Abstract
Purpose
Discrepancies in preadmission medication (PAM) are common and potentially harmful. Medication reconciliation is able to reduce the discrepancy rate, yet implementation is challenging. In order for reconciliation efforts to be more cost-effective, patients at high risk for reconciliation errors should be identified. The purpose of this systematic review is to identify predictors for unintentional discrepancies in PAM.
Methods
Medline and Embase were searched systematically until June 2017. Only studies concerning adult subjects were retained. Quantitative studies were included if predictors for unintentional discrepancies in the PAM had been determined on hospital admission. Variables were divided into patient-, medication-, and setting-related predictors based on a thematic analysis. Studies on identification of predictors for discrepancies and potentially harmful discrepancies were handled separately.
Results
Thirty-five studies were eligible, of which 5 studies focused on potentially harmful discrepancies. The following 16 significant variables were identified using multivariable prediction models: number of preadmission drugs, patient’s age, availability of a drug list, patients’ understanding of medication, usage of different outpatient pharmacies, number of high-risk drugs, discipline for which the patient is admitted, admitting physician’s experience, number and type of consulted sources, patient’s gender, type of care before admission, number of outpatient visits during the past year, class of medication, number of reimbursements, use of an electronic prescription system, and type of admission (elective vs emergency). The number of preadmission drugs was identified as a predictor in 20 studies. Potentially harmful discrepancies were ascertained in 5 studies with age found to have a predictive value in all 5 studies.
Conclusion
Multiple suitable predictors for PAM-related discrepancies were identified of which higher age and polypharmacy were reported most frequently.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Transitions of care, such as admission to and discharge from the hospital, have been associated with adverse drug events (ADEs). Part of these medication-related problems is due to inadequate communication between community care services and hospitals [1, 2]. Up to 27% of all hospital prescribing errors can be attributed to discrepancies in medication histories at the time of admission [3]. Up to 67% of adult patients admitted to the hospital have at least one unintended medication discrepancy [3]. A recent systematic review showed that the median proportion of all potentially harmful discrepancies was 34% [2]. However, the causal impact of these discrepancies on clinical outcome (e.g., length of stay, readmission, and mortality) is less obvious [2, 4]. An inaccurate preadmission medication (PAM) list can lead to errors in drug treatment during admission as well as in discharge medication orders and can result in unintentional changes of the patient’s chronic therapy [5, 6]. Obtaining a complete and accurate PAM list is essential in preventing avoidable medication errors during and after hospital stay [7].
Medication reconciliation during care transitions aims to reduce medication discrepancies, including those with a potential for harm, and has been mandated by health care accreditation organizations [1, 8,9,10,11]. Medication reconciliation should be performed in all patients during the initial 24 h after hospital admission. Usually, multiple sources are used to collect a best possible PAM list [12, 13]. In the study performed by Saint-Germain et al., the clinical pharmacist assessed on average 3.58 (±1.11) information sources to obtain the PAM list [13]. Up to 30 min might be spent on a structured reconciliation process [13,14,15]. Since different levels of expertise concerning reconciliation are available in the hospital setting, patients at higher risk for reconciliation errors should be interviewed preferentially by explicitly trained health care professionals, such as dedicated clinical pharmacists. Implementation of a structured medication reconciliation process can be a costly process in terms of human resources [16,17,18]. In order for reconciliation efforts to be more cost-effective and practically feasible, patients at high risk for reconciliation errors should be identified [1, 8, 19].
Aims
This systematic review was conducted in order to identify predictors of medication discrepancies. The aim was to identify those specific variables that are aligned with the highest risk for unintentional discrepancies in medication histories.
Methods
Data sources and searches
The PRISMA statement on how to conduct and report systematic reviews was followed in this review [20].
The used search string is summarized in Supplementary Table 1. The heuristic approach was applied to the bibliographic databases Medline and Embase. Additional relevant articles were identified through the snowball method.
Study selection
One reviewer (JH) selected the manuscripts; in case of doubt, manuscripts were retained if consensus was reached with two other researchers (LVdL and SDW). Initial assessment of the abstracts was performed for relevance; subsequently, full texts were examined for inclusion. Abstracts were included if the following criteria were met: medication reconciliation was mentioned in the study objectives, in particular gathering the best possible PAM list; studies had to include adult study subjects who were admitted to a hospital. Searches were limited to English, French, and Dutch articles published before June 2017. Only peer-reviewed investigative publications were retained.
The following criteria were used to further identify articles for inclusion. First, unintentional discrepancies had to be the primary objective of the studies. Unintentional discrepancies were defined as any difference between the best possible PAM list and the list gathered by usual care or involuntary differences between the best possible PAM list and admission orders. Second, predictors for the aforementioned discrepancies had to be described explicitly.
Data extraction and quality assessment
Data were extracted and compiled using a data collection form. The following information was extracted from the studies: author, country, study design, study population (sample size and target group), hospital setting, intervention (when, by whom, level of training, and type of intervention), type of drugs, type of discrepancies, severity of discrepancies, predictors (subdivided in three groups: patient-, medication-, and setting-related predictors), and statistical methods. If any of the previously mentioned criteria had not been described sufficiently, the author was contacted to acquire the necessary information. Only predictors that were available on hospital admission or shortly thereafter were retained for further analysis.
