Abstract
DNA electrotransfer is a successful technic for gene delivery. However, its use in clinical applications is limited since little is known about the mechanisms governing DNA electrotransfer in the complex environment occurring in a tissue. The objectives of this work were to investigate the role of the extracellular matrix (ECM) in that process. Tumor ECM composition was shown to modulate in vivo gene electrotransfer efficiency. In order to assess the effects of ECM composition and organization, as well as intercellular junctions and communication, in normal tissue response to electric pulses, we developed an innovative three-dimensional (3D) reconstructed human connective tissue model. 3D human dermal tissue was reconstructed in vitro by a tissue engineering approach and was representative of in vivo cell organization since cell–cell contacts were present as well as complex ECM. This human cell model presented multiple layers of primary dermal fibroblasts embedded in a native, collagen-rich ECM. This dermal tissue could become a useful tool to study skin DNA electrotransfer mechanisms. As proof of the concept, we show here that the cells within this standardized 3D tissue can be efficiently electropermeabilized by milliseconds electric pulses. We believe that a better comprehension of gene electrotransfer in such a model tissue would help improve electrogene therapy approaches such as the systemic delivery of therapeutic proteins and DNA vaccination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The clinical development of gene therapy requires the use of safe and efficient methods to deliver therapeutic genes to the targeted cell. Contrary to viral vectors, plasmid DNA vectors offer many advantages. They are safer than viral vectors, cheaper and easier to mass-produce, they have a high DNA content, and their administration can be repeated since they are non-immunogenic (Pfutzner 2010). However, their major disadvantage is their low effectiveness in vivo. Indeed, plasmid DNA vectors have to overcome several obstacles, namely, DNA diffusion through the extracellular matrix (ECM), uptake across the plasma membrane, intracellular migration to the nucleus, and through the nuclear envelope (Escoffre et al. 2010).
Physical techniques such as electroporation have been developed to improve the in vivo transfection rate and are now accepted in clinics. The method relies on the application of electric pulses to induce transient and localized cell permeabilization, a process that allows naked plasmid DNA uptake into cells (Neumann and Rosenheck 1972; Neumann et al. 1982). Thanks to electrogene transfer, safe local delivery can be achieved. A wide range of soft and hard tissues have already been successfully transfected using this method including skin, liver, muscle, joints, lung, spleen, brain, eyes, and tumors (Mir et al. 2005).
Electrogene transfer in skin, which is an easy organ to treat, allows multiple therapeutic approaches to be considered such as systemic delivery of therapeutic proteins and DNA vaccination (Rochard et al. 2011; Vandermeulen et al. 2007). Indeed, human skin is largely microvascularized, allowing transfected cells to systemically secrete therapeutic proteins. Furthermore, skin contains a numerous antigen-presenting cells, allowing a strong immune response after DNA vaccination. Thus, the first published phase I study on metastatic melanoma found that IL-12 electrogene transfer led to tumor necrosis and regression of untreated distant metastases (Daud et al. 2008).
In order to improve in vivo electrogene transfer efficacy in human skin and thus to develop clinical applications, we have to have a better understanding of the gene transfer mechanisms in a tissue context. A lot of in vitro studies performed on cells in culture have been used in an attempt to optimize the electrical parameters and thus to apply this technique in clinics. However, even though they are useful, none of these studies were able to access the complexity of in vivo tissues. Accumulating evidence underlines that three-dimensional (3D) cell models are superior to classical 2D cell culture to mimic and predict in vivo situations (Ghajar and Bissell 2010; Nyga et al. 2011; Pampaloni et al. 2007).
This is why we and others have developed 3D cell culture models to study gene electrotransfer in vitro in a 3D context. The most common model, named the spheroid, is a 3D cellular model devoid of any exogenous material (Sutherland 1988). Even though mRNA for ECM components such as collagens, laminin, fibronectin, and glycosaminoglycans were found in spheroids, the model is especially relevant for intercellular junctions in a tumor context (Kunz-Schughart et al. 2006; Nederman et al. 1984; Stevens et al. 2009). We previously demonstrated that although the electrotransfection rate reached values higher than 25 % for cells in suspension, the transfection rate of cells in spheroids hardly reached 1 % under the same electrical conditions (Chopinet et al. 2012), a value which is close to in vivo tumor transfection rates (Rols et al. 1998). Mellor and coll showed that transfected cells were only located on the outer layers of the spheroid, in direct contact with plasmid DNA (Mellor et al. 2006). Similarly, we noted that reporter gene expression was only detected in one cap of the spheroid, the one facing the negative electrode, which is direct evidence for the involvement of electrophoretic forces in DNA electrotransfer (Wasungu et al. 2009) and is in agreement with the in vitro process (Golzio et al. 2002; Paganin-Gioanni et al. 2011). Interestingly, in another 3D cellular model, Haberl et al. confirmed that electrogene transfer within hamster cells dispersed in a type I collagen from rat tail gel was comparable to in vivo studies and depended on plasmid DNA concentration and pulse duration (Haberl and Pavlin 2010). Thus, close contacts between cells and ECM deposition may act as a physical barrier that limits/prevents uniform DNA distribution and could explain the low gene electrotransfer efficiency in tissue.
