Abstract
Oral anticoagulants (OA) are a leading cause of fatal haemorrhagic adverse events in relation with an important interindividual variability of response to these drugs. Besides several clinical factors, this interindividual variability of response to OA has a pharmacogenetic basis. Carriers of cytochrome P450 2C9 (CYP2C9)-deficient alleles have a reduced clearance of warfarin and are exposed to dramatic overdoses in the first weeks of treatment. Genetic polymorphisms of vitamin K epoxide reductase (VKORC1), the target of OA, identify patients with a high sensitivity to OA who are at risk of early overdose. Most pharmacogenetic evidence is presently restricted to warfarin. Several warfarin dosing algorithms have been constructed, adapted on CYP2C9 and VKORC1 genotypes and clinical factors, to predict the best dose for each patient. Carriers of one of allelic variant need a 20–30% reduction of warfarin dose. However, definite evidence concerning the usefulness of these algorithms in terms of reducing the frequency of major bleeding episodes is still lacking. Ongoing prospective randomised trials will ascertain definitive answer over the coming years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral anticoagulants (OA) have proven to be highly effective antithrombotic drugs for the treatment or prevention of deep venous thrombosis, pulmonary embolism, stroke and myocardial infarction for more than 50 years. Besides these well-demonstrated clinical benefits, OA are associated with a high risk of major bleeding, which unfortunately limits their use, particularly in the elderly [1]. In France, OA are associated with 17,000 hospitalisations for major bleeding annually. In the United States, more than 20 million patients are treated with OAs and 29,000 visits for bleeding complications are observed each year. Warfarin (WA) represents the first cause of lethal adverse drug reaction in the United States [2]. Several risk factors of bleeding have been identified, such as age, female gender, drug interactions, and previous bleeding [2]. Besides these classical risk factors, pharmacogenetic risk factors have been identified in the past decade and were introduced in the summarised product characteristics of WA by the US Food and Drug Administration (FDA) in 2007, indicating that lower initiation doses should be considered for patients carrying allelic variants of CYP2C9 and vitamin K epoxide reductase (VKORC1) [3]. Additional genetic variants of other genes have been identified (CYP4F2, GGCX, APOE, PROC and clotting factors [4–7]), but they play a minor role in OA pharmacodynamics and are out of the scope of this review considering practical applications of pharmacogenetics tests.
Different oral anticoagulant drugs
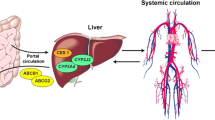
WA is available all over the world and represents the most prescribed OA in North America, Asia, and England, whereas acenocoumarol (AC), phenprocoumon, and fluindione are more commonly used in several European countries [8, 9]. WA, AC and phenprocoumon are administered as racemate, and their S-enantiomers retain the highest anticoagulant activity. There are some significant differences in the pharmacokinetic profile of the different OA [10], which can be classified as short- or long-acting drugs based on their terminal half-life (Table 1). They all act by decreasing vitamin-K-dependant clotting factors (II, VII, IX and X) via the inhibition of vitamin K epoxide reductase (VKOR), which recycles reduced vitamin K (inactive) into active oxidised vitamin K (Fig. 1). All OA have a similar tolerance profile, except for fluindione, an indanedione derivative, which is associated to more frequent immunoallergic adverse drug reaction such as hepatitis and nephritis [11].
CYP2C9 and oral anticoagulants metabolism
Cytochrome P4502C9 (CYP2C9) represents quantitatively the second CYP isoform expressed in the liver [12] and is involved in the metabolic clearance of different drugs such as oral hypoglycemic agents, nonsteroidal anti-inflammatory drugs, angiotensin II blockers, anticonvulsivants and antidepressant drugs [13]. Its role in the metabolism of WA was highlighted at the end of last century [14–16].
In vitro data concerning CYP2C9-dependant metabolism of oral anticoagulants
CYP2C9 metabolises S-warfarin, the the most active enantiomer, whereas CYP3A4, CYP2C19 and CYP1A2 are involved in R-warfarin metabolism [17–19]. Concerning acenocoumarol, CYP2C9 seems to be the most potent isoform involved in the metabolism of both enantiomers [20, 21]. Acenocoumarol CYP2C9-dependant intrinsic clearance is far higher compared with WA, which explains its shorter half-life in humans. The role of CYP2C9 in phenprocoumon metabolic clearance seems to be less pronounced compared with the two previous OA, with a similar involvement of CYP3A4 and CYP2C9 [10, 22]. Furtheremore, phenprocoumon is also extensively conjugated, implicating phase-2 enzymes in its metabolic clearance. No data are available for the metabolism of fluindione, exept that it is mainly cleared as hydroxylated and conjugated metabolites that have never been identified.
