Abstract
Roux-en-Y gastric bypass surgery (RYGB) is an effective treatment of morbid obesity, with positive effects on obesity-related complications. The treatment is associated with bone loss, which in turn might increase fracture risk. The aim of this study was to evaluate changes in bone mineral density (BMD) and bone architecture assessed using dual-energy X-ray absorptiometry (DXA) and high-resolution peripheral quantitative computed tomography (HR-pQCT), 6 and 12 months after RYGB, and correlate them to changes in selected biochemical markers. A prospective cohort study included 25 morbidly obese patients (10 males, 15 females). Patients were examined with DXA of the hip and spine, HR-pQCT of radius and tibia, and blood sampling before and 6 and 12 months after RYGB. Patients lost in average 33.5 ± 12.1 kg (25.8 ± 8.5 %) in 12 months. In tibia, we found significant loss of total, cortical and trabecular volumetric BMD after 12 months (all p < 0.001). Microarchitectural changes involved lower trabecular number, increased trabecular separation, and network inhomogeneity along with thinning of the cortex. Estimated bone failure load was decreased after 12 months (p = 0.005). We found only minor changes in radius. Results demonstrate significant alterations of bone microarchitecture suggesting an accelerated endosteal resorption along with disintegration of the trabecular structure which resulted in a loss of estimated bone strength in tibia. Such changes may underlie the recently reported increased risk of fracture in bariatric patients after surgery. We only observed bone structural changes in the weight-bearing bone, which indicates that mechanical un-loading is the primary mediator.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Morbid obesity, defined as a body mass index (BMI) > 40 kg/m2, is an increasing health problem. Bariatric surgery has become a popular treatment of obesity, when conservative methods are ineffective. One of the frequently used bariatric surgeries is Roux-en-Y gastric bypass (RYGB), which involves anatomical changes of the gastrointestinal tract, resulting in a significantly smaller reservoir for food, as well as induced malabsorption. The treatment has proven successful in significantly reducing weight and also has positive effects on type 2 diabetes, cardiovascular disorders, fertility, sleep apnoea, and other obesity-related complications [1, 2]. However, the procedure entails several short- and long-term risks, and the impact of bariatric surgery on long-term skeletal health is still poorly understood.
Malabsorption results in nutritional deficiencies such as low vitamin D and hypocalcaemia, thereby causing secondary hyperparathyroidism, which is a well-known complication of RYGB [3].
Previous studies have established a complicated interplay between bone and adipose tissue, however, the exact role of e.g. adipokines like leptin and adiponectin remains uncertain [4]. Leptin is produced by adipocytes, and leptin levels are directly dependent on fat mass. Also, high fat mass is related to leptin resistance [5, 6]. Leptin exerts both formative and resorptive remodelling of bone [7]; however, the overall role remains unclear.
The role of adiponectin, also produced in adipose tissue, in bone remodelling is controversial; however, most studies reported an anti-osteogenic effect [8, 9].
Furthermore, it has been established that changes in mechanical loading influence bone [10–12], but whether this influences bone fragility and fracture risk is an on-going area of investigation. Most studies have found a site-dependent difference in fracture risk in obese compared to normal-weight individuals, where fractures at the hip and pelvis were less prevalent and fractures at the humerus were more prevalent [4, 13–16]. Only a few studies have evaluated the risk of fracture in patients following bariatric surgery. One study found no increased risk of fracture [17], whereas a recent study report a 2.3-fold increased risk of fracture at any site [18]. Thus, changes in bone after bariatric surgery may compromise bone strength and lead to an increase in fracture risk.
Effects on bone after RYGB have primarily been evaluated by dual-energy x-ray absorptiometry (DXA) [9, 19, 20]. However, DXA precision declines with increasing BMI [21] and studies have shown errors in DXA measurement up to ± 20 % [22, 23]. Thus, it is possible that artefacts related to DXA measurements, could distort the observed changes in bone mineral density (BMD) [22–25].
Three previous studies have evaluated skeletal changes after RYGB by DXA, quantitative computed tomography (QCT) and high-resolution peripheral computed tomography (HR-pQCT) and find decreased volumetric BMD (vBMD) of both hip and spine by QCT and radius and tibia by HR-pQCT [24, 26, 27].
