Abstract
Hip fractures represent a major public health challenge worldwide. Multinational studies using a common methodology are scarce. We aimed to estimate the incidence rates (IRs) and trends of hip/femur fractures over the period 2003–2009 in five European countries. The study was performed using seven electronic health-care records databases (DBs) from Denmark, The Netherlands, Germany, Spain, and the United Kingdom, based on the same protocol. Yearly IRs of hip/femur fractures were calculated for the general population and for those aged ≥50 years. Trends over time were evaluated using linear regression analysis for both crude and standardized IRs. Sex- and age-standardized IRs for the UK, Netherlands, and Spanish DBs varied from 9 to 11 per 10,000 person-years for the general population and from 22 to 26 for those ≥50 years old; the German DB showed slightly higher IRs (about 13 and 30, respectively), whereas the Danish DB yielded IRs twofold higher (19 and 52, respectively). IRs increased exponentially with age in both sexes. The ratio of females to males was ≥2 for patients aged ≥70–79 years in most DBs. Statistically significant trends over time were only shown for the UK DB (CPRD) (+0.7 % per year, P < 0.01) and the Danish DB (−1.4 % per year, P < 0.01). IRs of hip/femur fractures varied greatly across European countries. With the exception of Denmark, no decreasing trend was observed over the study period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures represent a major public health challenge in developed countries due to the increasing age of the population [1]. In 2000, there were almost 1 million patients with an episode of hip fracture in the European Union, and it has been predicted that this figure will increase more than twofold in the coming 50 years [2]. The increasing trend in the incidence of hip fractures along with associated morbidity complications, dependence, and mortality [3, 4] make this condition a major public health concern. In addition, hospital resources for injury-related admissions are one of the major causes of total health-care costs in Europe [5]. Distribution of this injury in the world is heterogeneous [1], although Europe holds an important share of these fractures (37 %) worldwide [6].
In recent years an increasing number of studies have reported that the secular trends in the incidence of hip fractures have leveled off [7–9] or started to decline since the late 1990s [10] in some European countries. Allegedly, this would be the result of the effectiveness of national campaigns to prevent both osteoporosis and falls [2, 11]. A call to update the data for as many countries as possible has been made [12] in order to check whether this favorable trend is consistent. In the present study we describe the incidence of hip and femur fractures across five European countries (Denmark, Germany, The Netherlands, the United Kingdom, and Spain) using seven different electronic health-care record databases and compare the rates and trends over the period 2003–2009.
Patients and Methods
Data Sources
Seven European data sources located in five different countries were used in this study. The Danish national registries (DKMA; http://www.dkma.dk, http://www.sst.dk); the German bavarian association of statutory health insurance physicians database (Bavarian claims; http://subs.emis.de/LNI/Proceedings/); the Dutch Mondriaan project (http://www.projectmondriaan.nl) with two databases, Netherlands primary care research database (NPCRD) and Almere health care group (AHC; http://www.zorggroep-almere.nl); the Spanish Base de datos para la Investigación Farmacoepidemiológica en Atención Primaria (BIFAP; http://www.bifap.org); and two databases from the United Kingdom, the Clinical practice research datalink (CPRD, formerly known as the general practice research database; http://www.cprd.com) and the health improvement network (THIN; http://www.thin-uk.com).
Four are nationwide primary care databases covering a part of their country’s population: 2 % (Mondriaan NPCRD), 5.7 % (THIN), 6.8 % (BIFAP), and 8 % (CPRD). Mondriaan-AHC is a primary care regional database representing over 170,000 patients (90.3 % of citizens in 2008) from the newly built city Almere in The Netherlands. The Bavarian Claims database includes population-based data on diagnoses and medical services linked to outpatient treatment data through general practitioners (GPs) and specialists, covering 10.5 million people (85 % of the Bavarian population). Dates of prescribing and diagnoses are not available in the Bavarian Claims database, which includes only the quarter of the year a prescription or a diagnosis was registered. And finally, the Danish national registries, maintained by the National Institute for Health Data and Disease Control, contain information on all hospital contacts since 1995 (inpatient contacts since 1977 and emergency and outpatient contacts since 1995), medication dispensing on a pharmacy level linked to individuals who redeemed a prescription from 1994 onward, causes of death for the entire population (5.3 million inhabitants), and contact information of visits to GPs as well as specialists in private care.
