Abstract
Previously, our group described an antihypertensive peptide (Ala-His-Ile-Ile-Ile, MW: 565.3 Da) with angiotensin I-converting enzyme inhibitory and vasodilatory effects that was purified from Styela clava flesh tissue. In the present study, we investigated the metabolic effects of the antihypertensive peptide in skeletal muscle cells. We found that the antihypertensive peptide stimulated glucose uptake in differentiated L6 rat myoblast cells in a dose-dependent manner. Inhibition of AMP-activated protein kinase (AMPK) by compound C significantly inhibited the antihypertensive peptide-stimulated glucose uptake. Western blotting analyses revealed that the antihypertensive peptide stimulated AMPK phosphorylation and this enhancement could be specifically inhibited by compound C. Furthermore, the current study demonstrates that translocation of glucose transporter-4 (GLUT4) to the plasma membrane was stimulated by the antihypertensive peptide. In summary, the findings from this study suggest that the antihypertensive peptide may have beneficial effects on the glucose metabolism in skeletal muscle cells via a mechanism involving AMPK and possible stimulation of the intrinsic activity of GLUT4 transporter.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Insulin resistance develops when tissues in the body (skeletal muscle, adipose/fat, and liver) become less sensitive and ultimately resistant to insulin, the hormone that is produced by the β-cells in the pancreas [1, 2]. Furthermore, insulin resistance is a major defect underlying the development of type II diabetes and is a central factor in the development of the metabolic syndrome, a group of abnormalities including obesity and hypertension [3, 4]. Among all the tissues in the body, the skeletal muscle tissue is majorly responsible, accounting for 75–80 %, for insulin-stimulated glucose uptake in the postprandial state; it also plays a pivotal role in maintaining glucose homeostasis [5, 6]. In skeletal muscle tissue, insulin stimulates glucose uptake primarily by increasing the translocation of the glucose transporter-4 (GLUT4) from the internal membrane to the plasma membrane [7, 8]. The signaling mechanism by which insulin stimulates muscle glucose uptake is well known and involves binding of insulin to its receptor, phosphorylation of downstream insulin receptor substrates (IRS), and activation of phosphatidylinositol-3 kinase (PI3-K) and protein kinase B (Akt), which promotes GLUT4 translocation from a cellular pool in the plasma membrane [5, 9, 10]. AMP-activated protein kinase (AMPK) complex, a αβγ heterotrimer that functions as a cellular energy sensor, has been positively correlated with increased muscle glucose uptake, and in recent years, it has emerged as an attractive pharmacological agent for the treatment of insulin resistance and type II diabetes [5, 11, 12]. In skeletal muscles, AMPK is activated by exercise/contraction and numerous compounds including thiazolidinediones [13], metformin [14], and resveratrol [5], resulting in the stimulation of glucose uptake. The study of new compounds that activate AMPK and stimulate skeletal muscle glucose uptake is important, because the knowledge obtained from such studies could be used toward the development of treatments for insulin resistance and type II diabetes [6].
Hypertension is associated with insulin resistance and glucose intolerance. Increased skeletal muscle blood flow and the resulting improvements in insulin delivery are important mechanisms by which attenuation of the renin–angiotensin system (RAS) improves glucose uptake [15]. One potential mechanism involves the inhibition of angiotensin I-converting enzyme (ACE), which increases nitric oxide (NO) generation and enhances glucose transportation activity in skeletal muscles [15, 16]. In our previous studies, we purified and identified an antihypertensive peptide derived from S. clava flesh tissue and successfully demonstrated its ACE inhibitory effect and NO-mediated vasorelaxation [17, 18]. In the present study, we examined the effects of the antihypertensive peptide on glucose uptake and GLUT4 translocation and attempted to elucidate the mechanism of action underlying the antihypertensive peptide’s effects in L6 skeletal muscle cells.
Materials and methods
Materials
The rat myoblast cell line L6 was purchased from the Korean Cell Line Bank (KCLB; Seoul, KOREA). DMEM (Dulbecco’s modified Eagle’s medium), wortmannin, and compound C were purchased from Sigma (St. Louis, MO, USA). Antibodies against AMP-activated protein kinase (AMPK), phospho-AMPK (Thr172), and glucose transporter-4 (GLUT4) were from Cell Signaling Technology (Bedford, Massachusetts, USA). Second IgG HRP-linked antibodies were from Santa Cruz Biotechnology (Santa Cruz, CA, USA). The other chemicals and reagents used were of analytical grade.