To further elaborate effects on bone after RYGB, the aim of this study was to evaluate changes in BMD and bone architecture as assessed using DXA and HR-pQCT, 6 and 12 months after RYGB and subsequently correlate them to changes in selected biochemical markers.
Participants and Methods
Participants
The study group included 25 patients at baseline and 6 months follow-up (10 males, 15 females). Between 6 and 12 months one female patient was lost to follow-up.
Inclusion of patients was conducted at pre-operative information meetings between October 2011 and August 2012 at the Nutrition Clinic, Department of Endocrinology, Odense University Hospital and from the Department of Endocrinology, Hospital of Southwest Denmark.
All invited participants fulfilled the Danish national guideline criteria for referral to RYGB, which was age >25 years and BMI > 35 kg/m2 plus at least one obesity-related complication or BMI > 50 kg/m2. All included patients had undertaken an 8 % voluntary weight loss driven by dietary restriction in a 3–12 months period before surgery, as required by the national guidelines.
The RYGB surgery was performed at two public hospitals (Esbjerg and Odense) in the Region of Southern Denmark by the same surgeon at each location. The RYGB procedure involved creating a 20-ml gastric pouch, a 150-cm Roux-limb and a 60-cm biliopancreatic limb.
After surgery, patients were recommended a supplemental daily intake of 800 mg calcium and 1920 IU vitamin D. Mineral og vitamin status was assessed after 6 and 12 months and supplements were adjusted if necessary.
Exclusion criteria were any competing bone disease, on-going use of medication with influence on bone, inability to walk without walking aids, perimenopausal status (defined as irregular periods or last bleeding <1 year ago) or pregnancy. Patients with biochemical conversion from premenopausal to peri- or postmenopausal status under follow-up were excluded from data analysis.
Medical History
At baseline, medical and fracture history (all fractures, including traumatic), as well as medications, and menopausal status when relevant, were obtained by questionnaires.
Blood Sampling and Analysis
All patients had blood samples drawn, after an overnight fast, at each visit. Parathyroid hormone (PTH), estradiol, follicle stimulating hormone (FSH) and luteinizing hormone (LH) were analysed on the day of blood sampling. Parathyroid hormone was analysed by a solid-phase, two-site chemiluminescent enzyme-labelled immunometric assay (Immulite 2000, Siemens). Estradiol was analysed by a chemiluminescence method using a micropartial immunoassay (Abbott) and LH/FSH was analysed by TR-IFMAs (AutoDelfia, Perkin Elmer). The coefficient of variation (CV) ranged from 4 to 6 %.
Another blood sample was frozen and stored at minus 80 degrees Celcius until analysis for 25-OH-Vitamin D, leptin, adiponectin, procollagen type I amino-terminal propeptide (P1NP-intact) and C-terminal telopeptide of type 1 collagen (CTX-I). 25-OH-vitamin D was determined using the Elecsys Vitamin D total electro-chemiluminescence binding assay on the automated Cobas e411 analyzer (Roche Diagnostics, Rotkreuz, Switzerland). P1NP-intact and CTX-I was analysed by a chemiluminescence method using a fully automated immunoassay system (iSYS, Immunodiagnostic Systems Ltd., Boldon, England). The samples were analysed in a single run with the same batch of the reagents/assay. Moreover, samples were analysed for leptin and adiponectin using a Bio-Plex Pro assay (Bio-Rad Laboratories, Hercules, CA, USA) on a MagPix analyser system (Luminex Corporation, Austin, TX, USA). The intermediary precision CV ranged from 8 to 10 %.
Dual-Energy X-ray Absorptiometry
Areal BMD (aBMD) was measured in the hip (femoral neck, trochanteric region and total hip) and lumbar spine (L1–L4) using DXA (Hologic Discovery, Waltham, MA, USA). In addition, a DXA whole-body scan provided data on body composition.
The CV at our unit was 1 % in both hip and lumbar spine region.