One researcher (JH) performed the quality assessment. The Newcastle-Ottawa Quality Assessment Scale (NOS) [21] for cohort studies was used to assess the quality of the included studies as recommended by the Cochrane Handbook for Systematic Reviews of Interventions [22]. Thresholds for converting the NOS scales to Agency for Healthcare Research and Quality standards (good, fair, and poor) were performed based on the following rules [23]:
-
Good quality: 3 or 4 stars in selection domain AND 1 or 2 stars in comparability domain AND 2 or 3 stars in outcome/exposure domain
-
Fair quality: 2 stars in selection domain AND 1 or 2 stars in comparability domain AND 2 or 3 stars in outcome/exposure domain
-
Poor quality: 0 or 1 star in selection domain OR 0 star in comparability domain OR 0 or 1 star in outcome/exposure domain
Data synthesis and analysis
A qualitative synthesis of the studies was performed based on a thematic analysis. Findings were summarized in patient-, medication-, and setting-related predictors. Predictors for potentially harmful discrepancies were reported separately. Results were adopted from the original manuscripts without further statistical analysis. In the summary of the results, a distinction was made between simple non-parametric statistical tests and prediction models.
Neither meta-analysis nor meta-regression was performed, because of the scarcity of data and the heterogeneity in methods, interventions, type of drugs, type of discrepancies, and reported outcomes, which precluded formal analysis.
Results
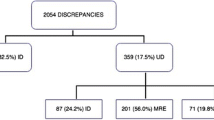
The search yielded 3615 articles; after removal of duplicates, 2977 abstracts were assessed of which 486 full articles were analyzed. A total of 35 cohort studies were used for analysis. The screening and selection progress is summarized in Fig. 1.
A detailed summary of the studies’ characteristics and quality assessment is provided in Table 1. Tamblyn et al. and Glintborg et al. had the highest score according to the NOS [24, 25]. Thirteen studies were scored “good” [5, 7, 8, 24,25,26,27,28,29,30,31,32,33].
An overview of all studied variables and relevant statistical details of the included studies has been added in Supplementary Table 2.
Results described in more detail below were statistically significant, unless mentioned otherwise. A distinction was made between risk factors for overall discrepancies and potential harmful discrepancies and is described separately.
Twenty-three studies corrected for confounders by performing multivariable analyses [5,6,7,8, 12,13,14, 24,25,26,27,28,29, 31,32,33, 35, 38, 39, 43, 46,47,48]. Statistically significant results provided by multivariable analysis are summarized in Table 2 for both all and specifically potentially harmful unintentional discrepancies.
Risk factors for unintentional discrepancies
Table 3 summarizes all variables that were examined as risk factors for unintentional PAM-related discrepancies both statistically significant or not. A division was made between non-parametric tests and prediction models. Information on statistical analysis, as performed in the original studies, is provided in the legend. Variables for which potential correlation with unintentional discrepancies was tested in several studies and found at least once to be statistically associated are discussed in more detail in the following.
Patient-related predictors
Age was investigated in 24 studies [5,6,7,8,9, 12, 13, 15, 24, 25, 27, 31, 32, 34, 35, 38, 43, 45,46,47,48,49,50,51]; only 9 found a significant result. Gleason et al. demonstrated, in a univariable analysis, that patients older than 65 years were more likely to have a discrepancy in their medication history [27]. Mendez et al. found that the number of unintentional discrepancies was strongly correlated with age (r = 0.67) [15]. Five studies inferred that older age was a predictor for discrepancies; this was not retained after adjustment for confounders [5, 32, 35, 46, 47]. De Winter et al. identified increasing age as a predictor for discrepancies in a multivariable analysis [31]. Saint-Germain et al. showed in a geriatric population that an increasing age is correlated with less discrepancies, as detected through multivariable analysis [13].
Gender was tested in 24 studies [5,6,7, 9, 12, 13, 15, 24, 25, 27, 31, 32, 34, 38, 39, 42, 43, 45,46,47,48,49,50,51], of which 5 found that the female sex was associated with more discrepancies [27, 31, 39, 42, 50]. Of these 5 studies, only Balon et al. and De Winter et al. adjusted for confounders [31, 39].
Type of care service before admission was the subject of analysis in eight studies [6, 7, 12, 13, 31, 35, 44, 48]. Hellström et al. confirmed in a multivariable analysis that patients living at home before admission without community care service were at higher risk for PAM-related discrepancies, compared to patients who lived in a nursing home [7]. There was no significant difference in discrepancy rate for patients who lived at home with community care service, compared to patients who lived in a nursing home [7]. De Winter et al. included the type of care model provided before hospital admission in their prediction model [31]. Five studies [12, 46,47,48, 50] examined the difference between an elective admission and an emergency admission on the discrepancy rate. Patients who were admitted through the emergency department (ED) presented with more discrepancies than patients with scheduled admissions in the study performed by Pascual et al. The opposite was found by González-García et al., even after adjustment for confounders [46, 47].
