Abstract
Purpose
Bisphosphonates are synthetic analogues of pyrophosphate usually used in treating bone disorders such as osteoporosis, Paget’s disease, fibrous dysplasia, hypercalcemia of malignancy, and inflammation-related bone loss. Though therapeutic effects of bisphosphonates depend primarily on their inhibitory effect on osteoclasts, increasing attention is being given to other effector cells, such as osteoblasts. This review focuses on the presumed effect of bisphosphonates on osteoblasts.
Methods
A review of the literature was conducted to evaluate the pharmacodynamic effects of bisphosphonates including inhibition of osteoclasts and apoptosis of osteocytes and osteoblasts as well as their potential stimulatory effects on the proliferation of osteoblasts.
Results
Studies have demonstrated that bisphosphonates may stimulate proliferation of osteoblasts and inhibit apoptosis of osteocytes and osteoblasts.
Conclusion
Considering that osteoblasts may be involved in bone disorders, such as osteoporosis, osteopetrosis, osteogenesis imperfecta, and Paget’s disease, and that bisphosphonates may stimulate proliferation of osteoblasts and inhibit apoptosis of osteocytes and osteoblasts, it is conceivable that a role for bisphosphonates exists in these diseases beyond merely the osteoclast influence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bisphosphonates (BPs) are synthetic analogues of pyrophosphate usually used in treating disorders of bone such as osteoporosis, Paget’s disease, fibrous dysplasia, hypercalcemia of malignancy, and inflammation-related bone loss [1–5].
BPs can further be separated into nitrogen-containing and non-nitrogen-containing BPs. Nitrogen-containing BPs, such as alendronate, ibandronate, risedronate, and zoledronate, inhibit the mevalonate pathway of cholesterol synthesis via inhibition of the enzyme farnesyl diphosphate synthase and blocking prenylation of small GTPases leading to interruption of osteoclast function [6]. Non-nitrogen-containing BPs, such as etidronate and clodronate, suppress bone resorption by incorporating into intracellular nonhydrolyzable ATP analogues that have no releasable energy content, thus leading to osteoclast death [7, 8]. Moreover, BPs are able to chelate calcium ions and bind to hydroxyapatite crystals on bone surfaces [9].
BPs determine an acidification process at the osteoclast-mineral interface, disrupt the actin attachment sites on the bone surface, and interrupt bone resorption by disturbing the ruffled border function [10–14].
Even if therapeutic effects of BPs depend on their inhibitory effect on osteoclasts, there is increasing evidence that BPs may play a role in osteoblastogenesis [15–21].
Osteoblasts
Osteoblasts are mononuclear specialized cells derived from mesenchymal precursor cells, responsible for formation, deposition, and mineralization of bone tissue, principally through the deposition of calcium phosphate crystals, such as hydroxyapatite, and extracellular matrix, including proteoglycans and type 1 collagen.
Osteoblasts are involved in osteoclast regulation [22]. The interaction of nuclear factor (NF)-ĸB ligand (RANKL), a membrane-residing protein on osteoblasts that may also be isolated as a soluble factor as a consequence of matrix metalloproteinases (MMPs) proteolysis, with RANK, a type I transmembrane receptor expressed on osteoclast precursors, is involved in osteoclast precursor differentiation into osteoclasts. The formation of the RANK-RANKL complex results in a cascade characterized by the trimerization of RANK and the activation of TNF receptor-associated factor 6 (TRAF6), which induces NF-ĸB and mitogen-activated protein kinases (MAPKs), including Jun N-terminal kinase (JNK) and p38, involved in the activation of transcription factors such as c-Fos, c-Src, and microphtalmia transcription factor (MITF) [23–25]. On the other hand, osteoblasts are also involved in osteoprotegerin (OPG) production, a soluble decoy receptor for RANKL, which competitively inhibits the binding of RANKL to RANK on the cell membrane of osteoclasts, thus impeding RANK activation and the subsequent osteoclast activation [26].
The control of osteoclastogenesis by osteoblasts underlines the importance of these cells in the modulation of bone resorption. Moreover, osteoblasts express numerous other molecules involved in the regulation of osteoclastogenesis such as tumor necrosis factor (TNF)-α, interleukin-1 (IL-1), and macrophage-colony stimulating factor (M-CSF).