Two main functional CYP2C9-deficient allelic variants were identified in the early 1990s: CYP2C9*2 (Arg 144 into Cys) and CYP2C9*3 (Ile 359 to Leu) [23]. Both polymorphisms were rapidly shown to be associated with decreased S-warfarin hepatic clearance and, as a consequence, to need lower steady-state daily doses to achieve a usual therapeutic target [International Normalised Ratio (INR) 2–3] [14, 16, 24]. The influence of CYP2C9 genetic polymorphism has also been observed for AC [25] and phenprocoumon, whereas no data are available for fluindione. Compared with WA, the influence of the CYP2C9-deficient allele CYP2C9*2 seems absent [26, 27] or less important for acenoucoumarol [10]. Furthermore, the contribution of CYP2C9-dependant clearance to the overall oral clearance of phenprocoumon seems to be lower than that observed with WA [10, 28]. The importance of CYP2C9 genetic polymorphism is probably higher among patients of Caucasian origin, in whom the frequencies of the CYP2C9-deficient alleles is almost the double compared with other ethnic groups. Indeed, the allelic frequencies of CYP2C9*2 and CYP2C9*3 are 0.1 and 0.08, 0.04 and 0.02 and 0.01 and 0.04 among subjects of Caucasian, African and Asiatic origins [29–31]. The CYP2C9-dependant pharmacogenetic effect observed for OA has three major clinical consequences, which are described below.
CYP2C9 and daily dose requirements
In 1999, Aithal et al. described for the first time that patients carrying the CYP2C9*2 and/or CYP2C9*3 allele needed much lower doses of WA at steady state [24] compared with noncarriers. These results were further confirmed by many different independent groups [32, 33]. A similar relationship between CYP2C9 genetic polymorphism and AC daily dose requirement was observed [26, 34, 35]. Concerning phenprocoumon, slightly lower dose requirements were described for carriers of CYP2C9-deficient alleles [36, 37], but this was not observed by all authors [38], probably in relation with the lower impact of CYP2C9-dependant metabolism of phenprocoumon compared with WA and acenocoumarol.
CYP2C9 and time to reach stable anticoagulation
Aithal et al. were the first to detect that patients treated with WA and carrying one CYP2C9-deficient allele had more difficulties reaching stable anticoagulation [24]. This observation was also confirmed by other groups [33] and with the other related OA, AC [34, 39] and phenprocoumon [36].
CYP2C9 and risk of bleeding
As a consequence of this difficulty finding the right dose and to achieve stable anticoagulation, it has been shown that carriers of CYP2C9 allelic variants have a 3.68 increased risk of major bleeding with WA [24]. The CYP2C9-dependant pharmacogenetic risk of bleeding is maximal during the initiation phase of the anticoagulant treatment. Increased risk of major haemorrhage with WA conferred by CYP2C9 allelic variants has been estimated to be 5.3 before stabilisation of therapy and 2.2 after stabilisation [32, 33]. A similar increased number of overanticoagulation episodes (INR > 6) and bleeding events has been described for carriers of CYP2C9 variants treated with AC [39, 40]. More conflicting data exist concerning the CYP2C9-dependant risk of bleeding with phenprocoumon [36, 40, 41], which is probably smaller than that observed with WA and AC due to a smaller involvement of CYP2C9 in phenprocoumon oral clearance [28].
VKORC, the target of oral anticoagulants
The gene that encodes VKOR (VKORC1), the target enzyme for OA (Fig. 1), was identified in 2004 [42, 43]. Rost et al. identified the VKORC1 gene from four independent families whose members were considered resistant to WA. One patient needed more than 17 mg/day of WA to achieve adequate anticoagulation, two others about 40 mg/d and the fourth did not respond to any dose of WA. They carried rare mutations of VKORC1 of amino acids 29 (Val/Leu), 45 (Val/Ala), 58 (Arg/Gly) and 128 (Leu/Arg) [42]. Several months later, other groups described that common VKORC1 single nucleotide polymorphisms (SNPs) were strongly associated with OA sensitivity [44–48]. VKORC1 genetic polymorphism has the same influence for all OA [37, 45, 49].
Several SNPs in complete linkage disequilibrium identify a haplotype combination called A [32, 48], which is associated with OA hypersensitivity. Two of these SNPs (−1639G>A, rs9934438 or 1173C>T, rs17878363) are usually used to identify (tag) this VKORC1 A haplotype group, which is associated with lower levels of hepatic VKORC expression [48]. Therefore, patients carrying the VKORC1 A haplotype have lower levels of hepatic VKOR and as a consequence are more sensible to OA. The allelic frequency of this VKORC1 A haplotype is rather low among subjects from African origin (0.15), high in Caucasians (0.42) and extremely frequent among Asians [32, 45, 47, 50]. As observed for CYP2C9, VKORC1 genetic polymorphism has three major clinical consequences on the pharmacodynamics of OA, which are described below.