Quélennec et al. detected, in a univariable analysis, that the proportion of patients with pneumonia was lower in the group of patients with discrepancies [9]. Nilsson et al. demonstrated that diabetic patients had a higher rate of discrepancies than non-diabetic patients; the association was no longer significant after adjusting for the number of treatments [51]. Tamblyn et al. also demonstrated that subjects with more than two ED visits in the past year had more discrepancies than subjects with none or only one ED visit. Adjustment for confounders rendered this effect insignificant [24]. Baena Parejo et al. showed that patients with an episode in the previous 3 months had more discrepancies on admission; after adjustment for confounders, this effect disappeared [32].
Two research teams investigated the effect of patients’ understanding of PAM on the number of discrepancies [12, 35]. Marinovic et al. found with a multivariable analysis that a low level of patients’ understanding was associated with more discrepancies [12]. Level of education was tested as a predictor by three studies [8, 12, 46]. Patients with no or limited to a primary educational level experienced more discrepancies in a bivariate analysis, but not when adjusted for other variables [46].
Comorbidities were subject of analysis in seven studies [5, 12, 15, 32, 45, 48, 49]. According to the univariate analysis performed by Rodríguez Vargas et al., the number of comorbidities could predispose a patient to discrepancies [48]. Mendes et al. and Baena Parejo et al. found a correlation between the Charlson comorbidity index and unintentional discrepancies [15, 32].
Medication-related predictors
The number of PAM was analyzed as a predictor in 26 studies [5,6,7,8, 12, 13, 15, 24, 27, 31,32,33,34,35, 38, 40,41,42,43, 45,46,47,48,49,50,51]. Twenty-three studies [6,7,8, 12, 13, 15, 24, 27, 31,32,33,34,35, 40, 42, 43, 45,46,47,48,49,50,51] found a significant effect, of which 13 [6,7,8, 12, 13, 24, 32, 33, 35, 43, 46,47,48] were able to show significance after adjustment for confounders; they demonstrated that a higher number of drugs was associated with a higher discrepancy rate.
In four studies, the link between specific drug classes and discrepancies was investigated [24, 25, 31, 34]. Tamblyn et al. concluded that therapeutic drug classes and the number of drugs correlated. Subsequently, only the number of drugs was included in the adjusted prediction model [24]. Chan et al. found that the PAM-related discrepancy rate for the “ear, nose, oropharynx, and eye,” “skin,” and “vitamins and mineral” classes was significantly higher than for the other classes in univariable analysis. Both prescription-only and over-the-counter (OTC) drugs were recorded, but dietary supplements and herbal or homeopathic products were excluded from the analysis as most of these products were not dispensed in the hospital [34]. Glintborg et al. furthermore showed that the type of Anatomical Therapeutic Chemical Classification, as defined by the WHO, was predictive for discrepancies upon admission in a multivariable analysis. Cardiovascular drugs were less likely to be omitted on admission [25]. De Winter et al. also found an association between specific drug classes and the number of discrepancies [31].
Setting-related predictors
The admitting service was tested as a predictor in four studies [28, 42, 46, 48]. Hatch et al. found that surgeons caring for trauma patients were likely to omit more medication compared to physicians caring for medical and non-trauma surgical patients [28].
Three studies examined whether the clinical experience of the admitting physicians had an influence on the discrepancy rate [31, 34, 48]. Rodríguez Vargas et al. found after adjustment for confounders that junior physicians had a higher risk on discrepancies than senior physicians [48].
Belda-Rustarao et al. and Baena Parejo et al. studied the effect of consulted sources on the discrepancy rate [32, 45]. Baena Parejo et al. found more discrepancies when the caregiver was interviewed as opposed to other sources [32].
Three studies investigated whether the number of consulted sources for the collection at the best possible PAM list was associated with more discrepancies [6, 13, 15]. Cornu et al. identified the number of information sources consulted as a risk factor for the presence of at least one discrepancy after adjustment for confounders [6].
Risk factors for potentially harmful unintentional discrepancies
Five studies focused on clinically relevant PAM-related errors [26, 27, 29, 30, 35]. In all these studies, the potential for patient harm of the PAM-related discrepancies was ascertained. In two studies, a systematic classification was used [27, 29], while in the other studies, assigning potential harm was based on expert opinion [26, 30, 35]. Adjustment for confounders was performed in four studies [26, 27, 29, 35]. The variables analyzed as risk factors for potentially harmful unintentional discrepancies are summarized in Table 4. Both statistically significant and insignificant results are shown in Table 4. A distinction was made between univariable and multivariable analyses as performed by the included studies.
Variables for which potential correlation with unintentional discrepancies was tested in several studies and found at least once to be statistically associated are discussed in more detail in the following.
Patient-related predictors
For each study, it was investigated whether age was a predictor for potentially harmful discrepancies [26, 27, 29, 30, 35]. In four studies, it was shown that older patients had a higher risk for clinically relevant discrepancies [26, 27, 30, 35]. In contrast, Pippins et al. concluded that patients older than 85 years had significantly less clinically relevant discrepancies compared to those younger than 50 years [29].
Three studies examined if gender was associated with more discrepancies [26, 27, 30]. Only Damlien et al. found that woman had more discrepancies than men [30].
Salanitro et al., Gleason et al., and Damlien et al. showed that patients with a medication list (available in the EMR (within 90 days prior to admission) or presented on admission) had less discrepancies with a potential for harm [27, 30, 35].
