Abstract
To determine the clinical manifestations and interfamilial variability of patients diagnosed with a mitochondrial cardiomyopathy, we reviewed the charts of 14 patients with cardiomyopathy out of 59 patients with mitochondrial disorders who attended the mitochondrial disease clinic at Wolfson Medical Center from 1996 to 2001. All patients underwent a metabolic evaluation including blood lactate, pyruvate, carnitine, and amino acids and urine organic acids. Respiratory chain enzymes were assessed in 10 patients. The mitochondrial DNA (mtDNA) was assessed for mutations.
The age at presentation ranged between 6 months and 24 years. Six of the patients died, 5 from heart failure. The cardiomyopathy was hypertrophic in 10 and dilated in 4. Conduction and rhythm abnormalities were present in 6. Eleven patients had family members with mitochondrial disorders. All the patients had additional involvement of one or more systems. Seven patients exhibited a deficiency of a respiratory chain enzyme in the muscle. The MELAS mtDNA point mutation (3243) was found in one patient. Blood lactic acid levels were increased in 5. Brain MRI abnormalities were observed in 4.
Conclusions
Mitochondrial dysfunction frequently affects the heart and may cause both hypertrophic and dilated cardiomyopathy. The cardiomyopathy is usually a part of a multisystem involvement and may rarely be isolated. The course may be stable for many years, but rapid deterioration may occur. Understanding the biochemical and genetic features of these diseases will enable us to comprehend the clinical heterogeneity of these disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Disorders of energy production are quite common among the inborn errors of metabolism [29]. Mitochondrial disorders comprise a heterogeneous group of diseases with multisystem presentations that affect ATP production [4, 6, 15, 22]. The most frequently and severely affected organs are those that depend on high-rate aerobic metabolism: brain, skeletal and cardiac muscle, sensory organs, and kidney. Mitochondrial cardiomyopathy can result from mutations in either nuclear or mitochondrial encoded genes, thus demonstrating the complexity of the inheritance patterns (e.g., maternal, autosomal recessive).
Cardiomyopathy is a frequent manifestation of mitochondrial respiratory chain disorders [12]. In a previous article we described cardiovascular involvement in 5 of 36 children with mitochondrial disorders [16]. Abnormal oxidative phosphorylation in childhood may lead to a hypertrophic or dilated cardiomyopathy [13]. When the cardiomopathy is hypertrophic it may eventually evolve into a dilated form during the course of the disease, a form more frequently reported in adults suffering from this condition [26]. Point mutations in the mitochondrial DNA (mtDNA) transfer ribonucleic acid (tRNA) genes have been associated with both hypertrophic and dilated cardiomyopathy [14].
Mitochondrial cardiomyopathy can either be isolated or associated with multisystem manifestations. Interestingly, different family members may present with different symptoms [14].
Several articles describe the molecular abnormalities in mitochondrial cardiomyopathies [8, 12, 13, 14, 26, 28]. However, there are only case reports describing the clinical phenotype and relation to the genotype (reviewed in [19]). We describe the clinical manifestations, interfamilial variability, and molecular, biochemical, and morphological findings in 14 patients with a mitochondrial cardiomyopathy.
Patients
We reviewed the charts of 59 patients with mitochondrial disorders who attended the mitochondrial disease clinic at Wolfson Medical Center from 1996 to 2001. Twelve patients with cardiomyopathy were identified; their charts and the charts of two deceased siblings of two of the patients were reviewed.
The diagnosis of cardiomyopathy was based on a pediatric cardiologic assessment plus echocardiography and ECG. The diagnosis of a mitochondrial disorder was given based on the presence of at least one of the following:(1) deficiency of respiratory chain enzymes in muscle, fibroblasts, or platelets; (2) evidence of mtDNA mutations or deletions; (3) characteristic changes such as ragged red muscle fibers (RRF) on trichrome Gomori stain, or decreased succinate dehydrogenase or cytochrome C oxidase staining in muscle biopsy; (4) evidence of abundant abnormal ultrastructure of mitochondria; (5) excretion of abnormal organic acids in urine characteristic of a known mitochondrial syndrome (for example, 3-methyl glutaconic acid); (6) a first-degree relative with a proven mitochondrial disease.