Purification and identification of the purified peptide and peptide synthesis
To extract the purified peptide from S. clava flesh tissue, a hydrolysis was performed using Protamex, a commercial food grade enzyme, under optimal conditions [17]. The Protamex hydrolysate was fractionated through ultrafiltration membranes with molecular weight (MW) cutoff of 5 kDa. The below 5 kDa fraction was again filtered and applied to a column saturated in Sephadex G-25 resin, which was previously equilibrated with distilled water. Further fractions were collected with a fraction collector. The fraction exhibiting the highest antihypertensive effect was further purified using reverse-phase HPLC on an octadecyl silica (ODS) column. Finally, the fraction with the greatest antihypertensive effect was collected; this was followed by identification of the amino acid sequence. Amino acid sequence of the purified peptide was identified as Ala-His-Ile-Ile-Ile (AHIII), with a molecular weight 565.3 Da.
Synthesis of antihypertensive peptide
In order to validate the glucose uptake of the antihypertensive peptide, a synthetic peptide with the same sequence was synthesized and tested. The antihypertensive peptide was chemically synthesized in the peptide synthesizer facility PepTron Inc. (Daejeon, Korea). The peptide was synthesized using the Fmoc solid-phase method with a peptide synthesizer (PeptrEX-R48, Peptron Inc., Daejeon, Korea). The synthetic peptide was purified using HPLC (SHIMADZU, Kyoto, Japan) on a Capcell Pak C18 column (Shiseido, Tokyo, Japan). The column was developed at a flow rate of 1.0 mL/min by a linear gradient of acetonitrile (0–20 %, 2 min; 20–50 %, 10 min; 50–80 %, 2 min) containing 0.1 % trifluoroacetic acid. The identity of peptide was confirmed by mass analysis using LC–MS (Agilent Technologies, CA, USA), and the purity of synthetic peptide was confirmed over 95 %.
Cell culture
Rat myoblast L6 cells were maintained in high-glucose DMEM supplemented with 10 % heat-inactivated FBS, penicillin (100 U/mL), and streptomycin (100 μg/mL). Cultures were maintained at 37 °C in 5 % CO2 incubator. For differentiation, the cells were seeded in appropriate culture plates, and after sub-confluence (about 80 %), the medium was changed to DMEM containing 2 % horse serum for 7 days, with medium changes every day. All experiments were performed in differentiated L6 myotubes after 7 days.
MTT assay
The cytotoxicity of antihypertensive peptide against the L6 cells was determined by a colorimetric MTT assay. Cells were seeded in a 24-well plate. After 24 h, the cells were treated with various concentrations (25, 50, 100, and 200 μM) of the antihypertensive peptide. The cells were then incubated for an additional 24 h at 37 °C. MTT stock solution (100 μL; 2 mg/mL in PBS) was then added to each well. After incubating for 4 h, the plate was centrifuged at 2000 rpm for 10 min and the supernatant was aspirated. The formazan crystals in each well were dissolved in DMSO. The amount of purple formazan was determined by measuring the absorbance at 540 nm.
Glucose uptake assay
L6 cells were seeded in a 24-well plate. After differentiation, the cells were starved in serum-free low-glucose DMEM for 12 h and then washed with PBS and incubated with fresh serum-free low-glucose DMEM. After that, the cells were treated with insulin (100 nM) for 1 h, or the indicated concentrations (to determine the dose response of L6 myotubes to antihypertensive peptide) of antihypertensive peptide. Glucose uptake was measured by glucose concentration in the medium solution using glucose oxidase assay kit (Asan Pharmaceutical corp., Korea).
In some experiments, 100 nM of Wortmannin (PI3 kinase inhibitor) and 10 μM of compound C (AMPK inhibitor) were added 30 min before the antihypertensive peptide treatment.