Patients’ understanding of their medication was scrutinized in two studies [29, 35]. Pippins et al. showed that patients with medium or low understanding of their medication had a higher risk for potentially harmful PAM-related discrepancies than patients with a high understanding of their medication [29].
Unroe et al. and Damlien et al. analyzed if the number of comorbidities was a potential predictor [26, 30]. Only Damlien et al. found that patients with more than three comorbidities had more discrepancies [30].
Medication-related predictors
Although it was investigated in each of the five abovementioned studies, if the total number of PAM was associated with potentially harmful discrepancies, only Salanitro et al., Damlien et al., and Gleason et al. showed that the risk for discrepancies increased per additional drug [27, 30, 35]. Pippins et al. found that five drug classes, which included gout medication, muscle relaxants, lipid-lowering agents, anti-depressants, and respiratory medication, were most frequently involved in the occurrence of potentially harmful discrepancies. They established that the intake of at least four of these drug classes increased the discrepancy rate [29]. Unroe et al. also found that the presence of high-risk medication, as defined by the authors as medication included on the Institute of Safe Medication Practice high-alert list or the North Carolina Narrow Therapeutic Index list, on admission was associated with a higher proportion of patients with PAM-related discrepancies [26].
Setting-related predictors
Unroe et al. showed that patients admitted to the general surgery ward were more likely to have a PAM-related discrepancy than those admitted to the cardiology ward [26].
Discussion
We found and assessed 56 potential predictors, of which 19 were significantly associated with discrepancies. The following 16 significant variables were identified using multivariable prediction models; they are listed hereafter according to the number of articles in which there was a statistically significant association: number of preadmission drugs, patient’s age, availability of a drug list, patients’ understanding of medication, usage of different outpatient pharmacies, number of high-risk drugs, discipline for which the patient is admitted, admitting physician’s experience, number and type of consulted sources, patient’s gender, type of care before admission, number of outpatient visits during the past year, class of medication, number of reimbursements, use of an electronic prescription system, and type of admission (elective vs emergency).
Some variables appeared contradictory. Four studies [26, 27, 30, 35] indicated that an increase in age increased the risk for potentially harmful discrepancies, in contrast to Pippins et al. [29], who found that patients older than 85 years had significantly less potentially harmful discrepancies than patients younger than 50. The latter was also seen by Saint-Germain et al., where in a geriatric population, a higher age was protective for all unintentional discrepancies [13]. This conflicting result could be explained by the possible difference in the degree of medical and social support between very old patients and other adults [29], signifying an inversion of the relation between age and discrepancy risk in the very old. As shown by Hellström et al., patients who lived in their own home with no care services had a higher risk for discrepancies than patients coming from a nursing home [7]. Remarkably, in contrast to Tamblyn et al. [24], Gleason et al. [27] found that patients visiting multiple community pharmacies were seen to have less PAM-related discrepancies. Pascual et al. [47] found that patients admitted trough the emergency department had more discrepancies than the ones with a scheduled admission; on the other hand, González-García [46] et al. found the opposite, while three other studies found no significant difference between an elective admission and an emergency admission [12, 48, 50].
Strengths and limitations
To our knowledge, this systematic review was the first attempt to identify predictors for unintentional discrepancies in medication histories, including patient-, medication-, and setting-related predictors. A portion of these predictors can be collected as part of patient care and are available upon hospital admission, such as age, gender, type of care before admission, and availability of a drug list. Other variables are possibly available shortly after admission or after the gathering of a PAM list by usual care, such as the number of preadmission drugs as reported by the admitting physician, the admitting service, and the admitting physician’s experience. These predictors could then be incorporated in clinical decision rules or care pathways to target high-risk patients in the medication reconciliation process on admission, especially when resources are limited.
Several of these factors were investigated in the majority of the assessed studies (e.g., age, number of preadmission drugs), while other predictors (e.g., availability of a drug list, health literacy, changes in therapy in the past year) were only subjected to analysis in few studies.
The methodological heterogeneity is characterized by the lack of uniform definitions or very diverse statistical analyses and subsequent reporting precluded meta-analysis. Furthermore, some of these methodological dissimilarities could explain the observed differences in (statistically significant) predictors.