TNF-α induces the production of RANKL both directly by expressing factors such as RANK, TRAF6, and NF-ĸB, which are involved in activation of osteoclast precursor cells in the early phase of osteoclast differentiation, and indirectly by stimulating osteoclastogenesis-supporting mesenchymal cells [27–30]. The binding of TNF-α to two receptors, TNF receptor type I (TNFRI) and TNF receptor type II (TNFRII), is responsible for its biological activity. Only the addition of neutralizing anti-TNFRI, but not anti-TNFRII antibodies, suppresses RANKL-induced osteoclastogenesis, suggesting that just TNFRI is involved in RANKL-induced osteoclastogenesis [31, 32].
IL-1 is a potential regulator of osteoclastogenis only in the presence of adequate levels of RANKL and induces the activation of a p38 MAP-kinase in osteoclast precursor and marrow stromal cells that is involved in TNF-α-mediated osteoclastogenesis [33].
M-CSF is involved in recruiting osteoclasts, as demonstrated in mice with mutation in the coding region of the M-CSF; the mice were characterized by osteoclast-deficient osteopetrosis [34]. M-CSF stimulates RANK expression on the cell surface of pre-osteoclasts rendering them reactive to RANKL [35]. Moreover, M-CSF induces osteoclast differentiation via binding to c-fms, a tyrosine kinase receptor that in turn induces ERK1/2 and PI3-K/AKT activation [36].
Role of osteoblasts in bone disorders
Several studies have showed that osteoblasts may be involved in bone disorders, such as osteoporosis, osteopetrosis, osteogenesis imperfecta, and Paget’s disease.
Even if osteoporosis is primarily characterized by an imbalance of bone turn-over favoring osteoclastic bone resorption, osteoblasts play a role in this disease. Osteoporosis is mainly observed in postmenopause because of the hormonal modification related to menopause. The decreased levels of estrogen in postmenopausal women are responsible for an increased osteoclastogenesis. In fact, estrogen has been demonstrated to increase OPG levels [37]. Moreover, estrogen has an inhibitory effect on osteoblast production of numerous paracrine factors, including IL-1, IL-6, and TNF-α, which are involved in osteoclastogenesis, and inhibits the transcription factor Egr-1, which is responsible for M-CSF production [38, 39]. In postmenopausal women, the decreased levels of estrogen are correlated with increased levels of IL-1, IL-6, TNF-α, and M-CSF, responsible for an augmented bone resorption.
Osteopetrosis is a descriptive term that refers to a group of rare, heritable disorders of the skeleton where the rate of bone formation is higher than the rate of bone resorption. Osteopetrosis is caused by failure of osteoclast development or function, and mutations in at least 10 genes have been identified as causative in humans, accounting for 70% of all cases. It has been hypothesized that osteopetrosis is characterized by an imbalance between bone formation and bone resorption due to an altered communication between osteoblasts and osteoclasts. It has been demonstrated that in cultured osteoblast-like cells from patients affected by osteopetrosis, the production of osteocalcin, which is a marker for mature osteoblasts, and M-CSF, which is involved in osteoclastogenesis, was inhibited, while normal levels of alkaline phosphatase were detected [40]. These results suggest that osteopetrosis is characterized by a deficient differentiation of pre-osteoblasts into mature osteoblasts, and a reduced maturation and differentiation of osteoclasts.
Osteogenesis imperfecta is a group of genetic bone disorders characterized by fractures with minimal or absent trauma, dentinogenesis imperfecta, and hearing loss. About 90% of individuals with osteogenesis imperfecta types I, II, III, and IV have an identifiable mutation in either gene COL1A1 or COL1A2. In recent years, a role for osteoblasts has been described in three new types of osteogenesis imperfecta. Differently from types I, II, and III, the new types, V, VI, and VII, do not have mutations within type 1 collagen and are characterized by reduced levels of alkaline phosphatase and normal levels of osteocalcin, suggesting the presence of an altered osteoblast differentiation, rather than bone formation [41–44].
