Abstract
We evaluated the demographic features, etiologic risk factors, treatment strategies, and outcome of the infants and children with urolithiasis (UL). A retrospective multicenter study was conducted including 23 Pediatric Nephrology centers in Turkey. The medical records of 2513 children with UL were reviewed. One thousand, three hundred and four boys and 1209 girls (1.1:1) were reported. The mean age at diagnosis was 39.5 ± 35 months (0.4–231 months), and 1262 patients (50.2%) were in the first year of life (infants). Most of the cases with infantile UL were diagnosed incidentally. Microlithiasis (< 3 mm) was found in 794 patients (31.6%), and 64.5% of the patients with microlithiasis were infants. Stones were located in the pelvis-calyces in 63.2% (n: 1530) of the cases. The most common stone type was calcium oxalate (64.6%). Hypocitraturia was the most common metabolic risk factor (MRF) in children older than 12 months, but in infancy, hypercalciuria was more common. Fifty-five percent of the patients had received at least one medical treatment, mostly potassium citrate. At the end of a year’s follow-up, most of the patients with microlithiasis (85%) showed spontaneous remission. The rate of spontaneous stone resolution in infants was higher than in children. Spontaneous remission rate was higher in cases with MRF ( − ) stones than in MRF ( +) stones. However, remission rate with medical treatment was higher in cases with MRF ( +) stones. This study represents the results of a large series of infants and children with UL and showed that there are several differences such as underlying metabolic and anatomic abnormalities, clinical course, and stone remission rates between infants and children with urinary stone disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urolithiasis (UL) is an important clinical health problem with increasing incidence in childhood, particularly in infancy [1]. The incidence, metabolic composition of the stones, and clinical findings of UL in children vary considerably between different geographic regions of the world. Urolithiasis in Turkey is an endemic disorder, affecting 10–20% of the children [2, 3]. UL in children has multifactorial etiology including mainly metabolic disorders (hypercalciuria, hypocitraturia, hyperoxaluria, hyperuricosuria and cystinuria, etc.), recurrent urinary tract infections, urinary tract anomalies causing urinary stasis (ureteropelvic junction (UPJ) obstruction, vesicoureteral reflux (VUR), ureterovesical (UV) stenosis, etc.), ethnic origin, genetics, climate, and changes in nutrition patterns [1,2,3,4].
Determining the underlying risk factors and special treatments may reduce possible stone recurrence and prevent morbidity in children [4]. The most common etiological risk factors of pediatric UL in Turkey were reported to be metabolic (33–83.2%) and anatomic abnormalities (8–32%), and the most frequently reported metabolic abnormalities were hypercalciuria and hypocitraturia [5,6,7,8]. It was reported that stone recurrence is higher in children having a metabolic risk factor (MRF) [1, 4,5,6,7,8,9].
Therapeutical approach in the setting of non-obstructive small stones involves specific medical treatments which are administered for the underlying metabolic disorder, such as potassium citrate or Shohl’s solution for urine alkalization, tiopronin for cystinuria, and hydrochlorothiazide for hypercalciuria, etc. For the treatment of obstructive pelvic-calyx or ureteral stones, interventional methods such as percutaneous nephrolithotomy (PNL), ureterorenoscopy (URS), and extracorporeal shock wave lithotripsy (ESWL) are preferred for the removal of the stones. Medical expulsive therapy, which has been used in adolescent children in recent years, provides the passage of obstructive ureteral stones without the need for invasive procedures [9].
There are certain differences in the clinical features of stone disease between adults and children. Similar to that, UL may also vary among infants and children. Although there are many studies dealing with pediatric and infantile UL separately, large-scale studies comparing UL in infants and children in terms of demographic and clinical features as well as outcome are still scarce. In this multicentric study, it is aimed to evaluate the demographic features, etiological risk factors, treatment strategies, and outcome in 2513 children with UL. This study also provides an evaluation of differences between infants and children in terms of demographics, etiological risk factors, stone characteristics, and response to treatment.