No uniform type for a discrepancy was used in the selected manuscripts. This varied from drug therapy omissions as compared to the PAM list [25, 38, 44] or a combination of omissions and commissions (added therapy) [24, 43] to also including differences in dose, dosage, or route of administration [5, 8, 12, 14, 15, 27, 29, 32, 39, 42]. Two different types of intervention were used: a structured interview or one based on community pharmacy records. Another factor that might explain why some found a specific predictor to be significant while others did not is the sample size calculation or lack thereof. Sample sizes varied from 39 to 3592, which could imply that some studies lacked power to detect a statistically significant result. In this review, significant results were presented, but there was no focus on effect size. Some variables had a barely significant result, shown by a p value close to 0.05 (e.g., the effect of patients’ understanding of medication on discrepancies reported by Marinovic et al. [12]) (OR 1.79 (95%CI 1.01–3.16), p = 0.046)). Some odds ratios were furthermore characterized by a very broad 95% confidence interval (e.g., number of high-risk medication (OR 76.68 (95%CI 9.13–643.76) [26]). Differences in study settings could also have contributed to the ambiguity described above; e.g., wards with predominantly unplanned admissions might detect more inadequate medication histories than wards with more elective admissions [28]. Although several studies included patients from different wards [14, 15, 26,27,28, 33, 39, 42, 43, 46, 48,49,50,51], only six studies [26,27,28, 42, 46, 48] considered the specific type of admission ward as a predictor. The level of communication between community care services and hospitals is likely to vary between settings and countries and could therefore influence the discrepancy rate and the associated variables. The included subjects differed among the gathered studies: in some, only elderly [6, 9, 13, 34, 42, 43, 45, 48, 49] were included; in others, patients taking less than four types of drugs [34, 41, 42, 45, 48] were excluded. Since some researchers concluded that age and the number of PAM could be predictive for unintentional discrepancies, the variables polypharmacy and age could already be biased due to the inclusion criteria of certain studies. Also, some research groups looked selectively at prescription-only drugs [5, 7, 24, 25, 27, 40]. The possible difference in the exact point in time of the reconciliation process might also prove to be of relevance, as certain variables only become available later on during hospital stay. Three research groups did not distinguish between predictors for discrepancies on admission and at discharge [5, 8, 29]. Choice of statistical tests differed as well; it varied from non-parametric tests to predictive models which were whether or not corrected for confounders. Besides, not all researchers used the same variables to correct for in their multivariable analysis. Adjustment for confounders is desirable, on account of a possible interaction between multiple predictors such as a possible interaction between high age and polypharmacy.
The search was restricted to two databases. Since there was a substantial number of additional manuscripts retrieved from the second database, some manuscripts within the scope of this review may have been missed; however, the selected databases are large and widely used for systematic literature reviews. Furthermore, the database results were complemented with the snowball method. This review was intentionally limited to medication reconciliation in the hospital setting, so our results should be carefully interpreted as regard to their application to the ambulatory setting. It was also limited to hospital admission, since, in our opinion, identification of reconciliation discrepancies should be carried out as early as possible to prevent downstream potential drug-related problems. Only one reviewer performed the selection of the articles and the quality assessment. Yet a stringent method was used for both. Also, two other reviewers evaluated articles in case of any uncertainty. There were multiple meetings to ensure the quality of this review, and agreement was established between the three reviewers. Due to a lack of a single quality scale for this variety of non-randomized controlled trials, the NOS for cohort studies was used as proposed by the Cochrane Handbook for Systematic Reviews of Interventions [21, 22]. Because of the typical design of the included studies—studies without control group and lack of follow-up period—only few criteria were considered appropriate for actual grading (e.g., representativeness, assessment of outcome, adjustment for confounders) and could be used to discriminate between the different studies. In addition, the scale did not inquire whether studies were sufficiently powered to identify predictors. Future research is necessary to develop a quality assessment tool allowing proper evaluation of this type of studies.
Of the 35 selected articles, the relation between the number of discrepancies and the incidence of new and potentially avoidable adverse events was only explored in five studies [26, 27, 29, 30, 35]. Pippins et al., Damlien et al., and Gleason et al. rated with an independent team the discrepancies’ potential for harm, including the presumed severity [27, 29]. Gleason et al. classified the harm according to an adjusted National Coordinating Council for Medication Error Reporting and Prevention Index [27]. Pippins et al. rated the supposed severity of the discrepancies according to a previously worked out classification of Bates et al. [29, 37]. In our opinion, the pursuit of predictors for clinically relevant discrepancies is important, as the prevention and early resolution of these discrepancies might eventually help in preventing avoidable adverse events altogether. Additional studies are needed to identify patients at risk for clinically significant discrepancies potentially causing harm and resulting in actual harm [2].
Additional prospective studies focusing on potentially harmful discrepancies with none or few exclusion criteria so that the results can be generalizable are necessary. The predictors should be clearly defined (e.g., ED triage acuity scale [52]) and limited to those that are readily available upon admission (or very shortly thereafter) (e.g., age). Afterwards, these predictors could be implemented in clinical decision rules or care pathways to predict patients with a high risk for unintentional discrepancies. Prospective validation of these prediction models including aforementioned predictors should be the next step to render these models useable in practice. In a subgroup analysis, Schnipper et al. advocated the use of a potential adverse drug event (PADE) risk score to identify those high-risk patients in whom medication reconciliation should be performed in order to effectively prevent PADE [10]. This risk score was developed by Pippins et al. [29]. At the time of this review, the validation study of the Medication Reconciliation Quality Improvement Study risk stratification tool was still ongoing, which included a risk stratification tool based on expert consensus. It aims to demonstrate a reduction in PAM-related discrepancies and an improvement in patient outcomes [53, 54]. Furthermore, more research is necessary to facilitate the medication reconciliation process by providing access to all health care providers pre- and post admission to all dispensed medications. Relying on electronic prescribing registers as the only source of drug record may potentially jeopardize patient care, as shown by Engqvist et al. [55] Electronic prescribing registers can provide accurate information at the moment of drug dispensation, but is not necessarily correct and complete at time of hospital admission. Hence, a structured medication reconciliation process based on multiple sources will still be of importance for some high-risk patients.
Conclusion
This systematic review has identified several predictors for (potentially harmful) discrepancies in medication histories upon hospital admission, including patient, medication-, and setting-related predictors. A high number of preadmission drugs were found to be a significant predictor for unintentional discrepancies. Also, age had a predictive value for potentially harmful discrepancies. These variables should be validated in risk prediction models and evaluated to improve their performance in a more generalizable population.
