Abstract
Rationale
Parkinson’s disease (PD) is characterized as a chronic and progressive neurodegenerative disorder, and PD patients have non-motor features such as depressive symptoms. Although there are several available medications to treat PD symptoms, these medications do not prevent the progression of the disease.
Objective
(R)-ketamine has greater and longer-lasting antidepressant effects than (S)-ketamine in animal models of depression. This study was undertaken to investigate whether two enantiomers of ketamine and its metabolite norketamine shows neuroprotective effects in an animal model of PD.
Methods
Effects of (R)-ketamine, (S)-ketamine, and their metabolites on MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine)-induced reduction of dopamine transporter (DAT) and tyrosine hydroxylase (TH) in the mouse striatum and substantia nigra (SNr) were examined.
Results
MPTP-induced reduction of DAT in the striatum was attenuated by subsequent repeated intranasal administration of both enantiomers of ketamine although (R)-ketamine was more potent than (S)-ketamine. MPTP-induced reduction of TH in the striatum and SNr was attenuated by administration of (R)-ketamine, but not (S)-ketamine. Interestingly, MPTP-induced reduction of DAT in the striatum was also attenuated by a single intranasal administration of (R)-ketamine. In contrast, MPTP-induced reduction of DAT in the striatum was not attenuated by repeated intranasal administration of two enantiomers of norketamine. Furthermore, the pretreatment with TrkB antagonist ANA-12 significantly blocked the neuroprotective effects of (R)-ketamine in the MPTP-induced reduction of DAT in the striatum.
Conclusions
These findings suggest that (R)-ketamine can protect against MPTP-induced neurotoxicity in the mouse brain via TrkB activation. Therefore, (R)-ketamine could represent a therapeutic drug for neurodegenerative disorders such as PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is a common and progressive neurodegenerative disease that affects predominately dopamine-producing neurons in substantia nigra (SNr) (Ascherio and Schwarzschild 2016; Kalia and Lang 2015). Although there are medications available to treat motor symptoms in PD patients, these compounds do not prevent the progression of the disease. There are no compounds with a disease-modifying or neuroprotective indication for PD (Dehay et al. 2015; Kieburtz et al. 2018). Therefore, the development of new drugs possessing disease-modifying and/or neuroprotective properties is an unmet medical need.
Depressive symptoms are common in patients with PD, and influence many other clinical aspects of the disease (Cummings 1992; Goodarzi et al. 2016; Schapira et al. 2017). Accumulating evidence demonstrated that N-methyl-D-aspartate receptor (NMDAR) antagonist (R,S)-ketamine exhibits rapid-onset and sustained antidepressant effects in treatment-resistant patients with depression (Berman et al. 2000; Hashimoto 2019; Kishimoto et al. 2016; Murrough et al. 2017; Newport et al. 2015; Zarate et al. 2006; Zhang and Hashimoto 2019). (R,S)-ketamine is a racemic mixture containing equal parts of (R)-ketamine (arketamine) and (S)-ketamine (esketamine). (S)-ketamine has an approximately 4-fold greater affinity for the NMDAR than (R)-ketamine (Ebert et al. 1997) (Fig. 1B). On March 5, 2019, US Food Drug Administration approved (S)-ketamine nasal spray for treatment-resistant depression. In contrast, preclinical studies demonstrated that (R)-ketamine showed greater potency and longer lasting antidepressant effects than (S)-ketamine in different animal models of depression (Fukumoto et al. 2017; Yang et al. 2015, 2017a, b, 2018a; Zanos et al. 2016; Zhang et al. 2014). Interestingly, (R)-ketamine induced a more potent beneficial effect on decreased dendritic spine density, brain-derived neurotrophic factor (BDNF)-TrkB signaling and synaptogenesis in the prefrontal cortex (PFC), CA3, and dentate gyrus (DG) of hippocampus from rodents with depression-like phenotype compared with (S)-ketamine (Yang et al. 2015). Given the comorbidity of depression in PD, we have a hypothesis that (R)-ketamine may have neuroprotective effects in an animal model of PD.
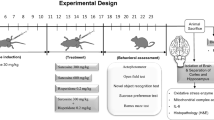
Schedule of treatment and chemical structure of ketamine and norketamine. a Schedule of treatment. Mice were randomly divided into four groups: control group, MPTP + saline group, MPTP + (R)-ketamine group, MPTP + (S)-ketamine group. MPTP (10 mg/kg × 3, 2-h interval. 9:00, 11:00 and 13:00) or saline (5 ml/kg × 3, 2-h interval) was injected intraperitoneally (i.p.) into mice. Saline (0.5 ml/kg), (R)-ketamine (10 mg/kg) or (S)-ketamine (10 mg/kg) was administered intranasally 3 h after the final administration of saline or MPTP. Subsequently, saline (0.5 ml/kg), (R)-ketamine (10 mg/kg) or (S)-ketamine (10 mg/kg) were injected intranasally at 16:00 for additional 6 days (days 2–7). On day 8, mice were deeply anesthetized with isoflurane and perfused for immunohistochemistry of DAT and TH. IN, intranasal. b Chemical structure of two enantiomers of ketamine, its major metabolite norketamine. The values in parentheses are the inhibitor constant values (Ki values) for NMDAR (Ebert et al. 1997)
Brain imaging studies demonstrated loss of dopamine transporter (DAT) in the caudate putamen from PD patients (Booij et al. 1997; Innis et al. 1993). Furthermore, biochemical studies on postmortem brain samples from PD patients showed the reduction of DAT in the striatum and TH in the SNr of PD patients (Miller et al. 1997; Nagatsu and Sawada 2007). Recent meta-analysis of brain imaging studies show that the density of DAT in the caudate putamen from PD patients are significantly lower than those of healthy control subjects (Kaasinen and Vahlberg 2017; Martini et al. 2018). Interestingly, it is likely that the measurement of the density of DAT using brain imaging is a useful imaging biomarker of the severity of PD (Takahashi et al. 2019).