Patients and methods
This study was approved by the ethics committee of the Erciyes University Medical Faculty (2019/59). The retrospective multicentric study was conducted by the Urolithiasis Working Group of the Turkish Pediatric Nephrology Association. The nation-wide data are obtained from 23 pediatric nephrology centers from different geographical regions of Turkey. The medical records of 2513 children (0–18 years) with UL between August 2018 and June 2019 were reviewed.
Data including demographic, clinical, laboratory and radiologic findings, gender, age at diagnosis, family history of stone disease, consanguinity, prematurity, a dietary history with emphasis on vitamin D administration, formula feeding (for infants), history of drug use that induces stone formation (antiepileptics, loop diuretics, etc.), presenting symptoms, physical examination findings, presence of urinary tract abnormalities and urinary tract infections (UTI), size, number and location of stones in the urinary system, evaluation of MRFs, and response to the medical or surgical treatments of the patients were obtained from the pediatric nephrology centers participating in the study retrospectively.
UTI was defined as having positive urine cultures as well as the presence of leukocyte esterase and nitrite positivity in dipstick test [10].
Patients were grouped based on their ages at diagnosis as infants (≤ 12 months) and children (> 12 months). Hyperechogenic spots on ultrasonography smaller than 3 mm were defined as microlithiasis [11]. The diagnosis of microlithiasis was confirmed by at least two different radiologists.
Evaluation of urinary metabolic risk factors, including hypercalciuria, hyperoxaluria, hypocitraturia, hyperuricosuria, cystinuria and hypomagnesuria were carried out by calculating mineral excretions in 24-h urine or random urine mineral-to-urine creatinine ratios. It was compared with the 95th percentile of age-specific reference values to confirm the abnormal urine mineral excretion [9,10,11,12,13] (presented in supplement Table). Blood urea nitrogen, serum creatinine, calcium, uric acid, phosphate, sodium, potassium, chloride, alkaline phosphatase and, 25 hydroxyvitamin D and parathyroid hormone levels in serum were also evaluated. Hypoparathyroidism, hyperparathyroidism, hypervitaminosis D and Vitamin D deficiency were defined using age-specific reference intervals [14, 15].
Follow-up data were collected retrospectively from the medical records of the patients. The patients were followed by pediatric nephrologists in 23 different centers. Ultrasonographic examinations at the time of diagnosis and in the follow-up were performed either by pediatric radiologists or by radiologists experienced in pediatric ultrasound. Follow-up data of the patients at the end of a year period were evaluated to determine whether there was stone resolution. It was noted that some patients were followed up without any medical therapy, and some patients did not use the prescribed treatment despite recommendation. At the end of 12 months, stone resolution and clinical recovery were evaluated in patients with and without treatment for UL. The absence of hyperechogenic calculi on follow-up ultrasonography was considered as stone resolution. Those who were in remission without treatment were accepted as spontaneous stone resolution. Information on stone recurrence could not be obtained due to the absence of long-term follow-up data.
Statistical analysis
Descriptive statistic and Chi-square tests were performed as statistical analysis using the statistical software package SPSS version 21.0. Descriptive statistics were expressed as mean and standard deviation, median and percentages. Results with p < 0.05 were regarded as statistically significant.
Results
Demographic data and clinical findings of the patients
Data of 2513 children with UL, 1304 male and 1209 female, collected from 23 pediatric nephrology centers, were analyzed. Male to female ratio was 1.1/1. Demographic and clinical findings of the infants and the children are presented in Table 1. The age at diagnosis of patients ranged from 14 days to 18 years, with a mean age of 39.5 ± 35 months (median 12 months). Half of all cases were at an infantile age (50.2%).
There were statistically significant differences between genders: The mean age at diagnosis was higher in the female group (44.4 ± 42 months) compared to the males (34.9 ± 32 months). The male-to-female ratio was found to be 1.2:1 in infants, whereas it was 0.9:1 in children. In both age groups, the history of UTI and UTI at the time of diagnosis was higher in girls. Antenatal hydronephrosis was frequent in infancy only in males.