References
Mueller SK, Sponsler KC, Kripalani S, Schnipper JL (2012) Hospital-based medication reconciliation practices: a systematic review. Arch Intern Med 172(14):1057–1069. doi:10.1001/archinternmed.2012.2246
Kwan JL, Lo L, Sampson M, Shojania KG (2013) Medication reconciliation during transitions of care as a patient safety strategy: a systematic review. Ann Intern Med 158(5 Pt 2):397–403. doi:10.7326/0003-4819-158-5-201303051-00006
Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE (2005) Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. Can Med Assoc J 173(5):510–515
Lehnbom EC, Stewart MJ, Manias E, Westbrook JI (2014) Impact of medication reconciliation and review on clinical outcomes. In: Ann Pharmacothered. (c) The Author(s) 2014., pp 1298–1312
Climente-Marti M, Garcia-Manon ER, Artero-Mora A, Jimenez-Torres NV (2010) Potential risk of medication discrepancies and reconciliation errors at admission and discharge from an inpatient medical service. Ann Pharmacother 44(11):1747–1754. doi:10.1345/aph.1P184
Cornu P, Steurbaut S, Leysen T, De Baere E, Ligneel C, Mets T, Dupont AG (2012) Effect of medication reconciliation at hospital admission on medication discrepancies during hospitalization and at discharge. Int J Clin Pharm 34(1):213–214. doi:10.1007/s11096-011-9602-2
Hellstrom LM, Bondesson A, Hoglund P, Eriksson T (2012) Errors in medication history at hospital admission: prevalence and predicting factors. BMC Clin Pharmacol 12:9. doi:10.1186/1472-6904-12-9
Feldman LS, Costa LL, Feroli ER Jr, Nelson T, Poe SS, Frick KD, Efird LE, Miller RG (2012) Nurse-pharmacist collaboration on medication reconciliation prevents potential harm. J Hosp Med 7(5):396–401. doi:10.1002/jhm.1921
Quelennec B, Beretz L, Paya D, Blickle JF, Gourieux B, Andres E, Michel B (2013) Potential clinical impact of medication discrepancies at hospital admission. Eur J Intern Med 24(6):530–535. doi:10.1016/j.ejim.2013.02.007
Schnipper JL, Hamann C, Ndumele CD, Liang CL, Carty MG, Karson AS, Bhan I, Coley CM, Poon E, Turchin A, Labonville SA, Diedrichsen EK, Lipsitz S, Broverman CA, McCarthy P, Gandhi TK (2009) Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events a cluster-randomized trial. Arch Intern Med 169(8):771–780
De Winter S, Vanbrabant P, Spriet I, Desruelles D, Indevuyst C, Knockaert D, Gillet JB, Willems L (2011) A simple tool to improve medication reconciliation at the emergency department. Eur J Intern Med 22(4):382–385. doi:10.1016/j.ejim.2011.03.010
Marinovic I, Marusic S, Mucalo I, Mesaric J, Bacic Vrca V (2016) Clinical pharmacist-led program on medication reconciliation implementation at hospital admission: experience of a single university hospital in Croatia. Croat Med J 57(6):572–581
Saint-Germain P, Ruelle M, Mary A, Sid Idris S, Hannat S, Pelloquin N, Jouanny P, Terrier-Lenglet A (2016) The clinical impact of treatment discrepancies recorded for 200 patients in an acute geriatric unit. Rev Med Interne 37(10):667–673. doi:10.1016/j.revmed.2016.02.017
Breuker C, Abraham O, di Trapanie L, Mura T, Macioce V, Boegner C, Jalabert A, Villiet M, Castet-Nicolas A, Avignon A, Sultan A (2017) Patients with diabetes are at high risk of serious medication errors at hospital: interest of clinical pharmacist intervention to improve healthcare. Eur J Intern Med 38:38–45. doi:10.1016/j.ejim.2016.12.003
Mendes AE, Lombardi NF, Andrzejevski VS, Frandoloso G, Correr CJ, Carvalho M (2016) Medication reconciliation at patient admission: a randomized controlled trial. Pharm Pract 14 (1) DOI: 10.18549/PharmPract.2016.01.656
Greenwald JL, Halasyamani L, Greene J, LaCivita C, Stucky E, Benjamin B, Reid W, Griffin FA, Vaida AJ, Williams MV (2010) Making inpatient medication reconciliation patient centered, clinically relevant and implementable: a consensus statement on key principles and necessary first steps. J Hosp Med 5(8):477–485. doi:10.1002/jhm.849
Grimes T, Fitzsimons M, Galvin M, Delaney T (2013) Relative accuracy and availability of an irish national database of dispensed medication as a source of medication history information: observational study and retrospective record analysis. J Clin Pharm Ther 38(3):219–224
Zoni AC, Duran Garcia ME, Jimenez Munoz AB, Salomon Perez R, Martin P, Herranz Alonso A (2012) The impact of medication reconciliation program at admission in an internal medicine department. Eur J Intern Med 23(8):696–700. doi:10.1016/j.ejim.2012.08.013
Sponsler KC, Neal EB, Kripalani S (2015) Improving medication safety during hospital-based transitions of care. Cleve Clin J Med 82(6):351–360. doi:10.3949/ccjm.82a.14025