VKORC1 and daily dose requirements
Since VKORC1 genetic polymorphism modulates WA sensitivity, it also influences the dose of WA at steady state to reach stable anticoagulation [48, 51]. Swartz et al. observed a clear gene–dose effect with VKORC1 A associated with a higher INR response, requiring lower doses of WA [51]. From a large cohort of patients treated with WA, it has been estimated that the dose should be reduced by 28% for each VKORC1 A allele [52]. Similar findings have been obtained for other OA, such as AC [53, 54] and phenprocoumon [37, 53]. VKORC1 genetic polymorphism also mainly explains why steady-state doses of OA differ between patients of different ethnic origins: VKORC1 A (linked to OA sensitivity) is rare among blacks, who need higher doses of OA; the same A haplotype is present in 90% of patients of Asian origin, who need the smallest doses to achieve stable anticoagulation.
VKORC1 and time to reach stable anticoagulation
WA-treated patients homozygous for the VKORC1 A/A haplotype (sensitive to OA) achieve their first INR in the target range 2.4 sooner compared with others and reach an INR above 4, 2.5 sooner [51]. They also spend twice as much time above the INR upper limit of 4 compared with other patients [51] and are thus more difficult to equilibrate.
VKORC1 and risk of bleeding
As a consequence of this difficulty to obtain of stable INR and a stable dose, VKORC1 genetic polymorphism has been rapidly recognised as an important risk for bleeding in patients treated with OA. This higher frequency of WA overdose among VKORC1 A/A patients was mainly observed during the first month following the introduction of the OA [51]. A similar increased risk of bleeding linked to VKORC1 genetic polymorphism has been observed with phenprocoumon [37, 53] and AC [54, 55].
Pharmacogenetic-based dosing algorithms
Different algorithms have been developed to determine the right dose for the right patient [56]. The first algorithms, which were employed for a long time, were based on clinical variables such as INR target, patient age, history of previous bleeding, reason for prescription (atrial fibrillation or venous thrombosis), associated diseases and concomitant drugs prescribed. As it has been estimated that CYP2C9 and VKORC1 genetic polymorphisms explain 35–50% of the interindividual variability of OA response during the initiation phase of the treatment, dosing algorithms rapidly integrated genotype information. One of the first of these pharmacogenetic-based dosing normograms including VKORC1 and CYP2C9 genotypes was proposed by Sconce et al. [57], which allowed in a replication cohort to explain about 80% of the interindividual variability of the WA dose needed to achieve an INR between 2 and 3. Different other pharmacogenetic-based normograms have been developed [58] for Caucasian and non-Caucasian ethnic groups [59]. At the time, one of the best validated dosing algorithm was proposed by Gage et al. [52] and includes not only CYPC2C9 and VKORC1 genetic data but also numerous clinically relevant items such as associated drugs, smoking status and ethnic origin. It explains 53–54% of the variability in the WA dose and was prospectively validated in a replication cohort. It was obtained from one of the largest collaborative cohorts (1,015 patients) and was made available online at www.warfarindosing.org. Tables 2 and 3 compare the dose of WA that should be introduced in a 70-year-old white nonsmoking man without concomitant drugs (statins or amiodarone) of 75 kg and 1.70 m tall based on two different dosing normograms. Both algorithms predict relatively similar doses. However, Gage et al.’s algorithm allows the dose to be adapted to much more relevant clinical factors. Pharmacogenetic-based algorithms for OA other than WA are missing at this time.
Pharmacogenetic prospective randomised clinical trials
Unfortunately, only three. small-scale prospective randomised trials were performed to determine whether an initial pharmacogenetic-adapted dose could improve the time to reach stable anticoagulation and the frequency of bleeding episodes during initiation of OA therapy [60–62]. The first study, which included only 38 patients, was just a pilot trial testing the feasibility of CYP2C9 genotyping before introducing WA; no differences could be observed between the CYP2C9-adapted and nonadapted patients [62]. The second study was aimed to decrease by 50% the time spent out of the INR range during the initiation of WA treatment [60]. The authors used a WA loading dose during the first 2 days of treatment and randomised the patients in two arms: one according to a standard clinical titration (99) and the other based on a CYP2C9- and VKORC1- adapted algorithm (101). The authors could not confirm their primary hypothesis in relation to a lower frequency of the clinical event compared with what was expected in the control group and a too ambitious planned difference between both groups (underpowered study for the main outcome). However, they could detect that patients in the pharmacogenetic-guided arm needed less INR controls and had less dose modifications. No differences could be observed concerning the bleeding events. The last trial was planned to reduce the time to reach the first therapeutic INR range and the time to reach stable anticoagulation [61]. Patients were randomised in two arms: one with a standardised dose of WA (142), and the other (141) with a pharmacogenetic-adapted dose of WA, which included only CYPC9 genotype in its normogram. Both study endpoints were reached sooner (2.23 days and 18.1 days, respectively) in the pharmacogenetic-adapted arm. Furthermore, in the pharmacogenetic-adapted arm, patients spent more time within the INR therapeutic range (80.4% vs 63.4%) and experienced less minor bleeding (3.2% vs 12.5%).
