Abstract
The efficacy of clodronate to reduce bone loss around uncemented stems after total hip arthroplasty (THA) was evaluated. Ninety-one patients operated with uncemented THA were randomized to receive either intramuscular clodronate at a dose of 100 mg weekly for 12 months or no treatment. Periprosthetic and contralateral bone mineral density (BMD) scans were performed and biochemical markers of bone turnover measured at baseline and at 3, 6, and 12 months. At month 12, with the exception of Gruen zones 4 and 5, patients treated with clodronate showed less bone loss at all zones, reaching statistical significance (P < 0.05) in Gruen zones 2 and 6 (difference of 6.6 and 5.9%, respectively). Analysis of data according to gender revealed sex-related differences in bone loss and efficacy of treatment. After 12 months, the difference in bone loss between treated and untreated women in five out of seven Gruen zones ranged from 6.2 to 13.3% (SS at zones 2 and 6), whereas comparison between treated and untreated men showed no BMD differences in all zones (P > 0.05). Median percent changes in serum levels of markers of bone metabolism by gender were consistent with BMD changes. A 1-year treatment with intramuscular clodronate determined a significant reduction of bone loss after THA. This was mainly attributed to its greater efficacy in the female population, which is at higher risk for bone loss. This observation suggests the need for the characterization of high-risk subjects as potential candidates for prevention strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Every year, more than 600,000 total hip arthroplasties (THAs) are implanted worldwide, and surgical replacement of the hip is one of the most cost-effective procedures in medicine [1].
Bone mechanical and biological competence is essential for the success of the implant. Implant failure can be expected in 3–10% of cases within 15 years from surgery; this can be attributed to aseptic loosening in about 75% of failures [2]. In aseptic loosening, wear debris produced by the articulating surfaces of the artificial joint induces a foreign body reaction, which generates massive osteoclast activation; eventually, the bone around the implant is reabsorbed and the implant becomes mobilized [3]. A preserved bone stock that provides primary stability of the implant and osseointegration, sealing the bone–implant interfaces, is a key factor to avoid aseptic loosening and to ensure the long-term survival of the prosthesis [4]. Later, the maintenance of a strong bone may be a protective factor against the risk of periprosthetic fractures and may facilitate revision surgery [5].
Significant osteoclast-mediated bone loss was demonstrated around the prosthesis due to surgical trauma, the absence of weight bearing, and stress-shielding from the implant [6]. Bone loss mainly involves the proximal femur, can be as great as 40% in certain regions, starts just after the operation, and subsides after 6–12 months [7–14]. Therefore, strategies to prevent such an extensive and commonly occurring bone loss and to preserve bone stock are desirable to improve the outcome of the operation.
Bisphosphonates, a family of pharmacological compounds with strong and well-established inhibitory effects on bone resorption that are used to treat osteoporosis and other metabolic bone diseases, represent good candidates for this purpose. A growing body of evidence on their positive effects on reducing periprosthetic bone loss has been collected from some randomized controlled studies [15–22]. Disodium clodronate is a non-amino bisphosphonate, used in the treatment of malignant hypercalcemia and Paget disease of bone, as well as in osteoporosis. It has an inhibitory effect on bone resorption, decreasing bone turnover, and has been proven to increase bone mineral density (BMD) and to reduce the risk of vertebral fractures in osteoporotic patients [23–25]. In contrast to amino bisphosphonates, clodronate has also been shown to possess anti-inflammatory [26] and analgesic [27] properties that make it suitable for the prevention of the periprosthetic bone loss known to occur as a result of an inflammatory process [3]. In a study on subjects who had undergone total-knee arthroplasty [28], 6-month treatment with clodronate resulted in a lesser tibial component migration with respect to the placebo group, providing greater mechanical competence of the periprosthetic bone.
The present multicenter, prospective, randomized study was planned to evaluate the effect of 1-year therapy with a weekly intramuscular administration of disodium clodronate on bone loss around uncemented stems after THA. The multicenter design of the study enabled the recruitment of a number of patients such as to allow a subgroup analysis by gender.
