Abstract
Background
Resistance to antidepressant drug treatment remains a major health problem. Animal models of depression are efficient in detecting effective treatments but have done little to increase the reach of antidepressant drugs. This may be because most animal models of depression target the reversal of stress-induced behavioural change, whereas treatment-resistant depression is typically associated with risk factors that predispose to the precipitation of depressive episodes by relatively low levels of stress. Therefore, the search for treatments for resistant depression may require models that incorporate predisposing factors leading to heightened stress responsiveness.
Method
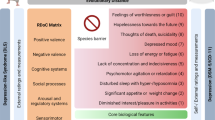
Using a diathesis-stress framework, we review developmental, genetic and genomic models against four criteria: (i) increased sensitivity to stress precipitation of a depressive behavioural phenotype, (ii) resistance to chronic treatment with conventional antidepressants, (iii) a good response to novel modes of antidepressant treatment (e.g. ketamine; deep brain stimulation) that are reported to be effective in treatment-resistant depression and (iv) a parallel to a known clinical risk factor.
Results
We identify 18 models that may have some potential. All require further validation. Currently, the most promising are the Wistar-Kyoto (WKY) and congenital learned helplessness (cLH) rat strains, the high anxiety behaviour (HAB) mouse strain and the CB1 receptor knockout and OCT2 null mutant mouse strains.
Conclusion
Further development is needed to validate models of antidepressant resistance that are fit for purpose. The criteria used in this review may provide a helpful framework to guide research in this area.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Depression is one of the major causes of ill-health and economic burden worldwide, and the need to develop effective and efficient therapies has never been greater. However, after half a century of intensive research since antidepressant drugs were introduced into clinical practice, their efficacy remains stubbornly low, at around 70 % (compared with a no-treatment recovery rate of around 50 %); the onset of action remains stubbornly slow, at around 4–6 weeks; and with very few exceptions, drugs newly introduced into clinical practice have been ‘me-too’ variants of existing drugs: there has been almost no progress towards the identification of novel targets to improve these clinical parameters (Belzung 2014).
The past two decades have seen remarkable progress in understanding the nature of the abnormalities of information processing that characterise depression, the changes in neural activity that accompany those changes and the relationships between the psychopathology and pathophysiology of depression (Willner et al. 2013; Belzung et al. 2015). As part of this endeavour, research using animal models of depression has proven invaluable in the development of an understanding of the cellular and neuroanatomical changes underpinning these psychophysiological relationships and in establishing in detail the mechanism of action of antidepressant drugs (Willner et al. 2013). This only increases the sense of frustration arising from the failure of such research to discover novel drugs to extend the reach of antidepressant therapy into the populations of patients who show little or no benefit. Animal models of depression have been of immense value in advancing an understanding of how antidepressants work and improving their side effect profile, and their continuing importance in these contexts is indisputable. However, the purpose of this paper is to explore a radical thesis: that in relation to the problem of treatment-resistant depression specifically (i.e. the situation in which antidepressants do not work), the animal models of depression in current use are not fit for purpose and a different approach is needed.
Animal models of depression
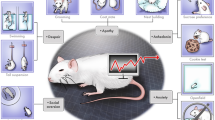
Animal models of psychiatric states may be defined as procedures applied to laboratory animals that engender behavioural changes which are intended to be homologous to aspects of psychiatric disorders, and can therefore be used as experimental tools to further the understanding of human psychopathology (Willner 2009). Animal models are developed for specific investigational purposes. The primary aim of early research was to elucidate psychological processes, but models are now used largely to address neurobiological issues, including the mechanisms of action of psychotherapeutic drugs; the neurotransmitter, neuroreceptor and intracellular changes underlying psychiatric states; the neuroanatomical basis of psychiatric states, and increasingly, questions about the role of specific genes; and of course, the evaluation of the potential psychotherapeutic value of novel pharmacological and non-pharmacological interventions.
According to this definition, animal models of psychopathology involve two elements: an input (a procedure used to elicit abnormal behaviour) and an output (a behavioural endpoint, often associated with biomarkers such as neuroendocrine changes, that is used to measure its effect). The inputs to the model may involve environmental manipulations (e.g. exposure to social or physical stressors, or training regimes), and/or alteration of the internal environment (e.g. by brain lesions or administration of psychotropic drugs), and/or identification of vulnerable individuals (by selective breeding or genomic methods). The behavioural endpoint represents a model of a process (or symptom) that is thought to be important in the disorder. Even if researchers often have the explicit intention to develop models of a pathology, the reality is that these models are typically limited in scope: they simulate specific aspects, reflected in the behavioural endpoint, rather than the entirety of the disorder. However, it may be found subsequently that further aspects of the disorder are also present. For example—as detailed below—the chronic mild stress (CMS) model of depression was developed around a specific endpoint, a decreased intake of sweet fluids, reflecting an impairment of rewarded behaviour, but was subsequently shown to include a wide range of additional depression-relevant behavioural and physiological abnormalities.
Behavioural models are used in psychopharmacology for two distinct purposes: as simulations within which to study aspects of psychiatric states and as screening tests for the development of new treatments. Screening tests are subject to logistical considerations: for example, the test should be completed in the shortest possible time and ideally will respond to acute drug treatment. However, in a model of a psychiatric condition, these same features may be counter-indicated. Antidepressant drugs are clinically ineffective if administered acutely and are largely inert if administered to non-depressed people: therefore, a model of clinical antidepressant action should involve chronic drug treatment, administered within a context of abnormal behaviour rather than to ‘normal’ animals. Thus, a particular time course of antidepressant action and a particular level of behavioural sophistication may be desirable or undesirable features, depending upon the purpose for which a procedure is being used. Some of the procedures that are most frequently used in antidepressant research, such as the forced swim test (FST: Porsolt et al. 1977) and the tail suspension test (TST: Steru et al. 1985), involve acute drug treatment to ‘normal’ animals and should be thought of as screening tests for antidepressant-like activity rather than animal models of depression. They may, however, be employed as behavioural endpoints within animal models of depression, to measure the effect of environmental or physiological manipulations: the FST in particularly is frequently used in this manner.
The above definition of animal models of psychopathology emphasises that they aim to be homologous, rather than analogous, to aspects of psychiatric disorders: that is, to simulate essentially the same process across species rather than to implement a process that simply looks the same. (For example, a bird’s wings are homologous to a mammal’s limbs, but only analogous to a fly’s wings.) It is this feature that provides their translational value. But to be useful for translational purposes, a model must be sufficiently valid, and an assessment of the validity of a model provides an indication of the degree of confidence that we can place in the hypotheses arising from its use. This involves an evaluation of strengths and weaknesses and areas of uncertainty, rather than a yes/no judgement. Several systems of evaluation have been proposed, which have the common feature that models are assessed on two or more independent dimensions. The most widely used method employs the three dimensions of predictive, face and construct validity: predictive validity means that performance in the test predicts performance in the condition being modelled (and vice versa); face validity means that there are phenomenological similarities between the two; and construct validity means that the model has a sound theoretical rationale (Willner 1984). Some reviewers have advocated the primacy of one or other of these three dimensions (Geyer and Markou 2002; Weiss and Kilts 1998; Sarter and Bruno 2002); more complex frameworks have also been proposed (Belzung and Lemoine 2011). In relation to animal models of depression, predictive validity refers primarily to specific and selective responsiveness to (drug and non-drug) antidepressants; face validity is assessed by comparison to DSM (now DSM-V) symptom checklists, with particular reference to core symptoms of depression; and construct validity is based on an argument for similarity of psychological constructs, such as responsiveness to rewarding events, or if they are known, the underlying neurobiological mechanisms (Willner 1984).
Most animal models of depression are based on the induction of a depressive-like phenotype by stress, which, of course, plays a major clinical role in the onset of depression. Among these, the CMS model is the most extensively validated. Despite early concerns about the reliability of the CMS model, it is now very widely used: the initial report on this model (Willner et al. 1987) and a review of the first 10 years of CMS research (Willner 1997) have each been cited in excess of a thousand times, and the model has been a major player in the development of the current understanding of antidepressant drug action (Willner et al. 2013). In the CMS model, rats or mice are exposed chronically to a constant bombardment of unpredictable micro-stressors, resulting in the development of a plethora of behavioural changes, including decreased response to rewards, a behavioural correlate of the clinical core symptom of depression, anhedonia. Reward sensitivity is usually tracked by periodic (typically weekly) tests in which the animal is given access to a highly preferred sweet solution, or to a choice between a sweet solution and plain water. Consumption of or preference for the sweet reward decreases over weeks of exposure but can be restored to normal levels by chronic treatment with antidepressant drugs. This effect typically takes several weeks, paralleling the clinical situation. In addition to a decreased response to sweet rewards, animals subjected to CMS are generally anhedonic in other tests of rewarded behaviour, such as place preference conditioning or intracranial self-stimulation, and also show all of the other symptoms of depression that it is possible to model in animals, such as decreases in sexual, investigative and other motivated behaviours, decreased self-care, weight loss, disrupted sleep patterns and phase advance of the diurnal rhythm. Some studies have used decreased self-care (Surget et al. 2009, 2011) or increased immobility in the FST as alternative, non-hedonic, behavioural endpoints (Willner 2005). CMS also has extensive physiological and neurochemical parallels with depression (Hill et al. 2012). Reversal of CMS effects has been seen with representatives of all of the clinically used chemical families of antidepressant drug, but not with non-antidepressants of various kinds. Overall, therefore, the model has a high degree of construct, face and predictive validity (Willner et al. 1987; Willner 1997, 2005). Occasionally, a pattern of behavioural and neurochemical changes has been reported that is opposite to what is usually observed. The basis for these anomalous effects has not been established, but they lead to a recommendation that behavioural validation of the model should always precede or accompany physiological investigations (Willner 2005).
In another frequently used procedure, the learned helplessness (LH) model, animals (originally, dogs; more typically rats or mice) are subjected to inescapable footshock and subsequently display an impairment in learning to escape when given the opportunity to do so (Maier and Seligman 1976). The learning impairment following inescapable shock, which is more evident the more difficult the learning task (for example, a chain of two responses rather than a single response), is interpreted as ‘helplessness’: the perception that escape is not possible (albeit that this interpretation has been questioned: Willner 1986). The procedure properly involves the use of a yoked control design, in which inescapably shocked animals receive the same shock regime as paired animals that are able to escape; the latter group shows no impairment relative to non-shocked animals. Many studies use a simpler (and less interpretable) procedure based on administration of inescapable shock and comparison of the performance of shocked and non-shocked animals. Animals subject to the learned helplessness procedure show many symptomatic parallels to major depression—so much so that it has been suggested that rodents subjected to uncontrollable shock could meet DSM diagnostic criteria (Weiss et al. 1982)! However, the learned helplessness paradigm is implemented in a variety of different ways in different laboratories, and the version of the paradigm giving rise to the broadest range of symptoms (Weiss et al. 1982) uses extremely high shock levels (4–6 ma) which are of doubtful relevance to depression. Furthermore, the effects of this regime largely dissipate within 2–3 days, and the effects of antidepressant treatment have not been studied using this procedure. Antidepressant effects have typically been studied using shocks of a considerably lower intensity (1.0–1.5 ma) which cause a far less pervasive pattern of behavioural impairment. For example, this procedure has not been reported to engender anhedonia; it does, however, cause some long-lasting physiological changes (e.g. Philbert et al. 2011). As with the CMS model, LH is reversed by a wide range of antidepressant drugs, with relatively few false positives or false negatives. There is some question as to whether LH is better considered as a model of depression or of post-traumatic stress disorder, which also responds to some degree to antidepressant treatment (Foa et al. 1992). Nevertheless, as with CMS, work using the LH model has made major contributions to the understanding of the neural systems underpinning antidepressant action (e.g. Maier and Watkins 2010).
An interesting hybrid model uses acute severe stress (shock) to elicit behavioural deficits then switches to chronic mild stress to maintain them (Gambarana et al. 2001). This model, however, has been little used. Various other precipitants have been employed to elicit depression-relevant and antidepressant-reversible behavioural endpoints, including repeated social defeat (Chaouloff 2013), withdrawal of rewards (Huston et al. 2013) and withdrawal from chronic drug treatment (D’Souza and Markou 2010). Again, these procedures, while interesting and providing some neurobiological insights, have not been extensively validated or utilised to study mechanisms of antidepressant action.
Why animal models of depression may be of limited value for the development of treatments to overcome antidepressant resistance
Over the past two decades, research using the CMS and LH models (and others), and parallel clinical research, has established that stress precipitates depression primarily by damaging the hippocampus, leading to changes in the activity of a distributed neural system involving various midbrain and forebrain structures, with a particular focus in the ventromedial prefrontal cortex (vm-PFC), and that antidepressants work by repairing the damaged hippocampus, thus restoring the normal balance of activity within that circuitry (Willner et al. 2013). This mechanism—reversal of the neurotoxic effects of stress—represents a significant limitation to the scope of antidepressant action, because it assumes that stress-induced neurotoxicity is the problem that antidepressants need to overcome. However, there are many factors that are known to increase vulnerability to depression, meaning that the role of stress as a precipitant is correspondingly diminished: these include a clinical history of depression and a variety of genetic, personality or developmental risk factors. Significantly, heightened vulnerability to depression is associated with resistance to antidepressant drug treatment (Willne et al. 2014). Thus, although antidepressants provide an efficient means of reversing the neurotoxic effects of stress, they are much less effective in conditions where vulnerability to depression is elevated, the role of stress in precipitating depression is correspondingly lower, and as a result, the major substrate for antidepressant action (stress-induced neurotoxicity) is absent or minor.
In light of these findings, we have argued elsewhere that progress towards drug therapies for treatment-resistant depression may require a paradigm shift away from stress-based models of depression and towards models of vulnerability to depression (Willner et al. 2013, 2014). Indeed, the ideal models to investigate the potential reversal of risk factors may be models in which conventional antidepressants are ineffective.
Animal models of predisposition to depression
Risk factors (diatheses) for depression may present as ‘silent’ until activated by stress (e.g. a genetic risk factor that does not directly elicit depressive symptoms, or a tendency towards depressive thinking that is well controlled), as a sub-syndromal depressive condition (recognised as depressive personality disorder in DSM-III, which was retained for research purposes in DSM-IV, but has now been dropped from DSM-V), or as dysthymia (pervasive depressive disorder in DSM-V), a low-grade chronic condition that is difficult to distinguish symptomatically from a major depressive episode. Consequently, animal models of a depressive diathesis could appear either as essentially ‘normal’ animals that are more sensitive to a precipitant used to induce ‘depressive’ behaviour, or could present ‘depressive’ features in the absence of any specific experimental manipulation. In the latter case, from a modelling perspective, there is little to distinguish chronic low-grade depression from a major depressive episode other than severity and chronicity. In relation to predictive validity, chronic low-grade depressions are less responsive to drug treatment, but to the extent that they are treatable, they respond to the same range of antidepressant drugs as major depression. There is greater clinical use of dopaminergic antidepressants such as amisulpride in dysthymia, and a recent meta-analysis found that amisulpride was more effective than the SSRI fluoxetine (Kriston et al. 2014), but dopaminergic antidepressants are also effective in major depression, so this does not differentiate the two syndromes. In relation to face validity, some features, including anhedonia and vegetative symptoms, are perhaps less prominent in pervasive depressive disorder than in major depression, but the differential diagnosis is made entirely on the basis of duration of illness. There are also no significant differences in the theoretical understanding of chronic low-grade depression and major depression (construct validity). In a nutshell, there are no distinctive validity criteria for animal models of chronic low-grade depression as distinct from major depression (Willner and Mitchell 2002).
