Abstract
Body mass index (BMI) has been found to be related to the risk of osteoporotic hip fractures in women, regardless of bone mineral density (BMD). The same relationship is under debate for other limb fragility fractures. Very few studies have investigated the comparison of fracture risk among BMI categories, classified according to the WHO criteria, despite the potential usefulness of such information for clinical purposes. To address these issues we studied 2,235 postmenopausal women including those with fragility fractures of the hip (187), ankle (108), wrist (226) and humerus (85). Statistical analyses were performed by logistic regression by treating the fracture status as the dependent variable and age, age at menopause, femoral neck BMD and BMI as covariates. BMI was tested as a continuous or categorical variable. As a continuous variable, increased BMI had a protective effect against hip fracture: OR 0.949 (95% CI, 0.900–0.999), but carried a higher risk of humerus fracture: OR 1.077 (95% CI, 1.017–1.141). Among the BMI categories, only leanness: OR 3.819 (95% CI, 2.035–7.168) and obesity: OR 3.481 (95% CI, 1.815–6.678) showed a significantly higher fracture risk for hip and humerus fractures, respectively. There was no relationship between ankle and wrist fractures and BMI. In conclusion, decreasing BMI increases the risk for hip fracture, whereas increasing BMI increases the risk for humerus fractures. Leanness-related low BMD and obesity-related body instability might explain the different BMI relationships with these two types of fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone mineral density (BMD) has been found to be the main predictor of fragility fractures [1]. Among other predictors of fragility fracture the body mass index (BMI), a height standardised measure of body weight, has also been found to be related to the risk of osteoporotic fractures [2, 3], thus representing a factor to be considered in their prevention. The role of BMI as a risk factor for fragility fracture is mediated mainly by its relationship with the BMD, of which BMI is one of the main determinants. Nevertheless, BMI may also be a risk factor for fragility fracture regardless of BMD by increasing the propensity to fall due to muscle weakness in lean people, or due to increased postural instability of obese people. These different modes of action may explain the reported divergent relationship of BMI with the fracture risk in different limb fractures. In fact, BMI has been found to be inversely related with the risk of osteoporotic hip fracture [2, 4, 5], while its relationship with other limb fragility fractures, such as humerus, wrist and ankle fractures, is still debated among authors [6–13]. A lack of, inverse, or direct correlation has been reported according to the fracture type. These contrasting relationships of body mass with the limb fragility fracture risk need to be investigated further not only for research purposes, but also for clinical reasons. In fact, advice on lifestyle habits to optimise BMI for fracture prevention should be given to patients, also taking into account that BMI is implicated in the prevention of metabolic and cardiovascular diseases [14]. To address these issues we assessed the BMD-independent relationship of the BMI in a cross-sectional study in a sample of Italian postmenopausal women, both as a continuous and categorical variable (categorising the BMI according to the WHO), with the risk of main limb osteoporotic fractures.
Subjects and methods
For this study we analysed the data of 2,235 postmenopausal women who had been screened for previous observational studies of osteoporosis (data only partially published) [15]. This group of consecutive not institutionalised in- and out-patients had femoral neck BMD (FN BMD) measurement at our centre from November 2002 to December 2004 for a bone mass checkup or for clinical reasons. The women were interviewed after menopause about previous fractures of the humerus, wrist, ankle and hip that had occurred within 5 years of the survey. Only fractures due to minimal trauma (falls when walking or standing) documented radiologically were considered. Controls were postmenopausal women without fracture. Women having undergone treatments with drugs known to affect bone, those having had malignancies, endocrine diseases, Paget’s bone disease, rheumatoid arthritis, long-term immobilisation, or arthroplasty were excluded. BMD was measured at the left hip, or the right hip in those having had left hip fracture, by using a Norland XR 36 pencil beam densitometer (Norland, Fort Atchinson, WI, USA). For DXA scan acquisition, the women were positioned according to the manufacturer’s instructions by using the dedicated leg fixture device. The machine daily quality assurance test was performed according to the manufacturer’s instructions. The coefficient of variation of the FN BMD measurement in our hands is 1.9 ± 0.7%, as previously reported [15]. Age, age at menopause, height and weight were also collected for each enrolled woman. Weight was measured by scales with a precision of ±500 g, and height was measured by a stadiometer with a precision of 0.5 cm (SECA model 220, Hamburg German.). BMI was calculated according to the formula: BMI = weight (kg)/height2 (m). BMI values of 18.5, 25 and 30 were used to categorise women into lean, normal weight, overweight and obese, respectively [16]. Approval of the local ethics committee was obtained for the original studies from which the data of the present study were extracted for statistical analyses.