The purpose of this study was to examine the effects of two enantiomers of ketamine in an animal model of PD using the neurotoxin MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) (Jackson-Lewis and Przedborski 2007). First, we examined the effects of (R)-ketamine and (S)-ketamine in the dopaminergic neurotoxicity in the mouse striatum after repeated administration of MPTP. Second, we examined the effects of (R)-norketamine and (S)-norketamine, major metabolites of ketamine enantiomers, in the MPTP-induced dopaminergic neurotoxicity in the mouse striatum. Finally, we examined the role of TrkB signaling in the neuroprotective effects of (R)-ketamine in MPTP-treated mice since brain-derived neurotrophic factor (BDNF)-TrkB system is shown to play a role in the antidepressant effects of (R)-ketamine (Yang et al. 2015, 2018a).
Methods and materials
Animals
Male adult C57BL/6 mice, aged 12 weeks (body weight 25–30 g, Japan SLC, Inc., Hamamatsu, Japan) were used. Animals were housed under controlled temperatures and 12 h light/dark cycles (lights on between 07:00 and 19:00 h), with ad libitum food (CE-2; CLEA Japan, Inc., Tokyo, Japan) and water. This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health, USA. The protocol was approved by the Chiba University Institutional Animal Care and Use Committee (permission number: 29-370 and 30-309). All efforts were made to minimize suffering.
Drugs
1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP: Tokyo Chemical Industry CO., LTD., Tokyo, Japan) was dissolved in saline. (R)-(+)-ketamine hydrochloride and (S)-(−)-ketamine hydrochloride were prepared by recrystallization of (R,S)-ketamine (Ketalar®, ketamine hydrochloride, Daiichi Sankyo Pharmaceutical Ltd., Tokyo, Japan) and D-(−)-tartaric acid and L-(+)-tartaric acid, respectively (Zhang et al. 2014). (R)-norketamine hydrochloride and (S)-norketamine hydrochloride were prepared as reported previously (Zanos et al. 2016; Yang et al. 2018b). The antidepressant dose (10 mg/kg as hydrochloride) dissolved in the physiological saline was used as previously reported (Yang et al. 2015, 2016, 2017a, b, 2018a, b). ANA-12 (N-[2-[[(Hexahydro-2-oxo-1H-azepin-3-yl)amino]carbonyl]phenyl]-benzo[b]thiophene-2-carboxamide: 0.5 mg/kg) (Maybridge, Ltd., Loughborough, Leicestershire, UK) were dissolved in phosphate-buffered saline containing 17% dimethylsulfoxide (DMSO), as previously reported (Cazorla et al. 2011; Ren et al. 2015; Yang et al. 2015; Zhang et al. 2015). Other reagents were purchased commercially.
MPTP-induced mouse model of PD
MPTP-induced neurotoxicity model was used as previously reported (Ren et al. 2018; Pu et al. 2019). Briefly, mice were randomly divided into four groups: (1): control group, (2): MPTP + saline group, (3): MPTP + (R)-ketamine group, (4): MPTP + (S)-ketamine group. MPTP (10 mg/kg × 3, 2-h interval. 9:00, 11:00 and 13:00) or saline (5 ml/kg × 3, 2-h interval) was injected into mice (Fig. 1A). Saline (0.5 ml/kg), (R)-ketamine (10 mg/kg) or (S)-ketamine (10 mg/kg) was administered intranasally 3 h after the final administration of saline or MPTP. Mice were restrained by hand, and saline or ketamine (or norketamine) was administered intranasally into awake mice using Eppendorf micropipette (Eppendorf Japan, Tokyo, Japan). Subsequently, saline, (R)-ketamine (10 mg/kg) or (S)-ketamine (10 mg/kg) were injected intranasally at 16:00 for additional 6 days (days 2–7) (Fig. 1A). On day 8, mice were deeply anesthetized with isoflurane and perfused transcardially with 10 ml of isotonic saline, followed by 40 ml of ice-cold 4% paraformaldehyde in 0.1 M phosphate buffer (pH 7.4). Brains were removed from the skulls and postfixed overnight at 4 °C, and brain was used for immunohistochemistry.
Second, mice were randomly divided into four groups: (1): control group, (2): MPTP + saline group, (3): MPTP + (R)-norketamine group, (4): MPTP + (S)-norketamine group. MPTP (10 mg/kg × 3, 2-h interval. 9:00, 11:00 and 13:00) or saline (5 ml/kg × 3, 2-h interval) was injected into mice. Saline (0.5 ml/kg), (R)-norketamine (10 mg/kg) or (S)-norketamine (10 mg/kg) was administered intranasally 3 h after the final administration of saline or MPTP. Subsequently, saline, (R)-norketamine (10 mg/kg) or (S)-norketamine (10 mg/kg) were injected intranasally at 16:00 for additional 6 days (days 2–7). On day 8, mice were deeply anesthetized with isoflurane and perfused as described above.