All patients underwent a metabolic evaluation including blood lactate, pyruvate, carnitine, and amino acids and urine organic acids. The respiratory chain enzymes were assessed in 10 patients (9 in a muscle biopsy and 1 in a cardiac biopsy). We assessed mtDNA for mutations suspected from the clinical presentation in 6 patients.
Methods
Biochemical Studies
Five percent muscle homogenate in 0.25 M, sucrose, 20 mM Tris, pH 7.2, 40 mM KCl, 2 mM EGTA, and 1-mg/mL albumin was prepared in Teflon-glass homogenizer from frozen specimens. The homogenate was centrifuged at 600 g for 10 min and the supernatant was used for enzyme determinations after being frozen/thawed (×3) in liquid nitrogen. Respiratory chain enzyme activities of complexes I+III (rotenone-sensitive NADH cytochrome c oxidoreductase), II+III (antimycine-sensitive succinate-cytochrome c oxidoreductase), II (succinate dehydrogenase), IV (cytochrome c oxidase), V (ATPase oligomycin sensitive), and activity of the marker enzyme citrate synthase in skeletal muscle were measured spectrophotometrically as described previously [9]. Activities of respiratory chain enzymes (specifically COX and ADP-stimulated respiration) in cybrids fused from the mitochondria of patient 5 and a donor nucleus were assayed (courtesy of Dr. Josef Houstek).
Molecular Studies
Total DNA was extracted from blood and fibroblasts using the Puregene kit (Gentra, Minneapolis, MN, USA), according to the manufacturer’s instructions. Muscle DNA was extracted from 50 mg of skeletal muscle collected from the quadriceps vastus intermedius by open biopsy. The frozen specimen was solubilized, digested with proteinase K, and further extracted as above. Ten-microgram samples of total DNA were analyzed by agarose gel electrophoresis following a 24-h digestion with PvuII. The Southern blot was hybridized as follows: 100 ng of a 519-bp polymerase chain reaction (PCR) product of mitochondrial DNA (expanding nucleotides 4981–5500) was radiolabeled with 32P-dCTP labeled using random prime kit (Roche). Hybridization was performed at 65°C. The blot was washed twice with 2× SSC, 0.2% SDS, and once with 1× SSC, 0.1% SDS, exposed, and read by a phosphoimager. For detection of point mutations, mtDNA in the appropriate region was amplified by PCR as described previously [21]. We analyzed the most frequent point mutations associated with maternally inherited cardiomyopathy [16], T9997C, A3260G, A4300G, T15889C, A15902G, A5600T, A3243G, C3303T, A4295G, and A8344G, in 5 patients. In patient 1 we also looked for point mutations associated with deafness: A1555G, A4269G, A7445G, Ins C7472, C4320T, and A8363G. In patient 11 we looked for the MELAS (Myopathy, Encephalopathy, Lactic Acidosis and Stroke-like episodes) mutation 3243 in mitochondrial tRNALeu (UUR) . HSP60 and 10 genes were sequenced (courtesy of Dr. Jens Jacobs Hansen) in patient 5. The G4.5 gene was sequenced in patient 7 (courtesy of Avraham Shaag).
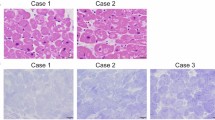
Histological and Electron Microscopy Analysis
Ten micrometers of muscle sections were stained with hematoxylin and eosin, modified Gomori trichrome, PAS, Sudan black B, NADH-tetrazolium reductase, succinate dehydrogenase, cytochrome oxidase, ATPase at pH 9.4, and after preincubation at pH 4.3 and 4.6. An additional specimen was fixed in 4% glutaraldehyde in phosphate buffer and prepared for electron microscopy by standard methods. An autopsy was performed in patient 10.
