Abstract
Genetic components are known to strongly influence bone mineral density (BMD) and bone architecture and turnover, playing an important role in determining risk of osteoporosis and fragility fractures. Twin and family linkage studies confirmed the importance of genetic factors in the individual variance of bone mass peak, BMD, bone geometry, and metabolism and, thus, in predisposition to osteoporosis and related fractures.
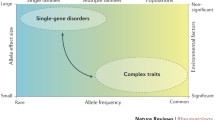
Osteoporosis is a complex, multifactorial disorder whose pathogenesis is due to the addictive effects of various genetic determinants interacting with environmental influences and lifestyle habits. Several genes have been associated with bone mass and other determinants of fracture risk, each of them exerting a relatively modest single effect on the bone tissue. The synergic action of various predisposing alleles, within different genes, in association with environmental and lifestyle risk factors is presumably responsible for osteoporosis development and fragility fracture occurrence.
This chapter aims to review the current knowledge on major genetic factors involved in the regulation of bone mass, architecture, and turnover, thus exerting a possible role also in the pathophysiology of osteoporosis.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
2.1 Introduction
Osteoporosis is a clinical condition of the skeleton, defined when value of bone mineral density (BMD) is lower than 2.5 standard deviations from the mean value of the young adult population (T-score values), usually measured at the lumbar spine (L1–L4) and femoral neck. Low bone mass is associated with deterioration in micro-architecture and geometry of the skeleton, and with a deregulated bone turnover, resulting in an excessive bone resorption and a reduced novel bone formation. The final clinical endpoints of osteoporosis are fragility fractures, mainly at the wrist, spine, and femoral neck that occur in about 30% of postmenopausal women and 12% of elderly men [1] and are responsible for the morbidity and mortality of the disease.
Bone strength is the parameter to measure the risk of fracture, and it is principally determined by the combination of BMD, bone size, and bone quality. For years BMD has been the only one measurable marker for assessing osteoporosis and fracture risk, and also today it is widely used to define the osteoporosis status. However, it is now well assessed that BMD value alone is not sufficient to determine the real risk of develop osteoporotic fracture, and other important parameters of bone quality (such as bone architecture and bone metabolism) have to be taken into account.
Osteoporosis risk depends by the failure to acquire the optimal bone mass peak during growth and by the capacity of maintain bone mass during the elderly and aspects that are both regulated by numerous dietary, lifestyle, hormonal, and genetic factors. Deficiency of calcium and/or vitamin D during childhood and adolescence may be responsible for the reduction of bone mass peak, while during the adulthood and elderly may have a fundamental negative role in increasing bone mass loss. The rapid decrease of estrogens at menopause strongly contributes to a rapid bone loss in postmenopausal women, and it is one of the main causes of the higher incidence of osteoporosis in women.
Today, it is well assessed that osteoporosis is a multifactorial complex disorder whose pathogenesis is due to the interaction and synergic effects of various predisposing genetic determinants regulating bone and mineral metabolism, of “non-skeletal” risk factors that could influence the risk of falling (i.e., muscle strength, balance, and visual acuity), of environmental influences, and of dietary and lifestyle habits.
2.2 Genetic Contribution to Osteoporosis
Principal skeletal determinants of osteoporosis predisposition and fragility fracture risk, such as BMD, bone geometry, and bone metabolism, are all under strong genetic influences. Major advances in the knowledge of genetic aspects of osteoporosis and fracture risk have been made in the last two decades, and they have been principally derived by study on monogenic bone diseases, linkage analyses in osteoporotic pedigrees, association case-control and population-based studies for candidate genes, and experimental crosses in animal models.
Twin and family studies allowed to assess that about 60–85% of human BMD variability is under control of genetic factors [2, 3], and the heritability of other bone characteristics, such as bone geometry and bone turnover markers, ranges between 50 and 80% [4, 5]. Moreover, genetic factors demonstrated to regulate up to 80% of individual variability of bone mass peak acquisition [6], acting principally before puberty. Conversely, the effect of genetic influences on fracture risk is less than 30% [7], maybe because fracture is a more complex phenotype that is determined not only by bone density and quality but also by other non-skeletal conditions.
Several genes have been associated with bone mass and other determinants of bone quality and fracture risk, but each of them has demonstrated to exert only a relatively modest single effect on bone tissue, suggesting that osteoporosis is the result of the synergic effect of various predisposing genetic variants, within different genes, in association with environmental and lifestyle risk factors. To date, more than 100 candidate gene polymorphic variants have been tested for their association with BMD, fractures, and other bone-related quantitative trait loci (QTLs).
Briefly, we reported data about studies on major genes involved in osteoporosis and related phenotypes, discussing the effect of their polymorphic variants on bone mass, bone quality, and metabolism.