Third, mice were randomly divided into five groups: (1): control group, (2): MPTP + vehicle + saline group, (3): MPTP + vehicle + (R)-ketamine group, (4): MPTP + ANA-12 (0.5 mg/kg) + (R)-ketamine group, (5): MPTP + ANA-12 (0.5 mg/kg) + saline group. MPTP (10 mg/kg × 3, 2-h interval. 9:00, 11:00 and 13:00) or saline (5 ml/kg × 3, 2-h interval) was injected into mice. Subsequently, saline (0.5 ml/kg), or (R)-ketamine (10 mg/kg) were injected intranasally at 16:00 for additional 6 days (days 2–7). Vehicle (10 ml/kg) or ANA-12 (0.5 mg/kg) was injected intraperitoneally into mice 30 min before intranasal injection of saline or (R)-ketamine. On day 8, mice were deeply anesthetized with isoflurane and perfused and perfused as described above.
Immunohistochemistry of dopamine transporter and tyrosine hydroxylase
Immunohistochemistry of DAT and TH was performed as reported previously (Ren et al. 2014, 2018; Zhang et al. 2006). The mouse brain sections (Bregma 0.86–1.54 mm and − 2.92–3.88 mm) were identified according to stereotaxic coordinates in Paxinos and Franklin’ Mouse Brain (2002). Free-floating sections were treated with 0.3% H2O2 in 0.05 M Tris-HCl saline (TBS) for 30 min and blocked in TBS containing 0.2% Triton X-100 (TBST) and 1.5% normal serum for 1 h, at room temperature. Samples were then incubated for 36 h at 4 °C, with rat anti-DAT antibody (1:10,000, Merck Millipore, MA, USA) or rabbit anti-TH antibody (1:500, Sigma-Aldrich, MO, USA). The sections were washed three in TBST, and processed according to the avidin-biotin-peroxidase method (Vectastain Elite ABC, Vector Laboratories, Inc., Burlingame, CA, USA). Sections for DAT were then incubated for 5 min in a solution of 0.15 mg/ml diaminobenzidine, containing 0.06% nickel chloride and 0.01% H2O2. Sections for TH were then incubated for 5 min in a solution of 0.15 mg/ml diaminobenzidine, containing 0.01% H2O2. The sections were mounted on gelatinized slides, dehydrated, cleared, and coverslipped under Permount® (Fisher Scientific, Fair Lawn, NJ, USA). The staining intensity of DAT and TH in the anterior regions (0.25 mm2) of the striatum were imaged and analyzed using Keyence BZ-9000 Generation microscope (Keyence Co., Ltd., Osaka, Japan) and ImageJ software package. The number of TH-positive cells in the regions (0.36 mm2) of SNr was analyzed using Keyence BZ-9000 Generation microscope (Keyence Co., Ltd., Osaka, Japan).
Statistical analysis
The data show as the mean ± standard error of the mean (S.E.M.). Comparisons between groups were performed using the one-way analysis of variance (ANOVA), followed by Fisher’s least significant difference (LSD) test. The P-values of less than 0.05 were considered statistically significant.
Results
MPTP-induced reduction of DAT in the striatum was attenuated after subsequent repeated administration of (R)-ketamine and (S)-ketamine
First, we examined the effects of two enantiomers of ketamine on MPTP-induced dopaminergic neurotoxicity in the striatum. After repeated injections of saline or MPTP, saline, (R)-ketamine (10 mg/kg/day), or (S)-ketamine (10 mg/kg/day) was administered intranasally to mice. Subsequently, saline, (R)-ketamine or (S)-ketamine was administered intranasally to mice from day 2 to day 7 (Fig. 1A). Repeated administration of MPTP significantly reduced DAT-immunoreactivity in the striatum (Fig. 2A–D). Interestingly, MPTP-induced reduction of DAT in the striatum was significantly attenuated after subsequent repeated administration of both enantiomers of ketamine. Interestingly, efficacy of (R)-ketamine was significantly more potent than (S)-ketamine (Fig. 2E).
Effects of ketamine enantiomers on MPTP-induced reduction of DAT in the striatum. a–d Typical immunohistochemistry of DAT in the striatum. a Saline + saline. b MPTP + saline. c MPTP + (R)-ketamine. d MPTP + (S)-ketamine. e The data of DAT immunoreactivity in the striatum (one-way ANOVA F3,30 = 28.02, P < 0.001). Data are shown as mean ± S.E.M. (n = 8 or 10). **P < 0.01, ***P < 0.001 compared with MPTP + saline group. ###P < 0.001 compared to MPTP + (S)-ketamine group.
MPTP-induced reduction of TH in the striatum and SNr was attenuated after subsequent repeated administration of (R)-ketamine, but not (S)-ketamine
Repeated administration of MPTP significantly reduced TH-immunoreactivity in the striatum (Fig. 3A–D). Interestingly, MPTP-induced reduction of TH-immunoreactivity in the striatum was significantly attenuated after subsequent repeated administration of (R)-ketamine, but not (S)-ketamine (Fig. 3E). Furthermore, repeated administration of MPTP significantly reduced the number of TH-positive cells in the SNr (Fig. 3F–I). Interestingly, MPTP-induced reduction of the number of TH-positive cells in the SNr was significantly attenuated after subsequent repeated administration of (R)-ketamine, but not (S)-ketamine (Fig. 3J).