A diathesis-stress perspective
The situation is different, however, when we consider the problem of drug-resistant depression within a diathesis-stress perspective. As outlined above, antidepressant resistance arises, at least in part, from the occurrence of depression in high-risk individuals (Willne et al. 2014). Therefore, an appropriate model within which to investigate antidepressant-resistant depression is one in which a valid model of depression is implemented in the context of a valid model of a risk factor for depression. In this situation, two clear criteria should be satisfied. First, depression-like behaviour should be elicited more readily in high-risk groups. As discussed above, this criterion may to some extent be automatically satisfied in relation to risk factors that by themselves elicit depressive-like features, but the features in question should be valid endpoints, such as hedonic measures. Second, and critically, the effectiveness of conventional antidepressants should be lower in high-risk than in low-risk groups. This is actually a less straightforward issue to investigate than might at first appear, because it requires a comparable pre-treatment behavioural baseline, which may be difficult to achieve if the high-risk group are more stress sensitive than the low-risk group.
We might tentatively propose a third criterion for models of antidepressant-resistant depression, that high-risk and low-risk groups should respond equally well to unconventional antidepressant treatments that act outside the hippocampus. The rationale for this proposal is that it is the action of antidepressants within the hippocampus that is responsible for the greater effectiveness of antidepressants in low-risk groups, where the effects of stress-induced neurotoxicity are more prominent. Thus treatments that bypass the hippocampus and act directly within other parts of the depression circuitry—in particular, the prefrontal cortex (PFC)—may not be limited in their action by a lesser involvement of stress in the precipitation of a depressive episode. For example, deep brain stimulation (DBS) of the vm-PFC has been reported to produce long-lasting antidepressant effects in treatment-resistant depressed patients (Mayberg 2009; Hamani et al. 2011; McGrath et al. 2014). A rapid reversal of CMS-induced anhedonia and other depression-related behaviours has also been demonstrated in rats following DBS of the vm-PFC (Hamani et al. 2012; Dournes et al. 2013; Veerakumar et al. 2014). For obvious reasons, DBS has not been used in antidepressant-responsive patients, but there is a reasonable expectation that it would be effective if implemented. Rapid improvements in antidepressant-refractory patients are also reported following single intravenous infusions of the NMDA receptor antagonist ketamine (Berman et al. 2000; Zarate et al. 2006; Diazgranados et al. 2010). These effects appear to be mediated by direct actions within the PFC, as ketamine has been shown to suppress activity in the rostral anterior cingulate cortex (Salvadore et al. 2009), a strong predictor of successful antidepressant treatment (Pizzagalli 2011), and this effect occurs too rapidly to be mediated through structural changes in the hippocampus. In the CMS model, a single injection of ketamine reversed not only the anhedonic and other behavioural deficits, but also the atrophy of dendritic spines in the PFC and the associated electrophysiological deficits (Li et al. 2010, 2011b; Duman et al. 2012). Ketamine has psychotomimetic effects, so again, for obvious reasons, it has not been tested in antidepressant-responsive patients.
Animal models of heightened vulnerability and antidepressant resistance
We will now consider some animal models of predisposition to depression in relation to specific risk factors that are known to be associated with an increased proclivity to depression and resistance to antidepressant treatment (Willne et al. 2014). In each case, we consider the extent to which the model can be said to meet the first two of the criteria we have outlined: increased sensitivity to stress in a valid animal model of depression and insensitivity of those effects to conventional antidepressant treatment. The third criterion, a good response to unconventional antidepressants that appear effective in treatment-resistant depression, is barely discussed for the simple reason that with three exceptions (the Wistar-Kyoto (WKY) and congenital learned helplessness (cLH) rat and high anxiety behaviour (HAB) mouse strains), the effectiveness of unconventional treatments for resistant depression has not been examined in any of the other models under consideration.
The models that we discuss all involve the application of stress to animals with a biological background that can be considered depression-related (Harro 2012); that is, they include both a putative risk factor and a proximal stressor. Not reviewed here in detail are procedures advanced as models of predisposition to depression—many of which, as discussed above, display a depressive-like phenotype—for which tests have not been conducted to confirm that they do actually involve heightened vulnerability. (This exclusion would apply, for example, to a genetically manipulated mouse for which the FST represents the extent of its behavioural evaluation.) We also do not discuss procedures that result in an antidepressant-like phenotype or that confer resilience to stress, because these models do not provide a test-bed for research on treatment-resistant depression.
History of depression
One of the most powerful risk factors for depression is a previous history of depressive episodes. Each episode of depression increases the probability of a further episode (American Psychiatric Association 2000; Solomon et al. 2000), and with each successive episode, the severity of stress needed to precipitate the episode decreases (Kendler et al. 2000; Dienes et al. 2006; Stroud et al. 2008; Morris et al. 2010; Slavich et al. 2011). Recurrent depressions are also more resistant to pharmacotherapy than first-episode depressions (O’Reardon et al. 2007; Souery et al. 2007; Kaymaz et al. 2008; Rush et al. 2011). However, this reflects a specific failure of antidepressant drug treatment: the efficacy of cognitive therapy for depression is maintained across repeated episodes (Leykin et al. 2007), which presumably reflects the fact that psychotherapy engages the PFC directly and differently from antidepressant drugs (Kennedy et al. 2007; Mayberg 2009; Clark and Beck 2010; Hamani et al. 2011).
We are aware of only a single study that has modelled a history of depression by repeated stress induction. Isingrini et al. (2010) subjected BALB/c mice to two 7-week periods of CMS separated by a 6-week interval. Using a relatively mild CMS procedure, a wider range of behavioural impairments was seen after the second, relative to the first, period of CMS exposure, indicating an increase in stress sensitivity. In animals maintained on a normal diet, chronic treatment with fluoxetine decreased all of the behavioural impairments. However, in mice fed a high-fat diet (modelling the vascular risk for depression: Camus et al. 2004), mice treated with fluoxetine showed no behavioural impairment after the first CMS period, but fluoxetine was without effect following the second CMS exposure. Thus, the study demonstrated increased stress sensitivity in previously stressed animals, and antidepressant resistance was induced by an interaction between a high-fat diet and a history of repeated stress exposure.
Early life stress
Developmental factors, such as multiple loss events or childhood adversity (Souery et al. 1999), are also associated with both vulnerability to depression and antidepressant treatment resistance. The developmental factor that has been most studied is childhood maltreatment. A recent meta-analysis reported that adults who had been abused as children had a greatly elevated risk of developing recurrent or persistent depression, as well as a substantial increase in rates of failure to respond to pharmacotherapy (Nanni et al. 2012). As with a history of depression, the elevated level of risk involves an increased sensitivity to stress rather than an increased exposure to stressors (Kendler et al. 2004; Harkness et al. 2006; Shapero et al. 2014), and adults who were abused as children were normally responsive to psychotherapeutic interventions, again indicating a specific resistance to antidepressant drug treatment (Nanni et al. 2012).
There are many and diverse animal models of early stress, including several paradigms involving interference with mother-pup interactions by periods of separation and variations in the quality of maternal care or the postnatal environment; there is also considerable variation in the comparison group used (Pryce et al. 2005). None of these manipulations in themselves produces a reliable depression-like phenotype in mice or rats (Millstein and Holmes 2007; Schmidt et al. 2011); in particular, there is little if any evidence that rats subjected to these early manipulations are anhedonic (Pryce et al. 2005). However, as discussed above, for present purposes, the major issue is whether any of these procedures produce an increase in stress precipitation of depression-relevant behaviours in later life. Again, there is little evidence that early life stress increases responsiveness to stress in adulthood; indeed, resilience to adult stress is often reported (Schmidt et al. 2011). In one study, separation of Sprague-Dawley rat pups from their mothers, for 15 min daily between postnatal days 2 and 14, led to an increase in anhedonia and other depression-relevant behaviours, hypothalamic-pituitary-adrenal (HPA) activity and gene expression in vm-PFC, following repeated restraint stress, but the response to antidepressant treatment was not studied (Uchida et al. 2010). However, in another study, early deprivation was reported to increase the acquisition of LH by adult rats of the Fischer strain (but not by Wistar rats), but the effect was reversed by chronic fluoxetine treatment, suggesting that this will not lead to a model for antidepressant resistance (Rüedi-Bettschen et al. 2004). A third study reported that naturalistically occurring poor maternal care led to an increased anhedonic response to CMS in outbred Wistar rats; the response to antidepressant treatment was not examined (Henningsen et al. 2012). However, there is evidence that greater adult emotionality between mouse strains may to some extent reflect differences in early maternal care (Calatayud and Belzung 2001), and this is not associated with resistance to antidepressant treatments (Ibarguen-Vargas et al. 2009). Overall, these data do not give confidence that work with combined early-life and late stress models will significantly improve the research environment for the development of treatments for antidepressant-resistant depression.
An important limitation of rodent studies of early-life stress is that the early post-natal period in rodents corresponds to the pre-natal period of brain development in humans, which casts doubt on the validity of early manipulations as models of childhood adversity. A closer parallel is provided by a model in which stress is applied to ‘juvenile’ rats in the post-weaning to pre-pubertal stage. Juvenile exposure to stressors, such as predator scent or a 3-day varied stress regime (forced swim, elevated platform and restraint), leads to increased emotional reactivity in adulthood, with around a third of subjects showing LH and other depression-related abnormalities, while the other two thirds exhibited anxiety-related behaviour (Tsoory and Richter-Levin 2006; Tsoory et al. 2007; Horovitz et al. 2012). Antidepressants have not been tested in this model.
Genetic factors
Depression has a strong familial component. For example, whereas women with a low genetic risk for depression showed the typical pattern of high stress exposure before a first episode of depression and a gradual decrease in the extent of stress exposure before subsequent episodes, in women with a family history of depression and a depressed co-twin, the first episode of depression was precipitated by very low levels of stress, and this did not change across episodes (Kendler et al. 2001a). These familial effects could reflect a shared environment, but are typically assumed to reflect genetic influences, and as discussed below, several genes have been identified that are associated with both predisposition to depression and resistance to antidepressant treatment.
Many transgenic mice have been designed to assess the effects of antidepressant drugs. Some of them are completely unrelated to depression. For example, the P-gp knockout mouse (abcb1a mouse, Uhr et al. 2000, 2003; Uhr and Grauer 2003; Karlsson et al. 2013) is a model targeting drug penetration across the blood-brain barrier, such that in the knockout mice, effects of drugs were prevented if they were Pg-p substrates, but not otherwise—so unlike other SSRIs, the effects of fluoxetine were unaffected. Due to the fact that Pg-P is a multidrug resistance protein completely unspecific to depression, no data have been published regarding the stress sensitivity of this model, so it is not possible to assess its validity in relation to our first criterion. However, this does parallel clinical data showing an association between a polymorphism of the ABCB1 gene and antidepressant response (Uhr et al. 2008).
As monoaminergic drugs are classically used in the treatment of depression, the contribution of the monoaminergic system to their effects has been extensively investigated. For example, PCPA, which blocks serotonin synthesis, suppressed the effects of subchronic treatment with fluoxetine and imipramine, but not those of noradrenergic compounds such as reboxetine or desipramine (O’Leary et al. 2007). In TPH2 (−/−) mice, the enzyme that enables serotonin synthesis in the brain is absent. While the knockout mice did not respond to SSRIs, their sensitivity to stress in the CMS and LH models was unchanged (Angoa-Pérez et al. 2014), so this model does not meet our first criterion.
In humans, the most studied of the monoaminergic genes is a functional polymorphism in the promoter region of the serotonin transporter gene, 5-HTTLPR, which has been reported to moderate the effects of stressful life events on depression. In the absence of stress, all genetic subtypes have the same low risk of depression, but as the frequency of stressful events increases, the risk of depression is greatly elevated in individuals homozygous for the short allele of the 5-HTTLPR gene relative to individuals homozygous for the long allele, with heterozygotes showing an intermediate level of risk (Caspi et al. 2003, 2010; Uher and McGuffin 2008; Karg et al. 2011). The parallel finding is that individuals homozygous for the short allele of the 5-HTTLPR gene are less responsive to antidepressant treatment than individuals homozygous for the long allele, with heterozygotes showing an intermediate response (Serretti et al. 2007; Zobel and Maier 2010; Licinio and Wong 2011).
Similar results have been found in primates, as the short allele of the 5-HTTLPR gene increased the neuroendocrine response to separation stress in infant macaques (Barr et al. 2004), increased sensitivity to social stress in adult rhesus monkeys (Jarrell et al. 2008), and was also associated with a decreased hormonal response to acute administration of the SSRI citalopram (Michopoulos et al. 2011). These results suggest that polymorphisms of the 5-HTTLPR gene may have similar effects on stress sensitivity and antidepressant responsiveness in humans and non-human primates. Similarly, in mice, the serotonin transporter knockout mouse may fulfil at least the two first validity criteria as a model of antidepressant resistance. These mutant mice display both heightened vulnerability to stress (Hariri and Holmes 2006; Muller et al. 2011) and an absence of effects of acute SSRIs (Holmes, et al. 2002). To our knowledge, the behavioural effects of chronic SSRIs have not been assessed after genetic deletion of the serotonin transporter. However, the effects of chronic duloxetine, a mixed 5-HT-NA uptake inhibitor, on brain-derived neurotrophic factor (BDNF) levels in the hippocampus and the frontal cortex were maintained in this model (Calabrese et al. 2010), suggesting that antidepressant resistance may be specific to SSRIs.
Others studies have investigated the effects of ablation of different 5-HT receptors. Mice bearing mutations of both 5-HT1A and 5-HT1B receptors show increased emotionality, but they still respond to chronic SSRIs (Guilloux et al. 2011). However, the effects of SSRIs but not of imipramine were abolished in 5-HT1A knockout mice (Santarelli et al. 2003). Interestingly, the mutants displayed increased anxiety (Ramboz et al. 1998; Heisler et al. 1998; Parks et al. 1998; Zhuang et al. 1999) and decreased depressive-like behaviour (Ramboz et al. 1998; Heisler et al. 1998; Parks et al. 1998), alongside increased physiological responses to acute and chronic stress (Patti et al. 2002; Carnevali et al. 2014). If we consider that the critical factor is stress sensitivity, rather than behaviour in depressive behaviour bioassays, this mutant fulfils the first two criteria as a model of antidepressant resistance, albeit that resistance would be restricted to SSRIs. This parallels clinical findings showing an association of a polymorphism of the 5-HT1A receptor with antidepressant resistance (Kato and Serretti 2010). In 5-HT1B knockout mice, the effects of acute but not of chronic SSRIs were prevented (Trillat et al. 1998; Mayorga et al. 2001) so this would not be considered a model of antidepressant resistance. However, a recent study reported that these mice displayed increased stress-induced autonomic and locomotor responses and no response to chronic fluvoxamine, suggesting that this model may merit further study (Vinkers et al. 2011). Genetic mutants studied in relation to other serotoninergic-receptor genes include mice with a deletion of the 5-HT2B receptor, which showed resistance to chronic fluoxetine and paroxetine (Diaz et al. 2012) but were not tested for stress sensitivity, and mice with a deletion of the 5-HT2C gene, which showed potentiation of the effects of acute fluoxetine in a bioassay (Cremers et al. 2004) but were not studied further to our knowledge. Studies on the 5-HT4 receptor null mutant showed that ablation of this receptor attenuated the response to stress-induced hypophagia (Compan et al. 2004), while repeated administration of citalopram produced a total inhibition of 5-HT firing in the knockouts, and only a partial inhibition in wild-type mice (Conductier et al. 2006): both results suggest that this might rather be a model of decreased antidepressant resistance. A final target related to serotoninergic neurotransmission is p11 (which recruits 5-HT1B receptors to the cell membrane) and its target SMARCA3. Ablation of p11 abolished the effects of chronic imipramine in the open field and induced increased thigmotaxis (suggesting heightened anxiety behaviour) (Svenningsson et al. 2006), while ablation of SMARCA3 suppressed the effect of chronic escitalopram on stress-induced anhedonia (Oh et al. 2013). However, ablation of SMARCA3 did not modify sucrose consumption after chronic stress (or the effects of acute escitalopram in the tail suspension test) (Oh et al. 2013). Overall, while there may be some interesting leads, none of the 5-HT receptor mutant mouse models stand out as clearly relevant to treatment-resistant depression.
