Abstract
There is evidence for a genetic contribution to bone mineral density (BMD×). Different loci affecting BMD have been identified by diverse linkage and genome-wide association studies. We studied the heritability of and the correlations among six densitometric phenotypes and four bone mass/fracture phenotypes. For this purpose, we used a family-based study of the genetics of osteoporosis, the Genetic Analysis of Osteoporosis Project. The primary aim of our study was to examine the roles of genetic and environmental factors in determining osteoporosis-related phenotypes. The project consisted of 11 extended families from Spain. All of them were selected through a proband with osteoporosis. BMD was measured using dual-energy X-ray absorptiometry. The proportion of variance of BMD attributable to significant covariates ranged from 25 % (for femoral neck BMD) to 48 % (for whole-body total BMD). The vast majority of the densitometric phenotypes had highly significant heritability, ranging from 0.252 (whole-body total BMD) to 0.537 (trochanteric BMD) after correcting for covariate effects. All of the densitometric phenotypes showed high and significant genetic correlations (from −0.772 to −1.000) with a low bone mass/osteopenia condition (Affected 3). Our findings provide additional evidence on the heritability of BMD and a strong genetic correlation between BMD and bone mass/fracture phenotypes in a Spanish population. Our results emphasize the importance of detecting genetic risk factors and the benefit of early diagnosis and especially therapeutic and preventive strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is one of the world’s most significant health issues and inflicts substantial social, economic, and clinical burdens [1]. It is a common systemic skeletal disorder characterized by low bone mass and microarchitectural deterioration of bone tissue, resulting in increased bone fragility and susceptibility to fracture, usually hip, vertebral, and wrist [2]. It has been estimated that osteoporosis affects 200 million people worldwide [3] and that over 9 million osteoporotic fractures occur every year [4].
The diagnosis of osteoporosis and the assessment of fracture risk are based on the measurement of bone mineral density (BMD) [5]. There are various causes of osteoporotic fractures, but the most important is low BMD. Since low BMD is a risk factor for fracture, therapeutic decisions to prevent fracture are based often on BMD measurements. Thus, for effective prevention of osteoporosis, it is necessary to identify factors involved in determining BMD.
There is strong evidence that genetic factors contribute to osteoporosis risk, such as BMD, bone turnover markers, as well as structural and strength properties of the hip [4, 6–11]. Also, there is significant evidence from studies of peak bone mass that genes contribute to the variation of BMD. At older ages, a large genetic contribution to BMD has been also demonstrated [12]. Environmental factors such as physical activity, lifestyle, and calcium intake may affect BMD also [13–15].
Thus, it is clear that risk of osteoporosis depends upon genetic and environmental factors acting jointly. With recent advances in genetics and epidemiology it is possible to quantify the genetic determinants of osteoporosis. The data indicate that 60–90 % of BMD variation can be explained by genetic factors [16, 17]. In addition, there is evidence for a genetic contribution to BMD, and different loci affecting BMD have been identified by diverse linkage [18–20] and genome-wide association studies [21]. Furthermore, variance component analysis increases the statistical power of genetic studies on families with extensive genealogy. For this reason, we designed a family-based study of the genetics of osteoporosis, the Genetic Analysis of Osteoporosis (GAO) Project. We studied a sample of extended families ascertained through individuals with osteoporosis. The primary aim of our study was to examine the relative roles of genetic and environmental factors in determining osteoporosis-related phenotypes.
Methods
The GAO Project included 11 extended families from Spain. We selected these families primarily on the basis of pedigree size, to maximize the statistical power of detecting genetic effects. In particular, to be included in the project, a family had to have at least 10 living individuals distributed in three or more generations. The structure of the families was verified by use of microsatellite genotyping and control for Mendelian inconsistencies [22]. Large pedigrees have comparably more power per sampled individual than small families, partially compensating for small sample sizes [23].