Positive family history for urinary stones was present in about half of the cases (54%) and consanguinity rate among the parents was 19.3%. The most common reason for admission to nephrology outpatient clinics was incidentally detected stones on urinary system ultrasound during their routine health check-ups or after the patient’s admission to hospital for other complaints apart from kidney stones. The most common presenting symptoms were restlessness or irritability in infants, and abdominal pain in children. Other symptoms were macroscopic hematuria (5.8%), vomiting (5.7%) and microscopic hematuria (4%). History of prematurity, high-dose vitamin D intake, hospital admission in the neonatal period and antenatal hydronephrosis were significantly higher in infants compared to children (p < 0.05).
Etiological factors for UL in the patients
When the patients were categorized based on the etiological risk factors; metabolic abnormalities were detected in 61.5% (n/N: 1522/2474), urinary tract infection in 18.3% (n/N: 455/2513), and anatomic abnormalities in 17% (n/N: 441/2513) of all patients. The UPJ obstruction (31%, 137/441) and VUR (19%, 86/441) were the most prevalent anatomic abnormalities.
58.4% of the infants and 64.5% of the children had at least one of the urinary MRF (p < 0.001). The most common urinary MRFs were hypercalciuria (26%), hypocitraturia (24%) and hypomagnesuria (17.8%). The most common urinary MRF was hypercalciuria in infants and hypocitraturia in children. In addition, hypercalcemia, hypervitaminosis D, hypoparathyroidism was significantly higher in infants compared to children, whereas vitamin D deficiency and hyperparathyroidism were common in children (p < 0.05) (Table 2).
Imaging findings and types of the urinary system stones
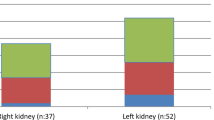
Stone types and imaging findings are shown in Table 3. Most of the stones were localized in the pelvis-calyx (63%), were multiple in number (60%), and ranged between 3 and 10 mm in size (62.6%). In infants, multiple stones were prevalent, and in children, stones were usually single. Microlithiasis was present in 31.6% of all patients. The rate of microlithiasis was higher in infants (40.6%) and 64.5% of the patients with microlithiasis were infants, and the rate of having stones larger than 10 mm was higher in children. Ureteral and bladder stones were significantly higher in children (p < 0.05). Urinary system X-ray was available in 341 patients and most of the stones were non-opaque in both age groups. While opaque stones were more common in children, semi-opaque stones were frequent in infants. Stone analysis was performed for a total of 274 cases. The most common stone types were calcium oxalate (64.6%), cystine (14.6) and mixed type stones (12%). Magnesium stones were detected in only 10 cases, uric acid stones in 7, and calcium phosphate stones in 6 cases.
Treatments and outcome
Conservative treatments such as salt-restricted diet and hydration by increasing oral fluid intake and frequent lactation for infants were recommended for all patients. At least one medical treatment was administered to 1388 (55%) of the cases. The most preferred medical treatment was potassium citrate or Shohl’s solution given for urinary alkalinization [9,10,11]. Interventional treatment was applied in 381 cases, mostly ESWL (n = 187), in addition to URS (n = 98), and PNL (n = 73). Most of the patients (84%), who underwent interventional treatment, had stones larger than 10 mm in size.
Stone resolution, excluding patients with stone surgery and those with under a year’s follow-up, was evaluated in 1682 cases. A total of 1351 cases (80.3%) had stone resolution after a year’s follow-up with or without medical treatment (Table 4). Stone resolution was observed in 83% of infants and 77.5% of children (p < 0.05). Spontaneous stone resolution was observed in 88% (615/697) of the cases followed without treatment (88.6% in infants, 87.8% in children). Half of the cases with spontaneous stone resolution (51.3%) had microlithiasis. However, most of the patients with microlithiasis (85.4%) showed spontaneous remission.
Total stone resolution rates were similar in patients with and without MRF. However, the spontaneous resolution rate of stones in cases without MRF (48.7%) was significantly higher than in cases having MRF (29.1%) (p < 0.0001). In addition, the stone resolution rate in cases with medical treatment was higher in MRF ( +) stones (50.2%) compared with MRF (−) stones (p < 0.0001). The effect of metabolic risk factor on stone resolution is presented in Table 5.