High-resolution Peripheral Quantitative Computed Tomography
Assessment of bone geometry, vBMD, trabecular and cortical microarchitecture and estimated strength at the nondominant distal radius and tibia (or the dominant extremity in case of previous fracture at the desired site) was achieved using HR-pQCT (XtremeCT, Scanco Medical AG, Brüttisellen, Switzerland). The image acquisition, image analysis and validation of the method have been described in detail elsewhere [28–31]. In brief, a 2D radiograph was obtained and the region of interest (ROI) was positioned with a 9.5 mm and 22.5 mm offset from the radius and tibia endplate, respectively, and extended 9.02 mm proximally. Each image comprised 110 slices with an isotropic 82-μm voxel size. The operator immediately viewed the most distal slice for motion artefacts (e.g. blurring or cortical discontinuities) and up to two repeat acquisitions at each site were performed in case of visible motion artefacts. After reconstruction, image quality was graded by one author (S.Hansen) using a five-step scale as suggested by the manufacturer (1 = best, 5 = worst) and images with grade >3 were disregarded [32]. To ensure identical ROI at baseline and follow-up, an automated matching procedure, based on changes in bone area throughout the scan region, was applied [33]. Changes in total bone area were, however, assessed using unmatched images. First, trabecular bone evaluation was performed using the manufacturer’s default method, where trabecular bone volume per tissue volume (BV/TV) was calculated from trabecular vBMD assuming a mineral density of fully mineralized bone of 1.2 mg hydroxyapatite (HA)/mg3 [33]. Trabecular number (Tb·N) was extracted using a distance transformation method, whereas trabecular thickness (Tb·Th) and trabecular separation (Tb·Sp) were derived from BV/TV and Tb.N [Tb·Th = (BV/TV)/Tb.N; Tb.Sp = (1 − BV/TV)/Tb.N]. Also, the standard deviation (SD) of 1/Tb·N was calculated, serving as an index of trabecular network inhomogeneity. Second, an automatic cortical bone analysis based on a dual-threshold approach was applied, which isolates the cortical region and allows for a direct 3D measure of cortical thickness, along with measures of cortical porosity (percent void cortical volume/total cortical volume) and mean cortical pore diameter [34, 35]. Finally, bone strength was estimated in a finite element analysis (FEA) solver using software provided by the manufacturer (μFE Element Analysis Solver v.1.15; Scanco Medical, Brüttisellen, Switzerland) as described by Pistoia and colleagues [36]. Voxels representing bone were converted into eight-node brick elements and boundary conditions represent a high-friction compression test. A Young’s modulus of 10 GPa and a Poisson’s ratio of 0.3 were applied. From the models, estimated bone stiffness was calculated along with an estimate of bone failure load, based on the assumption that the bone fails if >2 % of the elements are strained beyond 0.7 % [36].
In our unit, the CV for geometry, vBMD, microarchitecture and FEA measures ranges from 0.2 to 7.2 % as detailed elsewhere [37].
Statistical Analysis
Data are reported as mean ± SD or median and interquartile range (25;75 percentiles) as appropriate. Categorical outcomes were evaluated by the χ 2 test. DXA and HR-pQCT data were evaluated by a paired t test or Wilcoxon signed-rank test as appropriate, whereby each patient were considered their own control.
Univariate linear regression models were performed to identify associations between baseline age and gender and changes in bone parameters in tibia after 1 year. Also linear regression analysis of one-year changes in total weight, lean mass, P1NP, CTX-I, adiponectin, leptin and 25-OH-vitamin D versus one-year changes in bone parameters in tibia (only performed for those bone parameters that changed significantly from baseline to 1 year). Multiple regression analysis was used to identify the contribution of gender, age and one-year change in weight on one-year changes in bone parameters in tibia. P-values < 0.05 were considered statistically significant. STATA version 13.1 (StataCorp LP, College Station, TX, USA) was used for data analysis and graphics. GraphPad Prism version 6 (Graphpad Software Inc., San Diego, CA, USA) was used for graphics.
Results
Study Population Characteristics and Biochemistry
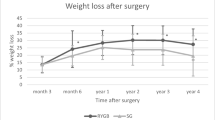
Of thirty-one eligible patients, one was excluded due to osteoporosis at baseline DXA, one was excluded due to kidney disease and need for dialysis and four women changed from pre- to perimenopausal status during follow-up and were excluded from data analysis (Fig. 1). No patients were excluded due to weight limits of DXA or HR-pQCT. Thus, 25 patients (15 women, 10 men) were included in the study. One of the 15 women was postmenopausal. The patients had a baseline age of 41.2 ± 8.1 years (Table 1) and had a pre-operative height and weight of 172.4 ± 9.5 cm and 126.0 (111.0;143.8) kg, respectively. Patients presented a substantial weight loss of 25.5 ± 7.0 kg (20.0 ± 4.9 %) at 6 months post-operatively, which increased to 33.5 ± 12.1 kg (25.8 ± 8.5 %) after one year.