Materials and Methods
Experimental Subjects
Male or postmenopausal female patients, aged 50–70 years, who had undergone primary uncemented THA within the previous 30 days were eligible for the study. Exclusion criteria were treatment with drugs active on bone metabolism (estrogen, progestin, calcitonin, bisphosphonates, fluoride, raloxiphen, glucocorticoids, calcium or vitamin D supplementation, and anabolizing steroids) within the preceding 6 months, rheumatoid arthritis or other polyarthritis, disorders affecting bone metabolism (Paget disease, hypo- or hyperparathyroidism, osteomalacia, secondary osteoporosis), gastrointestinal malabsorption, renal impairment (serum creatinine level >2 mg/dl), liver enzymes (aspartate transaminase or alanine transaminase) twice the upper level of the normal range, or cardiac failure (NYHA class 3 or 4).
From May 2002 to June 2005 patients were recruited into the study and randomized to receive either clodronate (CLD group, 50 patients) or no treatment (CNT group, 54 patients). Subjects were allocated to the clodronate or to the control group by a computer-generated randomization list with blocks of four and a 1:1 ratio.
Study Design and Methods
The study was a multicenter, prospective, randomized, open, two-parallel groups trial, conducted according to Good Clinical Practice (GCP) guidelines. The Ethics Committees of each of the six participating centers approved the study protocol and all the relevant documents. Patients received detailed information on study procedures and were required to give their written consent to be enrolled.
Patients assigned to active treatment received 100 mg/day of clodronate intramuscularly for 10 consecutive days and thereafter weekly for 50 weeks; the treatment period therefore lasted 52 weeks in total. Clodronate (Difosfonal®; SPA-Società Prodotti Antibiotici, Milan, Italy) was provided in ampoules containing 100 mg of active ingredient in 3.3 ml of solution for injection. Patients with osteoporosis (T score at neck area of contralateral hip lower than −2.5) of both groups received supplementation with 500 mg of calcium and 400 UI of vitamin D twice a day for the duration of the study.
At the first study visit, a detailed medical history was taken, information on the surgical procedure was provided, and demographic data were recorded. Periprosthetic and contralateral BMD scans were performed at baseline and after 3, 6, and 12 months by means of dual-energy X-ray absorptiometry (DXA) using a Hologic Discovery (Hologic, Waltham, MA; one center), a Hologic 4500 (two centers), a Hologic 2000 (one center), or a Norland Excel Plus (Norland Medical Systems, Fort Atkinson, WI; one center). DXA instruments were not cross-calibrated between study sites. Subjects were always imaged on the same instrument during their time in the study.
At the operated hip, bone mineral content (BMC, g), area (cm2), and BMD (g/cm2) were determined from seven regions of interest (Fig. 1) based on Gruen zones [29]. Furthermore, zones 1–7 were grouped to form a total region of interest (net average). In the contralateral femur, BMD was measured at the neck, trochanter, intertrochanter, Ward triangle, and total proximal femur. At each center, scans were performed following the detailed written instruction provided regarding positioning of operated and contralateral femur, area to be included, instrument quality controls, archiving, and transmission of scans. All scans were read centrally by an experienced operator unaware of study-arm assignment. Computer software (prosthetic hip and metal software version 6, Hologic) was used to measure the periprosthetic BMD in the seven Gruen zones.
Biochemical markers of bone turnover were measured at baseline and at 3, 6, and 12 months from serum-separated blood (3,500–3,800 rpm for 10–15 min) collected after overnight fast. Samples were stored at −20°C and sent to a central laboratory (Exacta Central Lab, Verona, Italy) for analyses. Bone turnover markers included serum bone alkaline phosphatase (BAP; Metra BAP EIA; Quidel, San Diego, CA) and C-terminal telopeptides of type l collagen (CTX; Serum CrossLaps ELISA; Osteometer Biotech, Herlev, Denmark).
Safety and tolerability were evaluated through physical examination performed at each study visit (baseline and months 3, 6, and 12), blood tests (blood cell counts and blood chemistry, including creatinine and liver enzymes), urinalysis at baseline and at the end of the study period, and reporting of adverse events during every study visit. Local tolerability was evaluated by recording spontaneous report of pain, pain intensity, duration, and frequency of occurrence. Compliance to treatment was assessed by determining the amount of drug returned at each study visit.