All participating databases fulfill quality standards for pharmacoepidemiology research [13]. A common protocol and data specifications, revised and approved by all study participants and by an external committee, were adopted by the seven databases. This study is part of the Pharmacoepidemiological Research on Outcomes of Therapeutics by a European Consortium (PROTECT; http://www.imi-protect.eu/). The study protocol has been registered in the European Network of Centres for Pharmacoepidemiology and Pharmacovigilance study registry (http://www.encepp.eu/).
Study Population
The study population comprised patients of all age groups within each database during the period from January 1, 2003 to December 31, 2009, fulfilling the quality criteria of valid registration status established by the respective database owners. Within this period, we selected as a start date the latest of the following: the date when the practice came up to a research standard, the date when the practice was enrolled into the database, or the date when a patient was enrolled into a practice or into the database (this does not apply to the Danish data, which included all citizens). End of follow-up was defined as the end of the study period or the earliest of the following events: the patient died, the patient was transferred out, the practice left the database, or the last event was recorded. For the Danish databases follow-up was stopped at the end of the study period or if the patient died or left Denmark. For the Mondriaan AHC database data from 2009 were not available, and the Bavarian Claims database provided data only from 2006 to 2008.
Outcome Definition
Although our main interest was hip fracture, defined as a fracture of the proximal femur in the cervix or in the trochanteric region, we considered “any femur fracture” to be the operational outcome definition for this study (hereinafter referred to as “hip/femur” fracture). The main reason was that some of the participating databases (the Dutch NPCRD and AHC and the Spanish BIFAP) use the International Classification of Primary Care (ICPC-2) for disease coding, which does not have a specific code for hip fracture but a broader code for “femur” fracture (L75); and a primary objective of PROTECT was to assure consistency in the outcome definition across databases. Additionally, the use of a broader code may avoid overlooking hip fractures by miscoding [14]. The codes applied for the outcome searching strategy are described in Online Resource I. The coding system was unchanged during the study period in each database.
We included all patients with a first ever diagnosis of hip/femur fracture during the study period. Patients with a history of past hip/femur fracture ever before were excluded, to increase the likelihood of including incident episodes only.
Analysis
Annual incidence rates (IRs) of hip/femur fractures were calculated for the whole study population. The numerator comprised all first ever recorded cases of hip/femur fracture, and the denominator was the total number of person-years of follow-up. We also calculated the annual IR among people aged 50 years or above separately as most fractures occurring before this age are primarily due to trauma and many studies use this age limit [15, 16].
For the comparison of the IRs in the whole population and the population 50 years or older across databases and over time, we carried out a direct sex and age standardization using the European Union population in 2008 (EUROSTAT) as the standard (http://epp.eurostat.ec.europa.eu/portal/page/portal/population/data/database).
We also calculated age- (in 10-year bands) and sex-specific IRs over the study period. Age of patients was computed at midyear within each calendar year of the study period. The incidence rate ratios (IRRs) and their 95 % confidence intervals (95 % CIs) were calculated to assess the effect of sex on different age groups within each database.
To quantify the trend over the study period, we performed linear regression analysis for both crude and standardized rates in each database, defining the annual IR as the dependent variable and the calendar year as the independent variable. The respective slope (β coefficient) was considered as the average change per year over the study period. This annual change was also expressed as a percentage of IR using the first year as reference. The null hypothesis of β = 0 was tested using the t test. P < 0.05 was considered significant. The 95 % CI of the slope was also calculated.
Results
IRs of Hip/Femur Fractures
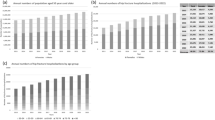
The data sources from the United Kingdom, The Netherlands, and Spain provided standardized IRs for the general population, mostly ranging from 9 to 11 per 10,000 person-years (py). The Bavarian Claims database displayed rates around 13 per 10,000 py, whereas the Danish database yielded rates around 19 per 10,000 py (Online Resource II: Table A).
The standardized IRs of hip/femur fracture for the population 50 years or older were two to three times higher than those for the general population, ranging 15–25 per 10,000 py in the United Kingdom, The Netherlands, and Spain to 52 per 10,000 py in Denmark and around 30 per 10,000 py in Germany (Table 1).