Effects of ketamine enantiomers on MPTP-induced reduction of TH-immunoreactivity in the striatum and SNr. a–d Typical immunohistochemistry of TH in the striatum. a Saline + saline. b MPTP + saline. c MPTP + (R)-ketamine. d MPTP + (S)-ketamine. e The data of TH immunoreactivity in the striatum (one-way ANOVA F3,30 = 15.26, P < 0.001). f–i Typical immunohistochemistry of TH in the SNr. f Saline + saline. g MPTP + saline. h MPTP + (R)-ketamine. i MPTP + (S)-ketamine. j The data of TH-positive cells in the SNr (one-way ANOVA F3,30 = 60.26, P < 0.001). Data are shown as mean ± S.E.M. (n = 8 or 10). ***P < 0.001 compared with MPTP + saline group. ##P < 0.01, ###P < 0.001 compared with MPTP + (S)-ketamine group. Scale bar = 50 μm
MPTP-induced reduction of DAT in the striatum was attenuated after subsequent single administration of (R)-ketamine
It is reported that (R)-ketamine has long-lasting antidepressant effects in rodents with depression-like phenotype (Yang et al. 2015, 2017a, b, 2018a; Shirayama and Hashimoto 2018). Therefore, we examined the effect of a single injection of (R)-ketamine on MPTP-induced reduction of DAT in the striatum. A single injection of (R)-ketamine significantly attenuated the MPTP-induced reduction of DAT in the striatum (Fig. 4).
Effects of a single dose of (R)-ketamine on MPTP-induced reduction of DAT in the mouse striatum. a Typical immunohistochemistry of DAT in the striatum from control group. b Typical immunohistochemistry of DAT in the striatum from MPTP + saline group. c Typical immunohistochemistry of DAT in the striatum from MPTP + (R)-ketamine group. d The data of DAT immunoreactivity in the striatum (one-way ANOVA F2,21 = 9.80, P = 0.001). Data are shown as mean ± S.E.M. (n = 8). **P < 0.01, ***P < 0.001 compared with MPTP + saline group
Lack of two enantiomers of norketamine in MPTP-induced reduction of DAT in the striatum
(R)-ketamine and (S)-ketamine are metabolized to (R)-norketamine and (S)-norketamine, respectively (Zanos et al. 2018; Yang et al. 2018b; Zhang and Hashimoto 2019) (Fig. 1B). We examined the effects of two enantiomers of norketamine on MPTP-induced dopaminergic neurotoxicity in the striatum. Both enantiomers of norketamine did not attenuate the MPTP-induced reduction of DAT in the striatum (Fig. 5). These data suggest that (R)-ketamine, but not its metabolite, can protect against MPTP-induced neurotoxicity in the striatum.
Lack of neuroprotective effects of (R)-norketamine and (S)-norketamine on MPTP-induced reduction of DAT in the mouse striatum. a Typical immunohistochemistry of DAT in the striatum from control group. b Typical immunohistochemistry of DAT in the striatum from MPTP + saline group. c Typical immunohistochemistry of DAT in the striatum from MPTP + (R)-norketamine group. d Typical immunohistochemistry of DAT in the striatum from MPTP + (S)-norketamine group. e The data of DAT immunoreactivity in the striatum (one-way ANOVA F3,19 = 5.85, P = 0.005). Data are shown as mean ± S.E.M. (n = 5 or 6). **P < 0.01 compared with control group
Role of TrkB signaling in the neuroprotective effects of (R)-ketamine for MPTP-induced neurotoxicity
It is reported that (R)-ketamine has rapid and long-lasting antidepressant effects via BDNF-TrkB signaling in the brain (Yang et al. 2015). Therefore, we examined the role of TrkB signaling in the protective effects of (R)-ketamine on MPTP-induced reduction of DAT in the striatum. Pretreatment with ANA-12 significantly blocked the protective effects of (R)-ketamine in the MPTP-induced neurotoxicity in the striatum. In contrast, ANA-12 alone did not affect MPTP-induced reduction of DAT in the striatum (Fig. 6).