Statistical Analysis
The percent change in BMD of the periprosthetic regions was the primary efficacy end point. The secondary end points were as follows: percent change in BMD of the contralateral hip, changes in markers of bone metabolism (BAP, CTX). All statistical analyses were performed by the SAS® System, version 9.1.2, setting the significance level at 5% (α = 0.05). Subjects who had at least one efficacy assessment during the treatment period entered the intent-to-treat population, on which all efficacy and safety analyses were performed. The demographics and baseline characteristics of the two treatment groups were compared by analysis of variance (ANOVA) applied to continuous quantitative data and by χ2 test or Wilcoxon’s two-samples test applied to dichotomous or nominal data. The ANOVA mode included the factors treatment, sex, and the treatment by sex interaction. If this latter was significant, the comparisons between treatments within each gender were performed with the Bonferroni correction for two contrasts.
With regard to BMD of periprosthetic regions and of the contralateral hip, differences in effect of the two treatments were searched at each visit by analysis of covariance (ANCOVA) applied to the percent changes from baseline, considering the factors treatment, sex, and the treatment by sex interaction and including in the model the baseline value as covariate. If the interaction was significant, the mean percent changes adjusted for baseline were used for comparisons between treatments within each gender with the Bonferroni correction for two contrasts. Concerning the within-group comparison versus baseline, a mean adjusted percent change from baseline was declared statistically significant if its 95% confidence interval (95% CI) did not include the 0 value.
Post-hoc power analysis was performed for BMD of periprosthetic regions 2 and 6, taking into account the differences in women at 12 months. The standard deviation (SD) and the difference in adjusted means were drawn from the ANCOVA results; the α level was set to 0.05.
The percent changes from baseline of markers of bone metabolism for the two groups were compared at each visit by the Wilcoxon two-samples test; the significance within groups versus baseline was tested by the signed rank test.
Results
Number of Patients and Characteristics
One hundred and four patients were recruited (Fig. 2). Thirteen patients (eight in the clodronate group and five in the control group) did not attend the first follow-up visit and were not included in the study analysis. Ninety-one patients with at least one follow-up visit were included in the results analysis. Seventy-nine remained in the study for the planned treatment period (12 months) and underwent the final study visit. All others (13.2%), four in the clodronate group and eight controls, dropped out from the study after the first follow-up visit (month 3) as they were lost to follow-up (four patients in both groups) because of protocol violation (two patients in the control group), adverse event (fracture of femur), or consent withdrawal (one each in the control group). No significant differences between study groups were reported in baseline demographic, bone mineral status, and serum levels of BAP and CTX (Table 1).
Treatment Effect on BMD
Mean BMD values of periprosthetic Gruen regions after surgery and percent changes from baseline during the study are shown in Table 2. At baseline, in all periprosthetic zones, bone density at the operated hip was lower in women with respect to men (data not shown), with differences ranging from 0.139 g/cm2 (zone 1) to 0.426 g/cm2 (zone 4). Osteoporosis was diagnosed in 12 women (five in the clodronate group and seven in the control group) from a neck T score lower than −2.5 at contralateral hip.
Concerning the control group, the bone loss with respect to baseline after 3 months from surgery was statistically significant in nearly all regions, with the upper regions (1, 2, 6, and 7) being those with the highest percentages of decrease (8.0–17.2%). At this time, women showed a statistically significant bone loss versus baseline in all Gruen zones with the exception of zone 5, whereas in men this was limited to the upper regions (1, 2, 6, and 7). From months 3 to 12, BMD values remained stable in regions 1 and 2 and increased in region 3 and 5, while a further marked decrease in bone density was observed in regions 6 and 7, leading, respectively, to 14 and 28% of total loss from baseline at 12 months. At month 12, a significant bone decrease versus baseline was still present in zones 1, 2, 3, 6, and 7 in women and only in zones 6 and 7 in men. In patients treated with clodronate, a similar pattern of bone changes was recorded throughout the three postoperative assessments. However, with the exception of regions 4 and 5, the clodronate group showed lower percentages of bone loss at all the measurements performed, achieving statistical significance against the control group at month 12, in zones 2 (6.6%) and 6 (5.9%) (Table 2).