Western blot analysis
L6 myotubes were grown in 100-mm dishes and were starved in serum-free low-glucose DMEM for 12 h prior to treatment with the indicated agents. Following treatment, the media were aspirated and the cells were washed twice in ice-cold PBS. The cell lysates were prepared with lysis buffer (20 mM Tris, 5 mM EDTA, 10 mM Na4P2O7, 100 mM NaF, 2 mM Na3VO4, 1 % NP-40, 25 μg/mL aprotinin, 25 μg/mL leupeptin, and 1 mM PMSF) for 60 min and then centrifuged at 12,000 rpm for 15 min at 4 °C. The protein concentrations were determined by using BCA™ protein assay kit. The lysate containing 30 μg of protein was subjected to electrophoresis on sodium dodecyl sulfate (SDS)-polyacrylamide gel, and the gel was transferred onto a nitrocellulose membrane. The membranes were blocked in 5 % nonfat dry milk in TBST (25 mM Tris–HCl, 137 mM NaCl, 2.65 mM KCl, 0.05 % Tween 20, pH 7.4) for 2 h. The primary antibodies were used at a 1:1000 dilution. Membranes incubated with the primary antibodies at 4 °C for overnight. And then the membranes were washed with TBST and then incubated with the secondary antibodies used at 1:3000 dilutions. Signals were developed using an ECL Western blotting detection kit and exposed to X-ray films.
Plasma membrane fractionation and immunoblot analysis
L6 myotubes were treated with the indicated agents and harvested. The cell lysates were prepared with lysis buffer [250 mM sucrose, 20 mM HEPES (pH 7.4), 10 mM KCl, 1.5 mM MgCl2, 1 mM EDTA, 1 mM EGTA, 1 mM dithiothreitol (DTT), and protease inhibitors (1 mM PMSF, 25 μg/mL aprotinin, and 25 μg/mL leupeptin)] and kept on ice for 10 min. The cell lysate was ultracentrifuged at 22,000 rpm for 1 h at 4 °C. The pallet was re-suspended in a lysis buffer and kept on ice for 10 min and then centrifuged at 8000 rpm for 5 min at 4 °C to obtain plasma membrane fraction from the middle layer of the supernatant. Immunoblot analyses of GLUT4 described in the method to 2.7.
Statistical analysis
All data were represented as the mean ± SD. Statistical comparisons of the mean values were performed by analysis of variance (ANOVA), followed by Duncan’s multiple-range test using SPSS (11.5) software. Statistical significance was considered at p < 0.05.
Results
The antihypertensive peptide, AHIII, does not affect the viability of L6 skeletal muscle cells
Prior to evaluating the glucose uptake of the antihypertensive peptide, we first examined its cytotoxic effect on the viability of L6 skeletal muscle cells. Cytotoxicity of different concentrations of the peptide AHIII (25, 50, 100, and 200 μM) was evaluated using the MTT assay. Compared to the control, AHIII did not have significant cytotoxic effects on L6 skeletal muscle cells (Fig. 1). Based on these findings, the above-mentioned concentrations were used for subsequent experiments.
The antihypertensive peptide stimulates glucose uptake in dose-dependent manner
Differentiated L6 skeletal muscle cells were used to determine the role of the peptide in the glucose metabolism. It was found that AHIII dose-dependently stimulated glucose uptake as shown in Fig. 2, and the effect at a 200 μM concentration was comparable to that of insulin; the antihypertensive peptide may have metabolic effects in skeletal muscle cells.
Antihypertensive peptide dose-dependently stimulates glucose uptake in L6 skeletal muscle cells. Cells were starved in serum-free media for 6 h and incubated for 1 h with increasing in antihypertensive peptide and insulin. The values are expressed as the mean ± standard deviation of triplicate experiments. *p < 0.05 indicate significant differences compared with the untreated group
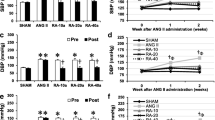
The antihypertensive peptide activates AMPK pathway in L6 skeletal muscle cells
To investigate the pathway responsible for the effect of the antihypertensive peptide on glucose uptake in L6 cells, the cells were pretreated with wortmannin, an inhibitor of phosphatidylinositol (PI)-3 kinase and compound C, a selective AMPK inhibitor. As shown in Fig. 3, compound C significantly inhibited the glucose uptake stimulated by peptide AHIII (200 μM). Further, the effect of AHIII on AMPK activation was investigated. We found that AHIII induced increased AMPK phosphorylation in L6 skeletal muscle cells (Fig. 4). However, the increase in AMPK phosphorylation was inhibited by a 30-min pretreatment of the cells with compound C (Fig. 4). Taken together, the findings strongly indicate that the antihypertensive peptide plays a metabolic role in skeletal muscle cells via the AMPK pathway.