Effects of ANA-12 in the neuroprotective effects of (R)-ketamine for MPTP-induced reduction of DAT in the mouse striatum. a Typical immunohistochemistry of DAT in the striatum from control group. b Typical immunohistochemistry of DAT in the striatum from MPTP + vehicle + saline group. c Typical immunohistochemistry of DAT in the striatum from MPTP + vehicle + (R)-ketamine group. d Typical immunohistochemistry of DAT in the striatum from MPTP + ANA-12 + (R)-ketamine group. e Typical immunohistochemistry of DAT in the striatum from MPTP + ANA-12 + saline group. f The data of DAT immunoreactivity in the striatum (one-way ANOVA F4,35 = 8.45, P < 0.001). Data are shown as mean ± S.E.M. (n = 6–9). *P < 0.05, **P < 0.01 compared with MPTP + vehicle + saline group. ###P < 0.001 compared with MPTP + ANA-12 + (R)-ketamine group
Discussion
The study suggests that (R)-ketamine would be a potential therapeutic drug for PD. The major findings of the present study are as follows: First, MPTP-induced reduction of DAT in the striatum was significantly attenuated by subsequent repeated intranasal administration of (R)-ketamine and (S)-ketamine although the efficacy of (R)-ketamine was significantly more potent that (S)-ketamine. Furthermore, MPTP-induced reduction of TH in the striatum and SNr was significantly attenuated by subsequent repeated intranasal administration of (R)-ketamine, but not (S)-ketamine. Interestingly, MPTP-induced reduction of DAT in the striatum was significantly attenuated by subsequent a single intranasal administration of (R)-ketamine, consistent with long-lasting antidepressant effects of (R)-ketamine (Shirayama and Hashimoto 2018; Yang et al. 2015, 2017a, b, 2018a). Second, MPTP-induced reduction of DAT in the striatum was not attenuated by subsequent repeated intranasal administration of major metabolites, (R)-norketamine or (S)-norketamine, suggesting that (R)-ketamine itself shows neuroprotective effects. Finally, the pretreatment with TrkB antagonist ANA-12 significantly blocked neuroprotective effects of (R)-ketamine in MPTP-induced model. Collectively, these findings suggest that (R)-ketamine can protect against MPTP-induced neurotoxicity via TrkB activation, and that (R)-ketamine might prove to be a promising prophylactic or therapeutic drug for PD.
The two enantiomers of ketamine share similar pharmacokinetic profiles (Fukumoto et al. 2017; Zanos et al. 2016), suggesting that the differential protective effects noted here between (R)-ketamine and (S)-ketamine are not due to differences in their pharmacokinetic profiles. In addition, (S)-ketamine (Ki = 0.30 μM) has an approximately 4-fold greater affinity for the NMDAR than the (R)-ketamine (Ki = 1.40 μM) (Fig. 1B) (Ebert et al. 1997). Furthermore, binding affinity of (S)-norketamine (Ki = 1.70 μM) and (R)-ketamine (Ki = 1.40 μM) at the NMDAR is similar (Fig. 1B) (Ebert et al. 1997). Although (S)-norketamine has antidepressant effects in animal models of depression (Hashimoto and Yang 2019; Yang et al. 2018b), both enantiomers of norketamine did not show protective effects against MPTP-induced neurotoxicity. It is therefore, unlikely that NMDAR plays a major role in the neuroprotective effects of (R)-ketamine in MPTP-induced model. To address this, further detailed studies examining the precise mechanisms underlying the neuroprotective effects of (R)-ketamine are needed.
It is suggested that DAT density in the caudate putamen from PD patients may be imaging biomarker for the severity of PD (Takahashi et al. 2019). From the current data, it is likely that (R)-ketamine might prevent or delay the progression of DAT reduction in PD patients, resulting in improvement of motor function in PD patients. Therefore, it is of great interest to investigate whether (R)-ketamine can prevent the progression of DAT reduction and motor function in early-stage PD patients since clinical trial of (R)-ketamine in humans is underway (Hashimoto 2019).
Accumulating evidence suggests that BDNF-TrkB signaling plays a key role in depression (Nestler et al. 2002; Hashimoto et al. 2004; Hashimoto 2010; Zhang et al. 2016). Previously, we reported that (R)-ketamine significantly attenuated reduced BDNF level in the PFC, CA3 and DG in mice with depression-like phenotype (Yang et al. 2015). Interestingly, ANA-12, a TrkB antagonist, was able to block the antidepressant effects of (R)-ketamine, suggesting a role for BDNF-TrkB signaling in (R)-ketamine’s long-lasting antidepressant mechanism. In addition, Zhu et al. (2015) reported that repeated administration of MPTP caused the reduction of BDNF in the mouse brain, suggesting that decreased BDNF-TrkB signaling may play a role in the MPTP-induced neurotoxicity. In this study, we found that (R)-ketamine can protect against MPTP-induced neurotoxicity via TrkB activation. Furthermore, ANA-12 alone did not affect the DAT density in the striatum of control naïve mice (Ren et al. 2014). Collectively, it is likely that (R)-ketamine exerts neuroprotective effects by activating BDNF-TrkB signaling in the striatum and SNr. Nonetheless, further detailed studies underlying the neuroprotective effects of (R)-ketamine in animal models of PD are necessary.
The psychotomimetic effects and dissociative symptoms in humans after ketamine infusion are well known (Short et al. 2018; Singh et al. 2017; Sanacora et al. 2017). Unlike (S)-ketamine, (R)-ketamine might not induce psychotomimetic side effects or exhibit abuse potential in rodents (Chang et al. 2019; Yang et al. 2015, 2016). In addition, unlike (R,S)-ketamine and (S)-ketamine, (R)-ketamine did not cause the expression of heat shock protein HSP-70 (a marker for neuronal injury) in the rat retrosplenial cortex after a single administration (Tian et al. 2018). A positron emission tomography study using conscious monkey showed a marked reduction of dopamine D2/3 receptor binding in the striatum after a single infusion of (S)-ketamine, but not (R)-ketamine (Hashimoto et al. 2017), suggesting that (S)-ketamine-induced dopamine release might be associated with acute psychotomimetic and dissociative side effects in humans (Hashimoto et al. 2017). Interestingly, it is suggested that (S)-ketamine contributes to the acute psychotomimetic and dissociative effects of ketamine, whereas (R)-ketamine may not be associated with these side effects (Vollenweider et al. 1997; Zanos et al. 2018). In the conditioned place preference test, abuse liability of (R)-ketamine in rodents is lower than (S)-ketamine (Yang et al. 2015; Chang et al. 2019). Taken all together, (R)-ketamine could be a safer drug in humans than (R,S)-ketamine and (S)-ketamine (Hashimoto 2016a, b, c, 2019).