A significant increase in both P1NP and CTX-I was observed after 6 (46.7 ± 66.0 % and 111.7 ± 101.4 % both p < 0.001) and 12 months (51.4 ± 65.2 % and 96.6 ± 99.4 % both p < 0.001). At baseline, patients presented with low 25-OH-Vitamin D (35.9 nmol/L (23.4;47.7), which increased to normal levels post-operative (6 months: 60.4 nmol/L (47.2;75.1); 12 months: 57.4 nmol/L (45.5;68.2) both p ≤ 0.002). No statistically significant change was observed in PTH.
Furthermore, we found a significant decrease in leptin (6 months: −63.4 % (−75.0;−50.3); 12 months: −70.7 % (−87.4;−61.0) both p < 0.001) and an increase in adiponectin (6 months: 55.9 ± 46.7 %; 12 months: 115.0 ± 84.9 % both p < 0.001).
DXA
One year after RYGB both spine (-3.1 ± 3.5 %; p < 0.001) and total hip aBMD (−8.1 ± 4.8 %; p < 0.001) declined significantly (Table 1). At baseline, patients had a median total fat percent of 47.0 (40.4;49.9). Following RYGB we observed a significant decrease in both fat mass (6 months: −31.7 ± 7.6 %; 12 months: −41.2 ± 18.5 % both p < 0.001), lean mass (6 months: −10.5 ± 4.8 % 12 months: −12.4 ± 6.8 % both p < 0.001) and fat percent (6 months: −14.7 ± 5.9 %; 12 months: −32.1 ± 14.6 % both p < 0.001). We found no changes in total body aBMD.
HR-pQCT
One radius image obtained at the six months visit was discarded due to motion artefacts. All tibia images had adequate quality.
In radius (Table 2), no statistically significant changes were observed in bone geometry, vBMD or bone microarchitecture after 6 months. After 12 months a slight decrease in trabecular vBMD (−0.6 % (−2.6;0.7); p = 0.04) along with decreased BV/TV (−1.5 ± 3.1 %; p = 0.04) and increased network inhomogeneity (3.7 % (−4.7;10.0); p = 0.04) were observed. No significant changes in bone area, Tb·N, Tb·Th, Tb.Sp or FEA estimated bone strength were found.
In tibia (Table 3), a slight decrease in total vBMD (−0.4 % (−1.6;0.3); p = 0.04) was observed 6 months post-operatively whereas no other indices were significantly changed compared to baseline. After 1 year, trabecular area increased (0.5 ± 0.7 %; p = 0.007) and cortical area decreased (−3.2 ± 3.4 %; p < 0.001), whereas total area was unchanged. We observed significant cortical thinning after 12 months (−2.3 % (−5.6;−0.9); p = 0.049). Volumetric BMD in both the trabecular (−0.7 % (−5.1;0.3); p = 0.003) and cortical (−0.4 % (−1.4;0.1); p = 0.008) compartments declined, along with an overall decrease in total vBMD (−2.6 ± 2.5 %; p < 0.001). In the trabecular compartment, we observed a significant reduction in Tb.N (−5.2 ± 8.8 %; p = 0.004), with increased Tb·Sp (6.9 ± 10.6 %; p = 0.006). Bone volume per tissue volume decreased (−1.1 % (−5.4;0.0); p = 0.003) and trabecular network inhomogeneity increased (9.3 % (−0.5;15.5); p = 0.003). No changes were observed in cortical microarchitecture. By FEA, a significant decrease in both estimated bone stiffness and failure load were found after 1 year (−2.1 ± 4.3 %; p = 0.038 and −2.3 ± 3.6 %; p = 0.005, respectively).