Discussion
Our nation-wide study representing the largest case series of the pediatric and infantile UL in the literature provides information about the demographic, clinical and laboratory characteristics, etiologic risk factors, treatment strategies and the outcomes. It is known that pediatric UL is different from UL in the adult population. This study showed that there are some distinct properties of urinary stone disease differing between cases with the onset in infancy and childhood, such as gender predominance, presenting symptoms, underlying metabolic and anatomic abnormalities, frequencies of UTIs, stone features, clinical course, and stone remission rates with and without treatment. This study also clearly revealed that children with microlithiasis can be followed up without medical treatment if they do not have any metabolic and/or anatomical risk factors. Medical treatment should be reserved in cases having MRFs.
The incidence of UL varies according to the geographic regions. Kidney stone disease is endemic in Turkey which is located in the geographic area called as “the stone-belt” [1,2,3]. There has been a significant increase in the incidence of pediatric and infantile UL over the past decades [16, 17]. The rate of infantile UL has been reported as 9–23% in pediatric UL [18]. This rate was reported as 34% and 41%, respectively, in two different pediatric UL cases series from Turkey [19, 20]. In our study, half of all children with UL were infants (50.2%). We have found a higher rate of infantile UL compared to other studies. In addition to this, positive family history for UL was present in 54% of the infantile UL cases. We believe that, relatively high rates of consanguineous marriages in our country affect the prevalence of UL at young ages by increasing the genetic predisposition. In our case series, the most common reason for referral to the pediatric nephrology departments was the incidental diagnosis of kidney stones. We assume that it has become easier to access healthcare services in our country in recent years, and the widespread use of routine ultrasonography during the investigation of UTIs and infants with nonspecific symptoms, increases the rate of incidental diagnoses and, also, the detection of UL at younger ages.
It is known that the presentation of nephrolithiasis in children is variable depending on the age of the patient. Severe colicky abdominal pain is common in adolescents and school-aged children. Nonspecific symptoms of abdominal pain, nausea, vomiting, and irritability, rather than the typical renal colic, are seen in younger children [9]. Similar to the literature, in this study, the most common presenting symptom was irritability in infants, and abdominal pain, macroscopic hematuria, and vomiting in children.
Studies on gender predisposition in pediatric UL have variable results, with some reports suggesting equal prevalence in both sexes and others indicating slightly higher prevalence in males [21,22,23]. In the majority of the studies about infantile UL, a male predominance has been reported [19, 20, 24,25,26,27]. In our study, male-to-female ratio was 1:1.1 in all children with UL, and male predominance was seen in infants whereas female predominance was found in children older than 12 months. In our study, the mean age at diagnosis was higher in the female group when compared with the males. This difference might be attributed to the male predominance in infantile UL, as shown in many studies including ours. In other words, this study has shown that, there seems to be a significant shift from male to female predominance with increasing age. Furthermore, consistent with the literature [25], UTI history and the presence of UTI at the time of diagnosis were higher in females, while a history of antenatal hydronephrosis was higher in male infants. Although, certain studies investigating the effect of gender in pediatric stone disease have found some differences between both sexes in terms of metabolic risk factors [28, 29], no significant difference was found in our study.
It is fundamental to define the etiology of UL to treat the patients successfully and to prevent stone recurrence and morbidities such as kidney failure. Studies over the past few decades have identified metabolic disorders in 12–96% of pediatric patients with UL, whereas anatomic urinary abnormalities and infection were found in 8–32% and 2–24% of cases, respectively [7, 23, 27,28,29,30,31]. Metabolic and anatomical etiologies have been reported to be common in Turkish children with UL [5,6,7,8]. In our study, the rate of structural urinary anomaly was 17%, urinary infection rate was 18%, and the rate of having at least one metabolic disorder was 61.5%.