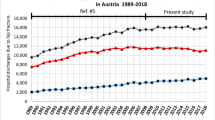
Time Trends
A significant trend in standardized IRs in people 50 years or older was only observed for the British CPRD (+0.7 % per year, P < 0.01) and the Danish database (−1.4 % per year, P < 0.01) (Table 1). For the remaining databases no significant trend was observed. The short study period available for the Bavarian Claims database precluded any trend analysis.
Sex- and Age-Specific IRs of Hip/Femur Fracture
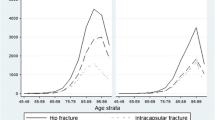
The crude and age-standardized IRs were two to three times higher in women than in men for the whole population (data not shown) and for the population 50 years or older, over the study period and across all databases (Fig. 1). In 2008, the median standardized IRR of females vs. males was 2.4 (range across databases 1.3–3.3) for the general population and 2.6 (range across databases 1.6–3.1) for the population 50 years or older. This ratio, however, was shown to be strongly dependent on age: for age groups less than 50 years the IRRs of females vs. males were consistently below 1 but then increased gradually, reaching a maximum at age 70–79 and then declining (Fig. 2).
The IRs of hip/femur fractures grew exponentially at the age of 50 years for both females and males (Fig. 3a, b, respectively), which was a constant feature for all databases and for the whole study period (see complete data for all databases in Online Resource III: Table B).
Trends of age- and sex-specific IRs over the study period showed that there was no relevant trend in any age group or sex in the British, Dutch, and Spanish databases. In the Danish database there appeared to be sex- and age-dependent trends: an increasing trend in females 50–59 years old and a decreasing trend in both males and females among the 70–79 age group, being stable or slightly decreasing among the other age groups (Online Resource IV: Figure a).
Discussion
To the best of our knowledge this is the first study to provide a direct comparison across European countries of incidence rates of hip/femur fractures and trends over time, using the same case definition and the same standard population. The main findings of our study were as follows: (1) Denmark showed age- and sex-standardized IRs of hip/femur fractures two times higher than those observed in the United Kingdom, The Netherlands, and Spain, while Germany yielded IRs in between; (2) in all countries, IRs were about two to three times greater in females than in males and grew exponentially with age regardless of sex, both patterns being constant in all databases; and (3) significant trends in standardized IRs over time were observed only in two databases (slight increasing trend in the British CPRD and a decreasing trend in the Danish databases), both among the general population and among the population 50 years or older.
Denmark showed the highest IRs throughout the study period with figures rather similar to those already published for the general population (21.1 per 10,000 population) [2] and for the population 50 years or older (45 per 10,000 py) [17]. The two UK databases participating in the present study yielded almost identical results and were similar to those reported for England (10.2 per 10,000 py) using hospital admission rates [18]. The IRs from the Spanish database in people 50 years or older are also similar to those reported by Hernandez et al. [8] using hospital discharge data from Cantabria in 2002 (25.9 per 10,000 py) and to those reported in Catalonia [19] using GP records in 2009 (22.3 per 10,000 py). The two GP databases from The Netherlands provided standardized IRs that fluctuated greatly over the study period, showing lower values than those based on hospital registries [15, 20]. One plausible explanation for these results is that there was a slight underregistration of ICPC codes by GPs until 2009 in The Netherlands. This has been proved since after a national campaign to stimulate ICPC coding in 2010–2011, the incidence of hip/femur fractures rose to 13.5 per 10,000, which is similar to both the hospital registration and the NPCRD Web site. Finally, IRs from the Bavarian claims database were marginally lower than those in other studies [7, 21], which might be due to differences in ICD coding and the data sources employed (national hospital discharge diagnosis opposed to outpatient diagnosis). Therefore, in general, the data provided in the present study seem to be consistent with results from previous studies using different data sources. Also, our data confirm the evidence that European Nordic countries exhibit greater IRs of hip/femur fractures than other European countries [1, 22]. There is no definitive explanation for that, but lifestyle, limited exposure to sunlight, and weather conditions may play a role [23, 24]. Regarding this latter factor, some studies performed in Nordic countries observed higher IRs in winter than summer, likely related to the fact that worse weather conditions with slippery roads and pavements increase the risk of falls [25, 26].