Regression Analysis
In univariate regression, we found that weight loss was correlated to declines in total vBMD (r = 0.51; p = 0.011) (Fig. 2). No significant correlations were found between baseline age or gender and changes in bone parameters.
Increase in CTX-I was associated with declines in cortical area (r = −0.52; p = 0.009), vBMD (r = −0.41; p = 0.049) and thickness (r = −0.49; p = 0.015) and with an increase in trabecular area (r = 0.42; p = 0.040). No significant correlations were found between increase in P1NP and changes in bone parameters.
Increase in adiponectin was associated with decrease in cortical thickness (r = −0.49; p = 0.015) while decreased leptin was correlated to increase in Tb.N (r = −0.44; p = 0.034).
Increased 25-OH-vitamin D was associated with reduced loss of trabecular vBMD (r = 0.45; p = 0.030) and BV/TV (r = 0.44; p = 0.036).
In a multivariate regression analysis, determining the joint contribution of gender, age and change in weight on changes in the abovementioned bone parameters after 12 months, we found that the change in weight was positively associated with total vBMD (R 2 = 0.26; p = 0.03). None of the other factors contributed significantly.
Discussion
Examining microstructural bone changes after RYGB, we found significant changes in both the trabecular and cortical compartment in tibia after 12 months (Fig. 3). The changes entail reduced cortical thickness, increased trabecular area and unaltered total bone area, which could be explained by altered endosteal bone remodelling. Speculatively, an accelerated bone remodelling combined with a net deficit in bone formation compared to bone resorption may have caused these alterations. This is in accordance with previous findings [24, 26]. Only a few changes were observed in radius. We found that changes in bone parameters were not statistically significant before 12 months, even though the highest rate of weight loss and level of bone resorption marker was seen 6 months after surgery. Evaluated by DXA we found significant loss of aBMD in the hip after 6 months and both the hip and spine after 12 months. This is in accordance with several previous studies [9, 19, 38, 39]. We did not find any significant changes in total aBMD by whole-body DXA, which might be explained by an uneven site distribution of changes in aBMD. Some [9, 40], but not all [24], previous studies found significant changes in whole-body DXA.
Loss of vBMD was associated with weight loss (Fig. 2), which remained significant after controlling for age and gender, and we found significant increases in bone turnover markers without signs of secondary hyperparathyroidism at both 6 and 12 months after RYGB.
Structural Changes in Radius and Tibia
We found only few significant changes in the non-weight-bearing radius including changes in the trabecular compartment, with increased trabecular vBMD, BV/TV and network inhomogeneity. In contrast, in tibia, we found reductions in total, trabecular and cortical vBMD. Furthermore, we found decreases in cortical area and thickness along with significantly altered trabecular microarchitecture with reduced number of trabeculae, lower BV/TV and increased Tb.Sp.
Stein et al. [26] evaluated bone alterations in obese women one year after RYGB or gastric banding using DXA and HR-pQCT and found cortical deterioration of both radius and tibia associated with secondary hyperparathyroidism. A recent study by Yu and colleagues [27] evaluated patients after RYGB with DXA, QCT and HR-pQCT and found changes, similar to ours, in trabecular architecture in tibia after 24 months [27]. The observation that bone changes in our study were primarily found in tibia and not radius, indicate that changes are mainly caused by mechanical un-loading, rather than hormonal changes. Patients were mobilised within a few hours post-operative, and urged to continue mobilisation after discharge, thus mechanical un-loading are attributable primarily to weight loss and not bed rest. Yu et al. report changes in radius after 24 months [27], thus, hormonal changes may still be relevant to the long-term bone remodelling after RYGB.
Fracture Risk After RYGB
It is still somewhat uncertain whether RYGB is related to a clinically relevant increase in fracture risk. Obesity has been found to increase the risk of fractures at the humerus, lower leg and vertebrae, but a decrease in the risk of fractures at the wrist, hip and pelvis. A recent study [18] reported an increased risk of fracture in the lower leg, femur, humerus and vertebrae in obese patients after RYGB. However, patients were compared to normal-weight controls and furthermore the findings cannot be solely related to RYGB, and may still also be related to obesity per se. The disintegration of cortical and trabecular bone we observed, resulted in decreased estimated failure load, assessed by FEA, which in theory may underlie the described increase in the risk of fractures in these patients. However, no studies exist, verifying a clinical correlation between FEA estimated failure load and risk of fracture.
