Abstract
Head-up tilt test (HUT) is widely used as a diagnostic tool. It reproduces vasovagal attacks in many susceptible patients. Although it is known to be safe and well tolerated, it is a procedure with potential neurologic complications. We observed that it could cause transient aphasia in some patients. To explore clinical characteristics and possible pathogenesis of aphasia induced by HUT, we reviewed the data of patients undergoing HUT in our hospital. 13 patients experienced transient aphasia in 3,488 cases. According to the hemodynamic changes, the incidence in vasodepressor, mixed, cardioinhibition and the negative response were 6.67, 5.52, 0 and 1.14 ‰ orderly, and not significantly different among the groups. It had significant difference between the positive response and the negative response and between vasodepressor and the negative response (both p < 0.05). The incidence in adults was significantly higher than that in children (<18 years) (p < 0.01), but not different between female and male. The average onset time was 11.33 ± 6.66 min (range 4–17 min) during baseline HUT or 4.90 ± 2.69 min (range 2–10 min) during sublingual nitroglycerin-provocated HUT. The duration was 3–60 min, except for one who was completely relieved of the disorder 4 h later. In conclusions, there is a risk of provoking transient aphasia during HUT. It reminds that performer should alert the possibility of transient aphasia during the test, especially when the patient is an adult and has a positive response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head-up tilt test (HUT) was first described as a diagnostic test for neurally mediated syncope in 1986 [1]. Since then, tilt testing protocols had varied with respect to many factors [2–6]. HUT is now in widespread use as a useful objective test for neurally mediated syncope and a research tool. Although it is proved to be safe and well tolerated, it is a procedure with potential neurologic complications, in spite that the incidence is low and most of neurologic complications are transient and reversible [7, 8]. In the clinical work, we observed that HUT aroused transient aphasia in few patients. In this context, we reviewed the data of patients experiencing HUT in our hospital, analyzed the clinical features of the patients who suffered from transient aphasia due to HUT and explored the possible pathogenesis.
Patients and methods
Patients
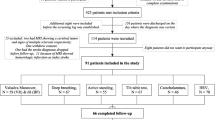
3,488 cases were studied, with unexplained syncope or presyncope, who saw a doctor at syncope specialist out-patient or were hospitalized in our hospital and underwent HUT between September 2000 and May 2013. The age of cases was from 2 to 79 years, mean 19.28 ± 15.05 years. Male and female was, respectively, 1,654 cases, 1,834 cases. 2,428 cases were younger than 18 years, aged from 2.00 to 17.83 years, mean 10.80 ± 2.94 years. 1,060 cases were older than 18 years, aged from 18 to 79 years, mean 38.68 ± 13.59 years.
Head-up tilt test
As a diagnostic tool, HUT was carried out in our hospital in September 2000. After giving informed consent, patient underwent HUT. The test was performed in the morning in a quiet room after overnight fasting, in the condition of patient under continuous monitoring. Blood pressure, heart rate, and rhythm were continuously monitored. A three-lead electrocardiogram was continuously traced throughout the test. Blood pressure and electrocardiogram were recorded every 2 min or continuously if symptoms developed. Rescue equipment and first-aid drugs were available at all times in the test room, and an experienced nurse executed the test.
HUT was performed after an initial observation with the patient in the supine position for 10 min. The test consisted of two consecutive phases. The first phase was baseline head-up tilt test (BHUT). The patients were tilted at 60° for 45 min without medication in accordance with the Westminster drug-free protocol [3]. If syncope did not develop, the patient underwent sublingual nitroglycerin-provocated head-up tilt test (SNHUT) keeping the same position for a further 20 min after given a sublingual nitroglycerin 0.3 mg [4]. The end points of the test were positive response and completion of the protocol. If syncope occurred during the test, the tilt table was rapidly lowered to the supine position and the test was terminated.