Statistics
All continuous variables are expressed as mean ± standard deviation of the mean. The unpaired t-test was performed to test hypotheses about means of different groups. When the Levene test for homogeneity of variances was significant (P < 0.05) the Mann–Whitney test was used to check t-test results. Pearson’s correlation test was used to measure the correlation between continuous variables. Pearson’s chi square test was performed to investigate the relationships between grouping variables. Logistic regression was performed as multivariate analysis to test the ability of the independent variable BMI to distinguish subjects with each one of the osteoporotic fracture group from those without fracture, with age, age at menopause and FN BMD used as covariates. BMI was tested both as a continuous and as a categorical variable after being divided into four categories (lean, normal weight, overweight, and obese). Normal weight women were used as a reference category and the effects of the other categories were expressed in comparison with the reference. The odds ratio (OR) and 95% confidence interval (CI) were calculated for each logistic regression with the Wald statistic.
Results
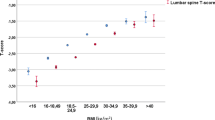
The total sample of 2,235 women included 1,629 women without fractures, 187 with hip fracture, 85 with humerus fracture, 226 with wrist fracture, and 108 with ankle fracture. According to the BMI categories there were 84 lean women, 1,215 normal weight, 727 overweight, and 209 obese women. Fracture distribution according to the BMI categories is reported in Table 1 together with the comparison of the fracture rate between the normal weight subjects and each one of the other BMI groups. The hip fracture rate was significantly higher (Pearson’s chi square test: P < 0.001) in lean women and significantly lower in obese ones (Pearson’s chi square test: P < 0.05) than in normal weight ones. Humerus fracture rate was significantly higher in obese women (Pearson’s chi square test: P < 0.05) than in normal weight women. In wrist and ankle fractures there were no statistically significant differences in fracture distribution among BMI categories.
Table 2 shows the relevant characteristics of the whole study population by grouping women according to the absence of fractures or their types. Women without fracture were significantly younger and had higher BMD than those of each fracture group. They also had a significantly higher BMI than those with hip fracture. There were no statistically significant differences between women with fractures compared to those without fractures with regards to age at menopause. Statistical significances did not change after age correction of the data.
Age was inversely correlated with BMD (R = −0.399, P < 0.0001). A positive correlation was found between BMI and BMD (R = 0.262, P < 0.0001).
Table 3 shows logistic regression in which BMI, considered as a continuous variable and adjusted for possible confounders (age, age at menopause and FN BMD), significantly discriminated subjects with hip fracture: OR 0.949 (95% CI, 0.900–0.999) and humerus fracture: OR 1.077 (95% CI, 1.017–1.141) from those without fracture, while it did not discriminate wrist and ankle fracture from not-fractured women.
Table 4 shows logistic regression, in which BMI is considered as a categorical variable, and adjusted for the possible confounders. In this case leanness significantly predicted hip fracture OR 3.819 (95% CI, 2.035–7.168), while overweight and obesity lacked significance in discriminating hip fracture in comparison with normal weighted women.
Obesity significantly predicted humerus fracture: OR 3.481(95% CI, 1.815–6.678), while overweight and leanness lacked significance in discriminating humerus fractures in comparison with normal weight women. No statistically significant associations between BMI categories and fracture risk were found by logistic regression for wrist and ankle fracture.