A role for osteoblasts has been hypothesized also in Paget’s disease. Although its etiology is still unknown, alterations in osteoclast function have been described [45]. Nevertheless, considering that Paget’s disease is characterized by a high alkaline phosphatase activity, which is an indicator of high osteoblast activity, the presence of a contextual imperfection in osteoblast function and in the osteoclast-osteoblast interaction has been hypothesized [45, 46]. Some data seem to support the hypothesis that a defect in the RANKL-OPG system is responsible for abnormal osteoclast activity that results in a further osteoblast activation in order to balance the augmented bone resorption. In fact, in patients affected by Paget’s disease, high RANKL mRNA transcripts, lower OPG levels, and a major responsiveness of osteoclast precursors to RANKL stimulation have been found in osteoblast-like cells compared to cells from normal patients [47–49].
BPs and osteoblasts
BPs are used to treat numerous diseases, such as osteoporosis, Paget’s disease, osteogenesis imperfecta, bone metastases, hypercalcemia of malignancy, fibrous dysplasia, and inflammation-related bone loss.
Already in the 1990s, in vitro studies showed that osteoblasts treated with BPs inhibit osteoclastogenesis [50, 51]. Although their primary action may be an inhibitory effect on osteoclasts, increasing attention is being given to other effector cells that may be influenced by BPs [52]. In recent years, it has been hypothesized that a further target of BPs may be osteoblasts, which subsequently influence osteoclasts. In fact, BPs control osteoblast metabolism, albeit with varying or conflicting effects, depending on the type of BPs used and the different experimental models.
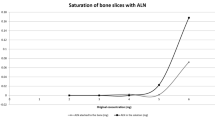
Laboratory data suggest that BPs have a mitogenic effect on osteoblasts [19–21]. Studies have demonstrated that BPs inhibit the expression of RANKL and increase the expression of OPG in human osteoblastic cells, suggesting that the antiresorptive effect of BPs is mediated by osteoblast influence on RANKL signaling [53, 54]. Moreover, other studies have showed that BPs may increase or decrease osteoblastogenesis in relation to their concentration: a pro-osteoblastogenic effect has been seen at lower concentrations of BPs ranging from 10−9 to 10−6 M, whereas the inhibitory effect has been found at concentrations higher than 10−5 M [21, 55–62].
Moreover, BPs may be involved in the treatment of skeletal conditions where macrophage-derived cytokines are important, including arthritis and implant loosening, by reducing the inhibitory effects of macrophages on osteoblasts, as demonstrated in vitro by addition of BPs to co-cultures of osteoblasts and macrophages [63].
By using in vitro models, Im et al. [21] have demonstrated the anabolic effect of alendronate and risedronate on osteoblasts. Following the proliferation of a primary human trabecular bone cell culture and MG-63 osteoblast-like cell line after treatment with BPs, the maturation of osteoblasts was assayed using alkaline phosphatase bioassay and reverse transcription-polymerase chain reaction for markers of osteoblast differentiation. Treatment with BPs appreciably increased the cell number and alkaline phosphatase activity over controls.
Pamidronate and zolendronate are responsible for increasing protein synthesis, secretion of type I collagen, and activity of alkaline phosphatase in osteoblasts even if they inhibit proliferation of other cells, including macrophages, linfocites, myeloma, and lung cancer cells. Their mechanism of action directly involves the cellular metabolism. On the other hand, other BPs, such as etidronate, are characterized by a different mechanism of action based on chelation of divalent ions in the culture medium, which probably is responsible for a different function. In fact, etidronate inhibits in vitro osteoblast proliferation at concentrations greater than pamidronate and zoledronic acid [64].
BPs are involved in inducing osteoblast precursor proliferation and stimulate the development of mineralized nodules in murine and human bone marrow cultures in vitro [65]. In particular, clodronate promotes osteoblast differentiation in cultures of osteoblast-like line cells, such as ST2 and MC3T3-E1 cells, and in rat organ cultures, while etidronate stimulates osteoblast differentiation only in MC3T3-E1 cells [66]. Moreover, etidronate stimulates osteoblastogenesis and wound closure in rat calvaria [67]. In contrast, alendronate and pamidronate show no effect on ST2 and MC3T3-E1 cells or in rat organ cultures of osteoblasts, while alendronate and risedronate significantly increase osteoblast and osteoblast progenitor proliferation in primary human trabecular bone cell culture and in MG-63 osteoblast-like cell line, suggesting that BPs may have different effects on osteoblast formation [66].