Long-term observational studies, with obese control cohorts are needed to further clarify these relations.
Associations Between Changes in Weight, Biochemistry and Bone Parameters
In univariate linear regression analysis, we found that a larger weight loss was associated with a larger decline in total vBMD (Fig. 2) which remained significant after controlling for age and gender.
CTX-I was associated with bone changes consistent with the process of endocortical resorption. At 12 months, both CTX-I and P1NP had increased with about 97 and 51 %, respectively. CTX-I, however, was increased at 6 months and were almost unchanged between 6 and 12 months, whereas P1NP continued to increase after 6 months.
This indicates an early bone remodelling, not driven by secondary hyperparathyroidism, even though significant bone structural changes were not measurable before 12 months. Also, bone formation tended to dominate the remodelling in time.
In univariate analysis, we found that increase in adiponectin were associated with decrease in cortical thickness in tibia, in accordance with the previously reported anti-osteogenic effect [8, 9]. Leptin was associated with increase in Tb·N; this is contrary to our reported decreasing Tb·N in tibia, which might indicate that change in Tb.N is primarily influenced by other factors, not accounted for in our regression analysis.
The bone microarchitectural changes were observed in spite of increasing levels of 25-OH-vitamin D and no significant changes in PTH levels, which are probably attributable to the calcium and vitamin D supplements given post-operatively.
Limitations
The study has some limitations. The small study group results in limited statistical power, when evaluating bone parameters with minor changes, and also implicate inability to stratify our data by gender. We only included one postmenopausal woman, which preclude us from applying our conclusions to this patient group. Also, all patients underwent a voluntary weight loss of at least 8 % prior to surgery, which possibly resulted in minor bone changes.
With the extensive weight loss, a change in adipose tissue thickness of the extremities, may influence the error in HR-pQCT measurements. However, a study by Yu and colleagues, find a smaller and more uniform error when adding fat layers in HR-pQCT measurements than in DXA measurements [23].
Conclusion
In conclusion, RYGB results in significant alterations of bone microarchitecture, regardless of gender, especially as cortical thinning along with disintegration of the trabecular structure in tibia. This might be a contributory cause of the recently reported long-term increased risk of fracture in this group. Patients had increasing vitamin D levels, probably as a result of supplements post-operative, and no significant changes in PTH. We found weight loss to be correlated to loss of total vBMD in tibia, which remained significant after controlling for gender and age. We mainly observed bone structural changes in the weight-bearing bone, which indicates that mechanical un-loading is the primary mediator of early bone changes after RYGB. More studies are necessary to further clarify the relationship between post-operative hormonal changes, microstructural bone changes and long-term fracture risk.
References
Sjöström L, Lindroos A, Peltonen M, Torgerson J, Bouchard C, Carlsson B et al (2004) Lifestyle, diabetes and cardiovascular Risk Factors 10 years after bariatric surgery. N Engl J Med 351(26):2683–2693
Davies SW, Efird JT, Guidry CA, Penn RI, Sawyer RG, Schirmer BD et al (2015) Twenty-first century weight loss: banding versus bypass. Surg Endosc 29(4):947–954
Hewitt S, Søvik TT, Aasheim ET, Kristinsson J, Jahnsen J, Birketvedt GS et al (2013) Secondary hyperparathyroidism, vitamin D sufficiency, and serum calcium 5 years after gastric bypass and duodenal switch. Obes Surg 23(3):384–390
Reid IR (2010) Fat and bone. Arch Biochem Biophys 503(1):20–27