In these zones, at month 12, the treatment by sex interaction was statistically significant or very close to significance (P = 0.016 and P = 0.051, in zones 6 and 2, respectively), indicating a gender-related difference in treatment effect; comparisons between treatments within gender revealed differences in bone loss between treated and untreated women of 12.6% (P = 0.010) in region 6 and 13.3% (P = 0.030) in region 2, while the corresponding values for treated and untreated men were 0.9 and 0.1% (both nonsignificant [NS]). The post-hoc power of accepting as statistically significant (α = 0.05) the above differences was 78% (one-sided test) and 67% (two-sided test) for region 2 (difference 13.3, SD 12.05) and 88% (one-sided test) and 79% (two-sided test) for region 6 (difference 12.6, SD 9.93).
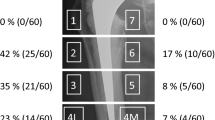
Differences in percentage of bone loss versus baseline between treated and untreated patients were higher in women than in men also in regions 1, 3, and 7, with values increasing with time (Fig. 3). After 12 months, in these regions, differences between treated and untreated women ranged from 6.2 to 9.9%, whereas in men differences did not vary with time and at month 12 were only 1.0–3.0%.
Adjusted means and SE of periprosthetic BMD changes (percentages from baseline) in the seven Gruen regions and in the total area. Women CLD clodronate-treated women; Men CLD clodronate-treated men; Women CNT untreated women; Men CNT untreated men. a P = 0.030, b P = 0.010 between untreated and clodronate-treated women
Regarding the contralateral hip, in the control group, a statistically significant BMD decrease versus baseline was seen at month 12 at the neck (−3.5 ± 0.98 SE), greater trochanter (−1.6% ± 0.67 SE), and intertrochanter (−1.0% ± 0.69 SE) regions and very close to the significance level at the total area (−1.20% ± 0.61 SE).
At the greater trochanter and intertrochanter regions and total area, a statistically significant decrease was seen starting after 3 months from operation (−1.50% ± 0.49 SE, −1.28% ± 0.39 SE, and −1.28% ± 0.49 SE, respectively).
In the clodronate group, contralateral BMD showed no statistically significant bone loss with respect to baseline at all assessment times and a significant increase in BMD in the intertrochanter region after 6 (1.20% ± 0.52 SE) and 12 (1.39% ± 0.65 SE) months.
A statistically significant difference in percent bone loss between the clodronate group and controls, ranging from 1.75 to 2.39% (P between <0.001 and 0.014), was seen at months 3, 6, and 12 in the intertrochanteric region. At this region the treatment by sex interaction was statistically significant at months 6 (P = 0.017) and 12 (P = 0.027), showing a gender-related difference; comparison between treated and untreated women at this region showed statistically significant differences in bone loss of 4.29% (P < 0.001) and 4.54% (P = 0.008) at months 6 and 12, respectively, while differences between treated and untreated men at the same times were 0.25 and 0.7% (both NS). At 12 months differences in percentage of bone density variations between treated and untreated women in the other contralateral regions and total area ranged between 2.7% (greater trochanter) and 7.4% (Ward triangle) with respect to −0.2% (total area) and 1.8% (Ward triangle) between the corresponding groups of men.
Markers of Bone Metabolism
Serum CTX showed a significant median percent reduction compared to baseline at all measurements over time in the clodronate group, with values that remained stable from month 3 (−47.7%) to the end of follow-up (Table 3); in the control group there was no decrease versus baseline throughout the study. Between-group comparison showed a statistically significant difference at all times of assessment. For serum BAP, a statistically significant percent rise versus baseline was observed at months 3 and 6 in both the clodronate and control groups (NS between groups). At month 12, serum BAP declined toward baseline in both clodronate and control groups. Median percent changes in serum levels of markers of bone metabolism according to gender were consistent with BMD changes. In women, baseline serum CTX values were higher than those observed in men (Table 1) and a greater suppression was observed (Fig. 4) in treated women with respect to that seen in treated men (−68.1 and −47.9%, at 3 months, respectively). Untreated women showed a lower percentage of CTX reduction at 3 and 6 months compared to untreated men (−9.4 and 0.0% vs. −14.8 and −20.5%, respectively). Baseline serum BAP values were similar in women and men: The highest increase was observed at month 3 in untreated women (65%), followed by treated women (39%) and by men in control and clodronate groups (34 and 27.5%, respectively).