Results
The clinical manifestations of the 14 patients (6 males and 8 females) are summarized in Table 1. The laboratory studies are described in Table 2. The age at presentation ranged between 6 months and 24 years. Six of the patients died, 4 in the first 2 years and 2 at an older age (9 and 16 years). Six patients had life-threatening cardiac insufficiency: 5 died from heart failure and 1 stabilized with Idebenone treatment. Three patients had moderate cardiac insufficiency, while 5 had no functional cardiac impairment. One patient with Leigh syndrome died from respiratory failure following severe neurological and cardiological deterioration.
The onset of the clinical signs and symptoms of cardiac failure was variable. Seven patients presented in the first year of life. The cardiomyopathy was hypertrophic in 10 and dilated in 4. Conduction and rhythm abnormalities were present in 6.
Our patients come from 10 pedigrees: 11 patients had family members with mitochondrial disorders, there were 4 pairs of siblings and 2 mothers and their sons. Patients 1 and 2 had two siblings with sensorineural deafness but no cardiomyopathy.
All the patients had additional involvement of one or more systems: clinical myopathy in 11, failure to thrive/short stature in 7, mental retardation in 4, gastrointestinal symptoms in 2, epileptic seizures in 2, stroke-like episodes in 2, sensorineural deafness in 2, diabetes in 1, blindness in 1, and premature ovarian failure in 1.
A specific mitochondrial syndrome was confirmed in 6 patients. Patients 5 and 10 had a clinical diagnosis of Leigh syndrome. Patient 10 developed normally until 3 months, when he developed chronic diarrhea and failure to thrive. He became hypotonic, and 2 months later generalized myoclonic seizures occurred. He died at the age of 8 months as a result of respiratory arrest. His lactate was elevated, but respiratory chain enzymes in muscle and flbroblasts were normal. A peripheral muscle biopsy was normal and structural mitochondrial abnormalities were found only in the retina, gastrointestinal tract, and heart muscle. This infant had progressive neurological involvement with autopsy findings diagnostic of Leigh syndrome. Two siblings had died in infancy from neurological deterioration, and the parents were consanguineous. Patient 5 was diagnosed at the age of 6 months. She presented with hypertrophic cardiomyopathy and Wolff-Parkinson-White syndrome, hypotonia, extra pyramidal movements, FTT, and basal ganglia lesions in her MRI. Low activity of complex V was found in the muscle biopsy and low complexes IV and V were found in her flbroblasts. Sequencing of the mtDNA encoding ATPase and COX subunits was negative. The enzyme deficiency was restored using cybrid cell lines that were generated from fibroblast mitochondria from the patient and rho(0) cells, thus confirming autosomal recessive inheritance in this family and enabling accurate genetic counseling.
Patient 11 presented with stroke-like episodes, non-insulin-dependent diabetes mellitus (NIDDM), and deafness, and a cardiac evaluation revealed cardiac hypertrophy. The classical 3243 MELAS (Mitochondrial Encephalopathy Lactic Acidosis and Stroke-like episodes) mutation was found. Patient 7 had Barth syndrome (neutropenia and short stature), and in patients 1, 2, and 12 the clinical diagnosis was maternally inherited myopathy and cardiomyopathy. Patient 1 presented in the first year of life with cardiomyopathy. Her brother, patient 2, died at the age of 9 years from cardiomyopathy that was first detected at the age of 3 years. Both children were hypotonic with slow motor development. Two siblings had sensorineural deafness without cardiomyopathy, and the mother complains of muscle cramps. Decreased activity of complexes I+III and II+III (which are coenzyme Q dependent) were found in the myocardium of patient 3, thus pointing to coenzyme Q (CoQ) depletion [10].
A muscle biopsy was performed in 10 patients. Ragged red fibers (RRF) were found in 4. Abnormal ultrastructure of the mitochondria was observed in 2.
Seven patients exhibited a deficiency of a respiratory enzyme in the muscle: two complex IV, one complex I, two complex II, one complexes IV+V, and one complex III. In patient 3, decreased activities of complexes I+III and II+III were found in the myocardium. Activities of respiratory chain enzymes in cybrids from patient 5 were normalized, thus indicating a nuclear origin of the defect.