In conclusion, this study shows that (R)-ketamine, but not (S)-ketamine, protects against MPTP-induced neurotoxicity in the mouse brain. Furthermore, TrkB antagonist ANA-12 blocked neuroprotective effects of (R)-ketamine in MPTP-induced neurotoxicity, suggesting a role of TrkB in the neuroprotective effects of (R)-ketamine. Therefore, (R)-ketamine appears to be a new prophylactic or therapeutic drug for neurodegenerative disorders such as PD.
References
Ascherio PA, Schwarzschild MA (2016) The epidemiology of Parkinson’s disease: risk factors and prevention. Lancet Neurol 15:1257–1272
Berman RM, Cappiello A, Anand A, Oren DA, Heninger GR, Charney DS, Krystal JH (2000) Antidepressant effects of ketamine in depressed patients. Biol Psychiatry 47:351–354
Booij J, Tissingh G, Boer GJ, Speelman D, Stoof JC, Janssen AG, Woilters EC, van Royen EA (1997) [123I]FP-CIT SPECT shows a pronounced decline of striatal dopamine transporter labelling in early and advanced Parkinson’s disease. J Neurol Neurosurg Psychiatry 62:133–140
Cazorla M, Prémont J, Mann A, Girard N, Kellendonk C, Rognan D (2011) Identification of a low–molecular weight TrkB antagonist with anxiolytic and antidepressant activity in mice. J Clin Invest 121:1846–1857
Chang L, Zhang K, Pu Y, Qu Y, Wang SM, Xiong Z, Ren Q, Dong C, Fujita Y, Hashimoto K (2019) Comparison of antidepressant and side effects in mice after intranasal administration of (R,S)-ketamine, (R)-ketamine, and (S)-ketamine. Pharmacol Biochem Behav 181:53–59
Cummings JL (1992) Depression and Parkinson’s disease: a review. Am J Psychiatry 149:443–454
Dehay B, Bourdenx M, Gorry P, Przedborski S, Vila M, Hunot S, Singleton A, Olanow CW, Merchant KM, Bezard E, Petsko GA, Meissner WG (2015) Targeting α-synuclein for treatment of Parkinson’s disease: mechanistic and therapeutic considerations. Lancet Neurol 14:855–866
Ebert B, Mikkelsen S, Thorkildsen C, Borgbjerg FM (1997) Norketamine, the main metabolite of ketamine, is a non-competitive NMDA receptor antagonist in the rat cortex and spinal cord. Eur J Pharmacol 333:99–104
Fukumoto K, Toki H, Iijima M, Hashihayata T, Yamaguchi JI, Hashimoto K, Chaki S (2017) Antidepressant potential of (R)-ketamine in rodent models: comparison with (S)-ketamine. J Pharmacol Exp Ther 361:9–16
Goodarzi Z, Mrklas KJ, Roberts DJ, Jette N, Pringsheim T, Holroyd-Leduc J (2016) Detecting depression in Parkinson disease: a systematic review and meta-analysis. Neurology 87:426–437
Hashimoto K (2010) Brain-derived neurotrophic factor as a biomarker for mood disorders: an historical overview and future directions. Psychiatry Clin Neurosci 64:341–357
Hashimoto K (2016a) Letter to the editor: R-ketamine: a rapid-onset and sustained antidepressant without risk of brain toxicity. Psychol Med 46:2449–2451
Hashimoto K (2016b) Ketamine’s antidepressant action: beyond NMDA receptor inhibition. Expert Opin Ther Targets 20:1389–1392
Hashimoto K (2016c) Detrimental side effects of repeated ketamine infusions in the brain. Am J Psychiatry 173:1044–1045
Hashimoto K (2019) Rapid-acting antidepressant ketamine, its metabolites and other candidates: a historical overview and future perspective. Psychiatry Clin Neurosci 2019. https://doi.org/10.1111/pcn.12902
Hashimoto K, Yang C (2019) Is (S)-norketamine an alternative antidepressant for esketamine? Eur Arch Psychiatry Clin Neurosci 2018. https://doi.org/10.1007/s00406-018-0922-2
Hashimoto K, Shimizu E, Iyo M (2004) Critical role of brain-derived neurotrophic factor in mood disorders. Brain Res Brain Res Rev 45:104–114
Hashimoto K, Kakiuchi T, Ohba H, Nishiyama S, Tsukada H (2017) Reduction of dopamine D2/3 receptor binding in the striatum after a single administration of esketamine, but not R-ketamine: a PET study in conscious monkeys. Eur Arch Psychiatry Clin Neurosci 267:173–176
Innis RB, Seibyl JP, Scanley BE, Laruelle M, Abi-Dargham A, Wallace E, Baldwin RM, Zea-Ponce Y, Zoghbi S, Wang S (1993) Single photon emission computed tomographic imaging demonstrates loss of striatal dopamine transporters in Parkinson disease. Proc Natl Acad Sci U S A 90:11965–11969
Jackson-Lewis V, Przedborski S (2007) Protocol for the MPTP mouse model of Parkinson’s disease. Nat Protoc 2:141–151
Kaasinen V, Vahlberg T (2017) Striatal dopamine in Parkinson disease: a meta-analysis of imaging studies. Ann Neurol 82:873–882