Frederich RC, Hamann A, Anderson S, Löllmann B, Lowell BB, Flier JS (1995) Leptin levels reflect body lipid content in mice: evidence for diet-induced resistance to leptin action. Nat Med 1(12):1311–1314
Maffei M, Halaas J, Ravussin E, Pratley RE, Lee GH, Zhang Y et al (1995) Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat Med 1(11):1155–1161
Chen XX, Yang T (2015) Roles of leptin in bone metabolism and bone diseases. J Bone Miner Metab 33(5):474–485
Lenchik L, Register TC, Hsu FC, Lohman K, Nicklas BJ, Freedman BI et al (2003) Adiponectin as a novel determinant of bone mineral density and visceral fat. Bone 33(4):646–651
Carrasco F, Ruz M, Rojas P, Csendes A, Rebolledo A, Codoceo J et al (2009) Changes in bone mineral density, body composition and adiponectin levels in morbidly obese patients after bariatric surgery. Obes Surg 19(1):41–46
Reid IR (2008) Relationships between fat and bone. Osteoporos Int 19(5):595–606
Spector ER, Smith SM, Sibonga JD (2009) Skeletal effects of long-duration head-down bed rest. Aviat Space Environ Med 80(5):23–28
LeBlanc AD, Spector ER, Evans HJ, Sibonga JD (2007) Skeletal responses to space flight and the bed rest analog: a review. J Musculoskelet Neuronal Interact 7(1):33–47
Beck TJ, Petit MA, Wu G, LeBoff MS, Cauley JA, Chen Z (2009) Does obesity really make the femur stronger? BMD, geometry, and fracture incidence in the women’s health initiative-observational study. J Bone Miner Res 24(8):1369–1379
Prieto-Alhambra D, Premaor MO, Fina Avilés F, Hermosilla E, Martinez-Laguna D, Carbonell-Abella C et al (2012) The association between fracture and obesity is site-dependent: a population-based study in postmenopausal women. J Bone Miner Res 27(2):294–300
Gnudi S, Sitta E, Lisi L (2009) Relationship of body mass index with main limb fragility fractures in postmenopausal women. J Bone Miner Metab 27(4):479–484
Nielson CM, Marshall LM, Adams AL, LeBlanc ES, Cawthon PM, Ensrud K et al (2011) BMI and fracture risk in older men: the osteoporotic fractures in men study (MrOS). J Bone Miner Res 26(3):496–502
Lalmohamed A, de Vries F, Bazelier MT, Cooper A, van Staa T-P, Cooper C et al (2012) Risk of fracture after bariatric surgery in the United Kingdom: population based, retrospective cohort study. BMJ 345:e5085
Nakamura KM, Haglind EGC, Clowes JA, Achenbach SJ, Atkinson EJ, Melton LJ et al (2014) Fracture risk following bariatric surgery: a population-based study. Osteoporos Int 25(1):151–158
Mahdy T, Atia S, Farid M, Adulatif A (2008) Effect of Roux-en Y gastric bypass on bone metabolism in patients with morbid obesity: mansoura experiences. Obes Surg 18(12):1526–1531
Vilarrasa N, Gómez JM, Elio I, Gómez-Vaquero C, Masdevall C, Pujol J et al (2009) Evaluation of bone disease in morbidly obese women after gastric bypass and risk factors implicated in bone loss. Obes Surg 19(7):860–866
Nelson L, Gulenchyn KY, Atthey M, Webber CE (2010) Is a fixed value for the least significant change appropriate? J Clin Densitom 13(1):18–23
Bolotin HH (2007) DXA in vivo BMD methodology: an erroneous and misleading research and clinical gauge of bone mineral status, bone fragility, and bone remodelling. Bone 41(1):138–154
Yu EW, Thomas BJ, Brown JK, Finkelstein JS (2012) Simulated increases in body fat and errors in bone mineral density measurements by DXA and QCT. J Bone Miner Res 27(1):119–124
Yu EW, Bouxsein ML, Roy AE, Baldwin C, Cange A, Neer RM et al (2014) Bone loss after bariatric surgery: discordant results between DXA and QCT bone density. J Bone Miner Res 29(3):542–550
Evans EM, Mojtahedi MC, Kessinger RB, Misic MM (2006) Simulated change in body fatness affects Hologic QDR 4500A whole body and central DXA bone measures. J Clin Densitom. 9(3):315–322
Stein EM, Carrelli A, Young P, Bucozsky M, Zhang C, Schrope B et al (2013) Bariatric Surgery Results in Cortical Bone Loss. J Clin Endocrinol Metab 98(2):541–549
Yu EW, Bouxsein ML, Putman MS, Monis EL, Roy AE, Pratt JS a., et al. (2015) Two-year changes in bone density after Roux-en-Y gastric bypass surgery. J Clin Endocrinol Metab 100(4):1452–1459