Structural anomalies that might cause obstruction or urinary stasis such as UPJ obstruction, UV stenosis, VUR, posterior urethral valves, and polycystic kidney can facilitate the formation of kidney stones. Anatomical abnormalities of the urinary tract are found in 8–32% of children, and in 12.6–19.7% of infants with UL [1, 5, 13, 20]. UPJ obstructions and vesicoureteral reflux are the two most common urinary tract abnormalities seen in 11% and 9% of all children, respectively. Among pediatric stone disease patients, UPJ obstruction was found in 40–55%, vesicoureteral reflux in 33%, and UV stenosis in 13–22%. [32, 33]. In consistent with the literature, we showed that ureteropelvic stenosis (31%) and vesicoureteral reflux (19%) were the most common anatomic abnormalities as expected since they both result in urinary stasis and UTI. In addition, although the history of contracting antenatal hydronephrosis was higher in infants than in children, we found that the rate of anatomic abnormality was lower in infants contrary to expectations. This is probably because the vast majority of antenatal hydronephrosis spontaneously resolves in the postnatal period. Cases with antenatal hydronephrosis that do not resolve spontaneously in the following years are usually anatomical anomalies that can cause urinary stasis and lead to stone formation as a result. This may explain why we found a higher rate of urinary tract anomalies in children with UL.
To increase the rate of success in treatment and prevent stone recurrence, it is important to evaluate the metabolic risk factors. Children with UL are more likely to have one or more metabolic risk factors, compared with adults. Therefore, the possibility of stone recurrence is higher in children. Metabolic abnormalities have been reported in a wide range of 12–96% in children with UL. This variability in the percentages of detected risk factors might arise from the differences between patient populations in ethnicity, nutrition habits, socioeconomic factors, and geographic regions [4, 30]. Although, most of the previous studies on pediatric UL have reported the most common underlying metabolic abnormality as hypercalciuria, current studies indicate that there is a shift from hypercalciuria to hypocitraturia in terms of the predominant metabolic abnormality in children with UL, possibly due to changes in dietary habits over the years [21, 27, 34, 35]. Hypercalciuria has been reported as the main metabolic disorder in the studies focusing on infantile UL [18,19,20, 26]. In our study, hypercalciuria in infants and hypocitraturia in children were found at a higher rate, which is in accordance with other global studies [18,19,20, 27, 29,30,31,32,33,34,35]. In addition, the incidence of hyperoxaluria and cystinuria was higher in children when compared with infants. It has been reported that the initial stone detection in most patients with cystinuria occurs during older childhood or adolescence, as in our study [36]. The changes in dietary habits and consumption of oxalate-rich foods among the children seem to be an important cause of hyperoxaluria in these children; studies have shown that hyperoxaluria is significantly higher when the children are > 1 year and are switched to solid foods [35].
There are limited reports on Vitamin D level and calcium metabolism in children with UL. In these studies, it was found that the risk of D hypervitaminosis, hypercalcemia and hypoparathyroidism were higher in infants using vitamin D and fed with formula, and it was recommended to be careful about the risk of stone formation [37, 38]. In our study, hypercalcemia, hypervitaminosis D and hypoparathyroidism were found to be more prevalent in infants compared with children. In Turkey, a daily routine of 400 u/day supplementation of vitamin D for infants is a health policy. But sometimes, overdose usage of vitamin D is observed in infants. Contrary to these findings, the rates of vitamin D deficiency and hyperparathyroidism were also higher in children. This may be due to the widespread sedentary lifestyle of children and adolescents resulting in low exposure to sunlight.
Consistent with the previous studies [8, 19, 38, 39], in this study, certain differences were found between infants and children in terms of radiological findings and the features of the stone. Infant stones tended to be mostly non-opaque/semi-opaque and multiple in number, and the rate of microlithiasis was higher among infants. While upper urinary tract stones were more common in all age groups, ureter and bladder stones were more prevalent in children. Calcium oxalate stones were the most common stone types in both infants and children, while the majority of mixed type stones were found in infants.
There is a lack of consensus regarding the evaluation and treatment strategies in children and infants with UL. For many years, children have been evaluated and treated like “small adults”, but there are significant differences between the pediatric and the adult age.