The test was considered positive if syncope or presyncope that was associated with hypotension, bradycardia, or both occurred. Syncope was defined as sudden transient loss of consciousness with inability to maintain postural tone and with spontaneous recovery. Presyncope was defined as the complex of premonitory signs and symptoms of imminent syncope (e.g., severe light-headedness, severe weakness, graying of vision, or hearing loss) with difficulty in maintaining postural tone. For the adult patients, the positive responses were classified according to the modification of the original VASIS classification [9]: (1) mixed: heart rate fell at the time of syncope, but the ventricular rate did not fall to <40 beats per minute (bpm), or fell to <40 bpm for <10 s with or without asystole of <3 s. Blood pressure fell before the heart rate fell. (2) Cardioinhibition without asystole:Heart rate fell to a ventricular rate <40 bpm for more than 10 s, but asystole of more than 3 s did not occur. Blood pressure fell before the heart rate fell. (3) Cardioinhibition with asystole: asystole occured for more than 3 s. Heart rate fall coincided with or preceded blood pressure fall. (4) Vasodepressor: heart rate did not fall more than 10 % from its peak at the time of syncope. The estimation of the positive responses in children was according to Qingyou et al. [10]: (1) systolic blood pressure <80 mmHg and/or diastolic blood pressure <50 mmHg. (2) Bradycardia: heart rate <75 bpm for 4- to 6-year-old children, <65 bpm for 7- to 8-year-old children, <60 bpm for 8-year-old or older children or sinus arrest >3 s. (3) Second-degree or higher atrioventricular block. (4) Atrioventricular junctional rhythm, including escape rhythm and accelerated idiorhythm. Three patterns of positive response were defined according to the changes in blood pressure and heart rate: (1) mixed patterns: a blood pressure fall with a heart rate decreased or an abnormal rhythm. (2) Cardioinhibitory patterns: a rapid decrease in heart rate presenting as bradycardia or an abnormal rhythm. (3) Vasodepressive patterns: just a rapid decrease in blood pressure.
Evaluation of hearing and cognition of the patients with transient aphasia
The patients were thought to be experiencing aphasia if they still could not speak after recovering from syncope or presyncope, after the tilting table was lowered to the horizontal position. Hearing and cognitive functions were evaluated by asking the patients some questions, letting the patients read a text and look at pictures. The patients answered “yes” by nodding or “no” by shaking head. If they could speak, the patients were asked to tell if they could hear during anepia, what the text and the pictures demonstrated, what feeling they experienced, and whether they were with hearing or cognition impairment before HUT.
Analysis of history data and HUT records
The history data and HUT records of 3,488 cases were read retrospectively; the data of the patients whose HUT records revealed transient aphasia were analyzed in detailed.
Statistical analysis
The SPSS 17.0 software was used for statistical analysis. Continuous variables were expressed as mean ± SD and differences between groups were compared by use of T test. Categorical variables were presented as numbers and percentages and were compared by use of the χ 2 test. A p value of <0.05 was used to determine statistical significance.
Results
The incidences of transient aphasia in patients with different hemodynamic changes and their differences
13 patients (3.73 ‰) showed transient aphasia in 3,488 cases and 5 of them had manifested transient aphasia in the spontaneous episodes of syncope. According to the hemodynamic changes, vasodepressor, mixed, cardioinhibition and the negative response were 1,349 cases, 362 cases, 29 cases and 1,748 cases, respectively. The incidence of transient aphasia in each type were 6.67 ‰ (9/1,349), 5.52 ‰ (2/362), 0(0/29) and 1.14 ‰ (2/1,748) orderly. The difference among the groups was not significant (χ 2 = 6.714, p > 0.05).The occurrence rate was significantly different between patients with a positive response and patients with a negative response [6.32 ‰ (11/1,740) vs 1.14 ‰ (2/1,748), χ 2 = 4.978, p < 0.05], between patients with a vasodepressive response and patients with a negative response (χ 2 = 5.104, p < 0.05).The difference was not found in the remaining comparisons between two groups. The distributions of the hemodynamic types and transient aphasia in patients are presented in Table 1.
Hemodynamic changes, onset and duration time of the patients with transient aphasia
In 13 patients, 11 patients had a positive response (2 cases during BHUT, 9 cases during SNHUT). Two patients had a negative response. The mean onset time was 11.33 ± 6.66 min (range 4–17 min) during BHUT or 4.90 ± 2.69 min (range 2–10 min) during SNHUT. The duration of aphasia was from 3 to 60 min, except for one who was completely relieved of the disorder 4 h later, the median time was 20 min. The detailed data are shown in Tables 2, 3.