2.2.1 Lipoprotein Receptor-Related Protein 5 (LRP5) and Lipoprotein Receptor-Related Protein 6 (LRP6) Genes
These two genes are discussed together since they form a receptor complex with frizzled (Fz) to activate the transcriptional activity of the beta-catenin within the Wnt signaling pathway that is involved in the regulation of osteoblast commitment, differentiation, and apoptosis, in the synthesis of bone matrix protein and mineralization process, as well as in the coupling to osteoclasts and induction of bone resorption [8]. Inactivating mutations of the LRP5 gene are responsible for the osteoporosis pseudoglioma (OPPG), an autosomal recessive monogenic Mendelian disorder, characterized by severe early juvenile osteoporosis, very low bone mass, and fragility fractures. Conversely, activating mutations of the LRP5 gene result in sclerosing bone dysplasias, clinical conditions characterized by an excessive bone mass. Due to its role in the development of these two rare inherited bone disorders, LRP5 has been suspected as a key regulator of bone mass, and common polymorphic variations of this gene have been investigated, by association studies, for their relationship with BMD and fragility fracture in the general population. The two most investigated variants were the missense single nucleotide polymorphism (SNP) c.2047G>A, the Val667Met in exon 9 (rs4988321), and the missense SNP c.4037C>T, Ala1330Val in exon 18 (rs3736228). Both c.2047A and c.4037T alleles were associated with reduced lumbar bone mineral content, vertebral bone area, and stature in Caucasian men, but not in women [9], accounting for up to 15% of variance for these traits. In the same year, a study on young Korean men failed to find any association between LRP5 polymorphism and peak bone mass and BMD at any site [10]. In a case-control study on middle-aged men (mean age 50 years) with idiopathic osteoporosis, both the rare alleles of these two polymorphisms and their haplotype have been associated with a threefold high risk of low BMD [11]. In 2006 the Rotterdam Study confirmed the association between the 1330Val allele and a reduced lumbar spine area and a higher risk of fracture at the femur, humerus, and pelvis in elderly men, but not in women [12]. The same study evidenced an interaction between the 1330Val allele and a missense SNP Ile1062Val in the LRP6 gene (rs2302685), showing that 1330Val and 1062Val alleles have a synergic effect on fracture risk [12]. In 2008 a Bayesian meta-analysis on 10 association studies, including a total of 16,705 individual (of whom the great majority were women (8444) aged 18–81 years) indicated that 1330Val variant has a modest association with BMD and authors concluded that this aspect may limit its clinical use [13]. More recently, a prospective, multicenter, and large-scale study on 37,534 individuals from 18 participating teams in Europe and North America by the GENOMOS study group confirmed that genetic variations of the LRP5 gene are associated with both BMD and fracture risk, very consistently across analyzed populations but with a modest clinical effect [14]. Conversely, the Ile1062Val SNP of LRP6 did not show a significant association with BMD [14].
2.2.2 Vitamin D Receptor (VDR) Gene
Bioactive form of vitamin D is fundamental for the acquisition of bone mass pick and for the maintenance of bone homeostasis. It acts through its binding to the vitamin D receptor (VDR). Mutations of the VDR gene cause the syndrome of vitamin-resistant rickets a recessive Mendelian condition, characterized by severe rickets, hypocalcemia, and hypophosphatemia, which is resistant to vitamin D supplementation. Due to the importance of vitamin D in bone metabolism, VDR has been the first candidate gene whose polymorphic variants have been analyzed in association studies for osteoporosis in 1994, showing that common allelic variants of VDR can be used to predict differences in BMD, accounting for up to 75% of the total genetic effect on BMD in healthy individuals [15]. Association studies between VDR and osteoporosis have been principally focused on two polymorphisms in intron 8 (BsmI and ApaI), one silent polymorphism in exon 9 (TaqI), a polymorphism affecting exon 2 and creating an alternative start codon and responsible for two different isoforms of VDR protein which differ in length by three amino acids (FokI), and a functional polymorphism in the promoter region at the binding site for the transcription factor Cdx-2. BsmI, ApaI, and TaqI are in linkage disequilibrium, and maybe they are also in linkage disequilibrium with other sequence variations in the 3′ untranslated region (UTR) of the VDR gene that could affect mRNA stability and, thus, VDR protein expression. Numerous association studies have been published, presenting conflicting and/or inconclusive data, maybe due to inadequate population sampling, ethnicity, gender, age, confounding factors, gene-gene interactions, and gene-environment interactions; a linkage disequilibrium between VDR polymorphisms and other bone metabolism genes cannot be excluded. Today, results of association studies on large populations seem to strongly reduce the role of VDR polymorphisms in the risk of osteoporosis and fragility fractures. The GENOMOS study (26,242 participants; 18,405 women) evaluated association between Cdx-2, FokI, BsmI, ApaI, and TaqI polymorphisms, and DXA-measured femoral neck and lumbar spine BMD, and fractures concluding that FokI, BsmI, ApaI, and TaqI are not associated with BMD or with fractures, and only Cdx-2 showed a very modest effect on the risk of vertebral fractures [16].
A haplotype meta-analysis by Thakkinstian et al. [17] evidenced that VDR single polymorphisms were not significantly associated to osteoporosis, while specific BsmI/ApaI/TaqI haplotypes were significantly associated to the clinical condition. Data from this study seem to indicate a gain in power when considering VDR haplotypes rather than polymorphisms separately, demonstrating the importance of haplotype studies rather than single polymorphism studies for the VDR gene.
In addition, some studies suggested a possible interaction between calcium and vitamin D intake and VDR polymorphisms in the regulation of BMD [6, 18], with the possibility that effect of VDR genotypes on BMD would be visible only in the presence of a low calcium intake [19] or a vitamin D deficiency. Conversely, the association between VDR genotypes and bone mass would be hidden by high calcium and/or vitamin D intake.
2.2.3 Estrogen Receptor Alpha (ERα) Gene
Estrogens are very important for the correct bone metabolism, for the skeletal growth, and for the maintenance of bone mass. Indeed, severe depletion of estrogens at menopause results in a rapid loss of bone mass, and it is one major cause of higher incidence of osteoporosis and fragility fractures in women than in men. Estrogens exert their action on bone cells through their specific steroid receptors (ERs). An inactivating mutation of the estrogen receptor alpha (ERα or ESR1) gene was identified in men affected by severe juvenile osteoporosis. This fact prompted ERα as an important candidate gene for osteoporosis. ERα and, very less frequently, estrogen receptor beta (ERβ or ESR2) genes have been widely studied about the association of their polymorphisms with osteoporosis and fragility fractures at the wrist, hip, and spine. In the last two decades, a large number of studies investigated about an association between ERα polymorphisms and bone mass, mostly focusing on two SNPs in the intron 1 of the gene, recognized, respectively, by the XbaI and PvuII restriction enzymes, and on a variable TA repeat in the promoter region. PvuII maps within consensus recognition sites for AP4 and Myb transcription factors and influences Myb-associated transcription in vitro [20]. Both XbaI and PvuII have shown to influence report gene transcription in vitro [21]. These data suggest a direct functional effect of XbaI and PvuII on ERα expression, but it is also possible a linkage disequilibrium with other functional polymorphic variations within ERα gene and/or contiguous genes.