The effects of targeted modifications of the noradrenergic system have also been investigated. For example, ablation of the gene encoding dopamine beta-hydroxylase (DBH), which converts dopamine into noradrenaline and adrenaline, prevented the antidepressant-like effects of noradrenergic drugs, such as desipramine or reboxetine, but it also abolished the action of drugs acting on other monoaminergic targets such as pargyline, bupropion and the SSRIs fluoxetine, sertraline and paroxetine, though strangely the effects of citalopram remained unchanged (Cryan et al. 2001, 2004). Further, the ablation of DBH increases sensitivity to restraint stress (Kvetnanský et al. 2008), albeit that depression-relevant behaviours have not been tested. Therefore, this mutant may satisfy two criteria as a model of antidepressant drug resistance. However, the antidepressant studies involved acute drug treatment in the FST: further studies using chronic drug treatment and a more valid behavioural model are needed.
Another interesting monoamine-related genetic model is the OCT2 (Organic Cation Transporter 2) null mutant mouse. OCT2 is involved in the clearance of noradrenaline and serotonin so the mutant mice display decreased levels of serotonin and noradrenaline, associated with increased anxiety and immobility in the FST (Bacq et al. 2012). Interestingly, the effects of acute selective noradrenaline or serotonin transporter blockers were increased in bioassays, but the effects of chronic venlafaxine in the chronic corticosterone model were decreased (Bacq et al. 2012). Subsequently, these mice were shown to exhibit an increased sensitivity to behavioural effects of CMS (Couroussé et al. 2014). Therefore, this model does appear to fulfil two criteria as a genetic model of antidepressant resistance (increased stress sensitivity and no response to chronic antidepressant treatment).
Other neurotransmitter-related mutants that have been investigated in relation to stress include mutants of the glutamatergic system. Effects reported include increased sensitivity to chronic stress or defeat stress for vGLUT1+/− mice (Garcia-Garcia et al. 2009; Venzala et al. 2012) and greater LH for mice with a GSK3 mutation inhibiting GSK3 phosphorylation (Polter et al. 2010). However, the effects of chronic antidepressants have not been assessed in these models. The endocannabinoid (eCB) system is a neuromodulatory system in which post-synaptic cannabinoids suppress presynaptic transmitter release from GABAergic and glutamatergic axon terminals via CB1 receptors. Clinical data have shown that both predisposition to depression and resistance to antidepressant treatment are linked to polymorphisms of genes coding for the CB1 receptor (Domschke et al. 2008; Juhasz et al. 2009). Endocannabinoids are metabolised by fatty acid amide hydroxylase (FAAH), and mice with deletion of the FAAH gene show resistance to chronic stress (Hill et al. 2013). Conversely, increased CMS-induced anhedonia has been observed in CB1 receptor knockout mice (Martin et al. 2002; Valverde and Torrens 2012). Further, sensitivity to subchronic (three injections) administration of desipramine or paroxetine was slightly altered in these mice (Steiner et al. 2008), suggesting the possibility of antidepressant resistance.
As antidepressant resistance in humans is associated with dysregulation of the HPA axis, (Belzung and Billette De Villemeur 2010), other studies have investigated modifications of genes encoding components of the stress axis. Various mutants of glucocorticoid receptors (GR) have been described, including models of loss of GR and models of increased GR. The models of loss include GR+/− mice, which exhibit a partial loss of GR in the whole body; GRNesCre mice, which have GR loss restricted to the entire brain, neurons and glial cells during adulthood; FBGRKO mice which display GR loss in forebrain neurons during adulthood; GRCaMKCre mice, which exhibit GR loss in neurons in brain and cells in the pituitary during development (at P6); Sim1Cre-GRe3D mice, which exhibit GR loss primarily in PVN neurons during adulthood; and GRPOMCCre mice, which show GR loss in the anterior pituitary cells throughout life. GR+/− mice display increased stress responsivity in the LH model (Ridder et al. 2005). Stress coping behaviour is increased in GRNesCre and GRPOMCCre mice while the opposite is found in FBGRKO mice (depending upon the genetic background), while no effect is detected in GRCaMKCre and Sim1Cre-GRe3D mice. Further, the GRNesCre and Sim1Cre-GRe3D mice show increased corticosterone levels after stress (Laryea et al. 2015). Additional models include loss of GR in dorsal raphe neurons (DRNGRKO), associated with increased stress coping behaviour (Vincent and Jacobson 2014), or loss of GR in DA neurons, which induces some resilience when GR have been inactivated in DA-innervated postsynaptic neurons, but not when they have been inactivated on presynaptic DA neurons (Barik et al. 2013). To our knowledge, out of all of the mutants so far mentioned, the effects of antidepressant treatments have only been investigated in the FBGRKO mice, revealing normal responses to acute or chronic antidepressants (Boyle et al. 2005; Vincent et al. 2013). Additionally, viral-induced knockdown of GR in the prefrontal cortex had no effect on corticosterone or behaviour in the FST but increased sensitivity to chronic imipramine (Hussain and Jacobson 2015). Mutants with increased GR function include mice overexpressing GR throughout the brain (so-called YGR mice because overexpression is achieved by a yeast artificial chromosome). Interestingly, they exhibit a hormonal and the behavioural resistance to immobilisation stress and are also more resistant to the development of LH (Ridder et al. 2005). To our knowledge, antidepressant sensitivity has not been tested in these mice.
The opposite profile was found in transgenic mice with GR overexpression in forebrain (GRov), which showed increased environmental reactivity and vulnerability to stress-induced cognitive deficits (Hebda-Bauer et al. 2010). GRov mice also showed evidence of impaired negative feedback inhibition of the HPA axis (Wei et al. 2007). However, as these mice are supersensitive to antidepressants (Wei et al. 2004), they cannot be considered a model of antidepressant resistance. Finally, mice overexpressing mineralocorticoid receptors (MR) in the forebrain exhibited decreased anxiety behaviour and corticosterone release in response to restraint stress (Rozeboom et al. 2007). So far, therefore, there is no evidence that direct manipulations of GR or MR produces a model of antidepressant resistance, though for most models the relevant experiments have not yet been conducted. A related target is the FK506 binding protein 51 (FKBP51), which is a regulator of the GR via its action on the chaperone Hsp90. Knockouts for FKBP51 have been generated that do display resistance both to the behavioural and physiological effects of chronic paroxetine while if anything being less sensitive to stress (Gassen et al. 2014).
In people, several studies have shown that genetic polymorphisms in the CRFR1 gene modulate the influence of exposure to childhood abuse on adult depression (Bradley et al. 2008; Ressler et al. 2010; Polanczyk et al. 2009; Kranzler et al. 2011; Grabe et al. 2010). In mice, two haplotypes of the CRFR1 gene have been described that are associated with single nucleotide polymorphisms on regulatory regions of the gene identical to the ones found in humans (Labermaier et al. 2014). The risk haplotype (TT homozygotes) is associated with higher sensitivity to chronic stress in adolescence, when compared to mice from the CC genotype (Labermaier et al. 2014), and this pattern is reversed by CRFR1 antagonists. However, the effects of more classical antidepressants have not yet been assessed in this mutant. Other CRH-related mutants include conventional CRF-overexpressing mice (Stenzel-Poore et al. 1994; van Gaalen et al. 2002), mice with CRH overexpression in neurons (Dirks et al. 2001; Groenink et al. 2002), CRFR1 knockout mice (Smith et al. 1998; Timpl et al. 1998), mice with transient perinatal forebrain CRF overexpression (Kolber et al. 2010), mice with conditional forebrain-restricted inactivation of CRFR1 (Muller et al. 2003), mice with CRH overexpression in the pituitary and mice with deficient CRF2 receptors (Bale et al. 2000, 2002). With the exception of the mice overexpressing CRF in the pituitary (Dedic et al. 2012), all other mutants exhibit increased anxiety like-behaviour but were not assessed for stress vulnerability. Interestingly, mice deficient in CRFR2 receptors are hypersensitive to stress exposure and display increased stress-induced corticosterone levels and increased anxiety-like behaviour (Bale et al. 2000, 2002). Unfortunately, to our knowledge, none of the CRF mutants has been tested in relation to antidepressant resistance. Finally, due to the synergistic effects of vasopressin with CRF in the control of the HPA axis, the phenotype of the V1b knockout has also been investigated. In these mice, release of ACTH and corticosterone following acute stress was attenuated (see Koshimizu et al. 2012), as were corticosterone levels after acute fluoxetine or desipramine (Stewart et al. 2008). Further, V1b knockout mice show decreased ACTH after chronic restraint (Lolait et al. 2007), which suggests increased stress sensitivity. However, to our knowledge, the effects of chronic antidepressants have not been assessed in this model. In conclusion, none of the HPA-related mutants (GR/MR/CRH/vasopressin) fulfils both the criteria of increased stress sensitivity and that of resistance to chronic antidepressants.
Other players in antidepressant resistance are transcription factors and their targets, for example, the transcription factor deltafosB and its targets GluA2 (an AMPA receptor subunit) and CaMKII. Overexpression of DeltaFos within the nucleus accumbens (achieved either using bitransgenic mice or by viral injection) promotes resilience to chronic social defeat, whereas increased expression of deltaJun in the same area has the opposite effects (Nestler 2015). Viral-mediated overexpression of GluA2 in the same structure also induced resilience to social defeat (Nestler 2015). The effects of chronic fluoxetine were abolished in mice with a viral-induced overexpression of deltafosB or CaMKII within the accumbens (Nestler 2015). However, in this model, antidepressant resistance is not associated with increased stress sensitivity.
Considering that BDNF mediates the chronic effects of monoaminergic antidepressants (D’Sa and Duman 2002), polymorphisms modifying the expression of BDNF could alter the therapeutic action of antidepressants. In human studies, two meta-analyses (Kato and Serretti 2010; Zou et al. 2010) reported a better response to antidepressants in Met allele carriers, while conversely, the val/val genotype was linked to resistance to chronic treatment with escitalopram (El-Hage et al. 2015). These findings have been translated to rodents, but with findings opposite to those predicted: BDNF (met/met) mice exhibit increased anxiety behaviour and a decreased response to long-term fluoxetine (3 weeks) (Chen et al. 2006). However, sensitivity to chronic stress has not been assessed in these mice. Interestingly, BDNF+/− mice exhibited normal effects of acute antidepressants (Saarelainen et al. 2003) and a normal response to CMS, but the effects of chronic imipramine in CMS mice were dampened (Ibarguen-Vargas et al. 2009), suggesting antidepressant resistance. These mice performed normally in various depression-related tests, other than an increase in LH that was attributable to a decrease in pain sensitivity (MacQueen et al. 2001). BDNF is known to function differently in different brain areas, and deletion of BDNF restricted to the dentate gyrus was found to attenuate the effects of subchronic injections of desipramine or citalopram in the FST (Adachi et al. 2008), but again, the effects of chronic stress were not assessed. Finally, some studies have explored the involvement of the target of BDNF, the TrkB receptor. First it was shown that TrkB ablation suppressed the effects of acute imipramine and fluoxetine in the FST (Saarelainen et al. 2003), and ablation of TrkB in hippocampal neural stem cells (but not in mature neurons of the dentate gyrus) suppressed the antidepressant-like effects of chronic (21 days) fluoxetine or imipramine. Unfortunately, the effects of chronic stress were again not assessed. Overall, these data suggest that there might be some potential for region-specific BDNF-related mutants, but research is at a very early stage.
Two final genetic models are not directly related to synaptic transmission or transduction. Aquaporins (AQPs) are water channel proteins involved in regulating water homeostasis, AQP4b being the predominant form in the brain where it is expressed in adult neural stem cells as well as in astrocytes. In the AQP4 knockout mouse, the antidepressant and anxiolytic effects of chronic fluoxetine were prevented, as were the fluoxetine-induced enhancement of adult hippocampal neurogenesis and the hippocampal CREB phosphorylation. However, mutants and wild-type mice were similar in their behavioural responses to CMS (Kong et al. 2009). Finally, mice with a genetic deletion of macrophage migration inhibitory factor (MIF), a pro-inflammatory cytokine expressed in the brain, particularly in hippocampal stem cells and proliferating cells, show increased immobility in the FST and decreased adult hippocampal neurogenesis, as well as resistance to the ability of chronic (14 days) fluoxetine to increase hippocampal neurogenesis (Conboy et al. 2011). Although the sensitivity of these mice to chronic stress has not been assessed and resistance to the behavioural effects of chronic antidepressants have not been tested, the observed phenotype suggests that this model could potentially fulfil our criteria for antidepressant resistance.
Personality factors
Much of the influence of both genetics and early traumatic events on depressive symptomatology is mediated through the personality factor of neuroticism (Kendler and Gardner 2011), which is one of the strongest risk factors for depression (Enns and Cox 1997; Christensen and Kessing 2006; Kendler and Myers 2010). Early-onset depression, in particular (first episode before the age of 30), is characterised by a higher level of neuroticism and a higher prevalence of comorbid personality disorders (Bukh et al. 2011). Neuroticism is also well established as a factor associated with resistance to antidepressant treatment (Souery et al. 1999; Bock et al. 2010).
There have been numerous attempts to model the personality risk for depression by selective breeding of animals with depressive characteristics, high levels of emotionality or dysfunctions of the stress axis. Roman low avoidance (RLA) and fawn hooded (FH) are two ‘classic’ high-emotionality rat strains. The RLA rat strain was selectively bred for poor avoidance in the shuttle box paradigm, while their high-avoidance (RHA) counterparts were selectively bred for their good performance in that task. RLA rats show behaviour characteristic of heightened emotionality in several tests, including increased immobility in the FST (Steimer and Driscoll 2003). However, RLA and RHA rats react similarly to social defeat (Meerlo et al. 1997), and in the FST RLA rats show a greater response to acute or chronic antidepressant treatment (Piras et al. 2014). FH rats exhibit hyperactivity of the HPA axis, a characteristic of depressive illness, increased ethanol intake and preference and increased immobility in the FST (Rezvani et al. 2002), though this has not always been observed (e.g. Lahmame et al. 1996). Again, these abnormalities are corrected by antidepressant treatment (Rezvani et al. 2002). These findings suggest that the RLA and FH strains are likely to prove of limited relevance to treatment-resistant depression.
One of the most studied ‘depressive’ rat strains is the Flinders sensitive line (FSL), which was originally bred for cholinergic supersensitivity, and subsequently shown to display a range of physiological and behavioural features characteristic of depression, including dysregulation of serotonergic neurotransmission, increased rapid eye movement (REM) sleep and elevated immobility in the FST (Overstreet and Wegener 2013). Significantly, the FSL rat does not show abnormal responses to rewards under baseline conditions (Pucilowski et al. 1993; Matthews et al. 1996) but does show increased anhedonia when subjected to CMS (Pucilowski et al. 1993). However, in comparison to the Flinders resistant line (FRL) control strain, the FSL rat is much more responsive to antidepressant reduction of immobility in the FST (Overstreet and Wegener 2013). While antidepressant studies have not been conducted in FSL rats subjected to CMS, these results suggest that the FSL rat also does not show promise in relation to treatment-resistant depression.
More promising are Wistar-Kyoto rats, which were originally bred as a normotensive control strain for the spontaneously hypertensive (SHR) rat strain, but were later found to display physiological and behavioural features suggestive of heightened emotionality, including increased immobility in the FST (Nam et al. 2014) and, of greater relevance, enhanced physiological responses to repeated stress (Morilak et al. 2005) and an increased propensity to develop LH (Belujon and Grace 2014). Strain differences in antidepressant responses have not been studied in relation to LH, but WKY rats have been shown repeatedly to be less responsive to antidepressants in the FST, with some studies reporting a specific sub-sensitivity to serotonergic antidepressants (López-Rubalcava and Lucki 2000) and others reporting a more general effect (Lahmame et al. 1997). WKY rats are also sub-sensitive to suppression of REM sleep by both noradrenergic and serotonergic antidepressants, despite showing a higher baseline of REM sleep (Ivarsson et al. 2005). Interestingly, LH was reversed by ketamine in WKY rats (Belujon and Grace 2014). There was no comparison with the control strains in this study; however, WKY rats were more responsive than outbred Wistar rats to ketamine reversal of immobility in the FST (Tizabi et al. 2012). These findings suggest that WKY rats go some way to satisfying all three of our criteria for a model of antidepressant treatment resistance.
