ORS can be prescribed instead of increased dietary salt intake for children and adolescents if the initial HUTT indicated a diagnosis of VVS.
There was a doubt in this study whether the 500 ml of water played a role for the reported improvement. Although the report [1] showed that an increased daily intake of fluid, without an accompanying high dose of salt, had no measurable beneficial effect on tolerance to head-up tilting in patients with neurocardiogenic syncope, a comparison would be better between 500 ml of water with no electrolytes in conventional therapy group and 500 ml of water with added ORS in conventional therapy plus ORS group daily.
Conclusions
ORS with 500 ml of water is an effective therapy for VVS. It can be recommended as one of non-pharmacological treatment measures in children and adolescents with VVS.
References
Bellard E, Fortrat JO, Custaud MA, Victor J, Greenleaf J, Lefthériotis G (2007) Increased hydration alone does not improve orthostatic tolerance in patients with neurocardiogenic syncope. Clin Auton Res 17(2):99–105
Boedtkjer E, Aalkjaer C (2012) Intracellular pH in the resistance vasculature: regulation and functional implications. J Vasc Res 49(6):479–496. doi:10.1159/000341235
Chen L, Du JB, Zhang QY et al (2007) A multicenter study on treatment of autonomous nerve-mediated syncope in children with beta-receptor blocker. Zhonghua Er Ke Za Zhi 45(12):885–888
Chu W, Wang C, Lin P, Li F, Wu L, Xie Z (2014) Transient aphasia: a rare complication of head-up tilt test. Neurol Sci 35(7):1127–1132. doi:10.1007/s10072-014-1664-1
Cooper VL, Hainsworth R (2002) Effects of dietary salt on orthostatic tolerance, blood pressure and baroreceptor sensitivity in patients with syncope. Clin Auton Res 12(4):236–241
Crimi E, Taccone FS, Infante T, Scolletta S, Crudele V, Napoli C (2012) Effects of intracellular acidosis on endothelial function: an overview. J Crit Care 27(2):108–118. doi:10.1016/j.jcrc.2011.06.001
Driscoll DJ, Jacobsen SJ, Porter CJ, Wollan PC (1997) Syncope in children and adolescents. J Am Coll Cardiol 29(5):1039–1045
El-Sayed H, Hainsworth R (1996) Salt supplement increases plasma volume and orthostatic tolerance in patients with unexplained syncope. Heart 75(2):134–140
Fang Y, Mu JJ, He LC, Wang SC, Liu ZQ (2006) Salt loading on plasma asymmetrical dimethylarginine and the protective role of potassium supplement in normotensive salt-sensitive asians. Hypertension 48(4):724–729
Fenton AM, Hammill SC, Rea RF, Low PA, Shen WK (2000) Vasovagal syncope. Ann Intern Med 133(9):714–725
Fitzpatrick AP, Theodorakis G, Vardas P, Sutton R (1991) Methodology of head-up tilt testing in patients with unexplained syncope. J Am Coll Cardiol 17(1):125–130
Harris JP, Garfunkel LC, Wycoff C et al (1999) Cardiovascular aspects of neurally mediated syncope in adolescents. Pediatr Res 45:4A
He FJ, Marciniak M, Carney C et al (2010) Effects of potassium Chloride and potassium bicarbonate on endothelial function, cardiovascular risk factors, and bone turnover in mild hypertensives. Hypertension 55(3):681–688. doi:10.1161/HYPERTENSIONAHA.109.147488
Kapoor WN (2000) Syncope. N Engl J Med 343(25):1856–1862
Linzer M, Pontinen M, Gold DT, Divine GW, Felder A, Brooks WB (1991) Impairment of physical and psychosocial function in recurrent syncope. J Clin Epidemiol 44(10):1037–1043
McHarg ML, Shinnar S, Rascoff H, Walsh CA (1997) Syncope in childhood. Pediatr Cardiol 18(5):367–371
Moya A, Sutton R, Ammirati F et al (2009) Guidelines for the diagnosis and management of syncope (version 2009). Eur Heart J 30(21):2631–2671. doi:10.1093/eurheartj/ehp298
Mtinangi BL, Hainsworth R (1998) Early effects of oral salt on plasma volume, orthostatic tolerance, and baroreceptor sensitivity in patients with syncope. Clin Auton Res 8(4):231–235
Pilcher TA, Saarel EV (2014) A teenage fainter (dizziness, syncope, postural orthostatic tachycardia syndrome). Pediatr Clin N Am 61(1):29–43. doi:10.1016/j.pcl.2013.09.009
Rose MS, Koshman ML, Spreng S, Sheldon R (2000) The relationship between health-related quality of life and frequency of spells in patients with syncope. J Clin Epidemiol 53(12):1209–1216
Shannon RP, Wei JY, Rosa JY, Epstein FH, Rowe JW (1986) The effect of age and sodium deletion on cardiovascular response to orthostasis. Hypertension 8(5):438–443
Shi DC, Mu JJ, Chen ER et al (2006) Endothelial function evaluation in salt-sensitive normotensive and mild hypertensive subjects and effects of potassium supplement. Zhonghua Xin Xue Guan Bing Za Zhi 34(1):38–41
Wieling W, Colman N, Krediet CT, Freeman R (2004) Nonpharmacological treatment of reflex syncope. Clin Auton Res 14(Suppl 1):62–70
Xu Y, Lin P, Wang C et al (2013) Investigation of 24-hour blood pressure monitoring for evaluating treatment outcome of nerve-mediated syncope in children. Zhongguo Dang Dai Er Ke Za Zhi 15(6):458–461
Younoszai AK, Franklin WH, Chan DP, Cassidy SC, Allen HD (1998) Oral fluid therapy: a promising treatment for vasodepressor syncope. Arch Pediatr Adolesc Med 152(2):165–168
Zhang FW, Liao Y, Li XY, Chen L, Jin HF, Du JB (2011) Therapies for postural tachycardia syndrome in children. Zhonghua Er Ke Za Zhi 49(6):428–432
Acknowledgments
The work was supported by the National Twelfth Five-Year Plan for Science and Technology Support of China (2012BAI03B03), the Natural Science Foundation of Hunan Province of China (13JJ5014).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chu, W., Wang, C., Wu, L. et al. Oral Rehydration Salts: An Effective Choice for the Treatment of Children with Vasovagal Syncope. Pediatr Cardiol 36, 867–872 (2015). https://doi.org/10.1007/s00246-015-1097-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-015-1097-5