Association studies between ERα polymorphisms and BMD showed inconsistent and controversial results. A meta-analysis by Ioannidis et al. [22], including more than 5000 women from 22 different studies (of which 11 including Caucasian women and 11 including Asian women), evidenced an association between XbaI genotypes and both BMD and fractures, with the XX genotype (XbaI) resulting associated with higher femur and spine BMD values (+1 to 2%) and with a reduced risk of fractures.
In 2004, the GENOMOS study group performed a large-scale association study between XbaI, PvuII, and TA repeat polymorphisms of ERα (both as single polymorphism and as haplotypes) and both BMD and occurrence of fragility fractures in 18,917 unrelated individuals from eight European centers [23]. None of the three polymorphisms or haplotypes showed any statistically significant effect on BMD. Conversely women with the homozygote XX genotype of XbaI had a reduced incidence of 19% for all fractures and of 35% for vertebral fractures. No significant effects on fracture risk were seen for PvuII and TA repeats. The study seems to indicate XbaI as a risk marker for fracture, independently by BMD values [23].
Very few studies investigated the role of polymorphic variants of ERβ in determining BMD and fracture risk, principally focused on a CA repeat in the intron 5 of the gene. The Framingham study analyzed the association of this genetic variation and four other intronic polymorphisms with BMD in 723 men and 795 women [24]. The CA repeat genotypes resulted associated with femoral BMD but not with the spine BMD, both in women and in men. Two other SNPs, rs1256031 and rs1256059 (respectively, in the intron 11 and the intron 15 of ERβ), showed an association with femoral BMD in men, and rs1256031, in particular, accounted for up to 4.0% difference in mean femoral BMD. The haplotype C-23CA-T (rs1256031, CA repeat, rs1256059) was significantly associated with reduced femoral BMD in women, with BMD value differences ranging from 3.0 to 4.3%. In the same year, the CA repeat was investigated for its association with BMD in 226 healthy postmenopausal women (60–98 years), evidencing that women with less than 25 CA repeats had significantly higher BMD at the total skeleton, lumbar spine, and femoral neck with respect to women bearing more than 25 CA repeats [25].
Two years later a large population-based cohort study analyzed the association of ERβ polymorphisms with risk of vertebral and incident fragility fracture in postmenopausal women, alone or in association with polymorphisms of ERα and insulin-like growth factor I (IGF1) genes, showing a synergic effect of genotypes interaction on fracture risk, and, thus, reinforcing the idea of the polygenic and complex nature of osteoporosis [26].
2.2.4 Aromatase Gene (CYP19)
The CYP19 gene encodes for aromatase, the enzyme responsible for estrogen synthesis by catalyzing the aromatization of C19 androgens to C18 estrogens. Inactivating mutations of CYP19 cause aromatase deficiency, and they have been associated to clinical conditions affecting also bone growth and mineralization. Common polymorphisms of CYP19 have been, in vitro, associated with enzymatic activity. A study by Masi et al. first reported an association between a tetranucleotide (TTTA) repeat polymorphism in intron 4 of the CYP19 gene and BMD in postmenopausal Italian women [27]. The association of these polymorphisms with BMD was also studied in Italian elderly men but without evidencing a statistical significance [28]. The association between TTTA repeat and BMD was not confirmed in Finnish early postmenopausal women [29]. Another study reported an association between a common SNP in the 5′ untranslated region (UTR) of CYP19 (rs1062033) and BMD in Spanish late postmenopausal women [30]. More recently, six polymorphisms (rs4646, rs10046, rs3784307, rs1062033, rs936306, and rs190258), located throughout the entire CYP19 gene (including also the 5′ and 3′ UTRs), were associated with bone mass in 286 Spanish postmenopausal women [31]. The rs10046 SNP in the 3′UTR resulted associated with BMD; the postmenopausal decrease in bone mass appeared to be slower in women with the AA genotype, than in those with AG or GG genotypes. This polymorphism is in strongly linkage disequilibrium with the TTTA repeat and the rs4646 SNP in the 3′UTR, and they are all three associated with BMD. Two SNPs, located in exon I.6 and promoter I.6 of CYP19, were analyzed in a cohort of 256 Spanish postmenopausal women [32], and rs4775936 was associated with lumbar spine BMD, with the homozygote AA genotype exhibiting a significantly higher lumbar spine BMD if compared with GG or GA women.
Association of CYP19 functional polymorphisms with BMD and/or fracture was also confirmed by other studies on different populations [33,34,35,36,37].
2.2.5 Collagen Type I Alpha I (COLIA1) Gene
Collagen type 1 is the most represented protein of bone extracellular matrix (about 80% of total proteins in bone tissue). Alterations of collagen synthesis, properties, and relative quantity of its two chains affect mechanical features of bone tissue and increase susceptibility to fragility fractures. Inactivating mutations of the gene encoding the alpha I chain of type I collagen (COLIA1) are responsible for osteogenesis imperfecta, a hereditary Mendelian disorder characterized by severe osteoporosis and skeletal fracture in early life. Therefore, COLIA1 is one of the principal candidate genes for fragility fractures in osteoporosis. A common polymorphism in the intron 1 of the COL1A1 gene, (Sp1 polymorphism, rs1800012) alters the binding site for the Sp1 transcription factor, affecting COL1A1 transcription and resulting in an alteration of the normal equilibrium between α1 and α2 chains (2:1). In particular, the s allele has an increased affinity for Sp1, resulting in a higher amount of α1 with respect to α2 chain; the Ss genotype is responsible for a collagen chain ratio of 2.3 (respect to the normal 2, typical of the SS genotype) [38]. Association studies evaluated the effect of Sp1 polymorphism on BMD and fragility fractures, showing a mild association with BMD values but a stronger relationship to osteoporotic fractures, particularly at the spine [38,39,40,41]. In particular, a higher prevalence of fragility fracture was found among ss and Ss genotypes with respect to the SS genotype [38,39,40,41], with an increase in fracture risk of about 68% for each copy of the s allele and independently by a significant reduction of BMD value [38].