Distributions of gender and age of the patients with transient aphasia
The patients enduring transient aphasia consisted of 4 males (30.8 %) and 9 females (69.2 %), with a mean age 32.62 ± 19.25 years (range 10–64 years). The incidence of adults was significantly higher than that of children [8.49 ‰ (9/1,060) vs. 1.65 ‰ (4/2,428), χ 2 = 7.554, p < 0.01)]. The difference between male and female did not reach statistical significance [2.42 ‰ (4/1,654) vs. 4.91 ‰ (9/1,834), χ 2 = 0.858, p > 0.05].
Clinical manifestations of transient aphasia
All the patients performing transient aphasia were without hearing impairment and the disturbance of cognition when HUT was executed, and hearing and cognition were also normal during aphasia. The clinical manifestations of 13 patients were not completely alike, except transient aphasia. After regaining the ability of speaking, they all emphatically told that they wanted to talk, but could not speak out and could understand what the operator or someone else was talking about. The two patients with a negative response, one was a 20-year-old girl who could not speak suddenly at the fourth minute during BHUT, with normal blood pressure, heart rate and electrocardiogram and without any symptoms and signs of syncope or presyncope. She was immediately put back to the supine position and could speak fluently 6 min later. Another was a 42-year-old woman who had the similar experience lasting 5 min. The transient aphasia arose in another eleven patients accompanying the appearance of syncope or presyncope induced by hypotension, bradycardia, or both. Taking one patient for example, a 12-year-old girl, the first HUT presented a vasodepressive response without impact on speech function. After two weeks, the second HUT was executed. Syncope could not be reproduced during BHUT. So she was given a sublingual nitroglycerin 0.3 mg. At the fifth minute, the patient manifested restlessness, uncomfort, palpitation, blurring of vision, pallor. The blood pressure was not measured out, heart rate and electrocardiogram were normal. The tilting table was promptly lowered down; the patient was subjected to the loss of consciousness during this course. After the tilting table was put back to the supine position, the blood pressure was 63/28 mmHg. Two minutes later, blood pressure returned to normal, and the symptoms described above disappeared completely, but the patient was not still able to speak. The evaluation of hearing and cognitive function was normal. Twenty-five minutes later, she could speak fluently.
Discussion
Aphasia is a neurological term that generally refers to a focal neurologic deficit. It is the most common in stroke patients. Aphasia caused by the diseases other than stroke had been reported sporadically, and was generally transient [11–13]. In the clinical work, we observed that transient aphasia could be also caused by HUT.
HUT drives a withdrawal of sympathetic activity and an increase of vagal tone by changing body position from supine to tilt. It reproduces a transient, self-limited loss of consciousness and postural tone caused by reduction of blood flow to the reticular activating system, the neuronal network in the brain stem responsible for maintaining consciousness [14]. The working mechanism activated in a specific episode can differ in each patient and probably also in the same patient in different episodes, in spite that the final consequence is a compound of bradycardia and hypotension [15]. So the mechanism of transient aphasia due to the episode of syncope aroused by HUT may be different. Up to now, the mechanism behind aphasia remains unclear.
Some scholars believe that hypoperfusion of language function areas is involved in the pathogenesis of aphasia. The classic speech centers are believed to be located in Wernicke’s area and Broca’s area in the brain. Hillis and his co-workers [16–18] demonstrate that adequate perfusion for tissue function in Wernicke’s area (BA 22) is necessary for lexical–semantic tasks. The specific regions of hypoperfusion on magnetic resonance perfusion-weighted imaging are strongly associated with specific deficits in language processing. More severe deficits in lexical semantics reflect more severe hypoperfusion of BA 22 in the absence of infarct of BA 22. Hypoperfusion of specific areas of the brain can result in specific lexical deficits that improve with reperfusion of those same areas. Kessler et al. [19] show that the increase of brain blood flow can improve recovery of language functions in the left transverse temporal gyrus, the left superior temporal gyrus (Wernicke’s region), and the triangular part of the left frontal gyrus (Broca’s area) in the piracetam-treated aphasia patients.