The enrollment period for our study was between March 2009 and March 2012. All of the families were selected through a proband with osteoporosis, which was defined as (1) hip neck, total hip, or spine BMD yielding a T score <−2.5 or (2) the occurrence of at least one osteoporotic fracture in subjects over 21 years of age.
A medical history was obtained from all of the participants. It included menstrual period, history of all clinical fractures (traumatic and nontraumatic), and current medications with a negative (e.g., corticoids, heparin, proton pump inhibitors, insulin, or thiazolidinediones) or a positive (e.g., bisphosphonates, calcium, strontium, parathyroid hormone, thiazide diuretics, vitamin D) effect on bone remodeling. Coffee, alcohol, and smoking habits; dietary calcium intake; sun exposure; and physical activity were recorded also. The questionnaire and definitions are available in the Appendix.
The ethics committee of our institution approved all recruitment protocols (08/015/281). Adult subjects gave informed consent for themselves and for their minor family members.
Spine, femur, and whole-body dual-energy X-ray absorptiometry (DXA) scans were performed on all participants using a Discovery DXA system with APEX v2.3 software (Hologic, Bedford, MA, USA), following the manufacturer’s recommendations. The measurement of total-hip BMD is a conglomerate of femoral neck, trochanteric, Ward’s triangle, and other components. To analyze strength and geometrical properties of the hip, we used the hip structural analysis software included in APEX. Scans were performed and reviewed by the same technician and physician, both of them certified by the International Society for Clinical Densitometry. Our study focused on six densitometric phenotypes that we considered clinically relevant. Table 1 contains a description of the phenotypes as well as a guide for the abbreviations.
Apart from the six osteoporosis-related quantitative traits mentioned previously, we studied also four categorical phenotypes of particular clinical interest:
-
1.
Phenotype “Affected 1,” corresponding to low bone mass according to the most common definition of osteoporosis; it included individuals ≥21 years old who presented one or more of the following characteristics: (1) T score ≤−2.5 (column, hip neck, or total hip), (2) at least one osteoporotic (nontraumatic) fracture, (3) antiresorptive or forming agent treatment.
-
2.
Phenotype “Affected 2,” corresponding to patients who suffered at least one osteoporotic fracture.
-
3.
Phenotype “Affected 3,” corresponding to a broad spectrum of skeletal conditions, encompassing (1) “Affected 1” individuals and (2) patients with a T score ≤−1 (column, hip neck, or total hip).
-
4.
Phenotype “Affected 4,” corresponding to an extension of “Affected 1” as it includes also individuals <21 years old who presented Z scores ≤−2.5 (column, hip neck, or total hip).
We checked the 11 pedigrees for Mendelian inconsistencies with FBAT v2.0.3 [24], and we corrected most of them by genotyping. However, in two family branches involving nine individuals, we discovered systematic inconsistencies for more than one microsatellite marker, so those participants were excluded from our study [22].
For usual statistical analysis, SPSS 21 software was used (SPSS, Chicago, IL, USA).
We used a variance component analysis to determine the contribution of genetic and individual-specific environmental factors to the variation of intermediate (i.e., quantitative traits) and final (i.e., status) osteoporotic phenotypes in the GAO pedigrees.
We modeled the level of a trait y for individual i (y i ) as a linear function as follows:
where μ is the trait mean, x ij is the jth covariate and β j is its regression coefficient.
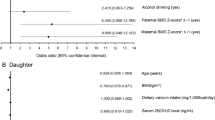
Covariates included age, age2, gender, body mass index (BMI), age at menopause for postmenopausal women, alcohol intake, smoking, and use of osteoporosis-related medication, as well as interactions of age and age2 with gender. Age-related covariates were scaled so that their regression coefficients represented the effect produced by a 10-year deviation from the mean age. Discrete covariates (gender, alcohol intake, and smoking) were scaled so that regression coefficients represented the effect of the covariate presence versus absence. A special case is the use of osteoporosis-related medication, which was scaled so that its regression coefficient represented a positive, negative, or no effect of the covariate.