Antihypertensive peptide-induced increase in glucose uptake was reduced by wortmannin and compound C. After 6-h starvation, L6 skeletal muscle cells were pretreated with or without 100 nM wortmannin (phosphatidylinositol (PI)-3 kinase inhibitor) and 10 μM compound C (AMPK inhibitor) for 30 min and then treated with 200 μM of antihypertensive peptide for 1 h. The values are expressed as the mean ± standard deviation of triplicate experiments. *P < 0.05 versus untreated group or between two groups as indicated
Effect of the antihypertensive peptide on AMPK signaling pathway. Cells were pretreated with or without 10 μM compound C for 30 min and then treated with the indicated concentrations of the antihypertensive peptide and insulin for 1 h and 10 min, respectively. The cell lysates were analyzed via Western blotting using anti-phospho-AMPK (Thr172) and anti-AMPK. The values are expressed as the mean ± standard deviation of triplicate experiments. *P < 0.05 versus untreated group or between two groups as indicated
The antihypertensive peptide stimulates glucose uptake by increasing GLUT4 translocation through the AMPK pathway
We examined the effect of the antihypertensive peptide on the AMPK signaling pathway responsible for the translocation of GLUT4 to the plasma membrane and increased glucose uptake. After L6 skeletal muscle cells were treated with peptide AHIII for 4 h, GLUT4 translocation was determined. As seen in Fig. 5, AHIII treatment markedly increased GLUT4 translocation to the plasma membrane of L6 skeletal muscle cells. However, the increased GLUT4 translocation to the plasma membrane of AHIII-treated L6 skeletal muscle cells was almost completely abolished by compound C pretreatment. These results suggest that the antihypertensive peptide stimulates GLUT4 translocation to the plasma membrane possibly via activation of the AMPK pathway.
Effect of the antihypertensive peptide on GLUT4 translocation to the plasma membrane. Cells were pretreated with or without 10 μM compound C for 30 min and then treated with the indicated concentrations of the antihypertensive peptide and insulin for 1 h and 10 min, respectively. The cell lysates were analyzed via Western blotting using anti-GLUT4. The values are expressed as the mean ± standard deviation of triplicate experiments. *P < 0.05 versus untreated group or between two groups as indicated
Discussion
Type II diabetes poses a major threat to human health worldwide and is the most common type of diabetes [19]. The available drugs for type II diabetes have a number of limitations, including adverse effects and high rates of secondary failure. In recent years, biological resources have become the focus of a considerable amount of attention from researchers searching for alternative therapies for diabetes [20, 21] because they are typically considered less toxic and to have fewer side effects than synthetic drugs do. Hence, the identification and characterization of bioactive peptides from biological sources have become increasingly important and are of great interest to researchers [22].
Generally, skeletal muscles play an important role in the regulation of energy balance and glucose metabolism [23]. Hence, L6 skeletal muscle cells were used to evaluate the antidiabetic properties of the antihypertensive peptide derived from S. clava flesh tissue. To our knowledge, this is the first report of an antihypertensive peptide that significantly stimulates glucose uptake. It is important to note that this study is particularly relevant owing to the effects observed in skeletal muscle cells.
As mentioned previously, glucose uptake in skeletal muscle tissue can be mediated by at least two major mechanisms: (1) through insulin-dependent activation of PI3-K/Akt and (2) the activation of AMPK by muscle contraction due to exercise in order to maintain the energy balance [24, 25]. Our findings in L6 skeletal muscle cells show that a significant increase in glucose uptake occurs owing to the antihypertensive peptide via the PI3-K/Akt pathway in the absence of insulin. In the presence of wortmannin, a selective PI3-K/Akt inhibitor, the antihypertensive peptide did not affect the PI3-K/Akt pathway. In contrast, compound C significantly reduced glucose uptake in L6 skeletal muscle cells.