Cerebrovascular autonomic dysregulation may be also responsible for the transient aphasia. Grubb et al. [20] report that patients with upright tilt-induced syncope concomitant with the development of hypotension, bradycardia, or presyncopal symptoms, reveal a significant decrease in middle cerebral artery diastolic velocity and mean velocity, an unchanged systolic velocity, a significant increase in pulsatility index and resistance index. After the patients are lowered to the supine position, the return of blood pressure and heart rate to normal levels as well as the return of consciousness in spite, the cerebral vessels continue to maintain an unchanged systolic and decreased diastolic flow pattern for 1–2 s afterward followed by a vasodilation pattern. So they propose that abnormal baroreceptor responses result in a derangement of cerebral autoregulation with paradoxical vasoconstriction in the face of increasing hypotension in patients with upright tilt-induced syncope. Claydon et al. [21] indicate that cerebrovascular autoregulation in patients with posturally related syncope is less effective than in healthy controls. Abnormalities of autoregulation of the cerebral circulation are associated with predisposition to syncope. Carey et al. [22] show that no deterioration in dynamic cerebral autoregulation during orthostatic stress in nonsyncopal control subjects, dynamic cerebral autoregulation deteriorates in patients and control subjects during presyncope and remains impaired during the immediate postsyncopal period.
Regional differences in cerebral circulation in neurally mediated syncope may participate in the occurence of the transient aphasia. Ilgin et al. [23] demonstrate that passive orthostatism can cause left hemispheric dominant reduction in cerebral perfusion, whereas subjects with a positive test had regional differences in brain perfusion, with a significantly lower perfusion of the right peri-insular posterior parietal and temporal regions.
In this study, the results suggested that the incidences of aphasia were significantly different between the positive response and the negative response and between vasodepressor and the negative response. So we thought transient aphasia of these patients was probably associated with above mechanisms. Moreover, in another two patients the aphasia bursted suddenly in the case that the blood pressure, heart rate and rhythm were all normal, and the patients were without any symptoms and signs of syncope or presyncope. We confused what caused it. May be psychogenic origin should be thought because the previous research had suggested that HUT could lead to psychological disorder [24] and psychogenic factors could cause nonorganic speech and language abnormalities [25].
The results also indicated that the incidence of transient aphasia in adults was significantly higher than that in children. We considered that it was possibly related to the potential higher risk of cerebrovascular disease in adults, such as local cerebral vasospasm, an embolic transient ischemic attack, or other cerebrovascular accident. The computed tomography or magnetic resonance imaging of the brain was not performed, so it was merely the speculation.
In conclusions, our investigation suggests that there is a risk of provoking aphasia in the performance of HUT. The aphasia is temporary without permanent impairment of language function. It reminds that the operators need to alert the possibility of transient aphasia during the test, especially when the patient is an adult and has a positive response. The pathogenesis of transient aphasia due to HUT needs to be further explored.
References
Kenny RA, Ingram A, Bayliss J, Sutton R (1986) Head-up tilt: a useful test for investigating unexplained syncope. Lancet 1(8494):1352–1355
Fitzpatrick A, Sutton R (1989) Tilting towards a diagnosis in recurrent unexplained syncope. Lancet 1(8639):658–660
Fitzpatrick AP, Theodorakis G, Vardas P, Sutton R (1991) Methodology of head-up tilt testing in patients with unexplained syncope. J Am Coll Cardiol 17(1):125–130
Raviele A, Menozzi C, Brignole M, Gasparini G, Alboni P, Musso G, Lolli G, Oddone D, Dinelli M, Mureddu R (1995) Value of head-up tilt testing potentiated with sublingual nitroglycerin to assess the origin of unexplained syncope. Am J Cardiol 76(4):267–272
Oraii S, Maleki M, Minooii M, Kafaii P (1999) Comparing two different protocols for tilt table testing: sublingual glyceryl trinitrate versus isoprenaline infusions. Heart 81(6):603–605