By using primary human osteoblast cultures obtained from cancellous bone of osteoarthritic and osteoporotic patients and a corresponding healthy control group, Corrado et al. [68] found that neridronate can modify the metabolic activity of human osteoblasts by enhancing or decreasing their biosynthetic activity, both in normal and in pathological conditions, depending on compound concentration and on different cell types. Recently, these data have been confirmed by using primary human osteoblast cultures obtained from cancellous bone of healthy subjects undergoing bone marrow biopsy, treated with increasing concentrations of zoledronate, with and without 1,25(OH)2 vitamin D3. The results of this study have demonstrated that BPs have different cellular biochemical effects depending on dosage and sustain the hypothesis that their positive effect on bone mineral density could be partially due to an anabolic action on osteoblasts [69].
Administration of BPs has been related to apoptosis inhibition on cells of the osteoblastic lineage [70–77]. The existence of different mechanisms of action for the prosurvival effect of BPs has been hypothesized. Recently, Bellido and Plotkin [78] demonstrated that the expression of connexin (Cx) 43 on osteoblast surface is responsible for this anti-apoptotic effect. In fact, the opening of Cx43 hemichannels leads to the sequential phosphorylation of kinases such as Src kinase, extracellular signal-regulated kinases (ERKs), ERK cytoplasmic target p90RSK kinase, BAD, and C/EBPβ, resulting in inhibition of apoptosis.
Concluding remarks
Though therapeutic effects of BPs depend primarily on their inhibitory effect on osteoclasts, increasing attention is being given to other effector cells, such as osteoblasts. BPs may stimulate proliferation of osteoblasts and inhibit apoptosis of osteocytes and osteoblasts. Although in vitro studies have demonstrated a role for BPs in osteoblast stimulation, effects of BPs on osteoblasts in vivo remain unclear because of numerous indirect effects on the remodeling cycle mediated through reduction of bone resorption. Indeed, in vitro studies with BPs require a careful interpretation with regard to the presence of many confounding factors, such as different BP concentrations and different models used, which may explain the presence of contrasting results. The significance of these data needs to be assessed considering that in vivo osteoblasts are exposed to different BPs concentrations in the bone microenvironment.
Considering that osteoblasts may be involved in bone disorders such as osteoporosis, osteopetrosis, osteogenesis imperfecta, and Paget’s disease, it is conceivable that there is a role for BPs in these diseases that goes beyond the mere osteoclast influence.
References
Ralston SH, Hacking L, Willocks L, Bruce F, Pitkeathly DA (1989) Clinical, biochemical, and radiographic effects of aminohydroxypropylidene bisphosphonate treatment in rheumatoid arthritis. Ann Rheum Dis 48:396–399
Eggelmeijer F, Papapoulos SE, van Paassen HC, Dijkmans BA, Breedveld FC (1994) Clinical and biochemical response to single infusion of pamidronate in patients with active rheumatoid arthritis: a double blind placebo controlled study. J Rheumatol 21:2016–2020
Lala R, Matarazzo P, Bertelloni S, Buzi F, Rigon F, de Sanctis C (2000) Pamidronate treatment of bone fibrous dysplasia in nine children with McCune-Albright syndrome. Acta Paediatr 89:188–193
Rodan GA, Martin TJ (2000) Therapeutic approaches to bone diseases. Science 289:1508–1514