Another interesting procedure is the congenital learned helplessness (cLH) strain. cLH rats, and their counterpart congenital non-LH controls, were bred by selecting for individuals that developed the most and least severe LH when tested with mild levels of shock that induce LH in only some of the subjects. After many generations, cLH animals were produced that fail to escape even without prior stress exposure (Vollmayr and Henn 2001). They are also anhedonic in several different behavioural tests (Vollmayr et al. 2004; Sanchis-Segura et al. 2005; Shumake et al. 2005; Shabel et al. 2014). Importantly, unlike LH, which is readily reversed by antidepressant treatment, cLH animals are said to be resistant to antidepressant reversal of their helpless behaviour (Sartorius et al. 2007; F. Henn, personal communication; B. Vollmayr, personal communication). However, an antidepressant effect in cLH rats was found with a high dose of the MAO-B inhibitor deprenyl, which preferentially protects DA rather than NA or 5-HT. Deprenyl has also been reported to be effective in treatment-resistant depression (Sunderland et al. 1994); uniquely, the effect in cLH rats required experience of repeated test trials, suggesting some form of learning process that has not been described for any other antidepressant (Schulz et al. 2010). Neuroimaging studies of cLH rats have shown metabolic and functional connectivity changes very similar to those observed in major depression (Shumake et al. 2000; Shumake and Gonzalez-Lima 2003; Gass et al. 2014). In particular, cLH rats show increased metabolism in the subgenual region of the cingulate cortex and in the lateral habenula, which are regions in which antidepressant effects of DBS have been reported in depressed patients (Sartorius et al. 2010; Hamani et al. 2011). Correspondingly, DBS or pharmacological inhibition of the lateral habenula has been found to restore normal escape behaviour in cLH rats (Li et al. 2011a; Winter et al. 2011). Thus, the cLH rat may also meet all three criteria for a model of antidepressant treatment resistance. Phenomenologically, the cLH rat could be considered as a model of the depressive personality, which is associated with both vulnerability to depression (Kwon et al. 2000; Ono et al. 2002) and resistance to antidepressant treatment (Hirschfeld et al. 1998; Souery et al. 2007; Takahashi et al. 2013).
Mice selectively bred for high anxiety behaviour (HAB mice) display reduced hippocampal neurogenesis and increased immobility in the FST. They are usually compared to mice displaying normal anxiety behaviour (NAB mice). A first study reported that chronic fluoxetine was able to alleviate the depressive-like features in HAB mice but had no effects on the anxiety behaviours and on hippocampal neurogenesis (Sah et al. 2012), while a second study from the same group reported that HAB mice responded normally to chronic noradrenergic drugs such as reboxetine or desipramine but were resistant to the effects of chronic SSRIs including fluoxetine, paroxetine and citalopram (Schmuckermair et al. 2013). However, HAB mice did respond to repeated DBS of the nucleus accumbens (Schmuckermair et al. 2013). In these selected lines, the effects of environmental enrichment have been assessed in HAB and the effects of CMS in NAB, with the objective of rescuing the differences, but CMS has not been assessed in HAB mice; also the main depression-relevant behavioural measures were the FST and TST. Nevertheless, there is a hint that HAB mice might also be able to meet all three criteria for a model of treatment-resistant depression. A HAB rat has also been described, which, compared with its low anxiety behaviour (LAB) counterpart, and like the HAB mouse, also shows increased immobility in the FST. However, unlike the HAB mouse, this effect in rats, along with associated neurochemical changes, was reversed by chronic paroxetine treatment (Keck et al. 2003, 2005).
Another set of mouse models is based on HPA reactivity. A bidirectional breeding strategy selecting mice according to differences in corticosterone secretion after stress produced the high (HR), intermediate (IR) and low (LR) reactivity mouse lines (Touma et al. 2008). HR mice display a hyperactive coping style (decreased floating in the FST), while LR mice show the opposite pattern (Touma et al. 2008, 2009; Knapman et al. 2010; Mattos et al. 2013). These opposite patterns are sometimes presented as models of the melancholic subtype of depression (HR mice) and of atypical depression (LR mice). Interestingly, chronic fluoxetine was able to reverse the phenotype of HR mice, which is consistent with the efficacy of antidepressants in melancholic depression, but it aggravated the depressive-like phenotype of the LR mice, which is consistent with the observation that atypical depression responds poorly to antidepressants (Surget et al. 2012). However, the LR mouse, while showing enhanced immobility in the FST and being resistant to fluoxetine, is sub-sensitive to stress (as its name indicates). This inconsistency merits further investigation.
A different strategy is to select sub-groups from a general population. When using chronic social defeat to differentiate stress-susceptible and stress-resistant rats, a greater anhedonic response (stress-induced reward threshold elevation) is associated with poor antidepressant-like effects of fluoxetine or desipramine (Der-Avakian et al. 2014), which suggests that the susceptible population can be considered as a model in which increased stress sensitivity is associated with antidepressant resistance. But applying the same strategy to mice, those selected for higher social avoidance after chronic social defeat showed good behavioural and neurochemical responses to chronic fluoxetine (Cao et al. 2010): so this strategy cannot be used to model antidepressant resistance in mice. However, in another mouse model, mice were selected on the basis of dexamethasone suppression after 2 weeks of CMS (low suppression (LS) indicating a higher stress response). These two sub-populations did not differ behaviourally after 9 weeks of stress but did exhibit differences in the response to chronic fluoxetine, the LS mice displaying partial antidepressant resistance (Khemissi et al. 2014).
Female sex
Depression is 1.5–3 times more common among women compared with men. However, although men and women tend to experience, and be affected by, different types of stressful life events, there is no overall difference in either frequency of exposure to stressful life events or sensitivity to their pathogenic effect (Kendler et al. 2001b). Moreover, the increased vulnerability among women is not accompanied by resistance to antidepressant treatment. Indeed, women have been reported to respond significantly better than men to SSRIs, though not to tricyclic antidepressants, possibly as a result of interactions between gonadal hormones and the 5-HT system (Khan et al. 2005). Furthermore, non-depressed women do not express a variety of physiological changes that are typically associated with other risk factors for depression (Willne et al. 2014).
Attention is frequently drawn to the anomaly of depression being more prevalent in women, whereas females are rarely tested in animal models of depression. However, in the learned helplessness and CMS models, female rats are actually less likely than males to develop depressive behaviours (Dalla et al. 2010; Franceschelli et al. 2014). Therefore, female sex is not associated with increased stress responsiveness in either people or rodents. So while it remains a matter of some importance to understand the basis for the sex difference in the incidence of depression (cf. Hyde et al. 2008; Siddaway et al. 2015), an increase in the use of females in animal models would be unlikely to lead to marked progress towards a solution to the problem of treatment-resistant depression.
Evaluation of the models
Table 1 summarises the models that, from the literature reviewed, may be of value for the study of treatment-resistant depression. For each model listed, the table summarises the position in relation to the three criteria discussed (increased stress responsiveness; decreased response to chronically administered conventional antidepressants; good response to novel antidepressant modalities) and the fourth, implicit, criterion of whether the model corresponds to a known clinical risk factor. To maintain readability, the table does not include references to support the statements made: all of the information in the table is taken from the earlier text. We have included in Table 1 studies for which there is partial information about how they meet the criteria we have considered, including some models for which this is as yet no information about antidepressant responsiveness. (Empty cells in the table indicate that those questions have not yet been asked.) We have not included many models discussed in the text that failed to display antidepressant resistance when tested.
The three models that stand out as most likely to prove informative are the WKY and cLH rat strains and the HAB mouse, which relate to neurotic (WKY, HAB) or depressive (cLH) personality features. In addition to increased stress responsivity and resistance to classic antidepressants, these three models have also been shown to respond to the novel antidepressant modalities that are claimed to be effective in treatment-resistant depression, ketamine (WKY) and DBS (cLH and HAB). Nevertheless, in all three cases, the evidence is patchy. For WKY, we currently lack evidence of resistance to chronic antidepressant treatment, and the evidence of antidepressant resistance in cLH is unpublished. HAB data are based on behaviour in the FST, which is also the case for the ketamine response in WKY. And DBS was applied to lateral habenula (cLH) or nucleus accumbens (HAB), but while clinical antidepressant effects have been reported for DBS of both of these structures, DBS of the anterior cingulate cortex, the major focus of clinical interest, has not yet been reported in these animal models.
The second section of the table includes four models related to specific human risk factors that show some evidence of heightened stress sensitivity and antidepressant resistance, but again, with significant limitations. Mice were more sensitive to a second bout of CMS and were antidepressant resistant, but this was only seen in animals fed a high-fat diet, which suggests that the relevance of this model may be limited to vascular depression. 5-HT transporter and 5-HT1A knockout mice are resistant to SSRIs (perhaps unsurprisingly) but appear to respond normally to non-serotonergic antidepressants; additionally, the 5-HT1A knockout does not display a depressive-like behavioural phenotype. Perhaps the most promising of this group is the CB1 knockout mouse, but currently, the evidence of antidepressant resistance only extends as far as 3 days of treatment.
The third section of the table lists three mutant mouse strains where the weight of behavioural evidence is comparable to those listed above, but there is no evidence from human studies for a role of the genes targeted, and again, the evidence is limited. 5-HT1B and DBH knockout mice show increased stress responsiveness, but in both cases, depression-relevant behavioural endpoints have not been tested. For DBH knockout mice, antidepressant resistance has been demonstrated for many antidepressants, including some (but not all) SSRIs, but only for acute administration; chronic drug administration has been used with 5-HT1A knockouts, but the results are inconsistent across studies. The most promising model in this group is the OCT2 null mutant mouse, which shows a range of heightened stress responses, including responses to CMS, and despite showing increased responses to acute antidepressant treatment, was found to be insensitive to chronic administration of the 5-HT/NA uptake inhibitor venlafaxine. Further evidence is needed of the effects of chronic treatment with a wider range of antidepressants to validate this model.
The final group of models listed in the table can be said to merit further study, insofar as there is in each case some intriguing evidence that falls well short of a convincing picture. Juvenile (unlike neonatal) stress causes heightened emotional responsiveness in adult rats, which in around a third of subjects is expressed as a depression-like phenotype. Similar depression-relevant responses to stress are seen in vGlut+/− and GSK3 mutant mice. However, in none of these models has the response to antidepressants been examined. Outbred mice carrying the TT haplotype of the CRHR1 gene also showed an increased neuroendocrine response to chronic stress, which was normalised by treatment with a CRF1 antagonist. There is also a paucity of behavioural data for 5-HT2B and p11 knockout mice. For these two strains, neither their stress sensitivity nor their drug responsiveness in depression-related tests has been assessed, but they are both reported to be sub-sensitive to anxiolytic effects of chronic antidepressant treatment: further work in more directly depression-related behavioural models is needed. The MIF knockout mouse has been reported to show both an increased stress response—but only in the FST—and antidepressant sub-sensitivity—but only for a neurochemical effect. Finally, rats selected as low dexamethasone suppressors showed some evidence of decreased sensitivity to fluoxetine, but their greater HPA activity was not accompanied by heightened sensitivity to the behavioural effects of CMS. The one model in this group for which drug resistance in a depression-related test has been reported is the FKBP1 knockout mouse, which was less resistant to acute amitriptyline and to acute or chronic paroxetine in the FST and on various neurochemical measures, but does not show an increased response to stress.
Evaluation of the criteria
Resistance to antidepressant treatment
It goes without saying that resistance to antidepressant treatment is an essential criterion for a model of treatment-resistant depression. However, some aspects of this criterion should be mentioned. First, it is also essential that resistance is demonstrated for chronic, not only acute, antidepressant treatment. This is not yet the case for several of the models listed in Table 1, including the Wistar-Kyoto rat which heads the list. Second, it may be possible to predict treatment resistance on the basis of the other criteria that we have considered, as indicated by the presence towards the bottom of Table 1 of several models in which antidepressants have not yet been tested. Third, because antidepressants are effective in both depression and anxiety, if the focus of interest is on treatment-resistant depression, then the model should involve depression-relevant rather than anxiety-relevant behavioural endpoints. As shown towards the foot of Table 1, this is not universally the case. Fourth, we note that for some of the models listed (e.g. the HAB mouse and some of the knockout mouse strains), treatment resistance extends only to serotonergic antidepressants. This highlights the importance of testing a wide range of antidepressants before concluding that treatment resistance has been demonstrated: for some of the models listed in Table 1, the range is narrow and further evidence is needed.
Fifth, and perhaps most important, the demonstration that a model is insensitive to chronic antidepressant treatment, while necessary, may not be sufficient to infer with confidence that the model will be a useful experimental tool. The working assumption behind efforts to develop novel treatments is that antidepressant effects are achieved at a site downstream from the site of action of conventional treatments. Specifically, there is extensive evidence that while many antidepressants act primarily within the hippocampus, their antidepressant effects result from consequent actions in the prefrontal cortex (Willner et al. 2013, 2014). The general proposition, that the brain contains alternative sites of antidepressant action distinct from those at which conventional antidepressants act, is supported by the efficacy of novel treatment modalities such as DBS. At the present stage of scientific development, a model that proved resistant to both conventional and novel antidepressants would not be helpful. For most of the models listed in Table 1, the extent of treatment resistance is unknown.
Finally, we should also mention that different clinical criteria have been proposed to define antidepressant treatment resistance (Table 2). These definitions have the common feature that patients are not considered treatment resistant until they have failed to respond to adequate therapy with at least two or more sequential treatments. According to these definitions, no animal model can be considered as an animal model of antidepressant treatment resistance because sequential application of different treatments has never been used as a strategy to counteract depression-related behaviours in animals.
Response to novel antidepressants
The recent clinical and preclinical studies of antidepressant and antidepressant-like responses to ketamine and DBS provide proof of principle that antidepressant resistance can be overcome. However, as shown in Table 1, the preclinical evidence is limited to only three models (the WKY and cLH rat) and the HAB mouse. And in two of these models (WKY and HAB), the FST was used as the behavioural endpoint, which is problematic because the FST has limitations, not least, a limited pharmacological specificity. Furthermore, as far as we are aware, DBS has not yet been applied in these particular models to the anterior cingulate cortex, the area most frequently targeted in clinical and preclinical studies. (DBS of the cingulate cortex did, however, reverse a behavioural effect of CMS in a sub-group of mice identified empirically as resistant to chronic fluoxetine (Dournes et al. 2013)). Clearly, more work is needed to establish the effectiveness of DBS of the anterior cingulate cortex in models of treatment resistance, to extend studies with ketamine and DBS to more relevant behavioural endpoints, and to examine the effects of these novel treatment modalities in a wider range of models, particularly those listed in the second section of Table 1. We note also that the optogenetic method can be used to generate depressive-like behaviours and to investigate the mechanisms underlying remission. Repeated stimulation of glutamatergic neurons from the anterior cingulate cortex is sufficient to elicit depressive-like behaviours (Barthas et al. 2015), while photoactivation of the vmPFC (Covington et al. 2010), of the projections from vmPFC to the DRN (Challis et al. 2014) or of the projections from VTA to mPFC (Friedman et al. 2014) all restore depressive behaviours elicited by social defeat. This procedure may be helpful in refining the targets for DBS.
In addition to ketamine and DBS, transcranial magnetic stimulation (TMS) applied to the left dl-PFC is another treatment that is known to be effective in treatment-resistant depression, either as monotherapy or as an add-on to ineffective antidepressant treatment (Solvason et al. 2014; Liu et al. 2014). However, while TMS is also effective in reversing behavioural and neurochemical abnormalities in animal models of depression (e.g. Keck et al. 2001; Feng et al. 2012; Kim et al. 2014; Wang et al. 2014), to our knowledge, TMS has not yet been tested in any of the models listed in Table 1 that are of interest in relation to treatment-resistant depression.