One might be surprised by the low number of randomised trials in this field despite strong scientific evidence indicating that CYP2C9 and VKORC1 explain about 50% of the interindividual variability of WA response. Unfortunately, this is a common problem in the field of pharmacogenetics, which lacks randomised trials. One reason is the recent discovery in 2005 of the influence of VKORC1 polymorphisms on OA response. Several randomised trials, some including a larger number of patients, are ongoing and are available at www.clinicaltrials.gov. The results of these trials will be available in the coming years and will hopefully definitively demonstrate the usefulness of a pharmacogenetically adapted dose of WA. The next explanation for so few randomised trials in the field is that the ultimate objective of such a study is to reduce the frequency of major bleeding episodes (the most clinically relevant endpoint), which occur in clinical trials in 1% of the study population per year [63]. Such an event frequency implicates inclusion of at least 1,000 patients. Another difficulty in performing such randomised trials is the need for rapid pharmacogenetic tests, the results of which must be sent to the physician within a few hours. Such rapid genotyping is for the moment restricted to several university hospitals, but this situation should change rapidly with the development of validated diagnostic kits, some of which have been approved by the FDA.
Future prospective randomised trials will also bring extremely important information concerning the frequency of recurrent thrombotic events. All pharmacogenetic efforts have focused on reducing OA overdose and the risk of bleeding. But difficulties attaining stable anticoagulation also includes INR episodes below 2 and possibly increased frequency of thrombotic recurrence. Furthermore, a pharmacogenetically adapted dose might limit the bleeding episodes but at the same time increase the early recurrence of thrombotic events, which might totally blunt the benefit of the pharmacogenetically adapted dosing. Therefore, attention must be paid to precisely evaluate the real risk/benefit ratio of a pharmacogenetically adapted dosing.
No randomised trials have been performed with OA other than WA. A prospective randomised trial is planned in Europe to compare the utility of a pharmacogenetic-based prescribing between WA, AC and phenprocoumon.
Conclusion
A large number of studies have demonstrated that the genetic polymorphisms of CYP2C9 and VKORC1 significantly influence OA pharmacokinetics and pharmacodynamics. However, most of the evidence is restricted to WA, and even for this drug, a definite demonstration of the utility of systematic genotyping to adapt its dose is still lacking. The benefit of such pharmacogenetic testing remains to be validated in terms of costs with a pharmacoeconomic approach.
The definitive answer concerning the usefulness of the pharmacogenetically based WA dosing will be available in the coming years. This process will probably take some time for the OA used in Europe. Meanwhile, physicians can benefit from the www.warfarindosing.org normogram, which has the advantage of including the first INR values and a delayed genotype.
References
Shireman T, Mahnken J, Howard P, Kresowik T, Hou Q, Ellerbeck E (2006) Development of a contemporary bleeding risk model for elderly warfarin recipients. Chest 130:1390–1396
Wysowski D, Nourjah P, Swartz L (2007) Bleeding complications with warfarin use. Arch Intern Med 167:1414–1419
FDA. New Labeling Information for Warfarin (marketed as Coumadin). http://www.fda.gov/cder/drug/infopage/warfarin/default.htm 2007
Caldwell M, Awad T, Johnson J, Gage B, Falkowski M, Gardina P, Hubbard J, Turpaz Y, Langaee T, Eby C, King C, Brower A, Schmelzer J, Glurich I, Vidaillet H, Yale S, Qi Zhang K, Berg R, Burmester J (2008) CYP4F2 genetic variant alters required warfarin dose. Blood 111:4106–1412