Lane JM, Khan SN, O’Connor WJ et al (2001) Bisphosphonate therapy in fibrous dysplasia. Clin Orthop 382:6–12
Reszka AA, Rodan GA (2004) Nitrogen-containing bisphosphonate mechanism of action. Mini Rev Med Chem 4:711–719
Frith JC, Monkkonen J, Blackburn GM, Russell RG, Rogers MJ (1997) Clodronate and liposome-encapsulated clodronate are metabolized to a toxic ATP analog, adenosine 5’-(beta, gammadichloromethylene) triphosphate, by mammalian cells in vitro. J Bone Miner Res 12:1358–1367
Frith JC, Monkkonen J, Auriola S, Monkkonen H, Rogers MJ (2001) The molecular mechanism of action of the antiresorptive and antiinflammatory drug clodronate: evidence for the formation in vivo of a metabolite that inhibits bone resorption and causes osteoclast and macrophage apoptosis. Arthritis Rheum 44:2201–2210
Rogers MJ (2003) New insights into the molecular mechanisms of action of bisphosphonates. Curr Pharm Des 9:2643–2658
Sato M, Grasser W (1990) Effects of bisphosphonates on isolated rat osteoclasts as examined by reflected light microscopy. J Bone Miner Res 5:31–39
Sato M, Grasser W, Endo N et al (1991) Bisphosphonate action. Alendronate localization in rat bone and effects on osteoclast ultrastructure. J Clin Invest 88:2095–2105
Murakami H, Takahashi N, Sasaki T et al (1995) A possible mechanism of the specific action of bisphosphonates on osteoclasts: tiludronate preferentially affects polarized osteoclasts having ruffled borders. Bone 17:137–144
Zimolo Z, Wesolowski G, Rodan GA (1995) Acid extrusion is induced by osteoclast attachment to bone. Inhibition by alendronate and calcitonin. J Clin Invest 96:2277–2283
Rodan GA, Fleisch HA (1996) Bisphosphonates: mechanisms of action. J Clin Invest 97:2692–2696
Tsuchimoto M, Azuma Y, Higuchi O et al (1994) Alendronate modulates osteogenesis of human osteoblastic cell in vitro. Jpn J Pharmacol 66:25–33
Giuliani N, Girasole G, Pedrazzoni M, Passeri G, Gatti C, Passeri M (1995) Alendronate stimulates b-FGF production and mineralized nodule formation in human osteoblastic cells and osteoblastogenesis in human bone marrow cultures. J Bone Miner Res 10:S171
Gallagher JA, Gundle R, Beresford JN (1998) Isolation and culture of bone-forming cells (osteoblasts) from human bone. In: Jones GE (ed) Methods in molecular medicine: human cell culture protocols. Humana, Totowa, pp 233–262
Giuliani N, Pedrazzoni M, Negri G, Passeri G, Impicciatore M, Girasole G (1998) Biphosphonates stimulate formation of osteoblast precursors and mineralized nodules in murine and human bone marrow cultures in vitro and promote early osteoblastogenesis in young and aged mice in vivo. Bone 22:455–461
Mathov I, Plotkin LI, Sgarlata CL, Leoni J, Bellido T (2001) Extracellular signal-regulated kinases and calcium channels are involved in the proliferative effect of bisphosphonates on osteoblastic cells in vitro. J Bone Miner Res 16:2050–2056
Viereck V, Emons G, Lauck V et al (2002) Bisphosphonates pamidronate and zoledronic acid stimulate osteoprotegerin production by primary human osteoblasts. Biochem Biophys Res Commun 291:680–686
Im G, Qureshi SA, Kenney J, Rubash HE, Shanbhag AS (2004) Osteoblast proliferation and maturation by bisphosphonates. Biomaterials 25:4105–4115
Mackie EJ (2003) Osteoblasts: novel roles in orchestration of skeletal architecture. Int J Biochem Cell Biol 35:1301–1305
Kim HH, Lee DE, Shin JN et al (1999) Receptor activator of NF-kB recruits multiple TRAF family adaptors and activates c-Jun N-terminal kinase. FEBS Lett 443:297–302