Discussion
In this study we assessed the relationship of BMI with the risk of the main osteoporotic limb fractures, regardless of age and BMD. As a preliminary observation we found, as expected, that the risk of each of the considered fractures had a significant inverse correlation with BMD and a direct correlation with age, in agreement with the literature [17–19]. Testing the BMI as a continuous variable in logistic regression, we found that its increase, regardless of BMD, age and age at menopause, carried a greater risk for humerus fracture [6, 20], but had a protective effect against hip fracture [9, 21–23], albeit, in the latter case, at borderline significance. In wrist and ankle fractures BMI did not discriminate subjects with from those without fracture, in agreement with some authors but in disagreement with others [3, 12, 24–26]. These data indicate that BMI has, regardless of BMD, different relationships with fracture risk according to different fracture types [13]; decreasing BMI increases the risk for hip fracture, whereas increasing BMI increases the risk for humerus fracture.
Since clinicians treating obesity-related metabolic diseases or anorexia may be interested to know how the fracture risk changes with the variation of the patients’ weight, from obesity or leanness to normal weight, we also analysed the BMI-related fracture risk after categorising the women’s BMI according to the WHO [16] classification, which is generally accepted for clinical and research purposes.
We found that lean women, regardless of age, age at menopause and BMD, effectively have a significantly higher risk of hip fracture than normal weight women, while the risk in obese women is not significantly different from that of normal weight ones. This suggests that the hip fracture protective effect of the increasing BMI, when considered as continuous variable, is more likely to be due to the increased fracture risk of lean people than to a real reduction of the fracture risk in obese ones. It also suggests that the lower hip fracture rate in obese women compared to normal weight ones is BMD-mediated because of the relationship between these two variables [27, 28]. Our data, therefore, show that obesity is not, per se, a safer condition for hip fracture prevention than normal weight, in agreement with other authors [29], and that leanness is the true age-BMD independent risk condition that needs to be corrected to reduce the fracture risk [29]. The reasons why leanness is an age-BMD independent risk factor for hip fracture have already been studied. These reasons include: muscle weakness [30], that increases the propensity to fall [31], while, at the same time, reduces protection during a fall; and insufficient protective padding around the hip [32]. In fact, concerning the latter reason, falls with impact on the side of the legs or directly on the hip are strongly related with proximal femur fractures [33, 34].
Propensity to fall has also been considered as a fracture risk for humerus fracture, as up to 97% of humerus fractures in the elderly follow a fall [35, 36]. Nevertheless, contrary to hip fractures, in humerus fractures we found that obese women have a more than three times higher risk of humerus fracture than normal weight ones, regardless of age and BMD, in disagreement with some [7] and in agreement with other authors [6]. The increased postural instability in obese subjects and their inaccuracy when performing rapid movements [37, 38] predisposes them to an increased propensity to fall [39] and might explain the BMD-independent association of obesity with humerus fracture risk. Our results suggest therefore that obesity-related falls are a main risk factor for humerus fracture, while leanness is not a safer condition than normal weight. Nevertheless, in addition to the obesity-related tendency to fall, also the way of falling and the absorption of impact forces at the arm level should be considered as factors implicated in the humerus fracture [40], as, unlike humerus fracture, the risk of wrist fracture, which also often follows a fall, did not show any association with BMI in our population. Differences in the fall direction and in the attempt to break the fall (less frequent in humerus fracture) are in fact reported as factors favouring the occurrence of wrist rather than humerus fracture after a fall [35].
The lack of the full range assessment of fracture risk factors certainly is a weakness in our study that, in addition, is cross-sectional. This kind of study design may have limited the certainty of our results compared with those of prospective cohort studies showing the association of poor nutrition with the humerus fracture risk [7, 8] or with the risk of major osteoporotic fracture, including humerus fracture [41]. The older age of subjects in these studies compared with the subject’s ages of those studies that find that humerus fracture risk is obesity related [6, 20], together with differences in race, ethnicity and study design among these studies, might explain discrepancies among authors on this topic. The fact that both direct [6, 20] and inverse relationship [7, 8, 41] between BMI/weight and humerus fracture risk have been reported, might finally suggest that there are two different relationships of BMI with humerus fracture risk in different sub-groups of the population, as already proposed by Holmberg and Coho workers [20]. Our study has other weaknesses: BMI at the measurement time might not be exactly that of the fracture time; our sample was not population based and the study was not prospective, so our result might not have universal validity in the community-dwelling population. However, data seem to indicate that BMI has different relationships with the risk of hip or humerus fragility fracture in postmenopausal women; lean women have a significantly higher risk of hip fracture and obese women have a significantly higher risk of humerus fracture compared with those with normal body weight. Our findings also suggest that there are no BMI categories that protect against these fragility fractures compared to that of normal body weight after adjusting for BMD and age. Further studies are needed to confirm these data.