Skin dermis is a connective tissue characterized by abundant ECM primarily synthesized by fibroblasts (Prost-Squarcioni et al. 2008). Dermis ECM is composed of collagen and elastic fibers providing tissue resistance to tensile forces and the amorphous ground substance, allowing the flow of water and dissolved molecules. In order to study gene electrotransfer mechanisms in skin, we developed here an innovative in vitro 3D human model of normal dermal tissue, where primary dermal fibroblasts produce their own, complex physiological ECM.
Materials and Methods
Cell Culture
Primary human dermal fibroblasts were isolated from human foreskin biopsy after posthectomy as previously described (Gibot et al. 2010). The cells were grown in Dulbecco’s Modified Eagles Medium (Gibco-Invitrogen, Carlsbad, USA) containing 4.5 g/L glucose, l-glutamine, and pyruvate, supplemented with 10 % (v/v) of heat-inactivated fetal calf serum, 100 U/ml penicillin, and 100 µg/ml streptomycin. Cells were maintained at 37 °C in a humidified atmosphere containing 5 % CO2.
Reconstruction of a Human 3D Dermal Tissue
The self-assembly approach (Auger et al. 2002) was used to produce human 3D dermal tissue in vitro. Schematically, primary human dermal fibroblasts were cultivated for 3 weeks in cell culture medium supplemented with 50 µg/mL of ascorbic acid (Sigma) as previously described (Gibot et al. 2010, 2013). Indeed, ascorbic acid is well known to improve collagen production, secretion, and maturation (Lyons and Schwarz 1984; Schwarz 1985). After 3 weeks, cells secreted enough ECM to form a cell sheet that was easy to manipulate. Since the cells used to produce the sheet are dermal fibroblasts, ECM is comparable to that found in the dermis compartment of the skin.
Histological Analysis
After fixation in formalin (Sigma-Aldrich) at room temperature for 1 h, transversal sections of cell sheet were embedded in paraffin for staining with Masson’s trichrome (Sigma-Aldrich). The Masson’s trichrome method stains cells red and collagens within the dermal tissue in blue (Masson 1929).
Transmission and Scanning Electron Microscopy
For transmission electron microscopy, cell sheets were fixed in 2 % glutaraldehyde in 0.1 M Sorensen phosphate buffer (pH 7.4) for 4 h at 4 °C, washed overnight in 0.2 M phosphate buffer, and then post-fixed for 1 h at room temperature with 1 % osmium tetroxide in 250 mM saccharose and 0.05 M phosphate buffer. They were stained overnight in 2 % uranyl acetate. The samples were then dehydrated in a series of graded ethanol solutions and embedded in an Epon–araldite resin (Embed 812-Araldite 502, Electron Microscopy Sciences). Finally, ultra-thin sections stained with uranyl acetate were observed under a transmission electron microscope (Hitachi HU12A electron microscope). For scanning electron microscopy, cell sheets were fixed in 2 % glutaraldehyde in 0.1 M sodium cacodylate buffer for 4 h at 4 °C. After two washes in the same buffer, the cell sheets were dehydrated in a graded ethanol series, dried by critical point drying with EMSCOPE CPD 750, coated with gold–palladium for 5 min at 100 Å min−1, and then observed with a S450 scanning electron microscope (Hitachi).
Collagens Detection by Second Harmonic Generation
Three dimensional stacks of 425 × 425 × 60 μm were acquired using a 7MP multiphoton laser scanning microscope (Carl Zeiss S.A.S., Jena, Germany), equipped with a 20× objective (NA 0.95) and coupled to a Ti-Sapphire femtosecond laser, Chameleon Ultra 2 (Coherent Inc) tuned to 800 nm. Organized fibrillar collagens were detected by second harmonic generation (SHG) at a wavelength of 400 nm. The acquired 3D images were stored and then analyzed off-line with Imaris software (Bitplane AG).