The MELAS mtDNA point mutation (3243) was found in one patient. No mtDNA mutations were found in the other 6 patients. No mutations were found in HSP60 and 10. A leucine 63-to-proline mutation was found in the G 4.5 gene in the patient with Barth syndrome.
Blood lactic acid levels were increased in 5 patients; urinary 3-methyl glutaconic acid was elevated in 2 patients. Brain MRI abnormalities were observed in 4 patients: brainstem and basal ganglia changes in the patient with Leigh syndrome, cortical atrophy in patients 4 and 6, porencephaly in patient 4, and white matter changes in patient 11. Microscopic examination of the brain in patient 10 showed numerous symmetrical foci of blood vessel proliferation and prominent astrocytes and microglia cells in the pons, medulla, and basal ganglia. The neurons within these foci had a variable appearance, with hyperchromatic, homogeneous nuclei and condensed basophilic perikaryon.
Discussion
Cardiomyopathy was diagnosed in 14 of 59 patients attending a mitochondrial disorder clinic. Cardiomyopathy was not isolated in any of the patients, but part of a mitochondrial disease involving at least one other system. In 4 patients, cardiomyopathy was the presenting symptom. A few groups have reported cardiac manifestations in patients diagnosed with respiratory chain disorders [3, 15, 16, 24]. Guenthard et al. [8] reviewed the clinical course, morphology, and pathophysiological mechanisms in 21 historical cases of mitochondrial cardiomyopathy since 1975, and their additional patient. All cases showed concentric hypertrophy of the myocardium without obstruction. In most patients the cardiomyopathy was diagnosed early in infancy and death occurred before the age of 2 years (16 of 22). A diagnosis of a specific mitochondrial syndrome (MELAS, Leigh syndrome) was made in 5 patients, but there was an additional myopathy or encephalopathy in all other patients. The most common respiratory enzyme defects were deficiencies of complex IV and I, found in 17 of the patients. Molecular tests of mtDNA point mutation or deletions were not obtained. Marin-Garcia et al. [13] examined skeletal muscle of young children presenting with cardiomyopathy for changes in the respiratory chain enzymes and mutations in the mtDNA. Seven of the 8 patients showed neonatal onset of cardiomyopathy, 4 patients had lactic acidosis, and all had generalized muscle weakness and died. A marked deficiency in specific enzyme activity was found in 6 of 8 patients’ muscle biopsy: complexes I, III, IV, and V. No pathogenic mutations associated with cardiomyopathy were detected, and no evidence for mtDNA deletions or depletion was found. The authors suggested that mitochondrial analysis of skeletal muscle from patients with cardiomyopathy should be an intrinsic part of the overall clinical evaluation.
Isolated cardiomyopathy is not described among patients with mitochondrial disorders attending metabolic clinics. However, when patients with this entity are referred from cardiology clinics for metabolic evaluation, mitochondrial causes can be found. Rustin et al. [20] described 3 patients with isolated hypertrophic cardiomyopathy presenting in the first few weeks of life, which were found to have respiratory enzyme deficiencies in endomyocardial biopsies. In a recent article, Marin-Garcia et al. [13] found mitochondrial respiratory chain enzyme abnormalities in a group of 16 children with primary, sporadic, nonfamilial cardiomyopathy and normal phenotypic features. They found decreased activities of complexes I, III, IV, and V but not of II, the only complex that is entirely nuclear encoded. Sequence analysis of cardiac mtDNA revealed heteroplasmic mtDNA mutations in cytb, tRNAArg, and ND5 in 4 patients, and 4 patients exhibited marked reduction in cardiac mtDNA levels. The authors suggest that the basis for the respiratory chain enzyme abnormalities can be explained in these patients as a result of either pathogenic mtDNA mutations or depletion of mtDNA.