Increased stress responsivity
Our proposal to include increased stress responsivity as a useful criterion for models of antidepressant resistance is perhaps the most controversial of the four criteria we have proposed. This proposal derives from the evidence that conventional antidepressants act primarily by reversing stress-induced neurotoxicity and are less effective in remediating components of depression that reflect long-standing predispositions that are present before the onset of current or recent stress (Willner et al. 2013, 2014). We have summarised here the evidence that such predispositions, associated with resistance to antidepressant treatment, can be identified clinically in relation to history of depression, early life stress, genetic factors and personality factors, and that in relation to each of these diatheses, animal models can also be identified in which increased stress sensitivity is associated with a decreased response to antidepressant treatment.
Obviously, increased responsiveness to stress could have many meanings. For some of the models listed in Table 1 as meeting this criterion (e.g. the WKY or cLH rat and the CB1 KO and OCT2 null mutant mouse), the procedure within which animals display hypersensitive to stress is one that is considered, on conventional criteria, to have good validity as a model of depression (CMS or LH). Other models have used a weaker behavioural endpoint, the FST (e.g. HAB mouse), or physiological endpoints (e.g. CRH1 TT haplotype mouse), and in one model (the 5-HT1 KO mouse), physiological and behavioural responses to stress are discrepant. Clearly, the more valid the depression model, the greater the confidence that an exaggerated response in the model will provide a useful model for studying antidepressant resistance. The use of CMS, LH or other models with some validity for depression (e.g. repeated defeat) is therefore to be encouraged.
While the clinical relationship between a predisposition to depression and antidepressant resistance provides a productive basis for finding a similar relationship between stress hypersensitivity and antidepressant resistance in animal models, it is apparent that there are also models of antidepressant resistance that do not involve hypersensitivity to stress (e.g. the FKBP1 KO mouse and the low dexamethasone suppression rat). The utility of these models remains to be determined (as, indeed, is the case for the majority of the models reviewed). There are also some known causes of antidepressant resistance that we have described as ‘theoretically trivial’ (Willner et al. 2013), including, for example, pharmacokinetic factors such as polymorphisms of liver cytochrome 450 enzymes or failure to penetrate the blood-brain barrier (El-Hage et al. 2013), which, if modelled in animals, would likely not be associated with increased stress sensitivity. And as we have pointed out, the greater propensity to depression in women relative to men is not associated with antidepressant resistance. This means that there are exceptions to the relationship between hypersensitivity to stress and antidepressant resistance in both directions. Therefore, increased stress sensitivity should be considered a potentially useful criterion when assessing animal models of drug resistance, but one that is far from absolute.
Human counterpart
There is substantial variability in the extent to which the predisposing factors known to be associated with antidepressant resistance have been modelled. Only a single study (Isingrini et al. 2010), with limited results, has attempted to model the effect of a history of depression. Perhaps more surprisingly, studies of early stress have generally failed to observe either hypersensitivity to adult stress or antidepressant resistance. This may reflect the different course of development of rodents and humans, since juvenile stress does produce a depressive-like phenotype in a proportion of adult rats, though antidepressants have not yet been tested in this model. By contrast, several of the genetic factors found to be associated with an increased risk of depression and antidepressant resistance are paralleled by similar effects in genetically modified mice (Table 1). There are also many genomic models listed in Table 1 for which there is no known human counterpart, and their relevance remains to be established. However, we are not aware of the converse situation, of genetic factors associated with increased clinical risk for depression and antidepressant resistance for which the corresponding genomic manipulation fails to model the risks. This is not the case for genetic models: we have discussed a number of ‘emotional’ or ‘depressive’ strains that fail to show reliable evidence of antidepressant resistance (e.g. the RLA, FH or FSL rat strains). However, three strains, the WKY and cLH rats and the HAB mouse, do show some evidence of heightened responses to stress associated with antidepressant resistance but a good response to ketamine and/or DBS. These are the front-runners in the present analysis. However, it will be apparent that the parallels between the behaviour of these strains and ‘neurotic’ or ‘depressive’ personality traits are very imprecise.
Conclusions
In conclusion, we have identified 18 models that may have some potential in relation to antidepressant resistance. All require further validation, and in most cases, this need is extensive. Currently, the most promising models are the CMS or LH procedures applied to the WKY and cLH rat strains, the HAB mouse strain and the CB1 knockout and OCT2 null mutant genetically modified mouse strains. Further development is needed to validate models of antidepressant resistance that are fit for purpose. The criteria used in this review may provide a helpful framework to guide research in this area.
References
Adachi M, Barrot M, Autry AE, Theobald D, Monteggia LM (2008) Selective loss of brain-derived neurotrophic factor in the dentate gyrus attenuates antidepressant efficacy. Biol Psychiatry 63:642–649
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Washington
Angoa-Pérez M, Kane MJ, Briggs DI, Herrera-Mundo N, Sykes CE, Francescutti DM, Kuhn DM (2014) Mice genetically depleted of brain serotonin do not display a depression-like behavioral phenotype. ACS Chem Neurosci 5:908–919
Bacq A, Balasse L, Biala G, Guiard B, Gardier AM, Schinkel A, Louis F, Vialou V, Martres MP, Chevarin C, Hamon M, Giros B, Gautron S (2012) Organic cation transporter 2 controls brain norepinephrine and serotonin clearance and antidepressant response. Mol Psychiatry 17:926–939
Bale TL, Contarino A, Smith GW, Chan R, Gold LH, Sawchenko PE, Koob GF, Vale WW, Lee KF (2000) Mice deficient for corticotropin-releasing hormone receptor-2 display anxiety-like behaviour and are hypersensitive to stress. Nat Genet 24:410–414
Bale TL, Picetti R, Contarino A, Koob GF, Vale WW, Lee KF (2002) Mice deficient for both corticotropin-releasing factor receptor 1 (CRFR1) and CRFR2 have an impaired stress response and display sexually dichotomous anxiety-like behavior. J Neurosci 22:193–199
Barik J, Marti F, Morel C, Fernandez SP, Lanteri C, Godeheu G, Tassin JP, Mombereau C, Faure P, Tronche F (2013) Chronic stress triggers social aversion via glucocorticoid receptor in dopaminoceptive neurons. Science 339:332–335
Barr CS, Newman TK, Shannon C, Parker C, Dvoskin RL, Becker ML, Schwandt M, Champoux M, Lesch KP, Goldman D, Suomi SJ, Higley JD (2004) Rearing condition and rh5-HTTLPR interact to influence limbic-hypothalamic-pituitary-adrenal axis response to stress in infant macaques. Biol Psychiatry 55:733–738
Barthas F, Sellmeijer J, Hugel S, Waltisperger E, Barrot M, Yalcin I (2015) The anterior cingulate cortex is a critical hub for pain-induced depression. Biol Psychiatry 77:236–245
Belujon P, Grace AA (2014) Restoring mood balance in depression: ketamine reverses deficit in dopamine-dependent synaptic plasticity. Biol Psychiatry 76(12):927–936. doi:10.1016/j.biopsych.2014.04.014
Belzung C (2014) Innovative drugs to treat depression: did animal models fail to be predictive or did clinical trials fail to detect effects? Neuropsychopharmacology 39(5):1041–1051. doi:10.1038/npp.2013.342
Belzung C, Billette De Villemeur E (2010) The design of new antidepressants: can formal models help? A first attempt using a model of the hippocampal control over the HPA axis based on a review from the literature. Behav Pharmacol 21:677–689
Belzung C, Lemoine M (2011) Criteria of validity for animal models of psychiatric disorders: focus on anxiety disorders and depression. Biol Mood Anxiety Disord 1(1):9
Belzung C, Willner P, Phillipot P (2015) Depression: from psychopathology to pathophysiology. Curr Opin Neurol 30C:24–30
Berman RM, Cappiello A, Anand A, Oren DA, Heninger GR, Charney DS, Krystal JH (2000) Antidepressant effects of ketamine in depressed patients. Biol Psychiatry 47:351–354
Bock C, Bukh JD, Vinberg M, Gether U, Kessing LV (2010) The influence of comorbid personality disorder and neuroticism on treatment outcome in first episode depression. Psychopathology 43:197–204
Boyle MP, Brewer JA, Funatsu M, Wozniak DF, Tsien JZ, Izumi Y, Muglia LJ (2005) Acquired deficit of forebrain glucocorticoid receptor produces depression-like changes in adrenal axis regulation and behavior. Proc Natl Acad Sci U S A 102:473–478
Bradley RG, Binder EB, Epstein MP, Tang Y, Nair HP, Liu W, Gillespie CF, Berg T, Evces M, Newport DJ, Stowe ZN, Heim CM, Nemeroff CB, Schwartz A, Cubells JF, Ressler KJ (2008) Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry 65:190–200
Bukh JD, Bock C, Vinberg M, Gether U, Kessing LV (2011) Differences between early and late onset adult depression. Clin Pract Epidemiol Ment Health 7:140–147
Calabrese F, Molteni R, Cattaneo A, Macchi F, Racagni G, Gennarelli M, Ellenbroek BA, Riva MA (2010) Long-term duloxetine treatment normalizes altered brain-derived neurotrophic factor expression in serotonin transporter knockout rats through the modulation of specific neurotrophin isoforms. Mol Pharmacol 77:846–853
Calatayud F, Belzung C (2001) Emotional reactivity in mice, a case of nongenetic heredity? Physiol Behav 74:355–362
Camus V, Kraehenbuhl H, Preisig M, Bula CJ, Waeber G (2004) Geriatric depression and vascular diseases: what are the links? J Affect Disord 81:1–16
Cao JL, Covington HE 3rd, Friedman AK, Wilkinson MB, Walsh JJ, Cooper DC, Nestler EJ, Han MH (2010) Mesolimbic dopamine neurons in the brain reward circuit mediate susceptibility to social defeat and antidepressant action. J Neurosci 30:16453–16458
Carnevali L, Mastorci F, Audero E, Graiani G, Rossi S, Macchi E (2014) Stress-induced susceptibility to sudden cardiac death in mice with altered serotonin homeostasis. PLoS One 7(7):e41184
Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R (2003) Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 301:386–389
Caspi A, Hariri AR, Holmes A, Uher R, Moffitt TE (2010) Genetic sensitivity to the environment: the case of the serotonin transporter gene and its implications for studying complex diseases and traits. Am J Psychiatry 167:509–527
Challis C, Beck SG, Berton O (2014) Optogenetic modulation of descending prefrontocortical inputs to the dorsal raphe bidirectionally bias socioaffective choices after social defeat. Front Behav Neurosci 8:43
Chaouloff F (2013) Social stress models in depression research: what do they tell us? Cell Tissue Res 354:179–190
Chen ZY, Jing D, Bath KG, Ieraci A, Khan T, Siao CJ, Herrera DG, Toth M, Yang C, McEwen BS, Hempstead BL, Lee FS (2006) Genetic variant BDNF (Val66Met) polymorphism alters anxiety-related behavior. Science 314:140–143
Christensen MV, Kessing LV (2006) Do personality traits predict first onset in depressive and bipolar disorder? Nord J Psychiatry 60:79–88
Clark D, Beck AT (2010) Cognitive theory and therapy of anxiety and depression: convergence with neurobiological findings. Trends Cogn Sci 14:418–424
Compan V, Zhou M, Grailhe R, Gazzara RA, Martin R, Gingrich J, Dumuis A, Brunner D, Bockaert J, Hen R (2004) Attenuated response to stress and novelty and hypersensitivity to seizures in 5-HT4 receptor knock-out mice. J Neurosci 24:412–419
Conboy L, Varea E, Castro JE, Sakouhi-Ouertatani H, Calandra T, Lashuel HA, Sandi C (2011) Macrophage migration inhibitory factor is critically involved in basal and fluoxetine-stimulated adult hippocampal cell proliferation and in anxiety, depression, and memory-related behaviors. Mol Psychiatry 16:533–547
Conductier G, Dusticier N, Lucas G, Côté F, Debonnel G, Daszuta A, Dumuis A, Nieoullon A, Hen R, Bockaert J, Compan V (2006) Adaptive changes in serotonin neurons of the raphe nuclei in 5-HT(4) receptor knock-out mouse. Eur J Neurosci 24:1053–1062
Couroussé T, Bacq A, Belzung C, Guiard B, Balasse L, Louis F, Le Guisquet AM, Gardier AM, Schinkel AH, Giros B, Gautron S (2014) Brain organic cation transporter 2 controls response and vulnerability to stress and GSK3β signaling. Mol Psychiatry. doi:10.1038/mp.2014.86
Covington HE 3rd, Lobo MK, Maze I, Vialou V, Hyman JM, Zaman S et al (2010) Antidepressant effect of optogenetic stimulation of the medial prefrontal cortex. J Neurosci 30:16082–16090
Cremers TI, Giorgetti M, Bosker FJ, Hogg S, Arnt J, Mørk A, Honig G, Bøgesø KP, Westerink BH, den Boer H, Wikstrom HV, Tecott LH (2004) Inactivation of 5-HT(2C) receptors potentiates consequences of serotonin reuptake blockade. Neuropsychopharmacology 29:1782–1789
Cryan JF, Dalvi A, Jin SH, Hirsch BR, Lucki I, Thomas SA (2001) Use of dopamine-beta-hydroxylase-deficient mice to determine the role of norepinephrine in the mechanism of action of antidepressant drugs. J Pharmacol Exp Ther 298:651–657
Cryan JF, O’Leary OF, Jin SH, Friedland JC, Ouyang M, Hirsch BR, Page ME, Dalvi A, Thomas SA, Lucki I (2004) Norepinephrine-deficient mice lack responses to antidepressant drugs, including selective serotonin reuptake inhibitors. Proc Natl Acad Sci U S A 101:8186–8191
Dalla C, Pitychoutis PM, Kokras N, Papadopoulou-Daifoti Z (2010) Sex differences in animal models of depression and antidepressant response. Basic Clin Pharmacol Toxicol 106:226–233
Der-Avakian A, Mazei-Robison MS, Kesby JP, Nestler EJ, Markou A (2014) Enduring deficits in brain reward function after chronic social defeat in rats: susceptibility, resilience, and antidepressant response. Biol Psychiatry 76:542–549