References
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312:1254–1259
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332:767–773
Porthouse J, Birks YF, Torgerson DJ, Cockayne S, Puffer S, Watt I (2004) Risk factors for fracture in a UK population: a prospective cohort study. QJM 97:569–574
Gunnes M, Lehmann EH, Mellstrom D, Johnell O (1996) The relationship between anthropometric measurements and fractures in women. Bone 19:407–413
Huang Z, Himes JH, McGovern PG (1996) Nutrition and subsequent hip fracture risk among a national cohort of white women. Am J Epidemiol 144:124–134
Chu SP, Kelsey JL, Keegan TH, Sternfeld B, Prill M, Quesenberry CP, Sidney S (2004) Risk factors for proximal humerus fracture. Am J Epidemiol 160:360–367
Kelsey JL, Browner WS, Seeley DG, Nevitt MC, Cummings SR (1992) Risk factors for fractures of the distal forearm and proximal humerus. The Study of Osteoporotic Fractures Research Group. Am J Epidemiol 135:477–489
Nguyen TV, Center JR, Sambrook PN, Eisman JA (2001) Risk factors for proximal humerus, forearm, and wrist fractures in elderly men and women: the Dubbo Osteoporosis Epidemiology Study. Am J Epidemiol 153:587–595
Margolis KL, Ensrud KE, Schreiner PJ, Tabor HK (2000) Body size and risk for clinical fractures in older women. Study of Osteoporotic Fractures Research Group. Ann Intern Med 133:123–127
Joakimsen RM, Fønnebø V, Magnus JH, Tollan A, Søgaard AJ (1998) The Tromsø Study: body height, body mass index and fractures. Osteoporos Int 8:436–442
Honkanen RJ, Honkanen K, Kröger H, Alhava E, Tuppurainen M, Saarikoski S (2000) Risk factors for perimenopausal distal forearm fracture. Osteoporos Int 11:265–270
Seeley DG, Kelsey J, Jergas M, Nevitt MC (1996) Predictors of ankle and foot fractures in older women. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 11:1347–1355
Honkanen R, Tuppurainen M, Kröger H, Alhava E, Saarikoski S (1998) Relationships between risk factors and fractures differ by type of fracture: a population-based study of 12, 192 perimenopausal women. Osteoporos Int 8:25–31
Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE, Hennekens CH, Speizer FE (1995) Body weight and mortality among women. N Engl J Med 333:677–685
Gnudi S, Sitta E (2005) Clinical risk factor evaluation to defer postmenopausal women from bone mineral density measurement: an Italian study. J Clin Densitom 8:199–205
WHO, World Health Organization (2000) Obesity: preventing and managing the global epidemic. WHO Technical Report Series 894. Geneva, Switzerland
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1936
Nguyen ND, Eisman JA, Center JR, Nguyen TV (2007) Risk factors for fracture in nonosteoporotic men and women. J Clin Endocrinol Metab 92:955–962
Blake GM, Fogelman I (2007) The role of DXA bone density scans in the diagnosis and treatment of osteoporosis. Postgrad Med J 83:509–517
Holmberg AH, Johnell O, Nilsson PM, Nilsson J, Berglund G, Akesson K (2006) Risk factors for fragility fracture in middle age. A prospective population-based study of 33,000 men and women. Osteoporos Int 17:1065–1077
van der Voort DJ, Geusens PP, Dinant GJ (2001) Risk factors for osteoporosis related to their outcome: fractures. Osteoporos Int 12:630–638
Ensrud KE, Lipschutz RC, Cauley JA, Seeley D, Nevitt MC, Scott J, Orwoll ES, Genant HK, Cummings SR (1997) Body size and hip fracture risk in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Am J Med 103:274–280
Meyer HE, Tverdal A, Falch JA (1995) Body height, body mass index, and fatal hip fractures: 16 years’ follow-up of 674,000 Norwegian women and men. Epidemiology 6:299–305