Mitochondrial cardiomyopathy can result from mutations in either nuclear or mitochondrial-encoded genes of respiratory chain enzymes. Both point mutations and deletions in the mtDNA have been described. MtDNA deletions have been found especially in tissues with slow or nondividing cells such as heart or brain. The most common deletion is a 5- or 7.4-kb deletion, although as many as 200 deletions have been reported so far. It is unclear whether the deletions are primary and cause the cardiomyopathy or represent somatic mutations that are secondary to an increase in oxygen free radicals, which are generated in the dysfunctional heart [26].
In addition to mutations in the subunits that are encoded by mtDNA, there are many reports of mitochondrial cardiomyopathy due to abnormalities in nuclear DNA genes. Recently a fatal infantile cardiomyopathy was associated with mutation in SCO1, which is involved in the assembly of COX subunits into a functional complex IV [25]. Mutations in SURF1 (another COX assembly gene) were found in Leigh syndrome with cardiomyopathy [23].
Our two Leigh patients demonstrated the variable clinical presentations in this syndrome. Both died in the first 2 years of life. This is a progressive neurodegenerative disorder with onset in infancy or early childhood and a characteristic neuropathology. Although primarily a neurological disorder, other systemic manifestations including hypertrophic cardiomyopathy are infrequently described in this syndrome. Rahman et al. [17] described cardiac problems in 3 of 67 patients with Leigh or Leigh-like syndrome. This syndrome is associated with multiple enzymatic defects in energy production. Specific point mutations in the mtDNA, including ATPase 6 and tRNALYS genes, and in nuclear genes encoding subunits of oxidative enzymes or 248 chaperones (SURF1), have been reported. [17, 23, 24]. In a number of cases no genetic loci have been clearly identified. There is no clear genotype–phenotype correlation in Leigh syndrome.
MIMyCa, a maternally inherited syndrome presenting with a variable combination of skeletal and heart muscle failure associated with a heteroplasmic A3260G transition in the tRNALeu(UUR) gene, was described in 1991 [27]. Since then many more maternally transmitted mutations have been described [21]. We assumed maternal inheritance in 3 of our families. However, this was confirmed only in the patient with the 3243 MELAS mutation. Cardiac involvement is described in 20–30% of the patients with this syndrome and is therefore not the predominant symptom [21]. Since there were ragged red fibers in two other muscle biopsies, we suspect that they may harbor a yet-unfound mitochondrial tRNA mutation.
The inheritance in patients 3 and 4 (a mother and her son) was initially assumed to be maternal, since both the patient’s mother and son were affected and the son’s muscle biopsy showed ragged red fibers. However, the mother’s endomyocardial biopsy showed deficiency of the quinone-dependent complexes, and none of the previously described mtDNA mutations associated with maternally inherited myopathy and cardiomyopathy were detected. There was a dramatic (although transient) improvement in her cardiac failure following treatment with Idebenone, a CoQ analog [10]. Therefore, we presume an abnormality in CoQ metabolism in this family. Inheritance may be dominant or X-linked, since the son is more severely involved than both his mother and grandmother. This family demonstrates the difficulties in establishing the mode of inheritance that has important implications for accurate genetic counseling.
Patient 7 presented at the age of 11 months with dilated cardiomyopathy, short stature, and neutropenia and was clinically diagnosed as having Barth syndrome (BTHS). This is an X-linked disorder characterized by the associated features of cardiac and skeletal myopathy, short stature, and neutropenia [1]. The clinical manifestations of the disease are quite variable, but cardiac failure as a consequence of cardiac hypertrophy is a constant finding and is a common cause of death in the first months of life. The gene responsible for the syndrome was recently found to be G4.5, on Xq28 [5]. The diagnosis was recently confirmed in our patient when a leucine 63-to-proline mutation in the G4.5 gene was found. X-linked infantile cardiomyopathies with cardiac dilatation, lacking other symptoms of BTHS, have been reported and it has been proposed that BTHS may be allelic with both X-linked endocardial fibroelastosis and other infantile cardiomyopathies [5]. These observations are important for clinicians evaluating male patients with isolated cardiomyopathy especially when there is a family history that might imply X-linked inheritance.