Dedic N, Touma C, Romanowski CP, Schieven M, Kühne C, Ableitner M, Lu A, Holsboer F, Wurst W, Kimura M, Deussing JM (2012) Assessing behavioural effects of chronic HPA axis activation using conditional CRH-overexpressing mice. Cell Mol Neurobiol 32:815–828
Diaz SL, Doly S, Narboux-Nême N, Fernández S, Mazot P, Banas SM, Boutourlinsky K, Moutkine I, Belmer A, Roumier A, Maroteaux L (2012) 5-HT(2B) receptors are required for serotonin-selective antidepressant actions. Mol Psychiatry 17:154–163
Diazgranados N, Ibrahim L, Brutsche NE, Newberg A, Kronstein P, Khalife S, Kammerer WA, Quezado Z, Luckenbaugh DA, Salvadore G, Machado-Vieira R, Manji HK, Zarate CA Jr (2010) A randomized add-on trial of an N-methyl-D-aspartate antagonist in treatment-resistant bipolar depression. Arch Gen Psychiatry 67:793–802
Dienes KA, Hammen C, Henry RM, Cohen AN, Daley SE (2006) The stress sensitization hypothesis: understanding the course of bipolar disorder. J Affect Disord 95:43–49
Dirks A, de Jongh R, Groenink L, van der Gugten J, Hijzen TH, Olivier B (2001) Footshock-induced sensitization of the acoustic startle response in two strains of mice. Behav Brain Res 123:17–21
Domschke K, Dannlowski U, Ohrmann P, Lawford B, Bauer J, Kugel H, Heindel W, Young R, Morris P, Arolt V, Deckert J, Suslow T, Baune BT (2008) Cannabinoid receptor 1 (CNR1) gene: impact on antidepressant treatment response and emotion processing in major depression. Eur Neuropsychopharmacol 18:751–759
Dournes C, Beeske S, Belzung C, Griebel G (2013) Deep brain stimulation in treatment-resistant depression in mice: comparison with the CRF1 antagonist, SSR125543. Prog Neuropsychopharmacol Biol Psychiatry 40:213–220
D’Sa C, Duman RS (2002) Antidepressants and neuroplasticity. Bipolar Disord 4:183–194
D’Souza MS, Markou A (2010) Neural substrates of psychostimulant withdrawal-induced anhedonia. Curr Top Behav Neurosci 3:119–178
Duman RS, Li N, Liu RJ, Duric V, Aghajanian G (2012) Signaling pathways underlying the rapid antidepressant actions of ketamine. Neuropharmacology 62:35–41
El-Hage W, Leman S, Camus V, Belzung C (2013) Mechanisms of antidepressant resistance. Front Pharmacol 4:146
El-Hage W, Vourc’h P, Gaillard P, Léger J, Belzung C, Ibarguen-Vargas Y, Andres CR, Camus V (2015) The BDNF Val(66)Met polymorphism is associated with escitalopram response in depressed patients. Psychopharmacology (Berlin) 232:575–581
Enns MW, Cox BJ (1997) Personality dimensions and depression: review and commentary. Can J Psychiatry 42:274–284
Feng SF, Shi TY, Fan-Yang, Wang WN, Chen YC, Tan QR (2012) Long-lasting effects of chronic rTMS to treat chronic rodent model of depression. Behav Brain Res 232:245–251
Foa EB, Zinbarg R, Rothbaum BO (1992) Uncontrollability and unpredictability in post-traumatic stress disorder: an animal model. Psychol Bull 112:218–238
Franceschelli A, Herchick S, Thelen C, Papadopoulou-Daifoti Z, Pitychoutis PM (2014) Sex differences in the chronic mild stress model of depression. Behav Pharmacol 25:372–383
Friedman AK, Walsh JJ, Juarez B, Ku SM, Chaudhury D, Wang J et al (2014) Enhancing depression mechanisms in midbrain dopamine neurons achieves homeostatic resilience. Science 344:313–319
Gambarana C, Scheggi S, Tagliamonte A, Tolu P, De Montis MG (2001) Animal models for the study of antidepressant activity. Brain Res Brain Res Protoc 7:11–20
Garcia-Garcia AL, Elizalde N, Matrov N, Harro J, Wojcik SM, Venzala E, Ramírez MJ, Del Rio J, Tordera RM (2009) Increased vulnerability to depressive-like behavior of mice with decreased expression of VGLUT1. Biol Psychiatry 66:275–282
Gass N, Cleppien D, Zheng L, Schwarz AJ, Meyer-Lindenberg A, Vollmayr B, Weber-Fahr W, Sartorius A (2014) Functionally altered neurocircuits in a rat model of treatment-resistant depression show prominent role of the habenula. Eur Neuropsychopharmacol 24:381–390
Gassen NC, Hartmann J, Zschocke J, Stepan J, Hafner K, Zellner A, Kirmeier T, Kollmannsberger L, Wagner KV, Dedic N, Balsevich G, Deussing JM, Kloiber S, Lucae S, Holsboer F, Eder M, Uhr M, Ising M, Schmidt MV, Rein T (2014) Association of FKBP51 with priming of autophagy pathways and mediation of antidepressant treatment response: evidence in cells, mice, and humans. PLoS Med 11(11):e1001755
Geyer MA, Markou A (2002) The role of preclinical models in the development of psychotropic drugs. In: Bloom F, Davis KL, Charney D, Coyle JT, Nemeroff C (eds) Neuropsychopharmacology: fifth generation of progress. www.acnp.org/asset.axd?id=a81d38da-94d9-4bea-86d3-244e52f15b2d
Grabe HJ, Schwahn C, Appel K, Mahler J, Schulz A, Spitzer C, Fenske K, Barnow S, Lucht M, Freyberger HJ, John U, Teumer A, Wallaschofski H, Nauck M, Völzke H (2010) Childhood maltreatment, the corticotropin-releasing hormone receptor gene and adult depression in the general population. Am J Med Genet B Neuropsychiatr Genet 153B:1483–1493
Groenink L, Dirks A, Verdouw PM, Schipholt M, Veening JG, van der Gugten J, Olivier B (2002) HPA axis dysregulation in mice overexpressing corticotropin releasing hormone Biol. Psychiatry 51:875–881
Guilloux JP, David DJ, Xia L, Nguyen HT, Rainer Q, Guiard BP, Repérant C, Deltheil T, Toth M, Hen R, Gardier AM (2011) Characterization of 5-HT(1A/1B)−/− mice: an animal model sensitive to anxiolytic treatments. Neuropharmacology 61:478–488
Hamani C, Mayberg H, Stone S, Laxton A, Haber S, Lozano AM (2011) The subcallosal cingulate gyrus in the context of major depression. Biol Psychiatry 69:301–308
Hamani C, Machado DC, Hipólide DC, Dubiela FP, Suchecki D, Macedo CE, Tescarollo F, Martins U, Covolan L, Nobrega JN (2012) Deep brain stimulation reverses anhedonic-like behavior in a chronic model of depression: role of serotonin and brain derived neurotrophic factor. Biol Psychiatry 71:30–35
Hariri AR, Holmes A (2006) Genetics of emotional regulation: the role of the serotonin transporter in neural function. Trends Cogn Sci 10:182–191
Harkness KL, Bruce AE, Lumley MN (2006) The role of childhood abuse and neglect in the sensitization of stressful life events in adolescent depression. J Abnorm Psychol 115:730–741
Harro J (2012) Animal models of depression vulnerability. Curr Topics Behav Neurosci. doi:10.1007/7854_2012_221
Hebda-Bauer EK, Pletsch A, Darwish H, Fentress H, Simmons TA, Wei Q, Watson SJ, Akil H (2010) Forebrain glucocorticoid receptor overexpression increases environmental reactivity and produces a stress-induced spatial discrimination deficit. Neuroscience 169:645–653
Heisler LK, Chu H, Brennan TJ, Danao JA, Bajwa P, Parsons LH et al (1998) Elevated anxiety and antidepressant-like responses in serotonin 5-HT1A receptor mutant mice. Proc Natl Acad Sci U S A 95:15049–15054
Henningsen K, Dyrvig M, Bouzinova EV, Christiansen S, Christensen T, Andreasen JT, Palme R, Lichota J, Wiborg O (2012) Low maternal care exacerbates adult stress susceptibility in the chronic mild stress rat model of depression. Behav Pharmacol 23:735–743
Hill MN, Hellemans KG, Verma P, Gorzalka BB, Weinberg J (2012) Neurobiology of chronic mild stress: parallels to major depression. Neurosci Biobehav Rev 36:2085–2117
Hill MN, Kumar SA, Filipski SB, Iverson M, Stuhr KL, Keith JM, Cravatt BF, Hillard CJ, Chattarji S, McEwen BS (2013) Disruption of fatty acid amide hydrolase activity prevents the effects of chronic stress on anxiety and amygdalar microstructure. Mol Psychiatry 18:1125–1135
Hirschfeld RM, Russell JM, Delgado PL, Fawcett J, Friedman RA, Harrison WM, Koran LM, Miller IW, Thase ME, Howland RH, Connolly MA, Miceli RJ (1998) Predictors of response to acute treatment of chronic and double depression with sertraline or imipramine. J Clin Psychiatry 59:669–675
Holmes A, Yang RJ, Murphy DL, Crawley JN (2002) Evaluation of antidepressant-related behavioral responses in mice lacking the serotonin transporter. Neuropsychopharmacology 27:914–923
Horovitz O, Tsoory MM, Hall J, Jacobson-Pick S, Richter-Levin G (2012) Post-weaning to pre-pubertal (‘juvenile’) stress: a model of induced predisposition to stress-related disorders. Neuroendocrinology 95:56–64
Hussain RJ, Jacobson L (2015) Increased antidepressant sensitivity after prefrontal cortex glucocorticoid receptor gene deletion in mice. Physiol Behav 138:113–117
Huston JP, Silva MA, Komorowski M, Schulz D, Topic B (2013) Animal models of extinction-induced depression: loss of reward and its consequences. Neurosci Biobehav Rev 37:2059–2070
Hyde JS, Mezykus AH, Abramson LY (2008) The ABCs of depression: integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev 115:291–313
Ibarguen-Vargas Y, Surget A, Vourc’h P, Leman S, Andres CR, Gardier AM, Belzung C (2009) Deficit in BDNF does not increase vulnerability to stress but dampens antidepressant-like effects in the unpredictable chronic mild stress. Behav Brain Res 202:245–251
Isingrini E, Camus V, Le Guisquet AM, Pingaud M, Devers S, Belzung C (2010) Association between repeated unpredictable chronic mild stress (UCMS) procedures with a high fat diet: a model of fluoxetine resistance in mice. Plos One 5:e10404
Ivarsson M, Paterson LM, Hutson PH (2005) Antidepressants and REM sleep in Wistar-Kyoto and Sprague-Dawley rats. Eur J Pharmacol 522:63–71
Jarrell H, Hoffman JB, Kaplan JR, Berga S, Kinkead B, Wilson ME (2008) Polymorphisms in the serotonin reuptake transporter gene modify the consequences of social status on metabolic health in female rhesus monkeys. Physiol Behav 93:807–819
Juhasz G, Chase D, Pegg E, Downey D, Toth ZG, Stones K, Platt H, Mekli K, Payton A, Elliott R, Anderson IM, Deakin JF (2009) CNR1 gene is associated with high neuroticism and low agreeableness and interacts with recent negative life events to predict current depressive symptoms. Neuropsychopharmacology 34:2019–2027
Karg K, Burmeiste M, Shedden K, Sen S (2011) The serotonin transporter promoter variant (5-HTTLPR), stress, and depression meta-analysis revisited. Arch Gen Psychiatry 68:444–454
Karlsson L, Carlsson B, Hiemke C, Ahlner J, Bengtsson F, Schmitt U, Kugelberg FC (2013) Altered brain concentrations of citalopram and escitalopram in P-glycoprotein deficient mice after acute and chronic treatment. Eur Neuropsychopharmacol. doi:10.1016/j.euroneuro.2013.01.003
Kato M, Serretti A (2010) Review and meta-analysis of antidepressant pharmacogenetic findings in major depressive disorder. Mol Psychiatry 15:473–500
Kaymaz N, van Os J, Loonen AJ, Nolen WA (2008) Evidence that patients with single versus recurrent depressive episodes are differentially sensitive to treatment discontinuation: a meta-analysis of placebo-controlled randomized trials. J Clin Psychiatry 69:1423–1436
Keck ME, Welt T, Post A, Muller MB, Toschi N, Wigger A, Landgraf R, Holsboer F, Engelmann M (2001) Neuroendocrine and behavioural effects of repetitive transcranial magnetic stimulation in a psychopathological animal model are suggestive of antidepressant-like effects. Neuropsychopharmacology 24:337–349
Keck ME, Welt T, Muller MB, Uhr M, Ohl F, Wigger A, Toschi N, Holsboer F, Landgraf R (2003) Reduction of hypothalamic vasopressinergic hyperdrive contributes to clinically relevant behavioural and neuroendocrine effects of chronic paroxetine treatment in a psychopathological rat model. Neuropsychopharmacology 28:235–243
Keck ME, Sartori SB, Welt T, Muller MB, Ohl F, Holsboer F, Landgraf R, SIngewald N (2005) Differences in serotonergic neurotransmission between rats displaying high or low anxiety/depression-like behaviour: effects of chronic paroxetine treatment. J Neurochem 92:1170–1179
Kendler KS, Gardner CO (2011) A longitudinal etiologic model for symptoms of anxiety and depression in women. Psychol Med 41:2035–2045
Kendler KS, Myers J (2010) The genetic and environmental relationship between major depression and the five-factor model of personality. Psychol Med 40:801–806
Kendler KS, Thornton LM, Gardner CO (2000) Stressful life events and previous episodes in the etiology of major depression in women: an evaluation of the “kindling” hypothesis. Am J Psychiatry 157:1243–1251
Kendler KS, Thornton LM, Gardner CO (2001a) Genetic risk, number of previous depressive episodes, and stressful life events in predicting the onset of major depression. Am J Psychiatry 158:582–586
Kendler KS, Thornton LM, Prescott CA (2001b) Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. Am J Psychiatry 158:587–593
Kendler KS, Kuhn JW, Prescott CA (2004) Childhood sexual abuse, stressful life events and risk for major depression in women. Psychol Med 34:1475–1482
Kennedy SH, Konarski JZ, Segal ZV, Lau MA, Bieling PJ, McIntyre RS, Mayberg HS (2007) Differences in brain glucose metabolism between responders to CBT and venlafaxine in a 16-week randomized controlled trial. Am J Psychiatry 164:778–788
Khan A, Brodhead AE, Schwartz KA, Kolts RL, Brown WA (2005) Sex differences in antidepressant response in recent antidepressant clinical trials. J Clin Psychopharmacol 25:318–324
Khemissi W, Farooq RK, Le Guisquet AM, Sakly M, Belzung C (2014) Dysregulation of the hypothalamus-pituitary-adrenal axis predicts some aspects of the behavioral response to chronic fluoxetine: association with hippocampal cell proliferation. Front Behav Neurosci 8:340
Kim SY, Lee DW, Kim H, Bang E, Chae JH, Choe BY (2014) Chronic repetitive transcranial magnetic stimulation enhances GABAergic and cholinergic metabolism in chronic unpredictable mild stress rat model: 1H-NMR spectroscopy study at 11.7 T. Neurosci Lett 20(572):32–37
Knapman A, Heinzmann JM, Hellweg R, Holsboer F, Landgraf R, Touma C (2010) Increased stress reactivity is associated with cognitive deficits and decreased hippocampal brain-derived neurotrophic factor in a mouse model of affective disorders. J Psychiatr Res 44:566–575
Kolber BJ, Boyle MP, Wieczorek L, Kelley CL, Onwuzurike CC, Nettles SA, Vogt SK, Muglia LJ (2010) Transient early-life forebrain corticotropin-releasing hormone elevation causes long-lasting anxiogenic and despair-like changes in mice. J Neurosci 30:2571–2581
Kong H, Sha LL, Fan Y, Xiao M, Ding JH, Wu J, Hu G (2009) Requirement of AQP4 for antidepressive efficiency of fluoxetine: implication in adult hippocampal neurogenesis. Neuropsychopharmacology 34:1263–1276
Koshimizu TA, Nakamura K, Egashira N, Hiroyama M, Nonoguchi H, Tanoue A (2012) Vasopressin V1a and V1b receptors: from molecules to physiological systems. Physiol Rev 92:1813–1864
Kranzler HR, Feinn R, Nelson EC, Covault J, Anton RF, Farrer L, Gelernter J (2011) A CRHR1 haplotype moderates the effect of adverse childhood experiences on lifetime risk of major depressive episode in African-American women. Am J Med Genet B Neuropsychiatr Genet 156B:960–968