BAP and CTX during 1-year follow-up, assessed by the median and interquartile range (IQR) of percent changes from baseline, according to gender and treatment. A statistically significant difference (* P < 0.05) in CTX was seen at months 3, 6, and 12 between untreated and clodronate-treated women. Women CLD clodronate-treated women; Men CLD clodronate-treated men; Women CNT untreated women; Men CNT untreated men
Adverse Events, Tolerability, and Compliance
A total of 13 adverse events were reported during the study: three (all nonserious) in three patients out of 42 under clodronate (7.1%) and 10 (four serious) in 10 patients in the control group (20.4%). Events involving the skeletal system were all within the control group: implantation of prosthesis at the contralateral hip, fracture of the radium, prosthesis dislocation, and fracture of the femur (as a consequence of a fall at the prosthesis side). Laboratory assessments at the end of the study did not reveal differences between study groups with respect to the number of values out of the reference range. Intramuscular clodronate at the dose of 100 mg weekly was well tolerated by patients, although pain at the injection site was experienced by nearly 50% of patients at least at some administrations. However, compliance to treatment was high both during the first 10-day period with a daily administration and then after, to month 12, when administration was weekly. Patients underwent a mean of 94.3% (SD 18.6) and 94.2% (SD 9.2) of due administrations in the two periods, respectively.
Discussion
The pattern of periprosthetic bone loss shown in this study confirms previously reported observations [7–14]. Bone loss after THA occurred mainly within the first 3 months and was greater in the proximal and middle Gruen zones (1, 2, 6, and 7); after the third month, there was partial recovery, mostly evident in the distal zones. The greatest bone loss (up to 29% at month 12) was found in the medial proximal region of the femur (Gruen zone 7).
A 12-month treatment with clodronate reduced the overall bone loss (+1.7% in the net average value compared to controls) and resulted in bone sparing ranging from 2.3% (Gruen zone 3) to 6.5% (Gruen zones 2 and 7); statistical significance was reached at Gruen zones 2 and 6. On the whole, the greatest BMD increase in treated patients was seen in the zones where a higher bone loss was observed. Areas such as zones 4 and 5, which had shown a lower rate of bone loss after 3 months and BMD values above baseline levels after 12 months following surgery, were found to have a lower increase in BMD following clodronate administration compared to controls (−1.9 and −1.6%, respectively). The efficacy of clodronate treatment was confirmed by BMD changes in some areas of the contralateral hip, resulting in lower reduction of bone density in treated patients.
As expected, clodronate treatment also resulted in a significant suppression of serum CTX versus baseline and controls throughout the study period; BAP was shown to increase in both groups during the first 6 months, suggesting that clodronate does not interfere with bone apposition and forming processes that take place postoperatively [30].
Studies already published on the prevention of bone loss with bisphosphonates [15–22] differ in the duration of follow-up, sample size, treatment scheme and dosage, patient characteristics and method of reporting. In a small study of five untreated versus eight treated patients with uncemented prosthesis, alendronate, at a dose of 10 mg daily, showed a lower bone loss of around 13 and 7.5% in Gruen zones 6 and 7, respectively, after 6 months of therapy [17]. Yamaguchi et al. [18] reported lower bone loss of around 15.5% in zone 7 and 7% in zone 6 compared to controls after 12 months of therapy with cyclic etidronate at a dose of 400 mg/daily for 2 weeks every 12 weeks, while Fokter et al. [19] failed to reach a statistically significant difference between the etidronate-treated group and controls in any of the Gruen zones using the same dosage scheme. Pamidronate as a single-dose infusion of 90 mg [20] led to a suppression of bone loss that was shown to be maximal 3 months after surgery, while risedronate reduced, over placebo, postoperative bone resorption after cementless THA by around 7 and 8% in zones 6 and 7, respectively, after 6 months of therapy at a dose of 2.5 mg/day [21].