Cytochrome C oxidase (COX) deficiency was found in the muscle biopsy of patients 8 and 9, who were siblings and presented with severe cardiomyopathy, myopathy, and neurological involvement. Three mitochondrial and nine nuclear genes encode COX. COX deficiency is genetically heterogeneous, and current diagnostic methods cannot easily distinguish between mitochondrial and nuclear defects [18]. COX deficiency, either total or partial, is the most commonly recognized respiratory chain defect in childhood [3], Since most of the COX subunits are nuclear encoded and additional nuclear-encoded factors are essential for assembly of the complex, it is likely that most cases of COX deficiency are caused by nuclear gene mutations. The parents of our two patients were not related but were from the same ethnic origin, Jewish-Iraqi, and there were no clinical symptoms in the maternal side, and so we suspect a nuclear-encoded COX deficiency. This mode of inheritance is also indicated in patients 13 and 14, who had complex II deficiency, which is entirely nuclear encoded.
The clinical presentations differed not only among different syndromes but also among patients from the same family. Patients 1 and 2 both presented with severe cardiomyopathy, but the male sibling was diagnosed at the age of 3 years and died at the age of 9 from cardiac failure, despite treatment, while his sister, who presented at 1 year of age with cardiomyopathy stabilized and has no signs of heart decompensation at the age of 9. Their two siblings have moderate deafness, but their hearts are normal. Patients 3 and 4 (mother and son) demonstrate an even more diverse clinical presentation: the mother has a cardiomyopathy and myopathy, while the son also has severe mental retardation, failure to thrive, deafness, and MRI changes. Patients 8 and 9 had a similar multisystem presentation, but the sister was much more severely affected and she died in fulminant lactic acidosis at the age of 16 years. The mother with MELAS (patient 11) has a son with profound mental retardation but no cardiomyopathy.
In conclusion, mitochondrial dysfunction frequently affects the heart and may cause both hypertrophic and dilated cardiomyopathy. The cardiomyopathy is usually part of multisystem involvement. Isolated mitochondrial cardiomyopathy has rarely been described in young patients who did not have the chance to develop manifestations in other organs. The course may be stable for many years, but rapid deterioration may occur. Consequently, as the biochemical and genetic features of the mitochondrion and mitochondrial diseases are becoming better defined, the pathophysiologic characteristics of mitochondrial heart disease are becoming better understood [7].
References
PG Barth HR Scholte JA Berden et al. (1983) ArticleTitleAn X-linked mitochondrial disease affecting cardiac muscle, skeletal muscle and neutrophil leucocytes. J Neurol Sci 2 327–355 Occurrence Handle10.1016/0022-510X(83)90209-5
D Bonnet P Lonlay Particlede I Gautier et al. (1998) ArticleTitleEfficiency of metabolic screening in childhood cardiomyopathies. Eur Heart J 19 790–739 Occurrence Handle10.1053/euhj.1997.0818 Occurrence Handle1:STN:280:DyaK1czot1OnsA%3D%3D Occurrence Handle9717014