In children, unlike adults, metabolic abnormalities are more common leading to stone recurrence [4]. In this study, infants and children with UL were evaluated in terms of their medical treatment and response to the treatment, and important results were obtained. Spontaneous stone resolution was observed in 88% of infants and children to whom medical treatment was not administered and were only recommended conservative treatment. Spontaneous stone resolution was associated with stone size and the presence of metabolic risk factors, rather than the patient’s age. The presence of hyperechogenic spots < 3 mm in diameter in the renal calyces are defined as renal calyceal microlithiasis [11]. Certain studies claimed that microlithiasis might be the beginning step in stone formation [11, 19, 20]. On the other hand, especially in infant kidney, misinterpretation of hyperechoic appearance of Bertin column and arcuate artery on sonography may also contribute to the increased incidence. Therefore, it is important that the diagnosis of microlithiasis is established by pediatric radiologists or radiologists experienced in pediatric ultrasound. In our study, spontaneous stone resolution was more prominent in patients with microlithiasis (85.4%) when compared to those with larger stones. In studies on microlithiasis, spontaneous stone resolution rates of 60–80% were reported. Therefore, it is recommended that patients with stone size < 3 mm should be followed only with preventive measures without any medical treatment [11, 19, 20, 26]. In our study, spontaneous recovery was observed more frequently in patients without any metabolic abnormalities (48.7%) than in those having MRF (29.1%). In accordance with this, stone remission rates with medical treatment were found to be higher in patients with MRF ( +) than in those with MRF (−). In the light of the results of our study, we recommend that, regardless of the age of the pediatric patient with UL, patients with microlithiasis and patients without any metabolic or anatomic risk factors should be followed up without medical treatment. Besides, if a patient has an MRF, specific medical treatment targeting the existing metabolic abnormality should be administered.
Limitations of this study: if the follow-up period had not been limited to 1 year, longer follow-up results might have been different. We could also have not relapse rates over the years.
The strength of our study is that it is a large-scale study of 2513 cases comparing many different characteristics of children and infants with UL.
Conclusions
This study presents the largest case series in the literature comparing infants and children with UL and detecting several differences, such as gender predominance, presenting symptoms, underlying metabolic and anatomic abnormalities, frequencies of UTIs, stone features, clinical course, and stone remission rates. Identifying the underlying risk factors, especially metabolic abnormalities, for children and infants with UL as early as is possible is necessary to avoid considerable morbidity. We suggest that infants with microlithiasis can be followed up without treatment if they do not have any metabolic and anatomical risk factors. We also recommend that if children with UL have any metabolic abnormalities, they should be treated for the current metabolic abnormality. Children with UL who received as well as children who did not receive treatment should be followed up regularly by both pediatric nephrologists and pediatric urologists.
References
Bowen DK, Tasian GE (2018) Pediatric stone disease. Urol Clin North Am 45:539–550. https://doi.org/10.1016/j.ucl.2018.06.002
Lopez M, Hoppe B (2010) History, epidemiology and regional diversities of urolithiasis. Pediatr Nephrol 25:49–59. https://doi.org/10.1007/s00467-008-0960-5