The GENOMOS study evaluated COLIA1 Sp1 alleles as a predictor of BMD and fracture in 20,786 unrelated individuals from several European countries and found only a modest association between the ss genotype and reduced BMD; no reduction of BMD was observed in Ss individuals [42]. Moreover, the s allele could predispose to incident vertebral fractures in women, but not in men, and the association with vertebral fracture has a 40% increase of risk for each copy of the s allele carried [42], independently by BMD.
A study by Uitterlinden et al. [43] investigated the interaction of polymorphisms of VDR and COLI1A genes in susceptibility to fractures in 1004 postmenopausal women. The “baT” (BsmI-ApaI-TaqI) VDR risk haplotype was evaluated in association with ss and Ss COLI1A risk genotypes, showing a significant interaction (p = 0.03) between VDR and COLIA1 genotype effects. In subjects bearing the SS genotype, the fracture risk was not VDR genotype-dependent. Conversely, in subjects carrying ss or Ss genotypes, the contemporaneous presence of the baT haplotype was associated with a higher risk of fracture of 4.4 and 2.1, respectively [43].
Moreover, an additive effect of the COLIA1 Sp1 polymorphism with 10565insGGA polymorphism of the sclerostin (SOST gene) was evidenced in an elderly male and female Caucasian healthy population [44].
Data from these two studies further confirmed the polygenic nature of osteoporosis and fracture risk.
2.2.6 Transforming Growth Factor Beta (TGF-β1)
Transforming growth factor beta (TGF-β1) is largely expressed by osteoclasts, and it has shown to control bone resorption and formation by directly acting on both osteoblasts and osteoclasts [45]. Therefore, polymorphic variants of TGF-β1 gene have been extensively studied in relation to osteoporosis. A C/T transition in exon 1 which causes a proline-leucine substitution at position 10 has been associated with higher level of circulating TGF-β1 protein, and the C allele was associated with higher BMD values and lower occurrence of fragility fractures in two Japanese populations [46]. A rare polymorphism in intron 4 (713-8delC variant) was associated with very low BMD, severe osteoporosis, and fracture risk in women with osteoporosis and with low bone mass and increased bone turnover in both osteoporotic and normal women [47]. The same research group evaluated, in 2003, the association between 8 polymorphisms of the TGF-β1 gene and osteoporosis in a case-control study of 96 osteoporotic patients with vertebral fractures vs 330 normal individuals, evidencing that the TT genotype of the 816-20 T>C variant in the intron 5 was less common in fractured osteoporotic patients than in healthy controls and that it was associated with higher lumbar spine and hip bone mass [48].
The GENOMOS study investigated associations between five TGF-β1 polymorphisms [G–1639A (G–800A, rs1800468), C–1348T (C–509T, rs1800469), T29C (Leu10Pro, rs1982073), G74C (Arg25Pro, rs1800471), and C788T (Thr263Ile, rs1800472)] and BMD and fractures in 28,924 male and female individuals from 10 different European research studies [49]. Only weak associations between the C–1348T SNP and lumbar spine BMD in men and between the C788T SNP and risk of incident vertebral fractures were reported [49], presumably indicating that polymorphic variations of the TGF-β1 gene do not play a major role in regulating BMD or susceptibility to fragility fractures.
Recently, a meta-analysis integrated all the eligible studies, including a total of 8 studies involving 1851 cases and 2247 controls, and it investigate whether T869C and T29C polymorphisms of the TGF-β1 gene were correlated with postmenopausal osteoporosis [50]. A significant association between T29C or T869C polymorphisms and osteoporosis risk was observed only in Asian, but not in Caucasian, population [50].
2.2.7 Other Genes
Polymorphisms of other genes, involved in the regulation of bone metabolism and turnover, have been, although more rarely, investigated about their association with BMD and fractures. They include sclerostin (SOST), bone morphogenetic protein 2 (BMP2), bone morphogenetic protein 4 (BMP4), osteoprotegerin (OPG, TNFRSF11B), receptor activator of nuclear factor kappa-B (RANK; TNFRSF11A), RANK ligand (RANKL; TNFSF11), and runt-related transcription factor 2 (RUNX2; CBFA1).
Principal results from their association and/or linkage studies are depicted in Table 2.1.
2.3 Novel Approaches to the Genetics of Osteoporosis: Genome-Wide Association Studies (GWAS)
Because of the polygenic nature of osteoporosis, in which few genes exert major effects on bone metabolism and homeostasis, while a large number of genes have only minor effects, classical single gene association and/or linkage studies present numerous limitations, such as inconclusive or controversial results, false-positive and/or false-negative associations, reduced sensibility in identifying genotype-phenotype associations, and inability to identify novel candidate genes and their genetic variants. The recent development of next generation sequencing (NGS) technique has allowed to design gene chips for the simultaneous analysis of hundreds genes and their polymorphic variants. Genome-wide association studies (GWAS) have opened new horizons for the discovery of genetic loci and variants associated with osteoporosis and fracture risk, and the application of this novel approach, in the last years, has obtained success in identifying replicated genetic loci associated with osteoporosis.
The first GWAS in osteoporosis was performed in 2007 and analyzed 100,000 SNPs in 1141 individuals from the Framingham Osteoporosis Study to examine genetic associations with bone quantitative traits: BMD (including the femoral neck, trochanter, and lumbar spine), calcaneal ultrasound, and geometric indices of the hip [79]. Of the 40 top SNPs with the highest number of significantly associations with BMD traits, a variable percentage of 30–50% of them maps within genetic loci or near genes that have not previously been studied for osteoporosis. The others were polymorphisms located within known osteoporosis candidate genes, such as rs1884052 and rs3778099 in ERα, rs4988300 in LRP5, rs2189480 in VDR, rs2075555 in COLIA1 and rs10519297, and rs2008691 in CYP19.
One year later, two major GWAS analyzed the association of over 300,000 SNPs with BMD and fractures [80, 81]. The first study [80] evidenced an association between BMD and two SNPs, rs4355801 on chromosome 8 near to the TNFRSF11B gene, and rs3736228, on chromosome 11 in the LRP5 gene. The second study [81] identified five genomic regions significantly associated with BMD, both in the discovery set population and in the replication set populations. Three of these regions map close to or within genes known to be important in bone homeostasis: TNFSF11, TNFRSF11B, and ERα.