The remaining variables, g i and e i , represent the random deviations from μ for individual i that are attributable to additive genetic and residual error effects, respectively. The residual error component included true random error, measurement error, and any nonadditive genetic components. The effects of g i and e i were assumed to be not correlated with one another and normally distributed with mean = 0 and variances σ 2g and σ 2e . The likelihood of the phenotypes of the family members is assumed to follow a multivariate normal distribution with a phenotypic covariance matrix that is a function of the kinship between individuals and the additive genetic and environmental variances.
We used the maximum-likelihood methods implemented in SOLAR v4.3.1 [23] to estimate simultaneously the mean and variances, as well as the covariate and genetic effects, for each trait. We assessed the significance of such effects with a likelihood-ratio test [25, 26]. Finally, we estimated the heritability for each trait as the proportion of the total phenotypic variability attributable to additive genetic effects. For this particular estimation, we considered only environmental covariates (i.e., we performed the analysis without BMI and age at menopause for postmenopausal women).
To study the genetic relationships between status phenotypes and quantitative variation in osteoporosis-related intermediate phenotypes, we used a modified variance component method for mixed discrete/continuous traits [27] incorporated in SOLAR. This method allowed for the phenotypic correlations between pairs of traits to be separated into common genetic influences and common environmental influences. The separation of phenotypic correlations (ρ p) into genetic (ρ g) and environmental (ρ e) components is a valuable tool because it reveals hidden relationships among traits [28].
Results
We enrolled 681 individuals from the 11 extended families. Once we excluded the deaths, children of early age (<5 years), and individuals with incomplete data or who we were unable to recruit, there remained 376 individuals available for the study. Finally, another 9 of the 376 subjects were excluded due to Mendelian inconsistencies, yielding a final sample size of 367 individuals.
The general characteristics of the 11 pedigrees as well as those of the probands used for recruitment are described in Table 2. Sample size per family ranged from 15 to 91, and the male to female gender ratio was 1.07. The ages ranged from 5 to 93 years (median 41). Moreover, the age of the 11 probands ranged from 40 to 89, and only one of the probands was male, while three probands presented multiple osteoporotic fractures. The total number of individuals with osteoporotic fractures in the cohort was 24 (6.5 % of the total sample size). Their distribution in the 11 pedigrees was nonrandom: 14 fractures occurred in families 1, 3, and 11, whereas no fractures were reported in families 4 and 8.
The covariates that had significant effects on BMD (p < 0.05) appear in Table 3. From the covariates that were initially included in the model, smoking and use of osteoporosis-related medication did not have any significant effect on the final phenotypes and, therefore, are not shown. Alcohol consumption was dichotomized between two groups: no consumption plus low consumption (group 0) and consumption above 30 g/day (group 1), even though there was no significant correlation with BMD. The rest of the environmental covariates collected and described in the Appendix did not show significant correlation. Table 3 shows the proportion of variance of BMD that is attributed to significant covariates, ranging from 25 % (for NeckBMD) to 48 % (for WBtotBMD).
The heritability of each of the densitometric phenotypes is shown in Table 4 and is based on the most parsimonious model of variance component analysis for each phenotype, including only significant sources of variation. The remaining variance not accounted for in Table 4 is attributable to random individual-specific environmental influences and random error. All of the results were statistically significant (p < 0.05). The spine and hip densitometric scans of two participants were excluded due to previous bilateral total hip replacement surgery and vertebral fractures.
The vast majority of the densitometric phenotypes showed highly significant heritability, ranging from 0.252 (WBTotBMD) to 0.537 (TrochBMD) after correcting for covariate effects.
Heritability of the phenotype (Affected 1–4) was generally higher when compared to the six quantitative traits. We observed a heritability of 0.501 for osteoporosis (Affected 1), whereas the highest heritability (0.827) was observed for both osteoporotic fractures (Affected 2) and a compound status condition including osteoporosis and low bone mass (Affected 3).