Matsumoto M, Sudo T, Saito T, Osada H, Tsujimoto M (2000) Involvement of p38 mitogen-activated protein kinase signaling pathway in osteoclastogenesis mediated by receptor activator of NF-kB ligand (RANKL). J Biol Chem 275:31155–31161
Kobayashi N, Kadono Y, Naito A et al (2001) Segregation of TRAF6-mediated signaling pathways clarifies its role in osteoclastogenesis. EMBO J 20:1271–1280
Simonet WS, Lacey DL, Dunstan CR et al (1997) Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell 89:309–319
Hofbauer LC, Lacey DL, Dunstan CR, Spelsberg TC, Riggs BL, Khosla S (1999) Interleukin-1beta and tumor necrosis factor-alpha, but not interleukin-6, stimulate osteoprotegerin ligand gene expression in human osteoblastic cells. Bone 25:255–259
Abu-Amer Y, Erdmann J, Kollias G, Alexopoulou L, Ross FP, Teitelbaum SL (2000) Tumor necrosis factor receptors types 1 and 2 differentially regulate osteoclastogenesis. J Biol Chem 275:27307–27310
Lam J, Takeshita S, Barker JE, Kanagawa O, Ross FP, Teitelbaum SL (2000) TNF-α induces osteoclastogenesis by direct stimulation of macrophages exposed to permissive levels of RANK ligand. J Clin Invest 106:1481–1488
Kaji K, Katogi R, Azuma Y, Naito A, Inoue JI, Kudo A (2001) Tumor necrosis factor alpha-induced osteoclastogenesis requires tumor necrosis factor receptor-associated factor 6. J Bone Miner Res 16:1593–1599
Zou W, Hakim I, Tschoep K, Endres S, Bar-Shavit X (2001) Tumor necrosis factor-a mediates RANK ligand stimulation of osteoclast differentiation by an autocrine mechanism. J Cell Biochem 83:70–83
Nakao A, Fukushima H, Kajiya H, Ozeki S, Okabe K (2007) RANKL-stimulated TNFa production in osteoclast precursor cells promotes osteoclastogenesis by modulating RANK signaling pathways. Biochem Biophys Res Commun 357:945–950
Wei S, Kitaura H, Zhou P, Ross FP, Teitelbaum SL (2005) IL-1 mediates TNF-induced osteoclastogenesis. J Clin Invest 115:282–290
Yoshida H, Hayashi S, Kunisada T et al (1990) The murine mutation osteopetrosis is in the coding region of the macrophage colony stimulating factor gene. Nature 345:442–444
Boyle WJ, Simonet WS, Lacey DL (2003) Osteoclast differentiation and activation. Nature 423:337–342
Faccio R, Takeshita S, Zallone A, Ross FP, Teitelbaum SL (2003) c-Fms and the αvβ3 integrin collaborate during osteoclast differentiation. J Clin Invest 111:749–758
Hofbauer LC, Khosla S, Dunstan CR, Lacey DL, Spelsberg TC, Riggs BL (1999) Estrogen stimulates gene expression and protein production of osteoprotegerin in human osteoblastic cells. Endocrinology 140:4367–4370
Troen BR (2003) Molecular mechanisms underlying osteoclast formation and activation. Exp Gerontol 38:605–614
Zaidi M, Blair HC, Moonga BS, Abe E, Huang CL (2003) Osteoclastogenesis, bone resorption, and osteoclast-based therapeutics. J Bone Miner Res 18:599–609
Lajeunesse D, Busque L, Menard P, Brunette MG, Bonny Y (1996) Demonstration of an osteoblast defect in two cases of human malignant osteopetrosis. Correction of the phenotype after bone marrow transplant. J Clin Invest 98:1835–1842
Glorieux FH, Rauch F, Plotkin H et al (2000) Type v osteogenesis imperfecta: a new form of brittle bone disease. J Bone Miner Res 15:1650–1658
Glorieux FH, Ward LM, Rauch F, Lalic L, Roughley PJ, Travers R (2002) Osteogenesis imperfecta type vi: a form of brittle bone disease with a mineralization defect. J Bone Miner Res 17:30–38
Labuda M, Morissette J, Ward LM et al (2002) Osteogenesis imperfecta type vii maps to the short arm of chromosome 3. Bone 31:19–25