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264–269 W264
Wells GA SB, O’Connell D, Peterson J, Welch V, Losos M ([cited31may2014]) The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Available from: URL:http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp In: ed
http://handbook.cochrane.org/ cited: 15 march 2015. In: ed
Oremus M HA, Raina P. (2011) Health risk appraisal [Internet]. Agency for Healthcare Research and Quality, (US)
Tamblyn R, Poissant L, Huang A, Winslade N, Rochefort CM, Moraga T, Doran P (2014) Estimating the information gap between emergency department records of community medication compared to on-line access to the community-based pharmacy records. J Am Med Inform Assoc 21(3):391–398. doi:10.1136/amiajnl-2013-001704
Glintborg B, Poulsen HE, Dalhoff KP (2008) The use of nationwide on-line prescription records improves the drug history in hospitalized patients. Br J Clin Pharmacol 65(2):265–269. doi:10.1111/j.1365-2125.2007.03017.x
Unroe KT, Pfeiffenberger T, Pharm SR, Jastrzembski J, Lokhnygina Y, Colon-Emeric C (2010) Inpatient medication reconciliation at admission and discharge: a retrospective cohort study of age and other risk factors for medication discrepancies. Am J Geriatr Pharmacother 8(2):115–126
Gleason KM, McDaniel MR, Feinglass J, Baker DW, Lindquist L, Liss D, Noskin GA (2010) Results of the Medications at Transitions and Clinical Handoffs (MATCH) study: an analysis of medication reconciliation errors and risk factors at hospital admission. J Gen Intern Med 25(5):441–447. doi:10.1007/s11606-010-1256-6
Hatch J, Becker T, Fish J (2011) Difference between pharmacist-obtained and physician-obtained medication histories in the intensive care unit. Hosp Pharm 46(4):262–268
Pippins JR, Gandhi TK, Hamann C, Ndumele CD, Labonville SA, Diedrichsen EK, Carty MG, Karson AS, Bhan I, Coley CM, Liang CL, Turchin A, McCarthy PC, Schnipper JL (2008) Classifying and predicting errors of inpatient medication reconciliation. J Gen Intern Med 23(9):1414–1422. doi:10.1007/s11606-008-0687-9
Damlien L, Davidsen N, Nilsen M, Godo A, Moger TA, Viktil KK (2015) Drug safety at admission to emergency department: an innovative model for PRIOritizing patients for MEdication Reconciliation (PRIOMER). Eur J Emerg Med. doi:10.1097/mej.0000000000000355
De Winter S, Vanbrabant P, Laeremans P, Foulon V, Willems L, Verelst S, Spriet I (2017) Developing a decision rule to optimise clinical pharmacist resources for medication reconciliation in the emergency department. Emerg Med J. doi:10.1136/emermed-2016-205804
Baena Parejo MI, Borrego AMJ, Ruiz JA, Monjó MC, García-Peláez M, Hernanz BC, Hernández MAC, Fernández MIC, Riera MP, Sánchez RG, Sánchez LG, López CV, Echeverria MDM, Serrano PM (2015) Medication list assessment in Spanish hospital emergency departments. J Emerg Med 48(4):416–423. doi:10.1016/j.jemermed.2014.06.063
Lubowski TJ, Cronin LM, Pavelka RW, Briscoe-Dwyer LA, Briceland LL, Hamilton RA (2007) Effectiveness of a medication reconciliation project conducted by PharmD students. Am J Pharm Educ 71(5):94
Chan AH, Garratt E, Lawrence B, Turnbull N, Pratapsingh P, Black PN (2010) Effect of education on the recording of medicines on admission to hospital. J Gen Intern Med 25(6):537–542. doi:10.1007/s11606-010-1317-x
Salanitro AH, Osborn CY, Schnipper JL, Roumie CL, Labonville S, Johnson DC, Neal E, Cawthon C, Businger A, Dalal AK, Kripalani S (2012) Effect of patient- and medication-related factors on inpatient medication reconciliation errors. J Gen Intern Med 27(8):924–932. doi:10.1007/s11606-012-2003-y
Schnipper JL, Roumie CL, Cawthon C, Businger A, Dalal AK, Mugalla I, Eden S, Jacobson TA, Rask KJ, Vaccarino V, Gandhi TK, Bates DW, Johnson DC, Labonville S, Gregory D, Kripalani S (2010) Rationale and design of the Pharmacist Intervention for Low Literacy in Cardiovascular Disease (PILL-CVD) study. Circ Cardiovasc Qual Outcomes 3(2):212–219. doi:10.1161/circoutcomes.109.921833
Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D, Laffel G, Sweitzer BJ, Shea BF, Hallisey R et al (1995) Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prev Study Group JAMA 274(1):29–34
Andersen SE, Pedersen AB, Bach KF (2003) Medication history on internal medicine wards: assessment of extra information collected from second drug interviews and GP lists. Pharmacoepidemiol Drug Saf 12(6):491–498
Balon J, Thomas SA (2011) Comparison of hospital admission medication lists with primary care physician and outpatient pharmacy lists. J Nurs Scholarsh 43(3):292–300