Kalia LV, Lang AE (2015) Parkinson’s disease. Lancet 386:896–912
Kieburtz K, Katz R, Olanow CW (2018) New drugs for Parkinson’s disease: the regulatory and clinical development pathways in the United States. Mov Disord 33:920–927
Kishimoto T, Chawia JM, Hagi K, Zarate CA, Kane JM, Bauer M, Correll CU (2016) Single-dose infusion ketamine and non-ketamine N-methyl-D-aspartate receptor antagonists for unipolar and bipolar depression: a meta-analysis of efficacy, safety and time trajectories. Psychol Med 46:1459–1472
Martini A, Dal Lago D, Edelstyn NMJ, Salgarello M, Lugoboni F, Tamburin S (2018) Dopaminergic neurotransmission in patients with Parkinson’s disease and impulse control disorders: a systematic review and meta-analysis of PET and SPECT studies. Front Neurol 9:1018
Miller GW, Staley JK, Heilman CJ, Perez JT, Mash DC, Eye DB, Levey AI (1997) Immunochemical analysis of dopamine transporter protein in Parkinson’s disease. Ann Neurol 41:530–539
Murrough JW, Abdallah CG, Mathew SJ (2017) Targeting glutamate signaling in depression: progress and prospects. Nat Rev Drug Discov 16:472–486
Nagatsu T, Sawada M (2007) Biochemistry of postmortem brains in Parkinson’s disease: historical overview and future prospects. J Neural Transm Suppl 72:113–120
Nestler EJ, Barrot M, DiLeone RJ, Eisch AJ, Gold SJ, Monteggia LM (2002) Neurobiology of depression. Neuron 34:13–25
Newport DJ, Carpenter LL, McDonald WM, Potash JB, Tohen M, Nemeroff CB, APA Council of Research Task Force on Novel Biomarkers and Treatments (2015) Ketamine and other NMDA antagonists: early clinical trials and possible mechanisms in depression. Am J Psychiatry 172:950–966
Paxinos G, Franklin K (2002) Paxinos and Franklin’s the mouse brain in stereotaxic coordinates, 4th edn. Academic Press, Cambridge
Pu Y, Qu Y, Chang L, Wang SM, Zhang K, Ushida Y, Suganuma H, Hashimoto K (2019) Dietary intake of glucoraphanin prevents the reduction of dopamine transporter in the mouse striatum after repeated administration of MPTP. Neuropsychopharmacol Rep 2019. https://doi.org/10.1002/npr2.12060
Ren Q, Zhang JC, Ma M, Fujita Y, Wu J, Hashimoto K (2014) 7,8-Dihydroxyflavone, a TrkB agonist, attenuates behavioral abnormalities and neurotoxicity in mice after administration of methamphetamine. Psychopharmacology 231:159–166
Ren Q, Ma M, Yang C, Zhang JC, Yao W, Hashimoto K (2015) BDNF–TrkB signaling in the nucleus accumbens shell of mice has key role in methamphetamine withdrawal symptoms. Transl Psychiatry 5:e666
Ren Q, Ma M, Yang J, Nonaka R, Yamaguchi A, Ishikawa KI, Kobayashi K, Murayama S, Hwang SH, Saiki S, Akamatsu W, Hattori N, Hammock BD, Hashimoto K (2018) Soluble epoxide hydrolase plays a key role in the pathogenesis of Parkinson’s disease. Proc Natl Acad Sci U S A 115:E5815–E5823
Sanacora G, Frye MA, McDonald W, Mathew SJ, Turner MS, Schatzberg AF, Summergrad P, Nemeroff CB, American Psychiatric Association (APA) Council of Research Task Force on Novel Biomarkers and Treatments (2017) A consensus statement on the use of ketamine in the treatment of mood disorders. JAMA Psychiatry 74:399–405
Schapira AHV, Chaudhuri KR, Jenner P (2017) Non-motor features of Parkinson disease. Nat Rev Neurosci 18:435–450
Shirayama Y, Hashimoto K (2018) Lack of antidepressant effects of (2R,6R)-hydroxynorketamine in a rat learned helplessness model: comparison with (R)-ketamine. Int J Neuropsychopharmacol 21:84–88
Short B, Fong J, Galvez V, Shelker W, Loo CK (2018) Side-effects associated with ketamine use in depression: a systematic review. Lancet Psychiatry 5:65–78
Singh I, Morgan C, Curran V, Nutt D, Schlag A, McShane R (2017) Ketamine treatment for depression: opportunities for clinical innovation and ethical foresight. Lancet Psychiatry 4:419–426
Takahashi H, Watanabe Y, Tanaka H, Mochizuki H, Kato H, Hatazawa J, Tomiyama N (2019) Quantifying the severity of Parkinson disease by use of dopaminergic neuroimaging. AJR Am J Roentgenol 213:163–168. https://doi.org/10.2214/AJR.18.20655
Tian Z, Dong C, Fujita A, Fujita Y, Hashimoto K (2018) Expression of heat shock protein HSP-70 in the retrosplenial cortex of rat brain after administration of (R,S)-ketamine and (S)-ketamine, but not (R)-ketamine. Pharmacol Biochem Behav 172:17–21