Ward LM, Rauch F, Travers R et al (2002) Osteogenesis imperfecta type vii: an autosomal recessive form of brittle bone disease. Bone 31:12–18
Bender IB (2003) Paget's disease. J Endod 29:720–723
Siris ES, Roodman GD (2003) Paget’s disease. In: Favus MJ (ed) Primer on the metabolic bone diseases and disorders of mineral metabolism. American Society for Bone and Mineral Research, Chicago, pp 495–508
Menaa C, Reddy SV, Kurihara N et al (2000) Enhanced rank ligand expression and responsivity of bone marrow cells in Paget's disease of bone. J Clin Invest 105:1833–1888
Neale SD, Smith R, Wass JA, Athanasou NA (2000) Osteoclast differentiation from circulating mononuclear precursors in Paget's disease is hypersensitive to 1,25-dihydroxyvitamin d(3) and RANKL. Bone 27:409–416
Buckley KA, Fraser WD (2002) Receptor activator for nuclear factor kappaB ligand and osteoprotegerin: regulators of bone physiology and immune responses/potential therapeutic agents and biochemical markers. Ann Clin Biochem 39:551–556
Sahni M, Guenther HL, Fleisch H, Collin P, Martin TJ (1993) Bisphosphonates act on rat bone resorption through the mediation of osteoblasts. J Clin Invest 91:2004–2011
Nishikawa M, Akatsu T, Katayama Y, Yasutomo Y, Kado S, Kugal N, Yamamoto M, Nagata N (1996) Bisphosphonates act on osteoblastic cells and inhibit osteoclast formation in mouse marrow cultures. Bone 18:9–14
Russell RG, Rogers MJ, Frith JC, Luckman SP, Coxon FP, Benford HL, Croucher PI, Shipman C, Fleisch HA (1999) The pharmacology of bisphosphonates and new insights into their mechanisms of action. J Bone Miner Res 2:53–65
Viereck V, Emons G, Lauck V, Frosch KH, Blaschke S, Grundker C, Hofbauer LC (2002) Bisphosphonates pamidronate and zoledronic acid stimulate osteoprotegerin production by primary human osteoblasts. Biochem Biophys Res Commun 291:680–686
Pan B, Farrugia AN, To LB, FindlayDM GJ, Lynch K, Zannettino AC (2004) The nitrogen containing bisphosphonate, zoledronic acid, influences RANKL expression in human osteoblast-like cells by activating TNF-alpha converting enzyme (TACE). J Bone Miner Res 19:147–154
Kim HK, Kim JH, Abbas AA, Yoon TR (2009) Alendronate enhances osteogenic differentiation of bone marrow stromal cells: a preliminary study. Clin Orthop Relat Res 467:3121–3128
Xiong Y, Yang HJ, Feng J, Shi ZL, Wu LD (2009) Effects of alendronate on the proliferation and osteogenic differentiation of MG-63 cells. J Int Med Res 37:407–416
Pan B, To LB, Farrugia AN, Findlay DM, Green J, Gronthos S, Evdokiou A, Lynch K, Atkins GJ, Zannettino AC (2004) The nitrogen-containing bisphosphonate, zoledronic acid, increases mineralisation of human bone-derived cells in vitro. Bone 34:112–123
Idris AI, Rojas J, Greig IR, van't Hof RJ, Ralston SH (2008) Aminobisphosphonates cause osteoblast apoptosis and inhibit bone nodule formation in vitro. Calcif Tissue Int 82:191–201
Orriss IR, Key ML, Colston KW, Arnett TR (2009) Inhibition of osteoblast function in vitro by aminobisphosphonates. J Cell Biochem 106:109–118
Pozzi S, Vallet S, Mukherjee S, Cirstea D, Vaghela N, Santo L, Rosen E, Ikeda H, Okawa Y, Kiziltepe T, Schoonmaker J, Xie W, Hideshima T, Weller E, Bouxsein ML, Munshi NC, Anderson KC, Raje N (2009) High-dose zoledronic acid impacts bone remodeling with effects on osteoblastic lineage and bone mechanical properties. Clin Cancer Res 15:5829–5839
Greiner S, Kadow-Romacker A, Lubberstedt M, Schmidmaier G, Wildemann B (2007) The effect of zoledronic acid incorporated in a poly(D, L-lactide) implant coating on osteoblasts in vitro. J Biomed Mater Res A 80:769–775
