Abstract
The environmental chemical 1,2-naphthoquinone (1,2-NQ) is implicated in the exacerbation of airways diseases induced by exposure to diesel exhaust particles (DEP), which involves a neurogenic-mediated mechanism. Plasma extravasation in trachea, main bronchus and lung was measured as the local 125I-bovine albumin accumulation. RT-PCR quantification of TRPV1 and tachykinin (NK1 and NK2) receptor gene expression were investigated in main bronchus. Intratracheal injection of DEP (1 and 5 mg/kg) or 1,2-NQ (35 and 100 nmol/kg) caused oedema in trachea and bronchus. 1,2-NQ markedly increased the DEP-induced responses in the rat airways in an additive rather than synergistic manner. This effect that was significantly reduced by L-732,138, an NK1 receptor antagonist, and in a lesser extent by SR48968, an NK2 antagonist. Neonatal capsaicin treatment also markedly reduced DEP and 1,2-NQ-induced oedema. Exposure to pollutants increased the TRPV1, NK1 and NK2 receptors gene expression in bronchus, an effect was partially suppressed by capsaicin treatment. In conclusion, our results are consistent with the hypothesis that DEP-induced airways oedema is highly influenced by increased ambient levels of 1,2-NQ and takes place by neurogenic mechanisms involving up-regulation of TRPV1 and tachykinin receptors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The respiratory system is responsible for gaseous exchange between the circulatory system and the outside world. Due to its position and functional role, the physical and chemical qualities of the inspired air can sometimes trigger acute and chronic inflammatory conditions in the airway wall that can lead to systemic effects (Nemmar et al. 2004; Kim et al. 2005; Franco et al. 2006; for review, see Widdicombe and Lee 2001). Moreover, epidemiological reports suggest that the healthy effects (e.g. cardiovascular disorders and airway diseases) of air pollution are primarily seen in susceptible patients, including those with compromised immune system (Wichmann et al. 2000) and diabetes (Goldberg et al. 2006). In fact, the increasing concentration of air pollution, such as ambient particulate matter (PM), is directly correlated with the high incidence of mortality and morbidity that are associated with respiratory (Frampton et al. 2004; Naess et al. 2007) and cardiovascular diseases (Peters et al. 2001; Pope et al. 2004; Jalaludin et al. 2004). Interestingly, in big cities such as São Paulo, the levels of air pollution are associated with the incidence of neonatal deaths (Pereira et al. 2004).
The engine emission diesel exhaust particles (DEP) represent one of the main constituents of ambient particulate matter (PM2.5) in most urban areas worldwide and, therefore, has been linked to respiratory and cardiovascular diseases (Harrod et al. 2003; Nemmar et al. 2007). By comparison, the highly reactive chemical quinones found in nature (e.g. plants, fungi) or in the environmental airborne pollutants including DEP (Cho et al. 2004; Xia et al. 2004), are well known to produce, via a complex mechanism, a variety of hazardous effects in humans, including changes in enzyme reactions, acute cytotoxicity, immunotoxicity and carcinogenesis (see reviews Monks and Jones 2002). More recently, a range of experimental approaches in vivo and in vitro has revealed some interesting toxicological findings mediated by the contaminant environmental quinones. For instance, a marked change in the leukocyte behaviour has been reported in rats treated with hydroquinone; this in turn accounted to exacerbate inflammatory responses in the animals (Macedo et al. 2006). Another in vitro study demonstrated that the redox-active 1,2-naphthoquinone (1,2-NQ) blocked acetylcholine-induced aorta endothelium-dependent vasorelaxation by inhibiting the endothelial nitric oxide synthase (eNOS) activity (Sun et al. 2006).
Human and animal airways, such as rodents, are densely innervated by a network of autonomic and sensory afferent nerves, which upon stimulation by a variety of endogenous inflammatory mediators and by exogenous chemical and/or biological agents initiate defensive responses including cough, mucus secretion, bronchoconstriction and vasodilatation (Lundberg et al. 1984; Coleridge and Coleridge 1984; Richardson and Webber 1987; Spina and Page 2002). The changes observed in the microvasculature [e.g. vasodilation (flare) and oedema due to plasma extravasation from postcapillary venules] in response to release of neuropeptides from stimulated sensory nerves are classically defined as neurogenic inflammation (for review, see Brain 1997). Interestingly, the presence of vanilloid receptor subtype 1 (TRPV1) in the respiratory system is likely to be implicated in cough and bronchoconstriction (Groneberg et al. 2004; Trevisani et al. 2005; Jia and Lee 2007).
In spite of toxicological evidences supporting the hazardous impact of quinones on cells and systems, little is known of the precise inflammatory interactions between components of DEP and sensory nerves. In this study, we have investigated the interaction between the acute exposure of the specific DEP organic chemical component 1,2-NQ and pure DEP. We have examined the inflammatory responses mediated by instillation of DEP alone and in combination to 1,2-NQ in the airway of healthy rats and the possible involvement of mechanisms involving sensory nerves.
Materials and methods
Chemicals
The [125I]-bovine serum albumin (specific activity = 0.037 MBq/μg) was provided by the Instituto de Pesquisas Nucleares (IPEN, São Paulo, SP, Brazil). The tachykinin NK2 receptor antagonist SR48968 was kindly donated by Sanofi-Aventis (Chilly-Mazarin, France). Capsaicin and the NK1 receptor antagonist L-732,138 were purchased from Sigma Chemical Co. (St. Louis, MO, USA). Lidocaine gel (2%) was obtained from Cristalia Produtos Químicos Ltda. (Itapira, São Paulo, SP, Brazil) and the anaesthetics xylazine and ketamine were purchased from König (Avellaneda, Argentina), respectively. The specific primers for both the tachykinins NK1 and NK2 receptors and TRPV1 receptor were obtained from Invitrogen (Sao Paulo, Brazil).