The IRs of hip/femur fractures increased exponentially with age for both males and females, as observed in other studies, which may be explained partly by the progressive bone mass reduction with aging [27] but also by the accumulation of other risk factors, such as disability and increasing risk of falls, as well as increasing use of drugs acting at the central nervous system (e.g., antidepressants, hypnosedatives, antiparkinsonians, opioids) or the cardiovascular system (e.g., antihypertensives, diuretics) or drugs affecting bone mineral density (e.g., corticosteroids, glitazones, SSRIs).
The female to male IR ratios steadily increased with age among the population over 50 years but declined at older ages (≥80 years), probably indicating that males approximate females in bone mineral density and major risk factors at very old ages [28]. This pattern was consistent across most databases and over the whole study period and is in accordance with previously published results [16, 29, 30]. Conversely, men presented higher IRs than women under the age of 50 years, most probably due to the greater incidence of trauma-related fractures among males [31].
Time trend analyses showed no decreasing trend in the standardized IRs over time in most databases, with the exception of the Danish database. Thus, the general picture is of a rather stable situation which appears to date back to the 1990s, as shown by previous reports in the same countries [3, 18]. Denmark is the only country in our study which showed a steady decline over the study period, in particular among the population 70–79 years old, in both males and females. This tendency is shared by other Nordic countries [32], as well as by the United States [33], Australia [34], Canada [35], and Scotland [36]. This decline in the Nordic countries might be attributable to a better management of osteoporosis (earlier screening, diagnosis, and treatment of patients at risk) [37] and a combination of healthier diet, increase of physical activity, and educative measures to prevent falls [38]. Also, a trend toward a lower consumption of certain drugs that increase the risk of falls and fractures may have contributed. Interestingly, in a parallel PROTECT study we observed an important decreasing trend in the use of benzodiazepines in Denmark during the same time period [39]. In the AHC database there was also the suggestion of a decreasing trend since 2005; but the IRs were based on a small number of cases, and this trend was not observed in the other Dutch database.
Among the strengths of the present study is the use of multiple databases that proved valid for pharmacoepidemiological research [13] including representative populations regarding age and sex. Additionally, a common protocol and data specifications were used by all participants, with consistent criteria for case searches and operational case definitions, which facilitates comparison of results across data sources. The present study is part of a larger research program aimed at describing and analyzing the discrepancies found among data sources from different European countries with respect to selected outcomes, drug exposures, and, particularly, associations between drug exposures and outcomes. Therefore, common analytical procedures were employed in order to minimize methodological discrepancies as much as possible. Nevertheless, each data source has its own limitations with regard to data collection, and each country has different health policies and prescription patterns, which, among other intrinsic characteristics of populations and their lifestyles, may contribute to the variability of our results.
As limitations we should mention that IRs of hip/femur fractures reported in this article come from codes recorded in the corresponding databases, and no further validation was performed [40]. This, in particular for the GP-based data sources, may result in an underreporting of hip fractures, in particular of fatal cases, which might not be reported to the GP. However, the IRs obtained in the present study were fairly consistent with those published previously by other authors using different data sources (most of them from hospital records), which reinforces the idea that the data provided can be used as reasonably valid estimates for each country. Importantly, the analysis of time trends should not be affected by such potential limitation as the search criteria were unchanged over the study period. However, the study period (7 years) may not be long enough to observe slight trends. On the other hand, the use of the outcome “hip/femur” fracture might have inflated the number of cases with respect to other studies which only focused on “hip” fractures. However, it is pertinent to note that some authors [14, 41] have recommended the use of this broader outcome for monitoring hip fractures, even when using hospital records, as “there is often miscoding between fractures of the neck of the femur and fractures of other parts or unspecified parts of the femur” [14]. However, this limitation is less important when the data are referred to the population 50 years or older as 90 % of femoral fractures beyond this age are of osteoporotic nature and mostly affect the neck or intertrochanteric site [42].
In conclusion, IRs of hip/femur fractures in the European countries that took part in this research showed no significant trend over the study period. A remarkable exception to this general picture is Denmark, which presented the highest IRs but showed a consistent decline in both males and females 70 years or older. Our results confirm the strong relation between this injury and age and sex, largely published in the literature, and give an updated overview of the IRs of this major public health issue in Europe. In addition, this study proves the value of GP databases to estimate and compare incidence of disease among multiple sources once common procedures are followed.