Table 5 shows the correlation of each of the six densitometric traits with the four different status phenotypes on the phenotypic (ρ P), genetic (ρ G), and environmental (ρ E) levels. In general terms, the phenotypic correlation can be considered the result of the mathematical combination of genetic and environmental correlation. Any correlation ≥0.70 was considered strong (Table 5). The majority of the correlations were negative.
The most significant correlations were observed on the genetic level (Table 5). We observed the highest correlations for TrochBMD (from −0.704 to −0.891), with three different status phenotypes (Affected 1, 3, and 4). Moreover, all densitometric phenotypes showed high and significant genetic correlations (from −0.772 to −1.000) with low bone mass/osteoporotic condition (Affected 3). Few high and significant correlations were observed on the environmental level and none on the total phenotypic level. The highest correlations on the environmental level were identified between Affected1 and NeckBMD (−0.692) and between Affected4 and NeckBMD (−0.726).
Discussion
The aim of the GAO Project, based on extended pedigrees, is to examine the role of genetic and environmental factors in determining osteoporosis-related phenotypes. One of the most important advantages of our study design is the extent and variety of phenotypic traits that we included. In contrast, most studies have examined a relatively low number of phenotypes. Our results include six quantitative phenotypes and four status phenotypes, all of them highly relevant clinically.
From the covariates that were initially included in our model, a statistically significant correlation with mineral density traits was observed for females, age, BMI, and age at menopause. The variance explained by these covariates ranged from 0.25 to 0.48. These findings are in accordance with previous data [18, 29–36]. The correlation of age and BMD was surprisingly positive. It has to be taken into account that in our sample one-third of the population was younger than 30 years (before peak bone mass is reached), and it is known that the projected area of the spine in children’s DXA can be lower than reality. Moreover, about 10 % of the population was older than 70 years, and the spinal degenerative changes in these patients could interfere with an accurate estimation of BMD, leading to overestimation.
The status phenotypes were significantly influenced by age and BMI, with age exerting a negative and BMI exerting a positive influence. High BMD was related to young age and high BMI. These results agree with those from other studies [35]. This relation was not present in Affected 2 (osteoporotic fracture), possibly due to the small sample and homogeneity of the age of patients with fractures.
In our study, the estimates of heritability of mineral density traits and phenotype status were clearly significant. Our estimates of heritability were generally lower than those reported elsewhere [6, 37], which could be explained by the fact that our study used family data. It is well known that family-based designs provide more conservative estimates of heritability compared to linkage [18, 20, 30, 31, 37–39] and genome-wide association [21]. Another possible explanation for the low h 2 values could be that children were included in our sample. When we analyzed the heritability of different phenotypic statuses, we obtained estimates that were higher (50–82 %) than those observed in other studies, although another study found that osteoporotic fracture had a lower heritability for wrist (54 %) and hip (68 %) in perimenopausal women [40]. These data cannot be compared directly to our data because of the heterogeneity of classification of fractures. The reviews carried out in genome-wide association studies for fractures concluded that many limitations exist in these results because the genetics of fracture risk is poorly understood, and much progress is likely to be made through the dissection of fracture risk, independently of BMD [21].
To our knowledge, our study is the largest Spanish family study to examine genetic correlations between various pairs of BMD traits (measured at different body sites) and phenotype status. We observed strong and significant genetic correlations between diverse BMD traits and statuses, especially Affected 3. Other studies have examined the relation between BMD traits at two different sites (demonstrating high heritability [>0.5], much higher than the environmental contribution [9, 34, 37, 41, 42]).
We found that the lowest genetic correlation of densitometric BMD traits was with the Affected 2 phenotype (presence of fractures), probably reflecting the fact that fractures depend less on genetic than on environmental factors. This information has been reflected in diverse studies [21, 41]. Our study confirms that genetic variants contributing to the low bone mass do not appear to influence the risk of fracture. As a consequence, there is a need to investigate other genetic loci that could influence osteoporotic fractures independently from BMD [41, 43].