U Caruso A Adami E Bertini et al. (1996) ArticleTitleRespiratory-chain and pyruvate metabolism defects: Italian collaborative survey on 72 patients. J Inherit Metab Dis 19 143–148 Occurrence Handle1:CAS:528:DyaK28XjsFWht7g%3D Occurrence Handle8739951
L Clark (1992) ArticleTitleMitochondrial disorders in pediatrics. Clinical biochemical and genetic implications. Pediatr Clin N Am 39 319–334
P D’Adamo L Fassone A Gedeon et al. (1997) ArticleTitleThe X-linked gene G4.5 is responsible for different infantile dilated cardiomyopathies. Am J Hum Genet 61 862–867 Occurrence Handle1:CAS:528:DyaK2sXmslCns7k%3D Occurrence Handle9382096
S DiMauro C Moraes (1993) ArticleTitleMitochondrial encephalomyopathies. Arch Neurol 50 1197–1208 Occurrence Handle1:STN:280:ByuD38bmsFY%3D Occurrence Handle8215979
S DiMauro M Hirano (1998) ArticleTitleMitochondria and heart disease. Curr Opin Cardiol 13 190–197 Occurrence Handle1:STN:280:DyaK1czhtlKhug%3D%3D Occurrence Handle9649942
J Guenthard F Wyler B Fowler R Baumgartner (1995) ArticleTitleCardiomyopathy in respiratory chain disorders. Arch Dis Child 72 223–226 Occurrence Handle1:STN:280:ByqB28%2FhsV0%3D Occurrence Handle7741568
IJ Holt AE Harding RK Petty JA Morgan-Hughes (1990) ArticleTitleA new mitochondrial disease associated with mitochondrial DNA heteroplasmy. Am J Hum Genet 46 428–433 Occurrence Handle1:STN:280:By%2BC2sfgslE%3D Occurrence Handle2137962
T Lerman-Sagie P Rustin D Lev et al. (2001) ArticleTitleDramatic improvement in mitochondrial cardiomyopathy following treatment with idebenone. J Inherit Metab Dis 24 28–34 Occurrence Handle10.1023/A:1005642302316 Occurrence Handle1:CAS:528:DC%2BD3MXivVajsrY%3D Occurrence Handle11286379
J Marin-Garcia M Ananthakrishnan Korson MJ Goldenthal A Perez-Atayde (1996) ArticleTitleCardiac mitochondrial dysfunction in Leigh syndrome. Pediatr Cardiol 17 387–389 Occurrence Handle10.1007/s002469900084 Occurrence Handle1:STN:280:BymA2snlvVU%3D Occurrence Handle8781089
J Marin-Garcia MJ Goldenthal (1997) ArticleTitleMitochondrial cardiomyopathy: molecular and biochemical analysis. Pediatr Cardiol 18 251–260 Occurrence Handle10.1007/s002469900169 Occurrence Handle1:STN:280:ByiA38%2FnsF0%3D Occurrence Handle9175519
J Marin-Garcia R Ananthakrishnan MJ Goldenthal JJ Filiano Perez-Atayde (1999) ArticleTitleMitochondrial dysfunction in skeletal muscle of children with cardiomyopathy. Pediatrics 103 456–459 Occurrence Handle10.1542/peds.103.2.456 Occurrence Handle1:STN:280:DyaK1M7is1Grtw%3D%3D Occurrence Handle9925841
J Marin-Garcia R Ananthakrishnan MJ Goldenthal ME Pierpont (2000) ArticleTitleBiochemical and molecular basis for mitochondrial cardiomyopathy in neonates and children. J Inherit Metab Dis 23 625–633 Occurrence Handle10.1023/A:1005638231195 Occurrence Handle1:CAS:528:DC%2BD3cXnsFGju7w%3D Occurrence Handle11032337
A Munnich A Rotig D Chretien JM Saudubray V Cormier P Rustin (1996) ArticleTitleClinical presentations of mitochondrial disorders in childhood. Eur J Pediatr 155 262–274 Occurrence Handle10.1007/s004310050399 Occurrence Handle1:STN:280:BymB287os1c%3D Occurrence Handle8777918
A Nissenkorn A Zeharia D Lev et al. (1999) ArticleTitleMultiple presentations of mitochondrial disorders. Arch Dis Child 81 209–214 Occurrence Handle1:STN:280:DyaK1MvitFGntg%3D%3D Occurrence Handle10451392
S Rahman RB Blok HH Dahl et al. (1996) ArticleTitleLeigh Syndrome: clinical features and biochemical and DNA abnormalities. Ann Neurol 39 343–351 Occurrence Handle1:CAS:528:DyaK28XisFyrsbw%3D Occurrence Handle8602753