References
Kanis JA, Oden A, McCloskey EV, Johansson H, Wahl DA, Cooper C (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23(9):2239–2256
International Osteoporosis Foundation (2008) Osteoporosis in the European Union in 2008: ten years of progress and ongoing challenges. http://www.sante.public.lu/publications/maladies-traitements/osteoporose/osteoporosis-eu-2008/osteoporosis-eu-2008.pdf. Accessed 2 Oct 2012
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359(9319):1761–1767
Salkeld G, Cameron ID, Cumming RG, Easter S, Seymour J, Kurrle SE, Quine S (2000) Quality of life related to fear of falling and hip fracture in older women: a time trade off study. BMJ 320(7231):341–346
Polinder S, Meerding WJ, van Baar ME, Toet H, Mulder S, van Beeck EF, EUROCOST Reference Group (2005) Cost estimation of injury-related hospital admissions in 10 European countries. J Trauma 59(6):1283–1291
Kanis J, on behalf of the World Health Organization Scientific Group (2007) Assessment of osteoporosis at the primary health care level. http://www.shef.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf. Accessed Nov 2012
Mann E, Meyer G, Haastert B, Icks A (2010) Comparison of hip fracture incidence and trends between Germany and Austria 1995–2004: an epidemiological study. BMC Public Health 10:46
Hernandez JL, Olmos JM, Alonso MA, Gonzalez-Fernandez CR, Martinez J, Pajaron M, Llorca J, Gonzalez-Macias J (2006) Trend in hip fracture epidemiology over a 14-year period in a Spanish population. Osteoporos Int 17(3):464–470
Lyritis GP, Rizou S, Galanos A, Makras P (2013) Incidence of hip fractures in Greece during a 30-year period: 1977–2007. Osteoporos Int 24:1579–1585
Korhonen N, Niemi S, Parkkari J, Sievanen H, Palvanen M, Kannus P (2013) Continuous decline in incidence of hip fracture: nationwide statistics from Finland between 1970 and 2010. Osteoporos Int 24:1599–1603
Lakatos P, Balogh A, Czerwinski E, Dimai HP, Hans D, Holzer G, Lorenc RS, Palicka V, Obermayer-Pietsch B, Stepan J, Takacs I, Resch H (2011) New considerations on the management of osteoporosis in central and eastern Europe (CEE): summary of the “3rd summit on osteoporosis-CEE”, November 2009, Budapest, Hungary. Arch Osteoporos 6(1–2):1–12
Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, Melton LJ, Cummings SR, Kanis JA (2011) Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int 22(5):1277–1288
Abbing-Karahagopian V, Kurz X, de Vries F, van Staa T, Alvarez Y, Hesse U, et al (2013) Bridging differences in outcomes of pharmacoepidemiological studies: design and first results of the PROTECT project. Curr Clin Pharmacol, in press
Balasegaram S, Majeed A, Fitz-Clarence H (2001) Trends in hospital admissions for fractures of the hip and femur in England, 1989–1990 to 1997–1998. J Public Health Med 23(1):11–17
Lalmohamed A, Welsing PM, Lems WF, Jacobs JW, Kanis JA, Johansson H, de Boer A, de Vries F (2012) Calibration of FRAX® 3.1 to the Dutch population with data on the epidemiology of hip fractures. Osteoporos Int 23(3):861–869
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12):1726–1733
Giversen IM (2006) Time trends of age-adjusted incidence rates of first hip fractures: a register-based study among older people in Viborg County, Denmark, 1987–1997. Osteoporos Int 17(4):552–564
Wu TY, Jen MH, Bottle A, Liaw CK, Aylin P, Majeed A (2011) Admission rates and in-hospital mortality for hip fractures in England 1998 to 2009: time trends study. J Public Health (Oxf) 33(2):284–291
Pages-Castella A, Carbonell-Abella C, Aviles FF, Alzamora M, Baena-Diez JM, Laguna DM, Nogues X, Diez-Perez A, Prieto-Alhambra D (2012) Burden of osteoporotic fractures in primary health care in Catalonia (Spain): a population-based study. BMC Musculoskelet Disord 13:79
Goettsch WG, de Jong RB, Kramarz P, Herings RM (2007) Developments of the incidence of osteoporosis in The Netherlands: a PHARMO study. Pharmacoepidemiol Drug Saf 16(2):166–172
Icks A, Haastert B, Wildner M, Becker C, Meyer G (2008) Trend of hip fracture incidence in Germany 1995–2004: a population-based study. Osteoporos Int 19(8):1139–1145