AMPK plays a key role in energy homeostasis in ATP-depleting metabolic states such as ischemia, hypoxia, heart shock, oxidative stress, and especially exercise [26, 27]. Once activated under such conditions, it accelerates ATP-generating catabolic pathways including glucose uptake and fatty acid oxidation through direct regulation of key metabolic enzymes [28]. In recently published studies, it has been reported that AMPK serves as a key metabolic sensor through cellular regulation of insulin-independent glucose uptake and glycogen metabolism [29]. Thus, AMPK is emerging as a potential target for the treatment of diabetes, especially because it could play a principal role in the exercise-induced adaptation of skeletal muscles, type II diabetes, obesity, and the metabolic syndrome [23, 30]. The present study showed a significant increase in AMPK phosphorylation by the antihypertensive peptide. Further, the antihypertensive peptide-mediated activation of AMPK is abolished by pretreatment of compound C, a highly selective AMPK inhibitor. Additionally, the peptide-induced increase in GLUT4 translocation to the plasma membrane suggests its involvement in AMPK regulation of glucose metabolism in L6 skeletal muscle cells.
In summary, these results demonstrate that the antihypertensive peptide improves glucose uptake via activation of the AMPK pathway in skeletal muscles. In particular, skeletal muscles play a major role in the regulation of energy balance [29] and are the primary tissues involved in glucose uptake and disposal.
In conclusion, the antihypertensive peptide increases glucose uptake via activation of the AMPK pathway and may potentially emerge as a novel target for the treatment of type II diabetes.
References
Carr DB, Utzschneider KM (2004) Intra-abdominal fat is a major determinant of NCEP ATP III criteria for the metabolic syndrome. Diabetes 53:2087–2094
Hu G, Qiao Q, Tuomilehto J, Eliasson M, Feskens EJ, Pyörälä K (2004) Plasma insulin and cardiovascular mortality in non-diabetic European men and women: a meta-analysis of data from eleven prospective studies. The DECODE Insulin Study Group. Diabetologia 47:1245–1256
Hotamisligil GS (2006) Inflammation and metabolic disorders. Nature 444:860–867
Moller DE, Flier JS (1992) Insulin resistance: mechanisms, syndromes, and implications. N Engl J Med 325:938–942
Breen DM, Sanli T, Giacca A, Tsiani E (2008) Stimulation of muscle cell glucose uptake by resveratrol through sirtuins and AMPK. Biochem Biophys Res Commun 374:117–122
Zygmunt K, Faubert B, MacNeil J, Tsiani E (2010) Naringenin, a citrus flavonoid, increases muscle cell glucose uptake via AMPK. Biochem Biophys Res Commun 398:178–183
Stephens JM, Pilch PF (1995) The metabolic regulation and vesicular transport of GLUT4, the major insulin-responsive glucose transporter. Endocr Rev 16:529–546
Zaid H, Antonescu CN, Randhawa VK, Klip A (2008) Insulin action on glucose transporters through molecular switches, tracks and tethers. Biochem J 413:201–215
Dugani CB, Randhawa VK, Cheng AW, Patel N, Klip A (2008) Selective regulation of the perinuclear distribution of glucose transporter 4 (GLUT4) by insulin signals in muscle cells. Eur J Cell Biol 87:337–351
Taniguchi CM, Emanuelli B, Kahn CR (2006) Critical nodes in signaling pathways: insights into insulin action. Nat Rev Mol Cell Biol 7:85–96
Kim JH, Lee JO, Lee SK, Jung JH, You GY, Park SH, Park M, Kim SD, Kim HS (2010) Clozapine activates AMP-activated protein kinase (AMPK) in C2C12 myotube cells and stimulates glucose uptake. Life Sci 87:42–48
Rogers NH, Witczak CA, Hirshman MF, Goodyear LJ, Greenberg AS (2009) Estradiol stimulates Akt, AMP-activated protein kinase (AMPK) and TBC1D1/4, but not glucose uptake in rat soleus. Biochem Biophys Res Commun 382:646–650
Konrad D, Rudich A, Bilan PJ, Patel N, Richardson C, Witters LA, Klip A (2005) Troglitazone causes acute mitochondrial membrane depolarisation and an AMPK-mediated increase in glucose phosphorylation in muscle cells. Diabetologia 48:954–966