Cooper G, Johnson J, Langaee T, Feng H, Stanaway I, Schwarz U, Ritchie M, Stein C, Roden D, Smith J, Veenstra D, Rettie A, Rieder M (2008) A genome-wide scan for common genetic variants with a large influence on warfarin maintenance dose. Blood Jun 5 [Epub ahead of print]
Wadelius M, Chen L, Eriksson N, Bumpstead S, Ghori J, Wadelius C, Bentley D, McGinnis R, Deloukas P (2007) Association of warfarin dose with genes involved in its action and metabolism. Hum Genet 121:23–24
Wadelius M, Chen L, Lindh J, Eriksson N, Ghori M, Bumpstead S, Holm L, McGinnis R, Rane A, Deloukas P (2008) The largest prospective warfarin-treated cohort supports genetic forecasting. Blood Jun 23 [Epub ahead of print]
Ansell J, Hollowell J, Pengo V, Martinez-Brotons F, Caro J, Drouet L (2007) Descriptive analysis of the process and quality of oral anticoagulation management in real-life practice in patients with chronic non-valvular atrial fibrillation: the international study of anticoagulation management (ISAM). J Thromb Thrombolysis 23:83–91
Pengo V, Pegoraro C, Cucchini U, Iliceto S (2006) Worldwide management of oral anticoagulant therapy: the ISAM study. J Thromb Thrombolysis 21:73–77
Ufer M (2005) Comparative pharmacokinetics of vitamin K antagonists: warfarin, phenprocoumon and acenocoumarol. Clin Pharmacokinet 44:1227–1246
Sparsa A, Bédane C, Benazahary H, De Vencay P, Gauthier M, Le Brun V, Boulinguez S, Loustaud-Ratti V, Soria P, Vidal E, Bonnetblanc J (2001) Drug hypersensitive syndrome caused by fluindione. Ann Dermatol Venereol 128:1014–1018
Shimada T, Yamazaki H, Mimura M, Inui Y, Guengerich FP (1994) Interindividual variations in human liver cytochrome P-450 enzymes involved in the oxydation of drugs, carcinogens and toxic chemicals: studies with liver microsomes of 30 Japanese and 30 Caucasians. J Pharmacol Exp Ther 270:414–423
Flockhart D. Cytochrome P450 drug interaction table, http://medicine.iupui.edu/flockhart/table.htm
Furuya H, Fernandez-Salguero P, Gregory W, Taber H, Steward A, Gonzalez FJ, Idle JR (1995) Genetic polymorphism of CYP2C9 and its effect on warfarin maintenance dose requirement in patients undergoing anticoagulation therapy. Pharmacogenetics 5:389–392
Rettie AE, Wienkers LC, Gonzalez FJ, Trager WF, Korzekwa KR (1994) Impaired (S)-warfarin metabolism catalysed by the R144C allelic variant of CYP2C9. Pharmacogenetics 4:39–42
Steward DJ, Haining RL, Henne KR, Davis G, Rushmore TH, Trager WF, Rettie AE (1997) Genetic association between sensitivity to warfarin and expression of CYP2C9*3. Pharmacogenetics 7:361–367
Rettie A, Korzekwa K, Kunze K, Lawrence R, Eddy A, Aoyama T, Gelboin H, Gonzalez F, Trager W (1992) Hydroxylation of warfarin by human cDNA-expressed cytochrome P-450: a role for P-4502C9 in the etiology of (S)-warfarin-drug interactions. Chem Res Toxicol 5:54–59
Zhang Z, Fasco M, Huang Z, Guengerich F, Kaminsky L (1995) Human cytochromes P4501A1 and P4501A2: R-warfarin metabolism as a probe. Drug Metab Dispos 23:1339–1346
Zhou Q, Zhou S, Chan E (2005) Effect of omeprazole on the hydroxylation of warfarin enantiomers in human: in-vitro studies with liver microsomes and cDNA-expressed cytochrome P450 isozymes. Curr Drug Metab 6:399–411
Hermans JJ, Thijssen HH (1993) Human liver microsomal metabolism of the enantiomers of warfarin and acenocoumarol: P450 isozyme diversity determines the differences in their pharmacokinetics. Br J Pharmacol 110:482–490
Thijssen HH, Flinois JP, Beaune PH (2000) Cytochrome P4502C9 is the principal catalyst of racemic acenocoumarol hydroxylation reactions in human liver microsomes. Drug Metab Dispos 28:1284–1290
Ufer M, Svensson J, Krausz K, Gelboin H, Rane A, Tybring G (2004) identification of cytochromes P450 2C9 and 3A4 as the major catalysts of phenprocoumon hydroxylation in vitro. Eur J Clin Pharmacol 60:173–182
Ingelman-Sundberg M, Daly A, Nebert D. Home Page of the Human Cytochrome P450 (CYP) Allele Nomenclature Committee http://www.imm.ki.se/CYPalleles/