Dhanwal DK, Dennison EM, Harvey NC, Cooper C (2011) Epidemiology of hip fracture: worldwide geographic variation. Indian J Orthop 45(1):15–22
Johnell O, Borgstrom F, Jonsson B, Kanis J (2007) Latitude, socioeconomic prosperity, mobile phones and hip fracture risk. Osteoporos Int 18(3):333–337
Elffors I, Allander E, Kanis JA, Gullberg B, Johnell O, Dequeker J, Dilsen G, Gennari C, Lopes Vaz AA, Lyritis G et al (1994) The variable incidence of hip fracture in southern Europe: the MEDOS study. Osteoporos Int 4(5):253–263
Fretland S, Kruger O (1998) Femoral neck fractures in Nord-Trondelag 1988–95. Incidence differences between winter and summer months [in Norwegian]. Tidsskr Nor Laegeforen 118(1):34–36
Gronskag AB, Forsmo S, Romundstad P, Langhammer A, Schei B (2010) Incidence and seasonal variation in hip fracture incidence among elderly women in Norway. The HUNT study. Bone 46(5):1294–1298
Poole KE, Compston JE (2006) Osteoporosis and its management. BMJ 333(7581):1251–1256
De Laet CE, van Hout BA, Burger H, Hofman A, Pols HA (1997) Bone density and risk of hip fracture in men and women: cross sectional analysis. BMJ 315(7102):221–225
Johnell O, Gullberg B, Allander E, Kanis JA (1992) The apparent incidence of hip fracture in Europe: a study of national register sources. MEDOS study group. Osteoporos Int 2(6):298–302
Dolan P, Torgerson DJ (1998) The cost of treating osteoporotic fractures in the United Kingdom female population. Osteoporos Int 8(6):611–617
Tafuri S, Martinelli D, Balducci MT, Fortunato F, Prato R, Germinario C (2008) Epidemiology of femoral neck fractures in Puglia (Italy): an analysis of existing data. Ig Sanita Pubbl 64(5):623–636
Nilson F, Moniruzzaman S, Gustavsson J, Andersson R (2012) Trends in hip fracture incidence rates among the elderly in Sweden 1987–2009. J Public Health (Oxf) 35(1):125–131
Adams AL, Shi J, Takayanagi M, Dell RM, Funahashi TT, Jacobsen SJ (2012) Ten-year hip fracture incidence rate trends in a large California population, 1997–2006. Osteoporos Int 24(1):373–376
Pasco JA, Brennan SL, Henry MJ, Nicholson GC, Sanders KM, Zhang Y, Kotowicz MA (2011) Changes in hip fracture rates in southeastern Australia spanning the period 1994–2007. J Bone Miner Res 26(7):1648–1654
Leslie WD, Sadatsafavi M, Lix LM, Azimaee M, Morin S, Metge CJ, Caetano P (2011) Secular decreases in fracture rates 1986–2006 for Manitoba, Canada: a population-based analysis. Osteoporos Int 22(7):2137–2143
Holt G, Smith R, Duncan K, Hutchison JD, Reid D (2009) Changes in population demographics and the future incidence of hip fracture. Injury 40(7):722–726
Greene D, Dell RM (2010) Outcomes of an osteoporosis disease-management program managed by nurse practitioners. J Am Acad Nurse Pract 22(6):326–329
EU Commission, Executive Agency for Health and Consumers (EAHC) (2009) PASEO (physical activity among sedentary older people). http://www.paseonet.org/the_project.html. Accessed Nov 2012
Huerta CA-KV, Requena G, Oliva B, Alvarez Y, et al (2013) Prevalence of use of benzodiazepines and related drugs in seven European databases: a cross-national descriptive study from the PROTECT-EU project. Presented at the 29th international conference on pharmacoepidemiology and therapeutic risk management, Montreal, 25–28 August 2013
Garcia Rodriguez LA, Ruigomez A (2010) Case validation in research using large databases. Br J Gen Pract 60(572):160–161
Evans JG, Seagroatt V, Goldacre MJ (1997) Secular trends in proximal femoral fracture, Oxford record linkage study area and England 1968–86. J Epidemiol Community Health 51(4):424–429
Schilcher J, Michaelsson K, Aspenberg P (2011) Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med 364(18):1728–1737
Acknowledgments