In 2009, a large-scale meta-analysis of five GWAS of femoral neck and lumbar spine BMD, including 19,195 individuals of Northern European descent, allowed to identify 20 genetic loci reaching the genome-wide significance (GWS; p < 5 × 10−8). Seven of them confirmed to be known bone-related loci/genes, 1p36 (ZBTB40), 6q25 (ERα), 8q24 (TNFRSF11B), 11q13.4 (LRP5), 12q13 (SP7), 13q14 (TNFSF11), and 18q21 (TNFRSF11A), while 13 mapped to new regions, not yet investigated as candidate genes for osteoporosis: 1p31.3 (GPR177), 2p21 (SPTBN1), 3p22 (CTNNB1), 4q21.1 (MEPE), 5q14 (MEF2C), 7p14 (STARD3NL), 7q21.3 (FLJ42280), 11p11.2 (LRP4, ARHGAP1, F2), 11p14.1 (DCDC5), 11p15 (SOX6), 16q24 (FOXL1), 17q21 (HDAC5), and 17q12 (CRHR1) [82].
Two years later, a larger meta-analysis of 17 GWAS of the femoral neck and lumbar spine BMD was performed on 32,961 subjects of European and East Asian ancestry and validated for marker replication of BMD association on 50,933 independent subjects and for association with risk of low-trauma fracture in 31,016 fractured individuals (cases) and 102,444 non-fractured controls [83]. The study identified 56 loci (32 novels) associated with BMD with a positive GWS; 14 of them resulted also associated with fracture risk. Numerous of these loci mapped near or within TNFRSF11B, TNFRSF11A, and TNFSF11 genes or near or within genes involved in the Wnt signaling pathways, in the mesenchymal stem cell differentiation and in the endochondral ossification.
GWAS highlighted the highly polygenic and complex nature of osteoporosis and fracture susceptibility and the difficulty to predict the risk of osteoporosis on genetic bases. Anyway, since the first GWAS on osteoporosis was performed in 1997, numerous and great advances have been made in the discovery and validation of genes and loci involved in the predisposition to osteoporosis. GWAS allowed, to date, the identification of more than 60 loci associated with BMD, osteoporosis, and fragility fractures, including novel loci, whose functional analysis has demonstrated that they have a clear effect on bone metabolism and, presumably, also on osteoporosis pathophysiology.
The association of GWAS results with functional studies revealed very useful to identify novel molecular targets for anti-fracture drugs and, thus, allowed the design of novel target therapies for osteoporosis.
References
Ralston SH. Genetic determinants of susceptibility to osteoporosis. Curr Opin Pharmacol. 2003;3:286–90.
Guéguen R, Jouanny P, Guillemin F, Kuntz C, Pourel J, Siest G. Segregation analysis and variance components analysis of bone mineral density in healthy families. J Bone Miner Res. 1995;10(12):2017–22.
Krall EA, Dawson-Hughes B. Heritable and life-style determinants of bone mineral density. J Bone Miner Res. 1993;8(1):1–9.
Arden NK, Baker J, Hogg C, Baan K, Spector TD. The heritability of bone mineral density, ultrasound of the calcaneus and hip axis length: a study of postmenopausal twins. J Bone Miner Res. 1996;11(4):530–4.
Garnero P, Arden NK, Griffiths G, Delmas PD, Spector TD. Genetic influence on bone turnover in postmenopausal twins. J Clin Endocrinol Metab. 1996;81(1):140–6.
Eisman JA. Genetics of osteoporosis. Endocr Rev. 1999;20:788–4.
MacGregor A, Snieder H, Spector TD. Genetic factors and osteoporotic fractures in elderly people. Twin data support genetic contribution to risk of fracture. BMJ. 2000;320(7250):1669–70.
Yavropoulou MP, Yovos JG. The role of the Wnt signaling pathway in osteoblast commitment and differentiation. Hormones. 2007;6(4):279–94.
Ferrari SL, Deutsch S, Choudhury U, Chevalley T, Bonjour JP, Dermitzakis ET, Rizzoli R, Antonarakis SE. Polymorphisms in the low-density lipoprotein receptor-related protein 5 (LRP5) gene are associated with variation in vertebral bone mass, vertebral bone size, and stature in whites. Am J Hum Genet. 2004;74(5):866–75.
Koh JM, Jung MH, Hong JS, Park HJ, Chang JS, Shin HD, Kim SY, Kim GS. Association between bone mineral density and LDL receptor-related protein 5 gene polymorphisms in young Korean men. J Korean Med Sci. 2004;19(3):407–12.
Ferrari SL, Deutsch S, Baudoin C, Cohen-Solal M, Ostertag A, Antonarakis SE, Rizzoli R, de Vernejoul MC. LRP5 gene polymorphisms and idiopathic osteoporosis in men. Bone. 2005;37(6):770–5.
van Meurs JB, Rivadeneira F, Jhamai M, et al. Common genetic variation of the low-density lipoprotein receptor-related protein 5 and 6 genes determined fracture risk in elderly white men. J Bone Miner Res. 2006;21(1):141–50.
Tran BNH, Nguyen ND, Eisman JA, Nguyen TV. Association between LRP5 polymorphism and bone mineral density: a Bayesian meta-analysis. BMC Med Genet. 2008;9:55.
van Meurs JBJ, Trikalinos TA, Ralston SH, et al. Large-scale analysis of association between LRP5 and LRP6 variants and osteoporosis. JAMA. 2008;299(11):1277–90.
Morrison NA, Qi JC, Tokita A, Kelly PJ, Crofts L, Nguyen TV, Sambrook PN, Eisman JA. Prediction of bone density from vitamin D receptor alleles. Nature. 1994;367(6460):284–7.