Akinci M, Esen T, Tellaloğlu S (1991) Urinary stone disease in Turkey: an updated epidemiological study. Eur Urol 20:200–203. https://doi.org/10.1159/000471700
Tasian GE, Kabarriti AE, Kalmus A, Furth SL (2017) Kidney stone recurrence among children and adolescents. J Urol 197:246–252. https://doi.org/10.1016/j.juro.2016.07.090
Ozokutan BH, Küçükaydin M, Gündüz Z, Kabaklioğlu M, Okur H, Turan C (2000) Urolithiasis in childhood. Pediatr Surg Int 16:60–63. https://doi.org/10.1007/s003830050016
Bak M, Ural R, Agin H, Serdaroglu E, Calkavur S (2009) The metabolic etiology of urolithiasis in Turkish children. Int Urol Nephrol. https://doi.org/10.1007/s11255-008-9513-x
Elmacı AM, Ece A, Akın F (2014) Clinical characteristics and metabolic abnormalities in preschool-age children with urolithiasis in southeast Anatolia. J Pediatr Urol 10:495–499. https://doi.org/10.1016/j.jpurol.2013.11.004
Girişgen İ, Yüksel S, Karcılı K, Becerir T (2019) Evaluation of the composition of urinary tract stones in children from the inner western Anatolian region in Turkey. Turk J Urol 46:152–158. https://doi.org/10.5152/tud.2019.19170
Edvardsson V (2016) urolithiasis in children. In: Avner ED, Harmon WE, Niaudet P, Yoshikawa N, Emma F, Goldstein SI (eds) pediatric nephrology, 7th edn. Springer, Berlin, pp 1821–1869
Okarska-Napierała M, Wasilewska A, Kuchar E (2017) Urinary tract infection in children: Diagnosis, treatment, imaging—comparison of current guidelines. J Pediatr Urol 13:567–573
Alpay H, Ozen A, Gokce I, Biyikli N (2009) Clinical and metabolic features of urolithiasis and microlithiasis in children. Pediatr Nephrol 24:2203–2209. https://doi.org/10.1007/s00467-009-1231-9
Hoppe B, Leumann E, Milliner DS (2008) Urolithiasis and nephrocalcinosis in childhood. In: Geary D, Schaefer F (eds) Comprehensive pediatric nephrology, 1st edn. Mosby, Philadelphia, pp 499–525
Baştuğ F, Düşünsel R (2012) Pediatric urolithiasis: causative factors, diagnosis, and medical management. Nat Rev Urol 9:138–146. https://doi.org/10.1038/nrurol.2012.4
Pınar A (2020) Laboratory reference values in childhood. In: Hasanoğlu E, Düşünsel R, Bideci A, Boduroğlu K (eds) Essential Pediatrics Book, 2nd edn. Güneş kitabevi, İstanbul, pp 3109–3145
Andropoulos DB (2012) Pediatric normal laboratory values. In: Gregory GA, Andropoulos DB (eds) Gregory’s pediatric anesthesia, 5th edn. Blackwell Publishing Ltd, Hoboken, pp 1263–1280
Clayton DB, Pope JC IV (2011) The increasing pediatric stone disease problem. Ther Adv Urol 3:3–12. https://doi.org/10.1177/1756287211400491
Dwyer ME, Krambeck AE, Bergstralh EJ, Milliner DS, Lieske JC, Rule AD (2012) Temporal trends in incidence of kidney stones among children: a 25-year population-based study. J Urol 188:247–252. https://doi.org/10.1016/j.juro.2012.03.021
Penido MG, Alon US (2021) Infantile urolithiasis. Pediatr Nephrol 36(5):1037–1040. https://doi.org/10.1007/s00467-020-04888-7
Alpay H, Gokce I, Özen A, Bıyıklı N (2013) Urinary stone disease in the first year of life: is it dangerous? Pediatr Surg Int 29:311–316. https://doi.org/10.1007/s00467-009-1231-9
Güven AG, Koyun M, Baysal YE, Akman S, Alimoglu E, Akbas H, Kabaalioglu A (2010) Urolithiasis in the first year of life. Pediatr Nephrol 25:129–134. https://doi.org/10.1007/s00467-009-1296-5
Bush NC, Xu L, Brown BJ, Holzer MS, Gingrich A, Schuler B, Tong L, Baker LA (2010) Hospitalizations for pediatric stone disease in United States, 2002–2007. J Urol 183:1151–1156. https://doi.org/10.1016/j.juro.2009.11.057
Coward RJ, Peters CJ, Duffy PG, Corry D, Kellett MJ, Choong S, Hoff van’t WG (2003) Epidemiology of paediatric renal stone disease in the UK. Arch Dis Child 88:962–965. https://doi.org/10.1136/adc.88.11.962