One of the strengths of our study is its design, based on the analysis of extended pedigrees, which may better estimate the genetic influences than other studies. For example, twin studies tend to overestimate the genetic contribution to the phenotype because environmental factors are more likely to be shared between twins than between nontwin siblings [38, 39]. At the same time, the inclusion of many members of the same family makes the separation of genetic from common environmental effects more challenging [30].
The strong genetic influences on BMD and status observed in our population provide a strong motivation for pursuing gene-mapping strategies, such as genome-wide linkage and association analyses. Recently, genome-wide association studies have had considerable success in identifying replicated loci that are associated with low bone mass and osteoporotic fractures [21].
In conclusion, our findings provide additional evidence of the statistically significant heritability of and strong genetic correlation between BMD and phenotypes status in a Spanish population. Our results emphasize the importance of detecting risk factors as well as developing early diagnosis for therapeutic and preventive strategies.
References
Oden A, McCloskey EV, Johansson H, Kanis JA (2013) Assessing the impact of osteoporosis on the burden of hip fractures. Calcif Tissue Int 92(1):42–49
Kanis J (1997) Diagnosis of osteoporosis. Osteoporos Int 7(3):S108–S116
Lin JT, Lane JM (2004) Osteoporosis: a review. Clin Orthop Relat Res 425:126–134
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22(3):465–475
Watts NB (2004) Fundamentals and pitfalls of bone densitometry using dual-energy X-ray absorptiometry (DXA). Osteoporos Int 15(11):847–854
Arden NK, Baker J, Hogg C, Baan K, Spector TD (1996) The heritability of bone mineral density, ultrasound of the calcaneus and hip axis length: a study of postmenopausal twins. J Bone Miner Res 11(4):530–534
Hunter DJ, de Lange M, Andrew T, Snieder H, MacGregor AJ, Spector TD (2001) Genetic variation in bone mineral density and calcaneal ultrasound: a study of the influence of menopause using female twins. Osteoporos Int 12(5):406–411
Kaprio J, Rimpela A, Winter T, Viken RJ, Rimpela M, Rose RJ (1995) Common genetic influences on BMI and age at menarche. Hum Biol 67(5):739–753
Nguyen TV, Blangero J, Eisman JA (2000) Genetic epidemiological approaches to the search for osteoporosis genes. J Bone Miner Res 15(3):392–401
Snieder H, MacGregor AJ, Spector TD (1998) Genes control the cessation of a woman’s reproductive life: a twin study of hysterectomy and age at menopause. J Clin Endocrinol Metab 83(6):1875–1880
Zintzaras E, Doxani C, Koufakis T, Kastanis A, Rodopoulou P, Karachalios T (2011) Synopsis and meta-analysis of genetic association studies in osteoporosis for the focal adhesion family genes: the CUMAGAS-OSTEOporosis information system. BMC Med 26(9):9
Styrkarsdottir U, Cazier JB, Kong A, Rolfsson O, Larsen H, Bjarnadottir E et al (2003) Linkage of osteoporosis to chromosome 20p12 and association to BMP2. PLoS Biol 1(3):E69
Berard A, Bravo G, Gauthier P (1997) Meta-analysis of the effectiveness of physical activity for the prevention of bone loss in postmenopausal women. Osteoporos Int 7(4):331–337
Simkin A, Ayalon J, Leichter I (1987) Increased trabecular bone density due to bone-loading exercises in postmenopausal osteoporotic women. Calcif Tissue Int 40:59–63
Kiel DP, Zhang Y, Hannan MT, Anderson JJ, Baron JA, Felson DT (1996) The effect of smoking at different life stages on bone mineral density in elderly men and women. Osteoporos Int 6(3):240–248