Uitterlinden AG, Ralston SH, Brandi ML, Carey AH, Grinberg D, Langdahl BL, Lips P, Lorenc R, et al. The association between common vitamin D receptor gene variations and osteoporosis: a participant-level meta-analysis. Ann Intern Med. 2006;145(4):255–64.
Thakkinstian A, D’Este C, Attia J. Haplotype analysis of VDR gene polymorphisms: a meta-analysis. Osteoporos Int. 2004;15(9):729–34.
Ferrari S, Rizzoli R, Chevalley T, et al. Vitamin-D-receptor-gene polymorphisms and change in lumbar-spine bone mineral density. Lancet. 1995;345(8947):423–4.
Ferrari S. Genetics, nutrition and bone health. In: Holick M, Dawson-Hughes E, editors. Nutrition and bone health. Totowa: The Humana press Inc; 2004. p. 19–41.
Herrington DM, Howard TD, Brosnihan KB, McDonnell DP, Li X, Hawkins GA, et al. Common estrogen receptor polymorphism augments effects of hormone replacement therapy on E-selectin but not C-reactive protein. Circulation. 2002;105:1879–82.
Maruyama H, Toji H, Harrington CR, Sasaki K, Izumi Y, Ohnuma T, et al. Lack of an association of estrogen receptor α gene polymorphisms and transcriptional activity with Alzheimer disease. Arch Neurol. 2000;57:236–40.
Ioannidis JP, Stravrou I, Trikalinos TA, Zois C, Brandi ML, Gennari L, et al. Association of polymorphisms of the estrogen receptor α gene with bone mineral density and fracture risk in women: a meta-analysis. J Bone Miner Res. 2002;17:2048–60.
Ioannidis JP, Ralston SH, Bennett ST, Brandi ML, Grinberg D, Karassa FB, et al. Differential genetic effects of ESR1 gene polymorphisms on osteoporosis outcomes. JAMA. 2004;292(17):2105–14.
Shearman AM, Karasik D, Gruenthal KM, Demissie S, Cupples LA, Housman DE, et al. Estrogen receptor beta polymorphisms are associated with bone mass in women and men: the Framingham Study. J Bone Miner Res. 2004;19(5):773–81.
Scariano JK, Simplicio SG, Montoya GD, Garry PJ, Baumgartner RN. Estrogen receptor beta dinucleotide (CA) repeat polymorphism is significantly associated with bone mineral density in postmenopausal women. Calcif Tissue Int. 2004;74(6):501–8.
Rivadeneira F, van Meurs JB, Kant J, Zillikens MC, Stolk L, Beck TJ, et al. Estrogen receptor beta (ESR2) polymorphisms in interaction with estrogen receptor alpha (ESR1) and insulin-like growth factor I (IGF1) variants influence the risk of fracture in postmenopausal women. J Bone Miner Res. 2006;21(9):1443–56.
Masi L, Becherini L, Gennari L, Amedei A, Colli E, Falchetti A, et al. Polymorphism of the aromatase gene in postmenopausal Italian women: distribution and correlation with bone mass and fracture risk. J Clin Endocrinol Metab. 2001;86:2263–9.
Gennari L, Masi L, Merlotti D, Picariello L, Falchetti A, Tanini A, et al. A polymorphic CYP19 TTTA repeat influences aromatase activity and estrogen levels in elderly men: effects on bone metabolism. J Clin Endocrinol Metab. 2004;89(6):2803–10.
Salmen T, Heikkinen AM, Mahonen A, Kröger H, Komulainen M, Pallonen H, et al. Relation of aromatase gene polymorphism and hormone replacement therapy to serum estradiol levels, bone mineral density, and fracture risk in early postmenopausal women. Ann Med. 2003;35(4):282–8.
Zarrabeitia MT, Hernández JL, Valero C, Zarrabeitia AL, García-Unzueta M, Amado JA, et al. A common polymorphism in the 5′-untranslated region of the aromatase gene influences bone mass and fracture risk. Eur J Endocrinol. 2004;150(5):699–704.
Riancho JA, Zarrabeitia MT, Valero C, Sañudo C, Hernández JL, Amado JA, et al. Aromatase gene and osteoporosis: relationship of ten polymorphic loci with bone mineral density. Bone. 2005;36(5):917–25.
Enjuanes A, Garcia-Giralt N, Supervía A, Nogués X, Ruiz-Gaspà S, Bustamante M, et al. A new SNP in a negative regulatory region of the CYP19A1 gene is associated with lumbar spine BMD in postmenopausal women. Bone. 2006;38(5):738–43.
Lorentzon M, Swanson C, Eriksson AL, Mellström D, Ohlsson C. Polymorphisms in the aromatase gene predict areal BMD as a result of affected cortical bone size: the GOOD study. J Bone Miner Res. 2006;21(2):332–9.
Mullin BH, Carter KW, Lewis JR, Ingley E, Wilson SG, Prince RL. Significant association between common polymorphisms in the aromatase gene CYP19A1 and bone mineral density in postmenopausal women. Calcif Tissue Int. 2011;89(6):464–71.
Koudu Y, Onouchi T, Hosoi T, Horiuchi T. Association of CYP19 gene polymorphism with vertebral fractures in Japanese postmenopausal women. Biochem Genet. 2012;50(5-6):389–96.
Markatseli AE, Lazaros L, Markoula S, Kostoulas H, Sakaloglou P, Tigas S, et al. Association of the (TTTA)n repeat polymorphism of CYP19 gene with bone mineral density in Greek peri- and postmenopausal women. Clin Endocrinol. 2014;81(1):38–44.
Casas-Avila L, Valdés-Flores M, Miranda-Duarte A, Ponce de León-Suárez V, Castro-Hernández C, Rubio-Lightbourn J, et al. Association of a (TTTA)n microsatellite and a TCT del/ins polymorphisms in the aromatase gene (CYP19) with hip fracture risk in Mexican postmenopausal women. Gynecol Endocrinol. 2015;31(12):987–91.
Mann V, Hobson EE, Li B, Stewart TL, Grant SF, Robins SP, et al. A COL1A1 Sp1 binding site polymorphism predisposes to osteoporotic fracture by affecting bone density and quality. J Clin Invest. 2001;107(7):899–907.