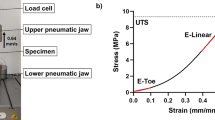
Electropermeabilization of 3D Human Dermal Tissue
Two flat parallel stainless steel electrodes (1 cm length, 1 cm width) were placed on the top of cell sheets and immersed in pulsing buffer (10 mM K2HPO4/KH2PO4 buffer, 1 mM MgCl2, 250 mM sucrose, pH 7.4) containing 100 µM propidium iodide (PI) (Sigma-Aldrich). Electropulsation used an electro cell S20 generator (βTech, Toulouse, France) which delivered square-wave electric pulses. An oscilloscope (Enertec, St. Etienne, France) was used to monitor pulse shape. The electrical conditions were as follows: eight pulses lasting 5 ms at a frequency of 1 Hz were applied from 0 to 600 V/cm at room temperature. Cell membrane permeabilization was assessed by multiphoton laser scanning microscopy on living tissues. An isosurface was made with Imaris software to visualize and isolate the permeabilized cells.
Results
Reconstruction of Human 3D Dermal Tissue Rich in Organized Collagens
In the first step, we visualized and characterized the ECM secreted by primary human dermal fibroblasts within our in vitro 3D reconstructed dermal tissue model. For this purpose, we identified collagens by different and complementary imaging tools. Primary human dermal fibroblasts cultured by the self-assembly approach are able to reproduce a physiological environment within 3 weeks, by secreting and organizing a dense 3D ECM rich in collagens (Fig. 1). Dermal tissue cross sections showed several layers of fibroblasts embedded in a 3D ECM rich in collagens (Fig. 1a). Both scanning and transmission electron microscopy showed intact, organized collagen fibrils within our dermal tissue model (Fig. 1b, c). Longitudinal sections of collagen fibrils showed the typical striation brought about by the arrangement of tropocollagen (Fig. 1d). In addition, multiphoton imaging allowed non-invasive high-resolution in vitro, in situ imaging of organized ECM structures and cells in living intact tissue-engineered models. Thus, abundant organized collagens fibrils were distinctly observed by SHG (Fig. 1e).
Human 3D dermal tissue characterization. a Cell sheet cross section stained with Masson’s trichrome. Cells are red and collagens are blue. b Scanning electron microscopy showing fibroblast cells and extracellular matrix. c Transmission electron microscopy of cell sheet. Arrows indicate collagen fiber cross sections. d Transmission electron microscopy of cell sheet. Arrows indicate longitudinal section of collagen bundles. e Organized fibrillar collagens within cell sheet produce second harmonic generation signal (Color figure online)
Cells were Efficiently Electropermeabilized Within 3D Reconstructed Dermal Tissue
To study the effect of electrical pulse parameters (i.e., millisecond electric pulses) currently used for gene electrotransfer, the permeabilization state of cells within 3D human dermal tissue was assessed using PI penetration. Permeabilization was followed on live human dermal tissue by multiphoton imaging (Fig. 2). Biphoton microscopy allowed observation of the entire thickness of the fresh tissue. For the control, dermal tissues were incubated with PI without any electrical pulses. We only observed a few permeabilized cells, corresponding to dead cells (Fig. 2a). Indeed, there is some cell renewal in our model, and dead cells are trapped within the tissue. For the electropulsed condition, by increasing electric field intensity, we observed that cells could be gradually permeabilized (Fig. 2b–d). These experiments showed that electric pulse intensities between 300 V/cm and 600 V/cm led to an efficient and homogeneous permeabilization of the cells. Thus, using the gene electrotransfer electrical parameters (i.e., millisecond pulses), we are able to efficiently electropermeabilize all the cells contained in the model tissue whatever their location in the cell sheet.
3D dermal tissue electropermeabilization. Reconstructed human dermal tissue was electropermeabilized in the presence of propidium iodide (red) with the following electrical parameters: 8 pulses of 5 ms duration at 1 Hz. Electric field intensity was 0 V/cm (a), 200 V/cm (b), 300 V/cm (c), 400 V/cm (d), 500 V/cm (e), 600 V/cm (f) and observed under a fluorescent biphoton microscope. Collagens are blue (Color figure online)
Discussion
In this study, we used a tissue engineering approach to in vitro reconstruction of human 3D dermal tissue rich in organized collagens. Indeed, primary human dermal fibroblasts cultured by the self-assembly approach reproduce a physiological environment within 3 weeks, by secreting and organizing a dense 3D ECM containing collagens and elastin, with characteristics similar to those observed in vivo (Pouliot et al. 2002), (L’Heureux et al. 1998). Using self-assembly approach, we are able to produce in a reproducible manner several tens of sheets of 50 µm average thickness. The production cost is less than 5€ for each cell sheet, which is dramatically cheaper than using rat tail collagen gel to mimic dermis compartment. The major limitation of self-assembly approach can be the time necessary for cells to produce handleable cell sheet, i.e., approximately 3 weeks, which can be overcome by a good logistical organization.