Laib A, Rüegsegger P (1999) Calibration of trabecular bone structure measurements of in vivo three-dimensional peripheral quantitative computed tomography with 28-microm-resolution microcomputed tomography. Bone 24(1):35–39
Laib A, Hildebrand T, Häuselmann HJ, Rüegsegger P (1997) Ridge number density: a new parameter for in vivo bone structure analysis. Bone 21(6):541–546
Müller R, Hildebrand T, Häuselmann HJ, Rüegsegger P (1996) In vivo reproducibility of three-dimensional structural properties of noninvasive bone biopsies using 3D-pQCT. J Bone Miner Res 11(11):1745–1750
Boutroy S, Bouxsein ML, Munoz F, Delmas PD (2005) In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 90(12):6508–6515
Pauchard Y, Liphardt A-M, Macdonald HM, Hanley DA, Boyd SK (2012) Quality control for bone quality parameters affected by subject motion in high-resolution peripheral quantitative computed tomography. Bone 50(6):1304–1310
Laib A, Häuselmann HJ, Rüegsegger P (1998) In vivo high resolution 3D-QCT of the human forearm. Technol Heal care 6(5–6):329–337
Burghardt AJ, Buie HR, Laib A, Majumdar S, Boyd SK (2010) Reproducibility of direct quantitative measures of cortical bone microarchitecture of the distal radius and tibia by HR-pQCT. Bone 47(3):519–528
Nishiyama KK, Macdonald HM, Buie HR, Hanley DA, Boyd SK (2010) Postmenopausal women with osteopenia have higher cortical porosity and thinner cortices at the distal radius and tibia than women with normal aBMD: an in vivo HR-pQCT study. J Bone Miner Res. 25(4):882–890
Pistoia W, van Rietbergen B, Lochmüller E-M, Lill CA, Eckstein F, Rüegsegger P (2002) Estimation of distal radius failure load with micro-finite element analysis models based on three-dimensional peripheral quantitative computed tomography images. Bone. 30(6):842–848
Hansen S, Hauge EM (2013) Beck Jensen JE, Brixen K. Differing effects of PTH 1-34, PTH 1-84, and zoledronic acid on bone microarchitecture and estimated strength in postmenopausal women with osteoporosis: an 18-month open-labeled observational study using HR-pQCT. J Bone Miner Res 28(4):736–745
Fleischer J, Stein EM, Bessler M, Della Badia M, Restuccia N, Olivero-Rivera L et al (2008) The decline in hip bone density after gastric bypass surgery is associated with extent of weight loss. J Clin Endocrinol Metab 93(10):3735–3740
Pereira FA, Foss MC (2007) Impact of marked weight loss induced by bariatric surgery on bone mineral density and remodeling. Braz J Med Biol Res 40:509–517
Vilarrasa N, San José P, García I, Gómez-Vaquero C, Miras PM, de Gordejuela AGR et al (2011) Evaluation of bone mineral density loss in morbidly obese women after gastric bypass: 3-year follow-up. Obes Surg 21(4):465–472
Acknowledgments
Thanks to Steffanie Anthony Christensen and the rest of the staff at the Osteoporosis clinic, Odense University Hospital, for patient management.
Funding
The study was supported by grants from the region of Southern Denmark.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KD. Frederiksen, S. Hanson S. Hansen, J. Gram and N.R. Jørgensen had no conflicts of interest related to the current study. K. Brixen has received consultant fees and grants from MSD, are investigator for MSD, Amgen, Novartis and NPS and part in speakers bureau for Amgen and GlaxoSmithKline. R.K. Stoving has received consultant and lecture fees from Novo Nordisk.
Human and Animal Rights and Informed Consent
All participants provided written informed consent before inclusion, and the study was approved by The Regional Scientific Ethical Committee for Southern Denmark (File No. 2011-0050).
Additional information
Katrine Diemer Frederiksen and Stine Hanson have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Frederiksen, K.D., Hanson, S., Hansen, S. et al. Bone Structural Changes and Estimated Strength After Gastric Bypass Surgery Evaluated by HR-pQCT. Calcif Tissue Int 98, 253–262 (2016). https://doi.org/10.1007/s00223-015-0091-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-015-0091-5