Kriston L, von Wolff A, Westphal A, Hölzel LP, Härter M (2014) Efficacy and acceptability of acute treatments for persistent depressive disorder: a network meta-analysis. Depress Anxiety 31:621–630
Kvetnanský R, Krizanova O, Tillinger A, Sabban EL, Thomas SA, Kubovcakova L (2008) Regulation of gene expression of catecholamine biosynthetic enzymes in dopamine-beta-hydroxylase- and CRH-knockout mice exposed to stress. Ann N Y Acad Sci 1148:257–268
Kwon JS, Kim YM, Chang CG, Park BJ, Kim L, Yoon DJ, Han WS, Lee HJ, Lyoo IK (2000) Three-year follow-up of women with the sole diagnosis of depressive personality disorder: subsequent development of dysthymia and major depression. Am J Psychiatr 157:1966–1972
Labermaier C, Kohl C, Hartmann J, Devigny C, Altmann A, Weber P, Arloth J, Quast C, Wagner KV, Scharf SH, Czibere L, Widner-Andrä R, Brenndörfer J, Landgraf R, Hausch F, Jones KA, Müller MB, Uhr M, Holsboer F, Binder EB, Schmidt MV (2014) A polymorphism in the Crhr1 gene determines stress vulnerability in male mice. Endocrinology 155:2500–2510
Lahmame A, Gomez F, Armario A (1996) Fawn-hooded rats show enhanced active behaviour in the forced swimming test, with no evidence for pituitary-adrenal axis hyperactivity. Psychopharmacology (Berlin) 125:74–78
Lahmame A, del Arco C, Pazos A, Yritia M, Armario A (1997) Are Wistar-Kyoto rats a genetic animal model of depression resistant to antidepressants? Eur J Pharmacol 22:115–123
Laryea G, Muglia L, Arnett M, Muglia LJ (2015) Dissection of glucocorticoid receptor-mediated inhibition of the hypothalamic-pituitary-adrenal axis by gene targeting in mice. Front Neuroendocrinol 36:150–164
Leykin Y, Amsterdam JD, DeRubeis RJ, Gallop R, Shelton RC, Hollon SD (2007) Progressive resistance to SSRI therapy but not to cognitive therapy in the treatment of moderate to severe major depressive episode. J Consult Clin Psychol 75:267–276
Li N, Lee B, Liu RJ, Banasr M, Dwyer JM, Iwata M, Li XY, Aghajanian G, Duman RS (2010) mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. Science 329:959–964
Li B, Piriz J, Mirrione M, Chung C, Proulx CD, Schulz D et al (2011a) Synaptic potentiation onto habenula neurons in the learned helplessness model of depression. Nature 470:535–539
Li N, Liu RJ, Dwyer JM, Banasr M, Lee B, Son H, Li XY, Aghajanian G, Duman RS (2011b) Glutamate N-methyl-D-aspartate receptor antagonists rapidly reverse behavioral and synaptic deficits caused by chronic stress exposure. Biol Psychiatry 69:754–761
Licinio J, Wong ML (2011) Pharmacogenomics of antidepressant treatment effects. Dialogues Clin Neurosci 13:63–71
Liu B, Zhang Y, Li L (2014) Repetitive transcranial magnetic stimulation as an augmentative strategy for treatment-resistant depression, a meta-analysis of randomized, double-blind and sham-controlled study. BMC Psychiatry 14:342
Lolait SJ, Stewart LQ, Jessop DS, Young WS 3rd, O’Carroll AM (2007) The hypothalamic-pituitary-adrenal axis response to stress in mice lacking functional vasopressin V1b receptors. Endocrinology 148:849–856
López-Rubalcava C, Lucki I (2000) Strain differences in the behavioral effects of antidepressant drugs in the rat forced swimming test. Neuropsychopharmacology 22:191–199
MacQueen GM, Ramakrishnan K, Croll SD, Siuciak JA, Yu G, Young LT, Fahnestock M (2001) Performance of heterozygous brain-derived neurotrophic factor knockout mice on behavioral analogues of anxiety, nociception, and depression. Behav Neurosci 115:1145–1153
Maier SF, Seligman MEP (1976) Learned helplessness: theory and evidence. J Exp Psychol Gen 1:3–46
Maier SF, Watkins LR (2010) Role of the medial prefrontal cortex in coping and resilience. Brain Res 1355:52–60
Martin M, Ledent C, Parmentier M, Maldonado R, Valverde O (2002) Involvement of CB1 cannabinoid receptors in emotional behaviour. Psychopharmacology (Berlin) 159:379–387
Matthews K, Baldo BA, Markou A, Lown O, Overstreet DH, Koob GF (1996) Rewarding electrical brain stimulation: similar thresholds for Flinders Sensitive Line Hypercholinergic and Flinders Resistant Line hypocholinergic rats. Physiol Behav 59:1155–1162
Mattos GE, Heinzmann JM, Norkowski S, Helbling JC, Minni AM, Moisan MP, Touma C (2013) Corticosteroid-binding globulin contributes to the neuroendocrine phenotype of mice selected for extremes in stress reactivity. J Endocrinol 219:217–229
Mayberg HS (2009) Targeted electrode-based modulation of neural circuits for depression. J Clin Invest 119:717–725
Mayorga AJ, Dalvi A, Page ME, Zimov-Levinson S, Hen R, Lucki I (2001) Antidepressant-like behavioral effects in 5-hydroxytryptamine(1A) and 5-hydroxytryptamine(1B) receptor mutant mice. J Pharmacol Exp Ther 298:1101–1107
McGrath CL, Kelley ME, Dunlop BW, Holtzheimer PE, Craighead WE, Mayberg HS (2014) Pretreatment brain states identify likely nonresponse to standard treatments for depression. Biol Psychiatry 76(7):527–535. doi:10.1016/j.biopsych.2013.12.005
Meerlo P, Overkamp GJ, Koolhaas JM (1997) Behavioural and physiological consequences of a single social defeat in Roman high- and low-avoidance rats. Psychoneuroendocrinology 22:155–168
Michopoulos V, Berga SL, Wilson ME (2011) Estradiol and progesterone modify the effects of the serotonin reuptake transporter polymorphism on serotonergic responsivity to citalopram. Exp Clin Psychopharmacol 19:401–408
Millstein RA, Holmes A (2007) Effects of repeated maternal separation on anxiety- and depression-related phenotypes in different mouse strains. Neurosci Biobehav Rev 31:3–17
Morilak DA, Barrera G, Echevarria DJ, Garcia AS, Hernandez A, Ma S, Petre CO (2005) Role of brain norepinephrine in the behavioral response to stress. Prog Neuropsychopharmacol Biol Psychiatry 29:1214–1224
Morris MC, Ciesla JA, Garber J (2010) A prospective study of stress autonomy versus stress sensitization in adolescents at varied risk for depression. J Abnorm Psychol 119:341–354
Muller MB, Zimmermann S, Sillaber I, Hagemeyer TP, Deussing JM, Timpl P, Kormann MS, Droste SK, Kuhn R, Reul JM, Holsboer F, Wurst W (2003) Limbic corticotropin-releasing hormone receptor 1 mediates anxiety-related behavior and hormonal adaptation to stress. Nat Neurosci 6:1100–1107
Muller JM, Morelli E, Ansorge M, Gingrich JA (2011) Serotonin transporter deficient mice are vulnerable to escape deficits following inescapable shocks. Genes Brain Behav 10:166–175
Nam H, Clinton SM, Jackson NL, Kerman IA (2014) Learned helplessness and social avoidance in the Wistar-Kyoto rat. Front Behav Neurosci 8:109
Nanni V, Uher R, Danese A (2012) Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am J Psychiatry 169:141–151
Nestler EJ (2015) ∆FosB: a transcriptional regulator of stress and antidepressant responses. Eur J Pharmacol 753:66–72
Nierenberg AA, Amsterdam JD (1990) Treatment-resistant depression: definition and treatment approaches. J Clin Psychiatry 51(Suppl):39–47, discussion 48–50
O’Reardon JP, Solvason HB, Janicak PG, Sampson S, Isenberg KE, Nahas Z, McDonald WM, Avery D, Fitzgerald PB, Loo C, Demitrack MA, George MS, Sackeim HA (2007) Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multisite randomized controlled trial. Biol Psychiatry 62:1208–1216
Oh YS, Gao P, Lee KW, Ceglia I, Seo JS, Zhang X, Ahn JH, Chait BT, Patel DJ, Kim Y, Greengard P (2013) SMARCA3, a chromatin remodeling factor, is required for p11-dependent antidepressant action. Cell 152:831–843
O’Leary OF, Bechtholt AJ, Crowley JJ, Hill TE, Page ME, Lucki I (2007) Depletion of serotonin and catecholamines block the acute behavioral response to different classes of antidepressant drugs in the mouse tail suspension test. Psychopharmacology (Berlin) 192:357–371
Ono Y, Ando J, Onoda N, Yoshimura K, Momose T, Hirano M, Kanba S (2002) Dimensions of temperament as vulnerability factors in depression. Mol Psychiatry 7:948–953
Overstreet DH, Wegener G (2013) The Flinders sensitive line rat model of depression—25 years and still producing. Pharmacol Rev 65:143–155
Parks CL, Robinson PS, Sibille E, Shenk T, Toth M (1998) Increased anxiety of mice lacking the serotonin1A receptor. Proc Natl Acad Sci U S A 95:10734–10739
Patti T, Groenink L, Hijzen TH, Oosting RS, Maes RAA, van der Gugten J, Olivier B (2002) Autonomic changes associated with enhanced anxiety in 5-HT1A receptor knockout mice. Neuropsychopharmacology 27:380–390
Petersen T, Papakostas GI, Posternak M, Kant A, Guyker WM, Iosifescu DV, Yeung AS, Nierenberg AA, Fava M (2005) Empirical testing of two models for staging antidepressant treatment resistance. J Clin Psychopharmacol 25:336–341
Philbert J, Pichat P, Beeské S, Decobert M, Belzung C, Griebel G (2011) Acute inescapable stress exposure induces long-term sleep disturbances and avoidance behavior: a mouse model of post-traumatic stress disorder (PTSD). Behav Brain Res 221:149–154
Piras G, Piludu MA, Giorgi O, Corda MG (2014) Effects of chronic antidepressant treatments in a putative genetic model of vulnerability (Roman low-avoidance rats) and resistance (Roman high-avoidance rats) to stress-induced depression. Psychopharmacology (Berlin) 231:43–53
Pizzagalli DA (2011) Frontocingulate dysfunction in depression: toward biomarkers of treatment response. Neuropsychopharmacol Rev 36:183–206
Polanczyk G, Caspi A, Williams B, Price TS, Danese A, Sugden K, Uher R, Poulton R, Moffitt TE (2009) Protective effect of CRHR1 gene variants on the development of adult depression following childhood maltreatment: replication and extension. Arch Gen Psychiatry 66:978–985
Polter A, Beurel E, Yang S, Garner R, Song L, Miller CA, Sweatt JD, McMahon L, Bartolucci AA, Li X, Jope RS (2010) Deficiency in the inhibitory serine-phosphorylation of glycogen synthase kinase-3 increases sensitivity to mood disturbances. Neuropsychopharmacology 35:1761–1774
Porsolt RD, LePichon M, Jalfre M (1977) Depression: a new animal model sensitive to antidepressant treatment. Nature 266:730–732
Pryce CR, Rüedi-Bettschen D, Dettling AC, Weston A, Russig H, Ferger B, Feldon J (2005) Long-term effects of early-life environmental manipulations in rodents and primates: potential animal models in depression research. Neurosci Biobehav Rev 29:649–674
Pucilowski O, Overstreet DH, Rezvani AH, Janowsky DS (1993) Chronic mild stress-induced anhedonia: greater effect in a genetic rat model of depression. Physiol Behav 54:1215–1220
Ramboz S, Oosting R, Ait Amara A, Kung HF, Blier P, Mendelsohn M et al (1998) Serotonin receptor 1A knockout: an animal model of anxiety related disorder. Proc Natl Acad Sci U S A 95:14476–14481
Ressler KJ, Bradley B, Mercer KB, Deveau TC, Smith AK, Gillespie CF, Nemeroff CB, Cubells JF, Binder EB (2010) Polymorphisms in CRHR1 and the serotonin transporter loci: gene × gene × environment interactions on depressive symptoms. Am J Med Genet B Neuropsychiatr Genet 153B:812–824
Rezvani AH, Parsian A, Overstreet DH (2002) The Fawn-Hooded (FH/Wjd) rat: a genetic animal model of comorbid depression and alcoholism. Psychiatr Genet 12:11–16
Ridder S, Chourbaji S, Hellweg R, Urani A, Zacher C, Schmid W, Zink M, Hörtnagl H, Flor H, Henn FA, Schütz G, Gass P (2005) Mice with genetically altered glucocorticoid receptor expression show altered sensitivity for stress-induced depressive reactions. J Neurosci 29:6243–6250
Rozeboom AM, Akil H, Seasholtz AF (2007) Mineralocorticoid receptor overexpression in forebrain decreases anxiety-like behavior and alters the stress response in mice. Proc Natl Acad Sci U S A 104:4688–4693
Rüedi-Bettschen D, Feldon J, Pryce CR (2004) The impaired coping induced by early deprivation is reversed by chronic fluoxetine treatment in adult Fischer rats. Behav Pharmacol 15:413–421
Rush AJ, Thase ME, Dubé S (2003) Research issues in the study of difficult-to-treat depression. Biol Psychiatry 53:743–753
Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, Niederehe G, Thase ME, Lavori PW, Lebowitz BD, McGrath PJ, Rosenbaum JF, Sackeim HA, Kupfer DJ, Luther J, Fava M (2006) Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry 163(11):1905–1917
Rush AJ, Wisniewski SR, Zisook S, Fava M, Sung SC, Haley CL, Chan HN, Gilmer WS, Warden D, Nierenberg AA, Balasubramani GK, Gaynes BN, Trivedi MH, Hollon SD (2011) Is prior course of illness relevant to acute or longer-term outcomes in depressed out-patients? A STAR*D report. Psychol Med 19:1–19
Saarelainen T, Hendolin P, Lucas G, Koponen E, Sairanen M, MacDonald E, Agerman K, Haapasalo A, Nawa H, Aloyz R, Ernfors P, Castrén E (2003) Activation of the TrkB neurotrophin receptor is induced by antidepressant drugs and is required for antidepressant-induced behavioral effects. J Neurosci 23:349–357
Sah A, Schmuckermair C, Sartori SB, Gaburro S, Kandasamy M, Irschick R, Klimaschewski L, Landgraf R, Aigner L, Singewald N (2012) Anxiety- rather than depression-like behavior is associated with adult neurogenesis in a female mouse model of higher trait anxiety- and comorbid depression-like behavior. Transl Psychiatry 2:e171
Salvadore G, Cornwell BR, Colon-Rosario V, Coppola R, Grillon C, Zarate CA Jr, Manji HK (2009) Increased anterior cingulate cortical activity in response to fearful faces: a neurophysiological biomarker that predicts rapid antidepressant response to ketamine. Biol Psychiatry 65:289–295
Sanchis-Segura C, Spanagel R, Henn FA, Vollmayr B (2005) Reduced sensitivity to sucrose in rats bred for helplessness: a study using the matching law. Behav Pharmacol 16:267–270
Santarelli L, Saxe M, Gross C, Surget A, Battaglia F, Dulawa S, Weisstaub N, Lee J, Duman R, Arancio O, Belzung C, Hen R (2003) Requirement of hippocampal neurogenesis for the behavioral effects of antidepressants. Science 301:805–809
Sarter M, Bruno JP (2002) Animal models in biological psychiatry. In: D’Haenen HA, den Boer JA, Willner P (eds) Biological psychiatry. Wiley, Chichester, pp 37–44
Sartorius A, Mahlstedt MM, Vollmayr B, Henn FA, Ende G (2007) Elevated spectroscopic glutamate/gamma-amino butyric acid in rats bred for learned helplessness. Neuroreport 18:1469–1473
Sartorius A, Kiening KL, Kirsch P, von Gall CC, Haberkorn U, Unterberg AW, Henn FA, Meyer-Lindenberg A (2010) Remission of major depression under deep brain stimulation of the lateral habenula in a therapy-refractory patient. Biol Psychiatry 67(2):e9–e11
Schmidt MV, Wang XD, Meijer OC (2011) Early life stress paradigms in rodents: potential animal models of depression? Psychopharmacology (Berlin) 214:131–140
Schmuckermair C, Gaburro S, Sah A, Landgraf R, Sartori SB, Singewald N (2013) Behavioral and neurobiological effects of deep brain stimulation in a mouse model of high anxiety- and depression-like behavior. Neuropsychopharmacology 38:1234–1244