Aithal GP, Day CP, Kesteven PJ, Daly AK (1999) Association of polymorphisms in the cytochrome P450 CYP2C9 with warfarin dose requirement and risk of bleeding complications. Lancet 353:717–719
Thijssen HH, Ritzen B (2003) Acenocoumarol pharmacokinetics in relation to cytochrome P450 2C9 genotype. Clin Pharmacol Ther 74:61–68
Hermida J, Zarza J, Alberca I, Montes R, Lopez ML, Molina E, Rocha E (2002) Differential effects of 2C9*3 and 2C9*2 variants of cytochrome P-450 CYP2C9 on sensitivity to acenocoumarol. Blood 99:4237–4239
Morin S, Bodin L, Loriot MA, Thijssen HH, Robert A, Strabach S, Verstuyft C, Tregouet DA, Dubert L, Laurent-Puig P, Funck-Brentano C, Jaillon P, Beaune PH, Becquemont L (2004) Pharmacogenetics of acenocoumarol pharmacodynamics. Clin Pharmacol Ther 75:403–414
Kirchheiner J, Ufer M, Walter EC, Kammerer B, Kahlich R, Meisel C, Schwab M, Gleiter CH, Rane A, Roots I, Brockmoller J (2004) Effects of CYP2C9 polymorphisms on the pharmacokinetics of R- and S-phenprocoumon in healthy volunteers. Pharmacogenetics 14:19–26
London SJ, Daly AK, Leathart JB, Navidi WC, Idle JR (1996) Lung cancer risk in relation to the CYP2C9*1/CYP2C9*2 genetic polymorphism among African-Americans and Caucasians in Los Angeles County, California. Pharmacogenetics 6:527–533
Scordo M, Aklillu E, Yasar U, Dahl M, Spina E, Ingelman-Sundberg M (2001) genetic polymorphism of cytochrome P450 2C9 in a Caucasian and black African population. Br J Clin Pharmacol 52:447–450
Yang JQ, Morin S, Verstuyft C, Fan LA, Zhang Y, Xu CD, Barbu V, Jaillon P, Becquemont L (2003) Frequency of cytochrome P450 2C9 allelic variants in the Chinese and French populations. Fundam Clin Pharmacol 17:373–376
Limdi N, McGwin G, Goldstein J, Beasley T, Arnett D, Adler B, Baird M, Acton R (2008) Influence of CYP2C9 and VKORC1 1173C/T Genotype on the Risk of Hemorrhagic Complications in African-American and European-American Patients on Warfarin. Clin Pharmacol Ther 83:312–321
Higashi MK, Veenstra DL, Kondo LM, Wittkowsky AK, Srinouanprachanh SL, Farin FM, Rettie AE (2002) Association between CYP2C9 genetic variants and anticoagulation-related outcomes during warfarin therapy. JAMA 287:1690–1698
Tassies D, Freire C, Pijoan J, Maragall S, Monteagudo J, Ordinas A, Reverter JC (2002) Pharmacogenetics of acenocoumarol: cytochrome P450 CYP2C9 polymorphisms influence dose requirements and stability of anticoagulation. Haematologica 87:1185–1191
Thijssen H, Verkooijen I, Frank H (2000) The possession of the CYP2C9*3 allele is associated with low dose requirement of acenocoumarol. Pharmacogenetics 10:757–760
Schalekamp T, Oosterhof M, van Meegen E, van Der Meer FJ, Conemans J, Hermans M, Meijerman I, de Boer A (2004) Effects of cytochrome P450 2C9 polymorphisms on phenprocoumon anticoagulation status. Clin Pharmacol Ther 76:409–417
Schalekamp T, Brasse BP, Roijers JF, van Meegen E, van der Meer FJ, van Wijk EM, Egberts AC, de Boer A (2007) VKORC1 and CYP2C9 genotypes and phenprocoumon anticoagulation status: interaction between both genotypes affects dose requirement. Clin Pharmacol Ther 81:185–193
Visser L, van Vliet M, van Schaik R, Kasbergen A, De Smet P, Vulto A, Hofman A, van Duijn C, Stricker B (2004) The risk of overanticoagulation in patients with cytochrome P450 CYP2C9*2 or CYP2C9*3 alleles on acenocoumarol or phenprocoumon. Pharmacogenetics 14:27–33
Schalekamp T, van Geest-Daalderop JH, de Vries-Goldschmeding H, Conemans J, Bernsen Mj M, de Boer A (2004) Acenocoumarol stabilization is delayed in CYP2C9*3 carriers. Clin Pharmacol Ther 75:394–402
Visser L, van Schaik R, van Vliet M, Trienekens P, De Smet P, Vulto A, Hofman A, van Duijn C, Stricker B (2004) The risk of bleeding complications in patients with cytochrome P450 CYP2C9*2 or CYP2C9*3 alleles on acenocoumarol or phenprocoumon. Thromb Haemost 92:61–66
Hummers-Pradier E, Hess S, Adham I, Papke T, Pieske B, Kochen M (2003) Determination of bleeding risk using genetic markers in patients taking phenprocoumon. Eur J Clin Pharmacol 59:213–219