Uitterlinden AG, Burger H, Huang Q, Yue F, McGuigan FE, Grant SF, et al. Relation of alleles of the collagen type I alpha1 gene to bone density and the risk of osteoporotic fractures in postmenopausal women. N Engl J Med. 1998;338(15):1016–21.
Mann V, Ralston SH. Meta-analysis of COL1A1 Sp1 polymorphism in relation to bone mineral density and osteoporotic fracture. Bone. 2003;32(6):711–7.
Efstathiadou Z, Tsatsoulis A, Ioannidis JP. Association of collagen I alpha 1 Sp1 polymorphism with the risk of prevalent fractures: a meta-analysis. J Bone Miner Res. 2001;16(9):1586–92.
Ralston SH, Uitterlinden AG, Brandi ML, Balcells S, Langdahl BL, Lips P, et al. Large-scale evidence for the effect of the COLIA1 Sp1 polymorphism on osteoporosis outcomes: the GENOMOS study. PLoS Med. 2006;3(4):e90.
Uitterlinden AG, Weel AE, Burger H, Fang Y, van Duijn CM, Hofman A, et al. Interaction between the vitamin D receptor gene and collagen type I alpha1 gene in susceptibility for fracture. J Bone Miner Res. 2001;16(2):379–85.
Uitterlinden AG, Arp PP, Paeper BW, Charmley P, Proll S, Rivadeneira F, et al. Polymorphisms in the sclerosteosis/van Buchem disease gene (SOST) region are associated with bone-mineral density in elderly whites. Am J Hum Genet. 2004;75(6):1032–45.
Massagué J, Chen YG. Controlling TGF-β signalling. Genes Dev. 2000;14:627–44.
Yamada Y, Miyauchi A, Goto J, Takagi Y, Okuizumi H, Kanematsu M, et al. Association of a polymorphism of the transforming growth factor-beta1 gene with genetic susceptibility to osteoporosis in postmenopausal Japanese women. J Bone Miner Res. 1998;13(10):1569–76.
Langdahl BL, Knudsen JY, Jensen HK, Gregersen N, Eriksen EF. A sequence variation: 713-8delC in the transforming growth factor-beta 1 gene has higher prevalence in osteoporotic women than in normal women and is associated with very low bone mass in osteoporotic women and increased bone turnover in both osteoporotic and normal women. Bone. 1997;20(3):289–94.
Langdahl BL, Carstens M, Stenkjaer L, Eriksen EF. Polymorphisms in the transforming growth factor beta 1 gene and osteoporosis. Bone. 2003;32(3):297–310.
Langdahl BL, Uitterlinden AG, Ralston SH, Trikalinos TA, Balcells S, Brandi ML, et al. Large-scale analysis of association between polymorphisms in the transforming growth factor beta 1 gene (TGFB1) and osteoporosis: the GENOMOS study. Bone. 2008;42(5):969–81.
Sun J, Zhang C, Xu L, Yang M, Yang H. The transforming growth factor-β1 (TGF-β1) gene polymorphisms (TGF-β1 T869C and TGF-β1 T29C) and susceptibility to postmenopausal osteoporosis: a meta-analysis. Medicine. 2015;94(4):e461.
Huang QY, Li GH, Kung AW. The -9247 T/C polymorphism in the SOST upstream regulatory region that potentially affects C/EBP alpha and FOXA1 binding is associated with osteoporosis. Bone. 2009;45(2):289–94.
Valero C, Zarrabeitia MT, Hernández JL, Pineda B, Cano A, García-Pérez MA, Riancho JA. Relationship of sclerostin and secreted frizzled protein polymorphisms with bone mineral density: an association study with replication in postmenopausal women. Menopause. 2011;18(7):802–7.
Piters E, de Freitas F, Nielsen TL, Andersen M, Brixen K, Van Hul W. Association study of polymorphisms in the SOST gene region and parameters of bone strength and body composition in both young and elderly men: data from the Odense Androgen Study. Calcif Tissue Int. 2012;90(1):30–9.
He J, Zhang H, Wang C, Zhang Z, Yue H, Hu W, et al. Associations of serum sclerostin and polymorphisms in the SOST gene with bone mineral density and markers of bone metabolism in postmenopausal Chinese women. J Clin Endocrinol Metab. 2014;99(4):E665–73.
Zhang H, He JW, Wang C, Zhang Z, Yue H, Hu WW, et al. Associations of polymorphisms in the SOST gene and bone mineral density in postmenopausal Chinese Women. Osteoporos Int. 2014;25(12):2797–803.
Medici M, van Meurs JB, Rivadeneira F, Zhao H, Arp PP, Hofman A, Pols HA, Uitterlinden AG. BMP-2 gene polymorphisms and osteoporosis: the Rotterdam Study. J Bone Miner Res. 2006;21(6):845–54.
McGuigan FE, Larzenius E, Callreus M, Gerdhem P, Luthman H, Akesson K. Variation in the BMP2 gene: bone mineral density and ultrasound in young adult and elderly women. Calcif Tissue Int. 2007;81(4):254–62.
Styrkarsdottir U, Cazier JB, Kong A, Rolfsson O, Larsen H, Bjarnadottir E, et al. Linkage of osteoporosis to chromosome 20p12 and association to BMP2. PLoS Biol. 2003;1(3):E69.
Ramesh Babu L, Wilson SG, Dick IM, Islam FM, Devine A, Prince RL. Bone mass effects of a BMP4 gene polymorphism in postmenopausal women. Bone. 2005;36(3):555–61.
Langdahl BL, Carstens M, Stenkjaer L, Eriksen EF. Polymorphisms in the osteoprotegerin gene are associated with osteoporotic fractures. J Bone Miner Res. 2002;17(7):1245–55.
Arko B, Prezelj J, Komel R, Kocijancic A, Hudler P, Marc J. Sequence variations in the osteoprotegerin gene promoter in patients with postmenopausal osteoporosis. J Clin Endocrinol Metab. 2002;87(9):4080–4.