Schulz D, Mirrione MM, Henn FA (2010) Cognitive aspects of congenital learned helplessness and its reversal by the monoamine oxidase (MAO)-B inhibitor deprenyl. Neurobiol Learn Mem 93:291–301
Serretti A, Kato M, De Ronchi D, Kinoshita T (2007) Meta-analysis of serotonin transporter gene promoter polymorphism (5-HTTLPR) association with selective serotonin reuptake inhibitor efficacy in depressed patients. Mol Psychiatry 12:247–257
Shabel SJ, Murphy RT, Malinow R (2014) Negative learning bias is associated with risk aversion in a genetic animal model of depression. Front Hum Neurosci 8:1. doi:10.3389/fnhum.2014.00001
Shapero BG, Black SK, Liu RT, Klugman J, Bender RE, Abramson LY, Alloy LB (2014) Stressful life events and depression symptoms: the effect of childhood emotional abuse on stress reactivity. J Clin Psychol 70:209–223
Shumake J, Gonzalez-Lima F (2003) Brain systems underlying susceptibility to helplessness and depression. Behav Cogn Neurosci Rev 2:198–221
Shumake J, Poremba A, Edwards E, Gonzalez-Lima F (2000) Congenital helpless rats as a genetic model for cortex metabolism in depression. Neuroreport 11:3793–3798
Shumake J, Barrett D, Gonzalez-Lima F (2005) Behavioral characteristics of rats predisposed to learned helplessness: reduced reward sensitivity, increased novelty seeking, and persistent fear memories. Behav Brain Res 164:222–230
Siddaway AP, Taylor PJ, Wood AM, Schulz J (2015) A meta-analysis of perceptions of defeat and entrapment in depression, anxiety problems, posttraumatic stress disorder and suicidality. J Affect Disord 184:149–159
Slavich GM, Monroe SM, Gotlib IH (2011) Early parental loss and depression history: associations with recent life stress in major depressive disorder. J Psychiatr Res 45:1146–1152
Smith GW, Aubry JM, Dellu F, Contarino A, Bilezikjian LM, Gold LH, Chen R, Marchuk Y, Hauser C, Bentley CA, Sawchenko PE, Koob GF, Vale W, Lee KF (1998) Corticotropin releasing factor receptor 1-deficient mice display decreased anxiety, impaired stress response, and aberrant neuroendocrine development. Neuron 20:1093–1102
Solomon DA, Keller MB, Leon AC, Mueller TI, Lavori PW, Shea MT, Coryell W, Warshaw M, Turvey C, Maser JD, Endicott J (2000) Multiple recurrences of major depressive disorder. Am J Psychiatry 157:229–233
Solvason HB, Husain M, Fitgerald PB, Rosenquist P, McCall WV, Kimball J, Glimer W, Demitrack MA, Lisanby SH (2014) Improvement in quality of life with left prefrontal transcranial magnetic stimulation in patients with pharmacoresistant major depression: acute and six month outcomes. Brain Stimul 7:219–225
Souery D, Amsterdam J, de Montigny C, Lecrubier Y, Montgomery S, Lipp O, Racagni G, Zohar J, Mendlewicz J (1999) Treatment resistant depression: methodological overview and operational criteria. Eur Neuropsychopharmacol 9:83–91
Souery D, Oswald P, Massat I, Bailer U, Bollen J, Demyttenaere K, Kasper S, Lecrubier Y, Montgomery S, Serretti A, Zohar J, Mendlewicz J, Group for the Study of Resistant Depression (2007) Clinical factors associated with treatment resistance in major depressive disorder: results from a European multicenter study. J Clin Psychiatry 68:1062–1070
Steimer T, Driscoll P (2003) Divergent stress responses and coping styles in psychogenetically selected Roman high-(RHA) and low-(RLA) avoidance rats: behavioural, neuroendocrine and developmental aspects. Stress 6:87–100
Steiner MA, Wanisch K, Monory K, Marsicano G, Borroni E, Bächli H, Holsboer F, Lutz B, Wotjak CT (2008) Impaired cannabinoid receptor type 1 signaling interferes with stress-coping behavior in mice. Pharmacogenomics J 8:196–208
Stenzel-Poore MP, Heinrichs SC, Rivest S, Koob GF, Vale WW (1994) Overproduction of corticotropin-releasing factor in transgenic mice: a genetic model of anxiogenic behavior. J Neurosci 14:2579–2584
Steru L, Chermat R, Thierry B, Simon O (1985) The tail suspension test: a new method for screening antidepressants in mice. Psychopharmacology 85:367–370
Stewart LQ, Roper JA, Young WS 3rd, O’Carroll AM, Lolait SJ (2008) The role of the arginine vasopressin Avp1b receptor in the acute neuroendocrine action of antidepressants. Psychoneuroendocrinology 33:405–415
Stroud CB, Davila J, Moyer A (2008) The relationship between stress and depression in first onsets versus recurrences: a meta-analytic review. J Abnorm Psychol 117:206–213
Sunderland T, Cohen RM, Molchan S, Lawlor BA, Mellow AM, Newhouse PA et al (1994) High-dose selegiline in treatment-resistant older depressive patients. Arch Gen Psychiatry 51:607–615
Surget A, Wang Y, Leman S, Ibarguen-Vargas Y, Edgar N, Griebel G, Belzung C, Sibille E (2009) Corticolimbic transcriptome changes are state-dependent and region-specific in a rodent model of depression and of antidepressant reversal. Neuropsychopharmacology 34:1363–1380
Surget A, Tanti A, Leonardo ED, Laugeray A, Rainer Q, Touma C, Palme R, Griebel G, Ibarguen-Vargas Y, Hen R, Belzung C (2011) Antidepressants recruit new neurons to improve stress response regulation. Mol Psychiatry 16:1177–1188
Surget A, Van Nieuwenhujzen P, Heinzmann M, Westphal WP, Touma C, Belzung C (2012) Antidepressant effects in the stress reactivity mouse model. Society for Neuroscience, New Orleans
Svenningsson P, Chergui K, Rachleff I, Flajolet M, Zhang X, El Yacoubi M, Vaugeois JM, Nomikos GG, Greengard P (2006) Alterations in 5-HT1B receptor function by p11 in depression-like states. Science 311:77–80
Takahashi M, Shirayama Y, Muneoka K, Suzuki M, Sato K, Hashimoto K (2013) Personality traits as risk factors for treatment-resistant depression. PLoS One 8(5):e63756
Thase ME, Rush AJ (1997) When at first you don’t succeed: sequential strategies for antidepressant nonresponders. J Clin Psychiatry 58(Suppl 1):23–29
Timpl P, Spanagel R, Sillaber I, Kresse A, Reul JM, Stalla GK, Blanquet V, Steckler T, Holsboer F, Wurst W (1998) Impaired stress response and reduced anxiety in mice lacking a functional corticotropin-releasing hormone receptor 1. Nat Genet 19:162–166
Tizabi Y, Bhatti BH, Manaye KF, Das JR, Akinfiresoye L (2012) Antidepressant-like effects of low ketamine dose is associated with increased hippocampal AMPA/NMDA receptor density ratio in female Wistar-Kyoto rats. Neuroscience 213:72–80
Touma C, Bunck M, Glasl L, Nussbaumer M, Palme R, Stein H, Wolferstätter M, Zeh R, Zimbelmann M, Holsboer F, Landgraf R (2008) Mice selected for high versus low stress reactivity: a new animal model for affective disorders. Psychoneuroendocrinology 33:839–862
Touma C, Fenzl T, Ruschel J, Palme R, Holsboer F, Kimura M, Landgraf R (2009) Rhythmicity in mice selected for extremes in stress reactivity: behavioural, endocrine and sleep changes resembling endophenotypes of major depression. PLoS One 4(1):e4325
Trillat AC, Malagié I, Bourin M, Jacquot C, Hen R, Gardier AM (1998) Homozygote mice deficient in serotonin 5-HT1B receptor and antidepressant effect of selective serotonin reuptake inhibitors. C R Seances Soc Biol Fil 192:1139–1147
Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D et al (2006) Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatr 163:28–40
Tsoory M, Richter-Levin G (2006) Learning under stress in the adult rat is differentially affected by ‘juvenile’ or ‘adolescent’ stress. Int J Neuropsychopharmacol 9:713–728
Tsoory M, Cohen H, Richter-Levin G (2007) Juvenile stress induces a predisposition to either anxiety or depressive-like symptoms following stress in adulthood. Eur Neuropsychopharmacol 17:245–256
Uchida S, Hara K, Kobayashi A, Funato H, Hobara T, Otsuki K, Yamagata H, McEwen BS, Watanabe Y (2010) Early life stress enhances behavioral vulnerability to stress through the activation of REST4-mediated gene transcription in the medial prefrontal cortex of rodents. J Neurosci 30:15007–15018
Uher R, McGuffin P (2008) The moderation by the serotonin transporter gene of environmental adversity in the aetiology of mental illness: review and methodological analysis. Mol Psychiatry 13:131–146
Uhr M, Grauer MT (2003) abcb1ab P-glycoprotein is involved in the uptake of citalopram and trimipramine into the brain of mice. J Psychiatr Res 37:179–185
Uhr M, Steckler T, Yassouridis A, Holsboer F (2000) Penetration of amitriptyline, but not of fluoxetine, into brain is enhanced in mice with blood-brain barrier deficiency due to mdr1a P-glycoprotein gene disruption. Neuropsychopharmacology 22:380–387
Uhr M, Grauer MT, Holsboer F (2003) Differential enhancement of antidepressant penetration into the brain in mice with abcb1ab (mdr1ab) P-glycoprotein gene disruption. Biol Psychiatry 54:840–846
Uhr M, Tontsch A, Namendorf C, Ripke S, Lucae S, Ising M, Dose T, Ebinger M, Rosenhagen M, Kohli M, Kloiber S, Salyakina D, Bettecken T, Specht M, Pütz B, Binder EB, Müller-Myhsok B, Holsboer F (2008) Polymorphisms in the drug transporter gene ABCB1 predict antidepressant treatment response in depression. Neuron 57:203–209
Valverde O, Torrens M (2012) CB1 receptor-deficient mice as a model for depression. Neuroscience 204:193–206
van Gaalen MM, Stenzel-Poore M, Holsboer F, Steckler T (2002) Effects of transgenic overproduction of CRH on anxiety-like behaviour Eur. J Neurosci 15:2007–2015
Veerakumar A, Challis C, Gupta P, Da J, Upadhyay A, Beck SG, Berton O (2014) Antidepressant-like effects of cortical deep brain stimulation coincide with pro-neuroplastic adaptations of serotonin systems. Biol Psychiatry 76:203–212
Venzala E, García-García AL, Elizalde N, Delagrange P, Tordera RM (2012) Chronic social defeat stress model: behavioral features, antidepressant action, and interaction with biological risk factors. Psychopharmacology (Berlin) 224:313–325
Vincent MY, Jacobson L (2014) Glucocorticoid receptor deletion from the dorsal raphé nucleus of mice reduces dysphoria-like behavior and impairs hypothalamic-pituitary-adrenocortical axis feedback inhibition. Eur J Neurosci 39:1671–1681
Vincent MY, Hussain RJ, Zampi ME, Sheeran K, Solomon MB, Herman JP, Khan A, Jacobson L (2013) Sensitivity of depression-like behavior to glucocorticoids and antidepressants is independent of forebrain glucocorticoid receptors. Brain Res 1525:1–15
Vinkers CH, Groenink L, Pattij T, Olivier B, Bouwknecht JA (2011) 5-HT(1A) receptor sensitivity in 5-HT(1B) receptor KO mice is unaffected by chronic fluvoxamine treatment. Eur J Pharmacol 667:250–257
Vollmayr B, Henn FA (2001) Learned helplessness in the rat: improvements in validity and reliability. Brain Res Brain Res Protoc 8:1–7
Vollmayr B, Bachteler D, Vengeliene V, Gass P, Spanagel R, Henn F (2004) Rats with congenital learned helplessness respond less to sucrose but show no deficits in activity or learning. Behav Brain Res 150:217–221
Wang HN, Wang L, Zhang RG, Chen YC, Liu L, Gao F, Nie H, Hou WG, Peng ZW, Tan Q (2014) Anti-depressive mechanism of repetitive transcranial magnetic stimulation in rat: the role of the endocannabinoid system. J Psychiatr Res 51:79–87
Wei Q, Lu XY, Liu L, Schafer G, Shieh KR, Burke S, Robinson TE, Watson SJ, Seasholtz AF, Akil H (2004) Glucocorticoid receptor overexpression in forebrain: a mouse model of increased emotional lability. Proc Natl Acad Sci U S A 101:11851–11856
Wei Q, Hebda-Bauer EK, Pletsch A, Luo J, Hoversten MT, Osetek AJ, Evans SJ, Watson SJ, Seasholtz AF, Akil H (2007) Overexpressing the glucocorticoid receptor in forebrain causes an aging-like neuroendocrine phenotype and mild cognitive dysfunction. J Neurosci 27:8836–8844
Weiss JM, Kilts CD (1998) Animal models of depression and schizophrenia. In: Schatzberg AF, Nemeroff CB (eds) Textbook of psychopharmacology. American Psychiatric Press, Washington, pp 89–131
Weiss JM, Bailey WH, Goodman PA, Hoffman LJ, Ambrose MY, Salman S, Charry JM (1982) A model for neurochemical study of depression. In: Spiegelstein MY, Levy A (eds) Behavioral models and the analysis of drug action. Elsevier, Amsterdam, pp 195–223
Willne P, Belzung C, Scheel-Kruger J (2014) Resistance to antidepressant drugs: the case for a more predisposition-based and less hippocampocentric research paradigm. Behav Pharmacol 25:352–371
Willner P (1984) The validity of animal models of depression. Psychopharmacology 83:1–16
Willner P (1986) Validating criteria for animal models of human mental disorders: learned helplessness as a paradigm case. Prog Neuropsychopharmacol Biol Psychiatry 10:677–690
Willner P (1997) Validity, reliability and utility of the chronic mild stress (CMS) model of depression: a ten-year review and evaluation. Psychopharmacology 134:319–329
Willner P (2005) Chronic mild stress (CMS) revisited: consistency and behavioural-neurobiological concordance in the effects of CMS. Neuropsychobiology 52:90–110
Willner P (2009) Animal models for psychiatric states. In: Stolerman IP (ed) Encyclopedia of psychopharmacology. Springer, Heidelberg. doi:10.1007/978-3-540-68706-1_336
Willner P, Mitchell PJ (2002) The validity of animal models of predisposition to depression. Behav Pharmacol 13:169–188
Willner P, Towell A, Sampson D, Muscat R, Sophokleous S (1987) Reduction of sucrose preference by chronic mild stress and its restoration by a tricyclic antidepressant. Psychopharmacology 93:358–364
Willner P, Scheel-Kruger J, Belzung C (2013) The neuropharmacology of depression and antidepressant treatment. Neurosci Biobehav Rev 37:2331–2371
Winter C, Vollmayr B, Djodari-Irani A, Klein J, Sartorius A (2011) Pharmacological inhibition of the lateral habenula improves depressive-like behavior in an animal model of treatment resistant depression. Behav Brain Res 216:463–465
Zarate CA Jr, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, Charney DS, Manji HK (2006) A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry 63:856–864
Zhuang X, Gross C, Santarelli L, Compan V, Trillat A, Hen R (1999) Altered emotional states in knockout mice lacking 5-HT1A or 5-HT1B receptors. Neuropsychopharmacology 21:52–60
Zobel A, Maier W (2010) Pharmacogenetics of antidepressive treatment. Eur Arch Psychiatry Clin Neurosci 260:407–417
Zou YF, Ye DQ, Feng XL, Su H, Pan FM, Liao FF (2010) Meta-analysis of BDNF Val66Met polymorphism association with treatment response in patients with major depressive disorder. Eur Neuropsychopharmacol 20(8):535–544
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Willner, P., Belzung, C. Treatment-resistant depression: are animal models of depression fit for purpose?. Psychopharmacology 232, 3473–3495 (2015). https://doi.org/10.1007/s00213-015-4034-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-015-4034-7