Study data were also analyzed according to gender, showing a greater bone loss and response to therapy in the female population. Although gender is included among predicting factors, a sex-related difference in bone loss after THA has not been previously widely investigated or reported. Since the percentage in change of bone loss after THA has been shown to be inversely correlated with preoperative BMD, which is usually lower in women with respect to men of matching age, a failure to observe differences between women and men should be interpreted. Aldinger et al. [10] showed no differences between men and women in change of relative BMD value during an 84-month longitudinal study; the authors commented that the patients followed in their study included women in premenopause, a condition with less rapid bone loss. Venesmaa et al. [14] reported no statistically significant difference in total BMD changes in the operated hip between women and men; however, the P value of their comparison was close to significance (P = 0.07), and the total initial BMD of their population was higher than that reported in our study (1.76 g/cm2 in men and 1.45 g/cm2 in women vs. 1.33 and 1.07 g/cm2). Furthermore, the comparison was not referred to areas were a higher bone loss usually occurs, and interestingly, they found a significant difference between sexes in the nonoperated hip (P = 0.003). In their work, Rahmy et al. [13] reported a P value close to significance for gender as an independent variable of bone loss in Gruen zone 7 (P = 0.09), whereas this trend was not observed with respect to total BMD or bone loss at Gruen zone 4.
All females recruited into our study had to be postmenopausal according to inclusion criteria, which may explain the observation that baseline periprosthetic and contralateral BMD were lower in females compared to recruited men (of similar age), with almost double the mean value of the bone resorption marker CTX.
After THA, an immediate (limited to 6 weeks) postoperative elevation of bone resorption was described [30] in a sample of 27 women and 26 men, with a decline to baseline value and below thereafter (−22.2% after 16 weeks and −17.1% at 24 weeks); a positive correlation between the highest level of serum CTX (at postoperative week 3) and bone loss after 1 year was also found [31]. The persistence of high levels of CTX seen in our study after 3 and 6 months in untreated women compared to untreated men (−9.4 and 0.0% vs. −14.8 and −20.5%, respectively) may reflect in postmenopausal women more intense and prolonged osteoclast activity in the postoperative period.
The difference in clodronate activity that we have seen between women and men could therefore be explained by the more intense bone turnover that women would undergo before and after implantation. The higher bone turnover level of our female population would be confirmed by the higher decrease in bone density that was found also in the contralateral hip, a finding observed in some works [32] but not in others [19, 22]. The lower benefit from prevention with clodronate that we observed in men could be explained by a lower contribution of osteoclastic reaction to bone loss in the male patients included in our study, particularly in the early postoperative phase.
To our knowledge, the evaluation of bisphosphonates in bone loss prevention after THA, according to gender, was reported in only one work, where no statistically significant differences between male and female patients were observed [22]. However, although baseline data according to sex were not reported, as it is possible to presume them from the whole population data, the female patients recruited into the Wilkinson et al. [22] study appear to be younger with respect to ours (58 years in placebo and 57 in treated groups vs. 66 and 64, respectively) and with a higher baseline net proximal femur BMD (1.77 g/cm2 in placebo and 1.45 g/cm2 in treated groups vs. 1.33 and 1.07 g/cm2). Bone turnover in the female patients recruited into the above-mentioned study, therefore, seems to be lower with respect to our female population.
Our data confirm that patients may differ in the risk for bone loss after THA, suggesting that response to preventive therapy also could vary. Postmenopausal women, in particular, seem to represent a population with a higher level of risk for BMD reduction that will benefit more from clodronate administration. In fact, several risk factors for periprosthetic bone loss are generally found in postmenopausal women: a lower baseline bone mass, an unfavorable bone–stem size ratio, and a higher bone turnover. According to this, an even more pronounced bone loss and therefore a more beneficial effect from preventive treatment could be expected in osteoporotic females.
The study has some limitations. Different prosthetic designs were included; however, being that all the prostheses were uncemented, a generalization of our results to all stems with this type of surface may be allowed. DXA scans were performed locally at each study center; although reading of scans was centralized to increase consistency, this may have caused higher data variability, probably precluding the data reaching statistical significance in some comparisons. Furthermore, the trial was not double-blinded, a placebo was not used, and a supplement of calcium and vitamin D was given only to patients with osteoporosis.
In conclusion, 1-year administration of intramuscular clodronate at the dose of 100 mg weekly after THA resulted in a reduction of periprosthetic bone loss similar to that reported in previous studies with other bisphosphonates, and this supports its role in the prevention of bone loss after hip replacement.
A gender-specific analysis of data demonstrated that postmenopausal women were at a higher risk for bone loss and that they showed greater benefit from therapy. This observation further indicates the need to carry out studies to better identify those patients who may be at higher risk for bone loss following hip arthroplasty and who may therefore show greater benefit from therapy.