To our knowledge, we are the first to implement and use these easily handleable cell sheets to study gene electrotransfer in tissue. We showed that using millisecond electric pulses, cells deep within the tissue were efficiently electropermeabilized.
After this proof of concept, we hope that our innovative model will be a valuable tool to assess the role of ECM secretion and organization, as well as intercellular junction and communication, in tissue responses to electric pulses. Indeed, it has already been proven in vivo that electric fields improve plasmid transport via electrophoresis across extracellular medium (Henshaw and Yuan 2008). However, electrophoretic transport of plasmid DNA is inversely correlated with collagen content in solid tissues (Zaharoff et al. 2002). Soft tumors containing few proteoglycans and collagens were found in vivo to be more efficiently electrotransfected with plasmid DNA than solid tumors with rich ECM (Mesojednik et al. 2007). The underlying mechanism seems to be that collagen influences tumor tissue resistance to macromolecule transport by binding and stabilizing glycosaminoglycans (Netti et al. 2000). These in vivo studies were performed on mice and provided access to gene delivery in tissue, but mouse skin is very different from human skin (Pasparakis et al. 2014). Furthermore, most of these studies were performed in a tumor context. We think that a better understanding of the role of ECM in gene electrotransfer in a healthy human 3D-relevant context will help improve gene therapy and DNA vaccination efficiency.
In addition, tissue engineering approaches to reconstructing normal human tissue lends itself to the philosophy of the 4R’s that promotes reliable alternatives to animal experiments in an attempt to reduce the numbers of animals used (responsibility, refining, replacement, and reduction). The simplicity of in vitro testing on reconstructed human dermal tissue will allow better development and adjustment of gene electrotransfer conditions in terms of plasmid DNA concentration and electrical parameters. With the development of dermal models reconstructed directly from patient cells, this technique could hold promise for the development of patient-adjusted gene therapy, i.e., personalized medicine. It will become possible to evaluate and then adapt the electric field pulse parameters (pulse number, amplitude, and width) far beyond what can be done in animal studies.
References
Auger, FA, et al. (2002). A truly new approach for tissue engineering: the LOEX self-assembly technique. In: Ernst Schering Res Found Workshop. pp 73–88
Chopinet L et al (2012) First explanations for differences in electrotransfection efficiency in vitro and in vivo using spheroid model. Int J Pharm 423:7–15
Daud AI et al (2008) Phase I trial of interleukin-12 plasmid electroporation in patients with metastatic melanoma. J Clin Oncol 26:5896–5903
Escoffre JM et al (2010) Gene transfer: how can the biological barriers be overcome? J Membr Biol 236:61–74
Ghajar CM, Bissell MJ (2010) Tumor engineering: the other face of tissue engineering. Tissue Eng Part A 16:2153–2156
Gibot L et al (2010) A preexisting microvascular network benefits in vivo revascularization of a microvascularized tissue-engineered skin substitute. Tissue Eng Part A 16:3199–3206
Gibot L et al (2013) Development of a tridimensional microvascularized human skin substitute to study melanoma biology. Clin Exp Metastasis 30:83–90
Golzio M et al (2002) Direct visualization at the single-cell level of electrically mediated gene delivery. Proc Natl Acad Sci USA 99:1292–1297
Haberl S, Pavlin M (2010) Use of collagen gel as a three-dimensional in vitro model to study electropermeabilization and gene electrotransfer. J Membr Biol 236:87–95
Henshaw JW, Yuan F (2008) Field distribution and DNA transport in solid tumors during electric field-mediated gene delivery. J Pharm Sci 97:691–711
Kunz-Schughart LA et al (2006) Potential of fibroblasts to regulate the formation of three-dimensional vessel-like structures from endothelial cells in vitro. Am J Physiol Cell Physiol 290:C1385–C1398
L’Heureux N et al (1998) A completely biological tissue-engineered human blood vessel. FASEB J 12:47–56