Knez L, Suskovic S, Rezonja R, Laaksonen R, Mrhar A (2011) The need for medication reconciliation: a cross-sectional observational study in adult patients. Respir Med 105(SUPPL. 1):S60–S66
Cornish PL, Knowles SR, Marchesano R, Tam V, Shadowitz S, Juurlink DN, Etchells EE (2005) Unintended medication discrepancies at the time of hospital admission. Arch Intern Med 165(4):424–429
Rodriguez Vargas B, Delgado Silveira E, Montero Errasquin B, Bermejo Vicedo T (2013) Conciliation of the pharmacological treatment of patients older than 65 years at hospital admission. Atencion Farmaceutica 15(1):35–39
Beers MH, Munekata M, Storrie M (1990) The accuracy of medication histories in the hospital medical records of elderly persons. J Am Geriatr Soc 38(11):1183–1187
Steurbaut S, Leemans L, Leysen T, De Baere E, Cornu P, Mets T, Dupont AG (2010) Medication history reconciliation by clinical pharmacists in elderly inpatients admitted from home or a nursing home. Ann Pharmacother 44(10):1596–1603. doi:10.1345/aph.1P192
Belda-Rustarazo S, Cantero-Hinojosa J, Salmeron-García A, González-García L, Cabeza-Barrera J, Galvez J (2015) Medication reconciliation at admission and discharge: an analysis of prevalence and associated risk factors. Int J Clin Pract 69(11):1268–1274. doi:10.1111/ijcp.12701
González-García L, Salmerón-García A, García-Lirola M, Moya-Roldán S, Belda-Rustarazo S, Cabeza-Barrera J (2016) Medication reconciliation at admission to surgical departments. J Eval Clin Pract 22(1):20–25. doi:10.1111/jep.12403
Pascual O, Real JM, Uriarte M, Larrodé I, Alonso YM, Abad MR (2015) Evaluation of medication reconcilliation in a trauma unit. Rev Esp Cir Ortop Traumatol 59(2):91–96. doi:10.1016/j.recot.2014.07.003
Rodriguez Vargas B, Delgado Silveira E, Iglesias Peinado I, Bermejo Vicedo T (2016) Prevalence and risk factors for medication reconciliation errors during hospital admission in elderly patients. Int J Clin Pharm 38(5):1164–1171. doi:10.1007/s11096-016-0348-8
Perehudoff K, Azermai M, Somers A, Vander Stichele R, Petrovic M (2015) Medication discrepancies in older patients admitted to non-geriatric wards: an exploratory study. Eur Geriatr Med 6(1):41–45. doi:10.1016/j.eurger.2014.10.005
Spalla LR, Castilho SR (2016) Medication reconciliation as a strategy for preventing medication errors. Braz J Pharm Sci 52(1):143–150. doi:10.1590/S1984-82502016000100016
Nilsson N, Lea M, Lao Y, Wendelbo K, Gløersen G, Mowé M, Blix HS, Viktil KK (2015) Medication discrepancies revealed by medication reconciliation and their potential short-term and long-term effects: a Norwegian multicentre study carried out on internal medicine wards. Eur J Hosp Pharm 22(5):298–303. doi:10.1136/ejhpharm-2015-000686
Wuerz RC, Milne LW, Eitel DR, Travers D, Gilboy N (2000) Reliability and validity of a new five-level triage instrument. Acad Emerg Med 7(3):236–242
Salanitro AH, Kripalani S, Resnic J, Mueller SK, Wetterneck TB, Haynes KT, Stein J, Kaboli PJ, Labonville S, Etchells E, Cobaugh DJ, Hanson D, Greenwald JL, Williams MV, Schnipper JL (2013) Rationale and design of the Multicenter Medication Reconciliation Quality Improvement Study (MARQUIS). BMC Health Serv Res 13:230
(Cited: 28 June 2015 ) Marquis implementation manual. A guide for medication reconciliation quality improvement. September, 2011. Available from URL: http://tools.hospitalmedicine.org/resource_rooms/imp_guides/MARQUIS/marquis.html In: ed
Engqvist I, Wyss K, Asker-Hagelberg C, Bergman U, Odar-Cederlöf I, Stiller CO, Fryckstedt J (2015) Which medication is the patient taking at admission to the emergency ward? Still unclear despite the Swedish prescribed drug register. PLoS One 10(6). doi:10.1371/journal.pone.0128716
Acknowledgements
We want to thank Marleen Michels, for peer-reviewing our search query.
Contributors
Julie Hias, Lorenz Van der Linden, and Sabrina De Winter participated in the study concept, retrieval of articles, data analysis, interpretation of data, and preparation of the manuscript. Isabel Spriet participated in the study concept, interpretation of data, and preparation of the manuscript. Jos Tournoy, Peter Vanbrabant, and Ludo Willems participated in the interpretation of data and preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
None.
Additional information
Julie Hias and Lorenz Van der Linden shared first author.
Rights and permissions
About this article
Cite this article
Hias, J., Van der Linden, L., Spriet, I. et al. Predictors for unintentional medication reconciliation discrepancies in preadmission medication: a systematic review. Eur J Clin Pharmacol 73, 1355–1377 (2017). https://doi.org/10.1007/s00228-017-2308-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-017-2308-1