Raviele A, Giada F, Brignole M, Menozzi C, Marangoni E, Manzillo GF, Alboni P (2000) Comparison of diagnostic accuracy of sublingual nitroglycerin test and low-dose isoproterenol test in patients with unexplained syncope. Am J Cardiol 85(10):1194–1198
O’Dwyer C, Bennett K, Langan Y, Fan CW, Kenny RA (2011) Amnesia for loss of consciousness is common in vasovagal syncope. Europace 3(7):1040–1045. doi:10.1093/europace/eur069
Zaidi A, Crampton S, Clough P, Fitzpatrick A, Scheepers B (1999) Head-up tilting is a useful provocative test for psychogenic non-epileptic seizures. Seizure 8(6):353–355
Brignole M, Menozzi C, Del Rosso A, Costa S, Gaggioli G, Bottoni N, Bartoli P, Sutton R (2000) New classification of haemodynamics of vasovagal syncope: beyond the VASIS classification. Analysis of the pre-syncopal phase of the tilt test without and with nitroglycerin challenge. Vasovagal syncope international study. Europace 2(1):66–76
Qingyou Z, Junbao D, Jianjun C, Wanzhen L (2004) Association of clinical characteristics of unexplained syncope with the outcome of head-up tilt tests in children. Pediatr Cardiol 25(4):360–364
Kim DH, Choi CH, Lee JH, Lee JI (2010) Transient global aphasia with hemiparesis following cerebral angiography: relationship to blood brain barrier disruption. J Korean Neurosurg Soc 48(6):524–527. doi:10.3340/jkns.2010.48.6.524
Katz RB, Packer C (2014) Lithium toxicity presenting as transient transcortical motor aphasia: a case report. Psychosomatics 55(1):87–91. doi:10.1016/j.psym.2013.05.004
Maini B, Narayan R, Bhardwaj AK, Sharma PD (2012) Expressive aphasia: an isolated and reversible complication of cerebral malaria in a child. J Vector Borne Dis 49(2):117–118
Franco Folino A (2007) Cerebral autoregulation and syncope. Prog Cardiovasc Dis 50(1):49–80
Folino AF (2006) Cerebral autoregulation in neutrally mediated syncope: victim or executioner? Heart 92(6):724–726
Hillis AE, Barker P, Beauchamp N, Winters B, Mirski M, Wityk R (2001) Restoring blood pressure reperfused Wernicke’s area and improved word meaning in subacute stroke. Neurology 56(5):670–672
Hillis AE, Kane A, Tuffiash E, Ulatowski JA, Barker PB, Beauchamp NJ, Wityk RJ (2001) Reperfusion of specific brain regions by raising blood pressure restores selective language functions in subacute stroke. Brain Lang 79(3):495–510
Hillis AE, Wityk RJ, Tuffiash E, Beauchamp NJ, Jacobs MA, Barker PB, Selnes OA (2001) Hypoperfusion of Wernicke’s area predicts severity of semantic deficit in acute stroke. Ann Neurol 50(5):561–566
Kessler J, Thiel A, Karbe H, Heiss WD (2000) Piracetam improves activated blood flow and facilitates rehabilitation of poststroke aphasic patients. Stroke 31(9):2112–2116
Grubb BP, Gerard G, Roush K, Temesy-Armos P, Montford P, Elliott L, Hahn H, Brewster P (1991) Cerebral vasoconstriction during head-up right tilt-induced vasovagal syncope. A paradoxic and unexpected response. Circulation 84(3):1157–1164
Claydon VE, Hainsworth R (2003) Cerebral autoregulation during orthostatic stress in healthy controls and in patients with posturally related syncope. Clin Auton Res 13(5):321–329
Carey BJ, Manktelow BN, Panerai RB, Potter JF (2001) Cerebral autoregulatory responses to head-up tilt in normal subjects and patients with recurrent vasovagal syncope. Circulation 104(8):898–902
Ilgin L, Olgunturk R, Kula S, Turan L, Tunaoğlu S, Temiz H, Gokcora N, Gücüyener K (2005) Brain perfusion assessed by 99-Tc-ECD SPECT imaging in pediatric patients with neurally mediated reflex syncope. Pacing Clin Electrophysiol 28(6):534–539
Kataoka H (2011) A case of orthostatic tachycardia syndrome presenting with panic attack during tilt table testing. Cardiology 120(2):91–94. doi:10.1159/000333131
Binder LM, Spector J, Youngjohn JR (2012) Psychogenic stuttering and other acquired nonorganic speech and language abnormalities. Arch Clin Neuropsychol 27(5):557–568. doi:10.1093/arclin/acs051
Acknowledgments
The work was supported by the National Twelfth Five-Year Plan for Science and Technology Support of China (2012BAI03B03), The Natural Science Foundation of Hunan Province of China (13JJ5014).
Conflict of interest
There is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chu, W., Wang, C., Lin, P. et al. Transient aphasia: a rare complication of head-up tilt test. Neurol Sci 35, 1127–1132 (2014). https://doi.org/10.1007/s10072-014-1664-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-014-1664-1