Lyons BL, Schwarz RI (1984) Ascorbate stimulation of PAT cells causes an increase in transcription rates and a decrease in degradation rates of procollagen mRNA. Nucleic Acids Res 12:2569–2579
Masson P (1929) Some histological methods; trichrome stainings and their preliminary technique. J Tech Methods 12:75–90
Mellor HR et al (2006) Optimising non-viral gene delivery in a tumour spheroid model. J Gene Med 8:1160–1170
Mesojednik S et al (2007) The effect of the histological properties of tumors on transfection efficiency of electrically assisted gene delivery to solid tumors in mice. Gene Ther 14:1261–1269
Mir LM et al (2005) Electric pulse-mediated gene delivery to various animal tissues. Adv Genet 54:83–114
Nederman T et al (1984) Demonstration of an extracellular matrix in multicellular tumor spheroids. Cancer Res 44:3090–3097
Netti PA et al (2000) Role of extracellular matrix assembly in interstitial transport in solid tumors. Cancer Res 60:2497–2503
Neumann E, Rosenheck K (1972) Permeability changes induced by electric impulses in vesicular membranes. J Membr Biol 10:279–290
Neumann E et al (1982) Gene transfer into mouse lyoma cells by electroporation in high electric fields. EMBO J 1:841–845
Nyga A et al (2011) 3D tumour models: novel in vitro approaches to cancer studies. J Cell Commun Signal 5:239–248
Paganin-Gioanni A et al (2011) Direct visualization at the single-cell level of siRNA electrotransfer into cancer cells. Proc Natl Acad Sci USA 108:10443–10447
Pampaloni F et al (2007) The third dimension bridges the gap between cell culture and live tissue. Nat Rev Mol Cell Biol 8:839–845
Pasparakis M et al (2014) Mechanisms regulating skin immunity and inflammation. Nat Rev Immunol 14:289–301
Pfutzner W (2010) Vectors for gene therapy of skin diseases. J Dtsch Dermatol Ges 8:582–591
Pouliot R et al (2002) Reconstructed human skin produced in vitro and grafted on athymic mice. Transplantation 73:1751–1757
Prost-Squarcioni C et al (2008) Functional histology of dermis. Ann Dermatol Venereol 135:1S5–1S20
Rochard A et al (2011) Genetic immunization with plasmid DNA mediated by electrotransfer. Human Gene Ther 22:789–798
Rols MP et al (1998) In vivo electrically mediated protein and gene transfer in murine melanoma. Nat Biotechnol 16:168–171
Schwarz RI (1985) Procollagen secretion meets the minimum requirements for the rate-controlling step in the ascorbate induction of procollagen synthesis. J Biol Chem 260:3045–3049
Stevens KR et al (2009) Physiological function and transplantation of scaffold-free and vascularized human cardiac muscle tissue. Proc Natl Acad Sci USA 106:16568–16573
Sutherland RM (1988) Cell and environment interactions in tumor microregions: the multicell spheroid model. Science 240:177–184
Vandermeulen G et al (2007) Optimisation of intradermal DNA electrotransfer for immunisation. J Control Release 124:81–87
Wasungu L et al (2009) A 3D in vitro spheroid model as a way to study the mechanisms of electroporation. Int J Pharm 379:278–284
Zaharoff DA et al (2002) Electromobility of plasmid DNA in tumor tissues during electric field-mediated gene delivery. Gene Ther 9:1286–1290
Acknowledgments
This research was performed in the scope of the EBAM European Associated Laboratory (LEA) and is a result of networking efforts within COST TD1104. We were supported by the Centre National de la Recherche Scientifique (CNRS), the Agence Nationale de la Recherche (ANR), Projet PIERGEN ANR-12-ASTR-0039, the Direction Générale de l’Armement (DGA), and the Midi-Pyrénées Région. Microscopy experiments were carried out on the Plateforme Genotoul Toulouse RIO Imaging. The authors would like to gratefully acknowledge Elisabeth Bellard (IPBS), Isabelle Fourquaux, and Nacer Benmeradi (CMEAB) for their technical assistance in imaging experiments, and Peter Winterton, a native English scientist, for his careful proofreading of this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Madi, M., Rols, MP. & Gibot, L. Efficient In Vitro Electropermeabilization of Reconstructed Human Dermal Tissue. J Membrane Biol 248, 903–908 (2015). https://doi.org/10.1007/s00232-015-9791-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00232-015-9791-z