Vollenweider FX, Leenders KL, Øye I, Hell D, Angst J (1997) Differential psychopathology and patterns of cerebral glucose utilization produced by (S)- and (R)-ketamine in healthy volunteers using positron emission tomography (PET). Eur Neuropsychopharmacol 7:25–38
Yang C, Shirayama Y, Zhang JC, Ren Q, Yao W, Ma M, Hashimoto K (2015) R-ketamine: a rapid-onset and sustained antidepressant without psychotomimetic side effects. Transl Psychiatry 5:e632
Yang C, Han M, Zhang JC, Ren Q, Hashimoto K (2016) Loss of parvalbumin-immunoreactivity in mouse brain regions after repeated intermittent administration of esketamine, but not R-ketamine. Psychiatry Res 239:281–283
Yang C, Qu Y, Abe M, Nozawa D, Chaki S, Hashimoto K (2017a) (R)-ketamine shows greater potency and longer lasting antidepressant effects than its metabolite (2R,6R)-hydroxynorketamine. Biol Psychiatry 82:e43–e44
Yang C, Qu Y, Fujita Y, Ren Q, Ma M, Dong C, Hashimoto K (2017b) Possible role of the gut microbiota-brain axis in the antidepressant effects of (R)-ketamine sin a social defeat stress model. Transl Psychiatry 7:1294
Yang C, Ren Q, Qu Y, Zhang JC, Ma M, Dong C, Hashimoto K (2018a) Mechanistic target of rapamycin–independent antidepressant effects of (R)-ketamine in a social defeat stress model. Biol Psychiatry 83:18–28
Yang C, Kobayashi S, Nakao K, Dong C, Han M, Qu Y, Ren Q, Zhang JC, Ma M, Toki H, Yamaguchi JI, Chaki S, Shirayama Y, Nakazawa K, Manabe T, Hashimoto K (2018b) AMPA receptor activation-independent antidepressant actions of ketamine metabolite (S)-norketamine. Biol Psychiatry 84:591–600
Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI, Alkondon M, Yuan P, Pribut HJ, Singh NS, Dossou KS, Fang Y, Huang XP, Mayo CL, Wainer IW, Albuquerque EX, Thompson SM, Thomas CJ, Zarate CA Jr, Gould TD (2016) NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Nature 533:481–486
Zanos P, Moaddel R, Morris PJ, Riggs LM, Highland JN, Georgiou P, Pereira EFR, Albuquerque EX, Thomas CJ, Zarate CA Jr, Gould TD (2018) Ketamine and ketamine metabolite pharmacology: insights into therapeutic mechanisms. Pharmacol Rev 70:621–660
Zarate CA, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, Charney DS, Manji HK (2006) A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry 63:856–864
Zhang K, Hashimoto K (2019) An update on ketamine and its two enantiomers as rapid-acting antidepressants. Expert Rev Neurother 19:83–92
Zhang L, Kitaichi K, Fujimoto Y, Nakayama H, Shimizu E, Iyo M, Hashimoto K (2006) Protective effects of minocycline on behavioral changes and neurotoxicity in mice after administration of methamphetamine. Prog Neuro-Psychopharmacol Biol Psychiatry 30:1381–1393
Zhang JC, Li SX, Hashimoto K (2014) R (−)-ketamine shows greater potency and longer lasting antidepressant effects than S (+)-ketamine. Pharmacol Biochem Behav 116:137–141
Zhang JC, Yao W, Dong C, Yang C, Ren Q, Ma M, Han M, Hashimoto K (2015) Comparison of ketamine, 7, 8-dihydroxyflavone, and ANA-12 antidepressant effects in the social defeat stress model of depression. Psychopharmacology 232:4325–4335
Zhang JC, Yao W, Hashimoto K (2016) Brain-derived neurotrophic factor (BDNF)-TrkB signaling in inflammation-related depression and potential therapeutic targets. Curr Neuropharmacol 14:721–731
Zhu G, Li J, He L, Wang X, Hong X (2015) MPTP-induced changes in hippocampal synaptic plasticity and memory are prevented by memantine through the BDNF-TrkB pathway. Bri J Pharmacol 172:2354–2368
Funding
This study was supported by AMED (to K.H., JP19dm0107119).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Hashimoto is an inventor on a filed patent application on “The use of (R)-ketamine in the treatment of psychiatric diseases,” “(S)-norketamine and salt thereof as pharmaceutical,” and “The use of (R)-ketamine in the treatment of neurodegenerative diseases” by Chiba University. Dr. Hashimoto has received research support from Dainippon-Sumitomo, Otsuka, and Taisho. Other authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fujita, A., Fujita, Y., Pu, Y. et al. MPTP-induced dopaminergic neurotoxicity in mouse brain is attenuated after subsequent intranasal administration of (R)-ketamine: a role of TrkB signaling. Psychopharmacology 237, 83–92 (2020). https://doi.org/10.1007/s00213-019-05346-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-019-05346-5