Mallmin H, Ljunghall S, Persson I, Bergström R (1994) Risk factors for fractures of the distal forearm: a population-based case-control study. Osteoporos Int 4:298–304
Valtola A, Honkanen R, Kröger H, Tuppurainen M, Saarikoski S, Alhava E (2002) Lifestyle and other factors predict ankle fractures in perimenopausal women: a population-based prospective cohort study. Bone 30:238–242
White SC, Atchison KA, Gornbein JA, Nattiv A, Paganini-Hill A, Service SK (2006) Risk factors for fractures in older men and women: The Leisure World Cohort Study. Gend Med 3:110–123
Felson DT, Zhang Y, Hannan MT, Anderson JJ (1993) Effects of weight and body mass index on bone mineral density in men and women: the Framingham study. J Bone Miner Res 8:567–573
Ribot C, Trémollières F, Pouillès JM (1994) The effect of obesity on postmenopausal bone loss and the risk of osteoporosis. Adv Nutr Res 9:257–271
De Laet C, Kanis JA, Odén A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, McCloskey EV, Mellstrom D, Melton LJ 3rd, Meunier PJ, Pols HA, Reeve J, Silman A, Tenenhouse A (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16:1330–1338
Bischoff HA, Stähelin HB, Dick W, Akos R, Knecht M, Salis C, Nebiker M, Theiler R, Pfeifer M, Begerow B, Lew RA, Conzelmann M (2003) Effects of vitamin D and calcium supplementation on falls: a randomised controlled trial. J Bone Miner Res 18:343–351
Willig R, Luukinen H, Jalovaara P (2003) Factors related to occurrence of hip fracture during a fall on the hip. Public Health 117:25–30
Nilsson BE (1970) Spinal osteoporosis and femoral neck fracture. Clin Orthop Relat Res 68:93–95
Wei TS, Hu CH, Wang SH, Hwang KL (2001) Fall characteristics, functional mobility and bone mineral density as risk factors of hip fracture in the community-dwelling ambulatory elderly. Osteoporos Int 12:1050–1055
Hayes WC, Myers ER, Morris JN, Gerhart TN, Yett HS, Lipsitz LA (1993) Impact near the hip dominates fracture risk in elderly nursing home residents who fall. Calcif Tissue Int 52:192–198
Palvanen M, Kannus P, Parkkari J, Pitkäjärvi T, Pasanen M, Vuori I, Järvinen M (2000) The injury mechanisms of osteoporotic upper extremity fractures among older adults: a controlled study of 287 consecutive patients and their 108 controls. Osteoporos Int 11:822–831
Court-Brown CM, Garg A, McQueen MM (2001) The translated two-part fracture of the proximal humerus. Epidemiology and outcome in the older patient. J Bone Joint Surg Br 83:799–804
Hue O, Simoneau M, Marcotte J, Berrigan F, Doré J, Marceau P, Marceau S, Tremblay A, Teasdale N (2007) Body weight is a strong predictor of postural stability. Gait Posture 26:32–38
Berrigan F, Simoneau M, Tremblay A, Hue O, Teasdale N (2006) Influence of obesity on accurate and rapid arm movement performed from a standing posture. Int J Obes 30:1750–1757
Corbeil P, Simoneau M, Rancourt D, Tremblay A, Teasdale N (2001) Increased risk for falling associated with obesity: mathematical modeling of postural control. IEEE Trans Neural Syst Rehabil Eng 9:126–136
Chiu J, Robinovitch SN (1998) Prediction of upper extremity impact forces during falls on the outstretched hand. J Biomech 31:1169–1176
Kanis JA A, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397
Acknowledgments
We would like to thank Mr Keith Smith for his assistance in revising the manuscript and Mrs Elettra Pignotti for statistical analysis.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Gnudi, S., Sitta, E. & Lisi, L. Relationship of body mass index with main limb fragility fractures in postmenopausal women. J Bone Miner Metab 27, 479–484 (2009). https://doi.org/10.1007/s00774-009-0056-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-009-0056-8