The research leading to these results was conducted as part of the PROTECT consortium (Pharmacoepidemiological Research on Outcomes of Therapeutics by a European Consortium; www.imi-protect.eu) which is a public–private partnership coordinated by the European Medicines Agency. The authors thank the excellent collaboration of physicians in the participating countries, whose contribution in recording their professional practice with high-quality standards made possible the availability of databases used in this research. M. L. De Bruin is employed by Utrecht University as a senior researcher conducting research under the umbrella of the WHO Collaborating Centre for pharmaceutical policy and regulation. This center receives no direct funding or donations from private parties, including the pharmaceutical industry. Research funding from public–private partnerships, e.g., IMI, TI Pharma (www.tipharma.nl), is accepted under the condition that no company-specific product or company-related study is conducted. The center has received unrestricted research funding from public sources, e.g., the Netherlands Organisation for Health Research and Development (ZonMW), the Dutch Health Care Insurance Board (CVZ), the EU 7th Framework Program (FP7), the Dutch Medicines Evaluation Board (MEB), and the Dutch Ministry of Health. The Escher Project is a project of the Top Institute Pharma (TI Pharma), a public–private partnership of the Dutch Government, academia, and pharmaceutical companies. The Escher Project focuses on regulatory science. The PROTECT project is a collaborative European project that comprises a program to address limitations of current methods in the field of pharmacoepidemiology and pharmacovigilance. The projects within the Escher Project and the PROTECT project are of a general nature and do not involve specific companies, products, or therapeutic areas. M. Miret was a Merck employee at the time this research was done; she is not currently working there. C. Schneider received an unconditional grant from Merck Serono, Geneva. S. Schmiedl received honoraria for a lecture from a German pharmaceutical company (Rottapharm Madaus, Cologne, Germany). M. C. H. De Groot received unrestricted funding for pharmacoepidemiological research from the Dutch private–public Top Institute Pharma. A. Bate is a Pfizer employee. A. Ruigómez and L. A. García-Rodríguez are employed by CEIFE, which has received research funding from AstraZeneca R&D (Mölndal, Sweden) and Bayer Pharma (Berlin, Germany). L. A. García-Rodríguez has also served as a speaker and an advisory board member for the above-mentioned companies. S. Johansson is an Astra Zeneca employee. R. Schlienger is a full-term Novartis employee and owns Novartis shares. R. Reynolds is an employee and a stockholder of Pfizer. O. H. Klungel received unrestricted funding for pharmacoepidemiological research from the Dutch private–public Top Institute Pharma.
Funding
The PROTECT project has received support from the Innovative Medicines Initiative Joint Undertaking (IMI JU; www.imi.europa.eu) under Grant 115004, resources of which are composed of financial contributions from the European Union’s Seventh Framework Programme (FP7/2007–2013) and the European Federation of Pharmaceutical Industries and Associations (EFPIA) companies’ in-kind contributions. In addition, as a special form of the IMI JU grant, Utrecht University and Alcalá University received a direct financial contribution from Pfizer and AstraZeneca, respectively. M. Miret, A. Bate, R. Schlienger, S. Johansson, and R. Reynolds belong to EFPIA member companies in the IMI JU, and costs related to their part in the research were carried by the respective company as in-kind contributions under the IMI JU scheme. The views expressed are those of the authors only and not of their respective institutions or companies.
Author information
Authors and Affiliations
Corresponding authors
Additional information
G. Requena, F. J. de Abajo, V. Abbing-Karahagopian, C. Huerta, Y. Alvarez, U. Hesse, H. Gardarsdottir, P. C. Souverein, J. Slattery, M. Rottenkolber, M. Gil, F. de Vries, and D. Montero declare they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Requena, G., Abbing-Karahagopian, V., Huerta, C. et al. Incidence Rates and Trends of Hip/Femur Fractures in Five European Countries: Comparison Using E-Healthcare Records Databases. Calcif Tissue Int 94, 580–589 (2014). https://doi.org/10.1007/s00223-014-9850-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-014-9850-y