Ward JB, Feinstein L, Pierce C, Lim J, Abbott KC, Bavendam T, Kirkali Z, Matlaga BR (2019) Pediatric urinary stone disease in the United States: the urologic diseases in America project. Urology 129:180. https://doi.org/10.1016/j.urology.2019.04.012
Baştuğ F, Gündüz Z, Tülpar S, Poyrazoğlu H, Düşünsel R (2013) Urolithiasis in infants: evaluation of risk factors. World J Urol 31:1117–1122. https://doi.org/10.1007/s00345-012-0828-y
Sas DJ (2011) An update on the changing epidemiology and metabolic risk factors in pediatric kidney stone disease. Clin J Am Soc Nephrol 6:2062–2068. https://doi.org/10.2215/CJN.11191210
Mohamed J, Riadh M, Abdellatif N (2007) Urolithiasis in infants. Pediatr Surg Int 23:295–299. https://doi.org/10.1007/s00383-007-1889-7
Alemzadeh-Ansari MH, Valavi E, Ahmadzadeh A (2014) Predisposing factors for infantile urinary calculus in south-west of Iran. Iran J Kidney Dis 8:53–57
Schwaderer AL, Raina R, Khare A, Safadi F, Moe SM, Kusumi K (2019) Comparison of risk factors for pediatric kidney stone formation: the effects of sex. Front Pediatr 7:32. https://doi.org/10.3389/fped.2019.00032
Yagisawa T, Hayashi T, Yoshida A, Kobayashi C et al (2000) Comparison of metabolic risk factors in patients with recurrent urolithiasis stratified according to age and gender. Eur Urol 38:297–301. https://doi.org/10.1159/000020296
Copelovitch L (2012) Urolithiasis in children medical approach. Pediatr Clin North Am 59:881–896. https://doi.org/10.1016/j.pcl.2012.05.009
Celiksoy MH, Yilmaz A, Aydogan G, Kiyak A, Topal E, Sander S (2015) Metabolic disorders in Turkish children with urolithiasis. Urology 85:909–913. https://doi.org/10.1016/j.urology.2014.12.032
Erbagci A, ErbagciAB YM, Yagci F, Tarakcioglu M, Yurtseven C et al (2003) Pediatric urolithiasis–evaluation of risk factors in 95 children. Scand J Urol Nephrol 37(2):129–133. https://doi.org/10.1080/00365590310008866
Tabel Y, Akin İM, Tekin S (2009) Clinical and demographic characteristics of children with urolithiasis: single-center experience from eastern Turkey. Urol Int 83:217–221. https://doi.org/10.1159/000230027
Ertan P, Tekin G, Oger N, Alkan S, Horasan GD (2011) Metabolic and demographic characteristics of children with urolithiasis in western Turkey. Urol Res 39:105–110. https://doi.org/10.1007/s00240-010-0306-1
Kovacevic L, Wolfe-Christensen C, Edwards L, Sadaps M, Lakshmanan Y (2012) From hypercalciuria to hypocitraturia-a shifting trend in pediatric urolithiasis? J Urol 188:1623–1627. https://doi.org/10.1016/j.juro.2012.02.2562
Servais A, Thomas K, Dello Strologo L, Sayer JA et al (2021) Metabolic nephropathy workgroup of the European reference network for rare kidney diseases (ERKNet) and eUROGEN. Cystinuria: clinical practice recommendation. Kidney Int 99:48–58. https://doi.org/10.1016/j.kint.2020.06.035
Tang J, Chonchol MB (2013) Vitamin D and kidney stone disease. Curr Opin Nephrol Hypertens 22:383–389. https://doi.org/10.1097/MNH.0b013e328360bbcd
Szmigielska A, Pańczyk-Tomaszewska M, Borowiec M, Demkow U, Krzemień G (2019) Vitamin D and calcium homeostasis in infants with urolithiasis. Adv Exp Med Biol 1133:75–81. https://doi.org/10.1007/5584_2018_310
Dursun I, Poyrazoglu HM, Dusunsel R, Gunduz Z, Gurgoze MK, Demirci D, Kucukaydin M (2008) Pediatric urolithiasis: an 8-year experience of single centre. Int Urol Nephrol 40:3–9. https://doi.org/10.1007/s11255-007-9234-6
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethical statement
This study was approved by the ethics committee of the Erciyes University Medical Faculty (2019/59).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Baştuğ, F., Ağbaş, A., Tülpar, S. et al. Comparison of infants and children with urolithiasis: a large case series. Urolithiasis 50, 411–421 (2022). https://doi.org/10.1007/s00240-022-01327-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00240-022-01327-0