Rost S, Fregin A, Ivaskevicius V, Conzelmann E, Hortnagel K, Pelz HJ, Lappegard K, Seifried E, Scharrer I, Tuddenham EG, Muller CR, Strom TM, Oldenburg J (2004) Mutations in VKORC1 cause warfarin resistance and multiple coagulation factor deficiency type 2. Nature 427:537–541
Li T, Chang C-Y, Jin D-Y, Lin P-J, Khvorova A, Stafford DW (2004) Identification of the gene for vitamin K epoxide reductase. Nature 427:541–543
D’Andrea G, D’Ambrosio RL, Di Perna P, Chetta M, Santacroce R, Brancaccio V, Grandone E, Margaglione M (2005) A polymorphism in the VKORC1 gene is associated with an interindividual variability in the dose-anticoagulant effect of warfarin. Blood 105:645–649
Bodin L, Verstuyft C, Tregouet DA, Robert A, Dubert L, Funck-Brentano C, Jaillon P, Beaune P, Laurent-Puig P, Becquemont L, Loriot MA (2005) Cytochrome P450 2C9 (CYP2C9) and vitamin K epoxide reductase (VKORC1) genotypes as determinants of acenocoumarol sensitivity. Blood 106:135–140
Wadelius M, Chen LY, Downes K, Ghori J, Hunt S, Eriksson N, Wallerman O, Melhus H, Wadelius C, Bentley D, Deloukas P (2005) Common VKORC1 and GGCX polymorphisms associated with warfarin dose. Pharmacogenomics J 5:262–270
Yuan HY, Chen JJ, Lee MT, Wung JC, Chen YF, Charng MJ, Lu MJ, Hung CR, Wei CY, Chen CH, Wu JY, Chen YT (2005) A novel functional VKORC1 promoter polymorphism is associated with inter-individual and inter-ethnic differences in warfarin sensitivity. Hum Mol Genet 14:1745–1751
Rieder MJ, Reiner AP, Gage BF, Nickerson DA, Eby CS, McLeod HL, Blough DK, Thummel KE, Veenstra DL, Rettie AE (2005) Effect of VKORC1 haplotypes on transcriptional regulation and warfarin dose. N Engl J Med 352:2285–2293
Becquemont L (2007) Pharmacogenetics of Vitamin K antagonists. Joint Cold Spring Harbor Laboratiry/Wellcome Trust conference on Pharmacogenomics, Hinxton :4
Larramendy-Gozalo C, Yang JQ, Verstuyft C, Bodin L, Dubert L, Zhang Y, Xu C, Fan L, Jaillon P, Becquemont L (2006) Genetic Polymorphism of Vitamin K Epoxide Reductase (VKORC1) 1173C>T in a Chinese and a Caucasian Population. Basic Clin Pharmacol Toxicol 98:611–613
Schwartz U, Ritchie M, Bradford Y, Li C, Dudek S, Frye-Anderson A, Kim R, Roden D, Stein C (2008) Genetic determinants of response to warfarin during initial anticoagulation. N Engl J Med 358:999–1008
Gage B, Eby C, Johnson J, Deych E, Rieder M, Ridker P, Milligan P, Grice G, Lenzini P, Rettie A, Aquilante C, Grosso L, Marsh S, Langaee T, Farnett E, Voora D, Veenstra D, Glynn R, Barrett A, McLeod H (2008) Use of Pharmacogenetic and Clinical Factors to Predict the Therapeutic Dose of warfarin. Clin Pharmacol Ther Feb 27 [Epub ahead of print]
Reitsma P, van der Heijden J, Groot A, Rosendaal F, Büller H (2005) A C1173T Dimorphism in the VKORC1 Gene Determines Coumarin Sensitivity and Bleeding Risk. PLOS Medicine 2:996–998
Schalekamp T, Brasse BP, Roijers JF, Chahid Y, van Geest-Daalderop JH, de Vries-Goldschmeding H, van Wijk EM, Egberts AC, de Boer A (2006) VKORC1 and CYP2C9 genotypes and acenocoumarol anticoagulation status: interaction between both genotypes affects overanticoagulation. Clin Pharmacol Ther 80:13–22
Quteineh L, Verstuyft C, Descot C, Dubert L, Robert A, Jaillon P, Becquemont L (2005) Vitamin K epoxide reductase (VKORC1) genetic polymorphism is associated to oral anticoagulant overdose. Thromb Haemost 94:690–691
Crowther M (2003) The impact of CYP2C9 and VKORC1 genetic polymorphism and patient characteristics upon warfarin dose. Semin Vasc Med 3:255–260
Sconce E, Khan T, Wynne H, Avery P, Monkhouse L, King B, Wood P, Kesteven P, Daly A, Kamali F (2005) The impact of CYP2C9 and VKORC1 genetic polymorphism and patient characteristics upon warfarin dose requirements: proposal for a new dosing regimen. Blood 106:2329–2333
Wu A (2007) Use of genetic and nongenetic factors in warfarin dosing algorithms. Pharmacogenomics 8:851–861