References
Chang RW, Pellisier JM, Hazen GB (1996) A cost–effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA 275:858–865
Furnes O, Lie A, Espehaug B, Vollset E, Engesaeter LB, Havelin I (2001) Hip disease, the prognosis of total hip replacements. A review of 53, 698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987–99. J Bone Joint Surg Br 83:579–586
Harris WH (2001) Wear and periprosthetic osteolysis: the problem. Clin Orthop 393:66–70
Sundfeldt M, Carlsson LV, Johansson CB, Thomsen P, Gretzer C (2006) Aseptic loosening, not only a question of wear: a review of different theories. Acta Orthop 77:177–197
Ries MD (2003) Complications in primary total hip arthroplasty: avoidance and management: wear. Instr Course Lect 52:257–265
Haynes DR, Crotti TN, Potter AE, Loric M, Atkins GJ, Howie DW, Findlay DM (2001) The osteoclastogenic molecules RANKL and RANK are associated with periprosthetic osteolysis. J Bone Joint Surg Br 83-B:902–911
Trevisan C, Bigoni M, Randelli G, Marinoni EC, Peretti G, Ortolani S (1997) Periprosthetic bone density around fully hydroxyapatite coated femoral stem. Clin Orthop 340:109–117
Massari L, Bagni B, Biscione R, Traina GC (1996) Periprosthetic bone density in uncemented femoral hip implants with proximal hydroxyapatite coating. Bull Hosp Jt Dis 54:206–210
Brodner W, Bitzan P, Lomoschitz F, Krepler P, Jankovsky R, Lehr S, Kainberger F, Gottsauner-Wolf F (2004) Changes in bone mineral density in the proximal femur after uncemented total hip arthroplasty: a five-year longitudinal study. J Bone Joint Surg Br 86-B:20–26
Aldinger PR, Sabo D, Pritsch M, Thomsen M, Mau H, Ewerbeck V, Breusch SJ (2003) Pattern of periprosthetic bone remodelling around stable uncemented tapered hip stems: a prospective 84-month follow-up study and a median 156-month cross-sectional study with DXA. Calcif Tissue Int 73:2115–2121
Yamaguchi KY, Masuhara K, Yamasaki S, Nakai T, Fuji T (2003) Predictive value of a preoperative biochemical bone marker in relation to bone remodelling after cementless total hip arthroplasty. J Clin Densitom 6:259–265
Ohta H, Kobayashi S, Saito N, Nawata M, Horiuchi H, Takaoka K (2003) Sequential changes in periprosthetic bone mineral density following total hip arthroplasty: a 3-year follow-up. J Bone Miner Metab 21:229–233
Rahmy AIA, Gosens T, Blake GM, Tonino A, Fogelman GM (2004) Periprosthetic bone remodelling of two types of uncemented femoral implant with proximal hydroxyapatite coating: a 3-year follow-up study addressing the influence of prosthesis design and preoperative bone density on periprosthetic bone loss. Osteoporos Int 15:281–289
Venesmaa PK, Kröger HP, Miettinen HJ, Jurvelin JS, Suomalainen OT, Alhava EM (2001) Monitoring of periprosthetic BMD after uncemented total hip arthroplasty with dual-energy X-ray absorptiometry-a 3-year follow-up study. J Bone Miner Res 16:1056–1061
Bhandari M, Bajammal S, Guyatt GH, Griffith L, Busse JW, Schünemann H, Einhorn TA (2005) Effect of bisphosphonates on periprosthetic bone mineral density after total joint arthroplasty. A meta-analysis. J Bone Joint Surg Am 87:293–301
Arabmotlagh M, Rittmeister M, Hennigs T (2006) Alendronate prevents femoral periprosthetic bone loss following total hip arthroplasty: prospective, randomized, double-blind study. J Orthop Res 24:1836–1841
Venesmaa PK, Kröger HPJ, Miettinen HJA, Jurvelin JS, Suomalainen OT, Alhava EM (2001) Alendronate reduces periprosthetic bone loss after uncemented primary total hip arthroplasty: a prospective randomized study. J Bone Miner Res 16:2126–2131
Yamaguchi K, Masuhara K, Yamasaki S, Nakai T, Fuji T (2003) Cyclic therapy with etidronate has a therapeutic effect against local osteoporosis after uncemented total hip arthroplasty. Bone 33:144–149