Nguyen TV, Howard GM, Kelly PJ, Eisman JA (1998) Bone mass, lean mass, and fat mass: same genes or same environments? Am J Epidemiol 147(1):3–16
Peacock M, Turner CH, Econs MJ, Foroud T (2002) Genetics of osteoporosis. Endocr Rev 23(3):303–326
Ralston SH, Uitterlinden AG (2010) Genetics of osteoporosis. Endocr Rev 31(5):629–662
Peacock M, Koller DL, Lai D, Hui S, Foroud T, Econs MJ (2009) Bone mineral density variation in men is influenced by sex-specific and non sex-specific quantitative trait loci. Bone 45(3):443–448
Xiao P, Shen H, Guo YF, Xiong DH, Liu YZ, Liu YJ, Zhao LJ, Long JR, Guo Y, Recker RR, Deng HW (2006) Genomic regions identified for BMD in a large sample including epistatic interactions and gender-specific effects. J Bone Miner Res 21(10):1536–1544
Richards JB, Zheng HF, Spector TD (2012) Genetics of osteoporosis from genome-wide association studies: advances and challenges. Nat Rev Genet 13(8):576–588
Athanasiadis G, Malouf J, Hernandez-Sosa N, Martin-Fernandez L, Catalan M, Casademont J, Soria JM (2014) Linkage and association analyses using families identified a locus affecting an osteoporosis-related trait. Bone 60:98–103
Blangero J, Almasy L (1997) Multipoint oligogenic linkage analysis of quantitative traits. Genet Epidemiol 14(6):959–964
Laird NM, Horvath S, Xu X (2000) Implementing a unified approach to family-based tests of association. Genet Epidemiol 19(1):S36–S42
Kendall M, Stuart A (1972) Advanced theory of statistics. Hafner, New York
Self SG, Liang KY (1987) Asymptotic properties of maximum likelihood estimators and likelihood ratio tests under non-standard conditions. J Am Stat Assoc 82:605–610
Williams JT, Duggirala R, Blangero J (1997) Statistical properties of a variance components method for quantitative trait linkage analysis in nuclear families and extended pedigrees. Genet Epidemiol 14(6):1065–1070
Comuzzie AG, Blangero J, Mahaney MC, Haffner SM, Mitchell BD, Stern MP et al (1996) Genetic and environmental correlations among hormone levels and measures of body fat accumulation and topography. J Clin Endocrinol Metab 81(2):597–600
Duncan EL, Cardon LR, Sinsheimer JS, Wass JA, Brown MA (2003) Site and gender specificity of inheritance of bone mineral density. J Bone Miner Res 18(8):1531–1538
Naganathan V, Macgregor A, Snieder H, Nguyen T, Spector T, Sambrook P (2002) Gender differences in the genetic factors responsible for variation in bone density and ultrasound. J Bone Miner Res 17(4):725–733
Orwoll ES, Belknap JK, Klein RF (2001) Gender specificity in the genetic determinants of peak bone mass. J Bone Miner Res 16(11):1962–1971
Kammerer CM, Schneider JL, Cole SA, Hixson JE, Samollow PB, O’Connell JR et al (2003) Quantitative trait loci on chromosomes 2p, 4p, and 13q influence bone mineral density of the forearm and hip in Mexican Americans. J Bone Miner Res 18(12):2245–2252
Karasik D, Hsu YH, Zhou Y, Cupples LA, Kiel DP, Demissie S (2010) Genome-wide pleiotropy of osteoporosis-related phenotypes: the Framingham Study. J Bone Miner Res 25(7):1555–1563
Yang TL, Zhao LJ, Liu YJ, Liu JF, Recker RR, Deng HW (2006) Genetic and environmental correlations of bone mineral density at different skeletal sites in females and males. Calcif Tissue Int 78(4):212–217
Mitchell BD, Kammerer CM, Schneider JL, Perez R, Bauer RL (2003) Genetic and environmental determinants of bone mineral density in Mexican Americans: results from the San Antonio Family Osteoporosis Study. Bone 33(5):839–846
Videman T, Levälahti E, Battié MC, Simonen R, Vanninen E, Kaprio J (2007) Heritability of BMD of femoral neck and lumbar spine: a multivariate twin study of Finnish men. J Bone Miner Res 22(9):1455–1462