Wen MS, Lee M, Chen JJ, Chuang HP, Lu LS, Chen CH, Lee TH, Kuo CT, Sun FM, Chang YJ, Kuan PL, Chen YF, Charng MJ, Ray CY, Wu JY, Chen YT (2008) Prospective Study of Warfarin Dosage Requirements Based on CYP2C9 and VKORC1 Genotypes. Clin Pharmacol Ther
Anderson JL, Horne BD, Stevens SM, Grove AS, Barton S, Nicholas ZP, Kahn SF, May HT, Samuelson KM, Muhlestein JB, Carlquist JF (2007) Randomized trial of genotype-guided versus standard warfarin dosing in patients initiating oral anticoagulation. Circulation 116:2563–2570
Caraco Y, Blotnick S, Muszkat M (2008) CYP2C9 genotype-guided warfarin prescribing enhances the efficacy and safety of anticoagulation: a prospective randomized controlled study. Clin Pharmacol Ther 83:460–470
Hillman MA, Wilke RA, Yale SH, Vidaillet HJ, Caldwell MD, Glurich I, Berg RL, Schmelzer J, Burmester JK (2005) A prospective, randomized pilot trial of model-based warfarin dose initiation using CYP2C9 genotype and clinical data. Clin Med Res 3:137–145
Kearon C, Ginsberg J, Kovacs M, Anderson D, Wells P, Julian J, MacKinnon B, Weitz J, Crowther M, Dolan S, Turpie A, Geerts W, Solymoss S, van Nguyen P, Demers C, Kahn S, Kassis J, Rodger M, Hambleton J, Gent M (2003) Comparison of low-intensity warfarin therapy with conventional-intensity warfarin therapy for long-term prevention of recurrent venous thromboembolism. N Eng J Med 349:675–683
Scordo MG, Pengo V, Spina E, Dahl ML, Gusella M, Padrini R (2002) Influence of CYP2C9 and CYP2C19 genetic polymorphisms on warfarin maintenance dose and metabolic clearance. Clin Pharmacol Ther 72:702–710
Takahashi H, Wilkinson GR, Caraco Y, Muszkat M, Kim RB, Kashima T, Kimura S, Echizen H (2003) Population differences in S-warfarin metabolism between CYP2C9 genotype-matched Caucasian and Japanese patients. Clin Pharmacol Ther 73:253–263
Taube J, Halsall D, Baglin T (2000) Influence of cytochrome P-450 CYP2C9 polymorphisms on warfarin sensitivity and risk of over-anticoagulation in patients on long-term treatment [In Process Citation]. Blood 96:1816–1819
Kamali F, Khan T, King B, Frearson R, Kesteven P, Wood P, Daly A, Wynne H (2004) Contribution of age, body size, and CYP2C9 genotype to anticoagulant response to warfarin. Clin Pharmacol Ther 75:204–212
Obayashi K, Nakamura K, Kawana J, Ogata H, Hanada K, Kurabayashi M, Hasegawa A, Yamamoto K, Horiuchi R (2006) VKORC1 gene variations are the major contributors of variation in warfarin dose in Japanese patients. Clin Pharmacol Ther 80:169–178
Millican EA, Lenzini PA, Milligan PE, Grosso L, Eby C, Deych E, Grice G, Clohisy JC, Barrack RL, Burnett RS, Voora D, Gatchel S, Tiemeier A, Gage BF (2007) Genetic-based dosing in orthopedic patients beginning warfarin therapy. Blood 110:1511–1515
Carlquist JF, Horne BD, Muhlestein JB, Lappe DL, Whiting BM, Kolek MJ, Clarke JL, James BC, Anderson JL (2006) Genotypes of the cytochrome p450 isoform, CYP2C9, and the vitamin K epoxide reductase complex subunit 1 conjointly determine stable warfarin dose: a prospective study. J Thromb Thrombolysis 22:191–197
Thijssen HH, Drittij MJ, Vervoort LM, de Vries-Hanje JC (2001) Altered pharmacokinetics of R- and S-acenocoumarol in a subject heterozygous for CYP2C9*3. Clin Pharmacol Ther 70:292–298
Montes R, Ruiz de Gaona E, Martínez-González M, Alberca I, Hermida J (2006) The c.-1639G > A polymorphism of the VKORC1 gene is a major determinant of the response to acenocoumarol in anticoagulated patients. Br J Haematol 133:183–187
Verstuyft C, Robert A, Morin S, Loriot MA, Flahault A, Beaune P, Funck-Brentano C, Jaillon P, Becquemont L (2003) Genetic and environmental risk factors for oral anticoagulant overdose. Eur J Clin Pharmacol 58:739–745
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Becquemont, L. Evidence for a pharmacogenetic adapted dose of oral anticoagulant in routine medical practice. Eur J Clin Pharmacol 64, 953–960 (2008). https://doi.org/10.1007/s00228-008-0542-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-008-0542-2