S Rahman BD Lake JW Taanman et al. (2000) ArticleTitleCytochrome oxidase immunohistochemistry: clues for genetic mechanisms. Brain 123 591–600 Occurrence Handle10.1093/brain/123.3.591 Occurrence Handle10686181
P Rustin D Chretien T Bourgeron et al. (1994) ArticleTitleBiochemical and molecular investigations in respiratory chain deficiencies. Clin Chim Acta 228 35–51 Occurrence Handle10.1016/0009-8981(94)90055-8 Occurrence Handle1:CAS:528:DyaK2cXltlWjsLc%3D Occurrence Handle7955428
P Rustin J Lebidois D Chretien et al. (1994) ArticleTitleEndomyocardial biopsies for early detection of mitochondrial disorders in hypertrophic cardiomyopathies. J Pediatr 124 224–228 Occurrence Handle1:STN:280:ByuC3s3pslM%3D Occurrence Handle8301427
FM Santorelli A Tessa G D’amati C Casali (2001) ArticleTitleThe emerging concept of mitochondrial cardiomyopathies. Am Heart J 141 E1 Occurrence Handle10.1067/mhj.2001.112088 Occurrence Handle1:STN:280:DC%2BD3M7lsVWrsQ%3D%3D Occurrence Handle11136504
J Shoffner D Wallace (1990) ArticleTitleOxidative phosphorylation diseases. Disorders of two genomes. Adv Hum Genet 19 267–330 Occurrence Handle1:CAS:528:DyaK3MXltlaktbg%3D Occurrence Handle2193491
V Tiranti K Hoertnagel R Carrozzo et al. (1998) ArticleTitleMutations of SURF-1 in Leigh syndrome associated with cytochrome c oxidase deficiency. Am J Hum Genet 63 1609–1621 Occurrence Handle10.1086/302150 Occurrence Handle1:CAS:528:DyaK1MXltF2qsw%3D%3D Occurrence Handle9837813
MH Tulinius E Holme B Kristiansson NG Larsson A Oldfors (1991) ArticleTitleMitochondrial encephalomyopathies in childhood. II. Clinical manifestations and syndromes. J Pediatr 119 251–259 Occurrence Handle1:STN:280:By6A3MfjvVU%3D Occurrence Handle1861210
I Valnot JC Kleist-Retzow Particlevon A Barrientos et al. (2000) ArticleTitleA mutation in the human heme A: farnesyltransferase gene (COX10) causes cytochrome c oxidase deficiency. Hum Mol Genet 9 1245–1249 Occurrence Handle10.1093/hmg/9.8.1245 Occurrence Handle1:CAS:528:DC%2BD3cXjsF2hur0%3D Occurrence Handle10767350
DC Wallace (2000) ArticleTitleMitochondrial defects in cardiomyopathy and neuromuscular disease. Am Heart J 139 IssueID2 pt 3 S70–S85 Occurrence Handle10.1067/mhj.2000.103934 Occurrence Handle1:CAS:528:DC%2BD3cXhtlKitb0%3D Occurrence Handle10650320
M Zeviani C Gellera C Antozzi et al. (1991) ArticleTitleMaternally inherited myopathy and cardiomyopathy: association with mutation in mitochondrial DNA tRNA (Leu) (UUR). Lancet 20 143–147 Occurrence Handle10.1016/0140-6736(91)90136-D
M Zeviani C Mariotti C Antozzi GM Fratta P Rustin A Prelle (1995) ArticleTitleOXPHOS defects and mitochondrial DNA mutations in cardiomyopathy. Muscle Nerve 3 S170–S174 Occurrence Handle1:STN:280:ByqA38jhsVY%3D Occurrence Handle7603520
M Zeviani B Bertagnolio G Uziel (1996) ArticleTitleNeurological presentations of mitochondrial diseases. J Inherit Metab Dis 19 504–520 Occurrence Handle1:STN:280:ByiD3sfpvFc%3D Occurrence Handle8884574
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lev, D., Nissenkorn, A., Leshinsky-Silver, E. et al. Clinical Presentations of Mitochondrial Cardiomyopathies. Pediatr Cardiol 25, 443–450 (2004). https://doi.org/10.1007/s00246-003-0490-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-003-0490-7