Park JH, Song YM, Sung J, Lee K, Kim YS, Park YS (2012) Genetic influence on bone mineral density in Korean twins and families: the healthy twin study. Osteoporos Int 23(4):1343–1349
Slemenda CW, Christian JC, Williams CJ, Norton JA, Johnston CC (1991) Genetic determinants of bone mass in adult women: a reevaluation of the twin model and the potential importance of gene interaction on heritability estimates. J Bone Miner Res 6(6):561–567
Tse KY, Macias BR, Meyer RS, Hargens AR (2009) Heritability of bone density: regional and gender differences in monozygotic twins. J Orthop Res 27(2):150–154
Andrew T, Antioniades L, Scurrah KJ, Macgregor AJ, Spector TD (2005) Risk of wrist fracture in women is heritable and is influenced by genes that are largely independent of those influencing BMD. J Bone Miner Res 20(1):67–74
Deng FY, Lei SF, Li MX, Jiang C, Dvornyk V, Deng HW (2006) Genetic determination and correlation of body mass index and bone mineral density at the spine and hip in Chinese Han ethnicity. Osteoporos Int 17(1):119–124
Livshits G, Deng HW, Nguyen TV, Yakovenko K, Recker RR, Eisman JA (2004) Genetics of bone mineral density: evidence for a major pleiotropic effect from an intercontinental study. J Bone Miner Res 19(6):914–923
Medina-Gomez C, Kemp JP, Estrada K et al (2012) Meta-analysis of genome-wide scans for total body BMD in children and adults reveals allelic heterogeneity and age-specific effects at the WNT16 locus. PLoS Genet 8:e1002718
International Physical Activity Questionnaire (2005) Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)—short and long forms. http://www.springer.com/home?SGWID=0-0-1003-0-0&aqId=2642693&checkval=f8ea8104a38699377b8a23954591c49e. Accessed 17 Mar 2014
Acknowledgments
The authors gratefully acknowledge all of the families who participated in the GAO Project. Without them, this work could never have been accomplished. The project was partially supported by the National Fund of Sanitary Investigations (FIS PI 11/01175). G. Athanasiadis was supported by the Subprograma Nacional de Contratación e Incorporación de Investigadores Juan de la Cierva (MICINN). We thank W. H. Stone for his helpful advice and constructive discussions.
Disclosure
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors declare that they have no competing interests.
Appendix
Appendix
Definitions
-
Level of sun exposure was defined as the weekly number of hours of exposure between 11:00 am and 2:00 pm.
-
Dietary calcium intake was defined as the number of glasses of milk or portions of yogurt or cheese that were consumed weekly.
-
Physical activity was quantified through the International Physical Activity Questionnaire [44]. Activity was classified as high, moderate, or low on the categorical score.
-
Smoking habit was evaluated as either ongoing or finished. Consumption was calculated as packs per year, and when finished, nonsmoking time was measured in years.
-
Alcohol habit was defined as nonconsumption, low consumption (less than 30 g/day or 3 units), moderate consumption (30–40 g/day or 3–4 units), and high consumption (more than 40 g/day or 4 units).
-
Coffee intake was estimated as 0, 1–2, 2–4, or >4 cups of coffee per day. Weight was measured in kilograms (within 0.1 kg of accuracy), height in centimeters (within 0.5 cm of accuracy), and BMI (kg/m2).
Rights and permissions
About this article
Cite this article
Sosa, N.Hd., Athanasiadis, G., Malouf, J. et al. Heritability of Bone Mineral Density in a Multivariate Family-Based Study. Calcif Tissue Int 94, 590–596 (2014). https://doi.org/10.1007/s00223-014-9852-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-014-9852-9