Zou MH, Kirkpatrick SS, Davis BJ, Nelson JS, Wiles WG, Schlattner U, Neumann D, Brownlee M, Freeman MB, Goldman MH (2004) Activation of the AMP-activated protein kinase by the anti-diabetic drug metformin in vivo role of mitochondrial reactive nitrogen species. J Biol Chem 279:43940–43951
Stump CS, Hamiton MT, Sowers JR (2006) Effect of antihypertensive agents on the development of type 2 diabetes mellitus. Mayo Clin Proc 81:796–806
Henriksen EJ, Jacob S (2003) Modulation of metabolic control by angiotensin converting enzyme (ACE) inhibition. J Cell Physiol 196:171–179
Ko SC, Lee JK, Byun HG, Lee SC, Jeon YJ (2012) Purification and characterization of angiotensin I-converting enzyme inhibitory peptide from enzymatic hydrolysates of Styela clava flesh tissue. Process Biochem 47:34–40
Ko SC, Kim DG, Han CH, Lee YJ, Lee JK, Byun HG, Lee SC, Park SJ, Lee DH, Jeon YJ (2012) Nitric oxide-mediated vasorelaxation effects of anti-angiotensin I-converting enzyme (ACE) peptide from Styela clava flesh tissue and its anti-hypertensive effect in spontaneously hypertensive rats. Food Chem 134:1141–1145
Zimmet P, Alberti K, Shaw J (2001) Global and societal implications of the diabetes epidemic. Nature 414:782–787
Chang MS, Oh MS, Kim DR, Jung KJ, Park S, Choi SB, Ko BS, Park SK (2006) Effects of Okchun-San, a herbal formulation, on blood glucose levels and body weight in a model of type 2 diabetes. J Ethnopharmacol 103:491–495
Jung UJ, Baek NI, Chung HG, Bang MH, Yoo JS, Jeong TS, Lee KT, Kang YJ, Lee MK, Yeo JY, Choi MS (2007) The anti-diabetic effects of ethanol extract from two variants of Artemisia princeps Pampanini in C57BL/KsJ-db/db mice. Food Chem Toxicol 45:2022–2029
Sarmadi BH, Ismail A (2010) Antioxidant peptides from food proteins: a review. Peptides 31:1949–1956
Lee SH, Kang SM, Ko SC, Lee DH, Jeon YJ (2012) Octaphlorethol A, a novel phenolic compound isolated from a brown alga, Ishige foliacea, increases glucose transporter 4-mediated glucose uptake in skeletal muscle cells. Biochem Biophys Res Commun 420:576–581
Lee MS, Hwang JT, Kim S, Yoon S, Kim MS, Yang HJ, Kwon DY (2010) Ginsenoside Rc, an active component of Panax ginseng, stimulates glucose uptake in C2C12 myotubes through an AMPK-dependent mechanism. J Ethnopharmacol 127:771–776
Ito Y, Obara K, Ikeda R, Ishii M, Tanabe Y, Ishikawa T, Nakayama K (2006) Passive stretching produces Akt-and MAPK-dependent augmentations of GLUT4 translocation and glucose uptake in skeletal muscles of mice. Pflugers Arch 451:803–813
Harder J, Bartels J, Christophers E, Schroder JM (2001) Isolation and characterization of human β-defensin-3, a novel human inducible peptide antibiotic. J Biol Chem 276:5707–5713
Raj PA, Dentino AR (2002) Current status of defensins and their role in innate and adaptive immunity. FEMS Microbiol Lett 206:9–18
Sheetz MJ, King GL (2002) Molecular understanding of hyperglycemia’s adverse effects for diabetic complications. JAMA 288:2579–2588
Ozcan U, Yilmaz E, Ozcan L, Furuhashi M, Vailancourt E, Smith RO, Gorgun CZ, Hotamosligil GS (2006) Chemical chaperones reduce ER stress and restore glucose homeostasis in a mouse model of type 2 diabetes. Science 313:1137–1140
Nakatani Y, Kaneto H, Kawamori D, Yoshiuchi K, Hatazaki M, Matsuoka K, Ozawa K, Ogawa S, Hori M, Yamasaki Y, Matsuhisa M (2005) Involvement of endoplasmic reticulum stress in insulin resistance and diabetes. J Biol Chem 280:847–851
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2012R1A1A2005479), and also supported Marine Biotechnology Program (20150220) Funded by Ministry of Oceans and Fisheries, Republic of Korea.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None.
Compliance with Ethics Requirements
This article does not contain any studies with human or animal subjects.
Rights and permissions
About this article
Cite this article
Ko, SC., Kim, JI., Park, SJ. et al. Antihypertensive peptide purified from Styela clava flesh tissue stimulates glucose uptake through AMP-activated protein kinase (AMPK) activation in skeletal muscle cells. Eur Food Res Technol 242, 163–170 (2016). https://doi.org/10.1007/s00217-015-2526-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00217-015-2526-7