Fokter SK, Komadina R, Repse-Fokter A, Yerby SA, Kocijancic A, Marc J (2005) Etidronate does not suppress periprosthetic bone loss following cemented hip arthroplasty. Int Orthop 29:362 336
Wilkinson JM, Stockley I, Peel NFA, Hamer AJ, Elson RA, Barrigton NA, Eastell R (2001) Effects of pamidronate in preventing local bone loss after total hip arthroplasty: a randomized, double-blind, controlled trial. J Bone Miner Res 16:556–564
Yamasaki S, Masuhara K, Yamaguchi K, Nakai T (2007) Risedronate reduces postoperative bone resorption after cementless total hip arthroplasty. Osteoporos Int 18:1009–1015
Wilkinson JM, Eagleton AC, Stockley I, Peel NFA, Hamer AJ, Eastell R (2005) Effect of pamidronate on bone turnover and implant migration after total hip arthroplasty: a randomized trial. J Orthop Res 23:1–8
Rossini M, Braga V, Gatti D, Gerardi D, Zamberlan N, Adami S (1999) Intramuscular clodronate therapy in postmenopausal osteoporosis. Bone 24:125–129
McCloskey E, Selby P, Davies M, Robinson J, Francis RM, Adams J, Kayan K, Beneton M, Jalava T, Pylkkänen L, Kenraali J, Aropuu S, Kanis JA (2004) Clodronate reduces vertebral fracture risk in women with postmenopausal or secondary osteoporosis: results of a double-blind, placebo-controlled 3-year study. J Bone Miner Res 19:728–736
McCloskey EV, Beneton M, Charlesworth D, Kayan K, deTakas D, Dey A, Orgee J, Ashford R, Forster M, Cliffe J, Kersh L, Brazier J, Nichol J, Aropuu S, Jalava T, Kanis JA (2007) Clodronate reduces the incidence of fractures in community-dwelling elderly women unselected for osteoporosis: results of a double-blind, placebo controlled randomized study. J Bone Miner Res 22:135–141
Makkonen N, Salminen A, Rogers MJ, Frith JC, Urtti A, Azhayeva E, Monkkonene J (1999) Contrasting effects of alendronate and clodronate on RAW 264 macrophages: the role of bisphosphonate metabolite. Eur J Pharm Sci 8:109–118
Bonabello A, Galmozzi MR, Bruzzese T, Zara GP (2001) Analgesic effect of bisphosphonates in mice. Pain 91:269–275
Hilding M, Aspenberg P (2006) Postoperative clodronate decreases prosthetic migration: 4-year follow-up of a randomized radiostereometric study of 50 total knee patients. Acta Orthop 77:912–916
Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop 141:17–27
Schneider U, Schmidt-Rohlfing B, Knopf U, Breusch SJ (2002) Effects upon bone metabolism following total hip and total knee arthroplasty. Pathobiology 70:26–33
Arabmotlagh M, Sabljic R, Rittmeister M (2006) Changes of the biochemical markers of bone turnover and periprosthetic bone remodelling after cemented hip arthroplasty. J Arthrop 21:129–134
Kröger H, Vanninen E, Overmyer M, Miettinen H, Rushton N, Suomalainen O (1997) Periprosthetic bone loss and regional bone turnover in uncemented total hip arthroplasty: a prospective study using high resolution single photon emission tomography and dual-energy X-ray absorptiometry. J Bone Miner Res 12:487–492
Acknowledgements
The study was funded by SPA-Società Prodotti Antibiotici (Milan, Italy). The authors are grateful to Patrizio Sala, BSc, of Data Management & Biometry (Cremona, Italy) for his support in data management and statistics.
Author information
Authors and Affiliations
Corresponding author
Additional information
P. Romano is employed by SPA-Società Prodotti Antibiotici. All other authors have stated that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Trevisan, C., Ortolani, S., Romano, P. et al. Decreased Periprosthetic Bone Loss in Patients Treated with Clodronate: A 1-Year Randomized Controlled Study. Calcif Tissue Int 86, 436–446 (2010). https://doi.org/10.1007/s00223-010-9356-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-010-9356-1