Zhao HY, Liu JM, Ning G, Zhao YJ, Zhang LZ, Sun LH, et al. The influence of Lys3Asn polymorphism in the osteoprotegerin gene on bone mineral density in Chinese postmenopausal women. Osteoporos Int. 2005;16(12):1519–24.
Arko B, Prezelj J, Kocijancic A, Komel R, Marc J. Association of the osteoprotegerin gene polymorphisms with bone mineral density in postmenopausal women. Maturitas. 2005;51(3):270–9.
Vidal C, Brincat M, Xuereb Anastasi A. TNFRSF11B gene variants and bone mineral density in postmenopausal women in Malta. Maturitas. 2006;53(4):386–95.
Mencej-Bedrač S, Preželj J, Marc J. TNFRSF11B gene polymorphisms 1181G > C and 245T > G as well as haplotype CT influence bone mineral density in postmenopausal women. Maturitas. 2011;69(3):263–7.
Zhang F, He C, Chen G, Li F, Gao H. Association analyses of osteoprotegerin gene polymorphisms with bone mineral density in Chinese postmenopausal women. Med Oncol. 2013;30(1):389.
Yu F, Huang X, Miao J, Guo L, Tao D. Association between osteoprotegerin genetic variants and osteoporosis in Chinese postmenopausal women. Endocr J. 2013;60(12):1303–7.
Lin H, Zhang G, Chen X, Wu X, Wu C, Ca H, et al. The relationship between the g.27450A>T genetic variant of OPG gene and osteoporosis in Chinese postmenopausal women. Int Immunopharmacol. 2014;21(2):464–7.
Boroňová I, Bernasovská J, Mačeková S, Petrejčíková E, Tomková Z, Kľoc J, et al. TNFRSF11B gene polymorphisms, bone mineral density, and fractures in Slovak postmenopausal women. J Appl Genet. 2015;56(1):57–63.
Koh JM, Park BL, Kim DJ, Kim GS, Cheong HS, Kim TH, et al. Identification of novel RANK polymorphisms and their putative association with low BMD among postmenopausal women. Osteoporos Int. 2007;18(3):323–31.
Işleten B, Durmaz B, Durmaz B, Onay H, Ozkınay F, Durmaz A, et al. The association of RANK gene C421T and C575T polymorphisms with bone mineral density in postmenopausal Turkish women. Arch Gynecol Obstet. 2013;288(4):917–23.
Tu P, Duan P, Zhang RS, Xu DB, Wang Y, Wu HP, et al. Polymorphisms in genes in the RANKL/RANK/OPG pathway are associated with bone mineral density at different skeletal sites in post-menopausal women. Osteoporos Int. 2015;26(1):179–85.
Mencej S, Prezelj J, Kocijancic A, Ostanek B, Marc J. Association of TNFSF11 gene promoter polymorphisms with bone mineral density in postmenopausal women. Maturitas. 2006;55(3):219–26.
Vaughan T, Pasco JA, Kotowicz MA, Nicholson GC, Morrison NA. Alleles of RUNX2/CBFA1 gene are associated with differences in bone mineral density and risk of fracture. J Bone Miner Res. 2002;17(8):1527–34.
Bustamante M, Nogués X, Agueda L, Jurado S, Wesselius A, Cáceres E, et al. Promoter 2 -1025 T/C polymorphism in the RUNX2 gene is associated with femoral neck bmd in Spanish postmenopausal women. Calcif Tissue Int. 2007;81(4):327–32.
Lee HJ, Koh JM, Hwang JY, Choi KY, Lee SH, Park EK, et al. Association of a RUNX2 promoter polymorphism with bone mineral density in postmenopausal Korean women. Calcif Tissue Int. 2009;84(6):439–45.
Pineda B, Hermenegildo C, Laporta P, Tarín JJ, Cano A, García-Pérez MÁ. Common polymorphisms rather than rare genetic variants of the Runx2 gene are associated with femoral neck BMD in Spanish women. J Bone Miner Metab. 2010;28(6):696–705.
Kim KC, Chun H, Lai C, Parnell LD, Jang Y, Lee J, et al. The association between genetic variants of RUNX2, ADIPOQ and vertebral fracture in Korean postmenopausal women. J Bone Miner Metab. 2015;33(2):173–9.
Kiel DP, Demissie S, Dupuis J, Lunetta KL, Murabito JM, Karasik D. Genome-wide association with bone mass and geometry in the Framingham Heart Study. BMC Med Genet. 2007;8(Suppl 1):S14.
Richards JB, Rivadeneira F, Inouye M, Pastinen TM, Soranzo N, Wilson SG, et al. Bone mineral density, osteoporosis, and osteoporotic fractures: a genome-wide association study. Lancet. 2008;371(9623):1505–12.
Styrkarsdottir U, Halldorsson BV, Gretarsdottir S, Gudbjartsson DF, Walters GB, Ingvarsson T, et al. Multiple genetic loci for bone mineral density and fractures. N Engl J Med. 2008;358(22):2355–65.
Rivadeneira F, Styrkársdottir U, Estrada K, Halldórsson BV, Hsu YH, Richards JB, et al. Twenty bone-mineral-density loci identified by large-scale meta-analysis of genome-wide association studies. Nat Genet. 2009;41(11):1199–206.
Estrada K, Styrkarsdottir U, Evangelou E, Hsu YH, Duncan EL, Ntzani EE, et al. Genome-wide meta-analysis identifies 56 bone mineral density loci and reveals 14 loci associated with risk of fracture. Nat Genet. 2012;44(5):491–501.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Marini, F., Masi, L., Marcucci, G., Cianferotti, L., Brandi, M.L. (2018). Genetics of Osteoporosis. In: Lenzi, A., Migliaccio, S. (eds) Multidisciplinary Approach to Osteoporosis. Springer, Cham. https://doi.org/10.1007/978-3-319-75110-8_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-75110-8_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-75108-5
Online ISBN: 978-3-319-75110-8
eBook Packages: MedicineMedicine (R0)