Kellinsalmi M, Monkkonen H, Monkkonen J, Leskela HV, Parikka V, Hamalainen M, Lehenkari P (2005) In vitro comparison of clodronate, pamidronate and zoledronic acid effects on rat osteoclasts and human stem cell-derived osteoblasts. Basic Clin Pharmacol Toxicol 97:382–391
Evans CE (2002) Bisphosphonates modulate the effect of macrophage-like cells on osteoblast. Int J Biochem Cell Biol 34:554–563
Rehinolz GG, Getz B, Pederson L et al (2000) Bisphosphonates directly regulate cell proliferation, differentiation and gene expression in human osteoblasts. Cancer Res 60:6001–6007
Giuliani N, Pedrazzoni M, Passeri G, Girasole G (1998) Bisphosphonates inhibit IL-6 production by human osteoblast-like cells. Scand J Rheumatol 27:38–41
Itoh F, Aoyagi S, Furihata-Komatsu H, Aoki M, Kusama H, Kojima M, Kogo H (2003) Clodronate stimulates osteoblast differentiation in ST2 and MC3T3-E1 cells and rat organ cultures. Eur J Pharmacol 477:9–16
D’Aoust P, McCulloch CA, Tenenbaum HC, Lekic PC (2000) Etidronate (HEBP) promotes osteoblast differentiation and wound closure in rat calvaria. Cell Tissue Res 302:353–363
Corrado A, Cantatore FP, Grano M, Colucci S (2005) Neridronate and human osteoblasts in normal, osteoporotic and osteoarthritic subjects. Clin Rheumatol 24:527–534
Corrado A, Neve A, Maruotti N, Gaudio A, Marucci A, Cantatore FP (2010) Dose-dependent metabolic effect of zoledronate on primary human osteoblastic cell cultures. Clin Exp Rheumatol 28:873–879
Plotkin LI, Weinstein RS, Parfitt AM, Roberson PK, Manolagas SC, Bellido T (1999) Prevention of osteocyte and osteoblast apoptosis by bisphosphonates and calcitonin. J Clin Invest 104:1363–1374
Abe Y, Kawakami A, Nakashima T et al (2000) Etidronate inhibits human osteoblast apoptosis by inhibition of pro-apoptotic factor(s) produced by activated T cells. J Lab Clin Med 136:344–354
Plotkin LI, Lezcano V, Thostenson J, Weinstein RS, Manolagas SC, Bellido T (2008) Connexin 43 is required for the anti-apoptotic effect of bisphosphonates on osteocytes and osteoblasts in vivo. J Bone Miner Res 23:1712–1721
Plotkin LI, Manolagas SC, Bellido T (2002) Transduction of cell survival signals by connexin-43 hemichannels. J Biol Chem 277:8648–8657
Kogianni G, Mann V, Ebetino F, Nuttall M, Nijweide P, Simpson H, Noble B (2004) Fas/CD95 is associated with glucocorticoid-induced osteocyte apoptosis. Life Sci 75:2879–2895
Abe Y, Kawakami A, Nakashima T, Ejima E, Fujiyama K, Kiriyama T, Ide A, Sera N, Usa T, Tominaga T, Ashizawa K, Yokoyama N, Eguchi K (2000) Etidronate inhibits human osteoblast apoptosis by inhibition of pro-apoptotic factor(s) produced by activated T cells. J Lab Clin Med 136:344–354
Gangoiti MV, Cortizo AM, Arnol V, Felice JI, McCarthy AD (2008) Opposing effects of bisphosphonates and advanced glycation end-products on osteoblastic cells. Eur J Pharmacol 600:140–147
Bivi N, Bereszczak JZ, Romanello M, Zeef LA, Delneri D, Quadrifoglio F, Moro L, Brancia FL, Tell G (2009) Transcriptome and proteome analysis of osteocytes treated with nitrogen-containing bisphosphonates. J Proteome Res 8:1131–1142
Bellido T, Plotkin LI (2011) Novel actions of bisphosphonates in bone: preservation of osteoblast and osteocyte viability. Bone 49:50–55
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maruotti, N., Corrado, A., Neve, A. et al. Bisphosphonates: effects on osteoblast. Eur J Clin Pharmacol 68, 1013–1018 (2012). https://doi.org/10.1007/s00228-012-1216-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-012-1216-7