Preparation of pollutants samples
DEP was kindly donated by the National Institute for Environmental Studies, Japan. The chemical 1,2-NQ was obtained from Tokyo Kasei Industries (Tokyo, Japan) and was purified by a preparative thin-layer chromatography with a solvent of chloroform/methanol (9:2, v/v). The details of sample conditions for DEP are described elsewhere (Cho et al. 2004). Prior to animal treatment, a stock solution of DEP (5 mg/ml) was immediately dissolved in PBS containing DMSO 0.01%, whereas a stock solution of 1,2-NQ (3 μmol/ml) was made in PBS containing 0.01% DMSO and 0.05% Tween 80.
Animals and general procedures for pollutants exposure
Experiments were carried out on both male and female Wistar rats aged between 7 and 8 weeks (250–300 g) obtained from the Animal House at the Institute of Biomedical Sciences (University of São Paulo, Brazil). Protocols included in this study were in agreement with the guidelines of the Animal Care Committee of the ICB-USP (Brazil). They were housed five to a cage under specific environmental conditions (12 h/12 h light/darkness cycle) and were fed laboratory diet and filtered water ad libitum.
Healthy rats were anaesthetised via intraperitoneal (i.p.) injection with the mixture of ketamine (80 mg/kg) and xylazine (20 mg/kg) and randomly assigned to receive pollutant or its vehicle. Either DEP (1 and 5 mg/kg) or 1,2-NQ (35 and 100 nmol/kg) was prepared in different concentrations and a single injection of each compound or both (DEP 1 mg/kg plus 1,2-NQ 35 nmol/kg) or its corresponding vehicle (100 μl/rat; DMSO:Tween 80:PBS; 0.01:0.05:99.84%; v/v) was given intra-tracheal (i.tr) and the animals tested 15 min or 3 h later. Three separate groups of rats were treated with the tachykinin NK1 L-732,138 (5 mg/kg, i.p.; 30 min; Bang et al. 2004) and NK2 receptor antagonists SR48968 (1.6 μmol/kg, i.v.; 5 min; Trevisani et al. 2005) or with capsaicin as neonates (Jancso et al. 1977; Costa et al. 1997) prior to pollutant-treatment.
Ability of pollutants to elicit acute hyper-permeability in the rat airways
Anaesthetised rats were used and plasma extravasation was determined by the extravascular accumulation of labelled 125I-bovine serum albumin (125I-BSA; 0.0925 MBq/rat) previously injected via the tail vein, as described elsewhere (Costa et al. 1997). Varying doses of DEP (1 and 5 mg/kg), and 1,2-NQ (35 and 100 nmol/kg) or DEP plus 1,2-NQ (1 mg/kg + 35 nmol/kg), capsaicin (160 nmol/kg; Ricciardolo et al., 1994) or corresponding vehicles were injected by i.tr. route in the anaesthetised animals. After 15 min, a blood sample (1 ml) was taken by cardiac puncture and centrifuged (10,000 g, 5 min). The animals were killed by anaesthetic overdose followed by cervical dislocation. The chest was carefully opened and a cannula was inserted into the right ventricle, and slowly washed twice with 20 ml of heparinized (10 UI/ml) phosphate-buffered saline (PBS; 0.1 mol/l, pH 7.4). The blood and perfusion fluid were expelled through an incision made in the left ventricle. The trachea, left lobe of lung and main bronchus were rapidly excised and placed in a Petri dish, where the fat and connective sheaths were removed using fine forceps and scissors. The tissue samples were weighed and analysed using a counter (Cobra II, Packard BioScience, Dreieich, Germany) together with 100 μl of plasma. The volume of plasma extravasation was calculated by comparing the amount of the accumulation of intravenously injected (i.v.) of 125I-human serum albumin (125I-BSA) present in the tissue with the amount present in the known volume of blood plasma. The blood samples were centrifuged at 8,000×g for 10 min to obtain a plasma sample. Results were expressed as volume of plasma extravasation (μl) per g of wet tissue compared to total counts in 1 ml of plasma.
RNA extraction and quantification of TRPV1 and tachykinin NK1 and NK2 receptors gene expression by RT-PCR
Animals were treated by i.tr. route with the test agents or corresponding vehicles for 3 h as described above. The main bronchus was immediately removed from the animal weighed and the total RNA was extracted using Brazol reagent (LGC Biotechnology, São Paulo, Brazil). RT was conducted in a total volume of 50 μl containing 2 μg of total RNA using 10 U of Superscript II reverse transcriptase according to the manufacturer’s protocol (Invitrogen; São Paulo, Brazil). Tachykinins NK1 and NK2 and the vanilloid (TRPV1) receptor primers for PCR amplification of a 380, 491 and 498-bp fragments were obtained from Invitrogen (São Paulo, Brazil), accordingly (Xin et al. 2005; Franco-Penteado et al. 2006; Ni et al. 2006). The forward (sense) primers for NK1, NK2 and TRPV1 were as follows: CATCAACCCAGATCTCTACC, CATCACTGTGGACGAGGGGG and TCATGGGTGAGACCGTCAACAAG and the reverse (antisense) primers were GCTGGAGCTTTCTGTCTAGGA, TGTCTTCCTCAGTTGGTGTC, and TGGCTTAAGGGATCCCGTATAAT. PCR was performed in a total volume of 25 μl, using 2.5 μl of cDNA template, 2.5 μl of 10× PCR buffer, 1.5 mM MgCl2, 0.2 mM dNTPs, 2 units of Taq DNA polymerase, oligonucleotide primer pair [5 μM] and internal control primer: glyceraldehyde-3-phosphate dehydrogenase-GAPDH [3 μM] (Invitrogen, São Paulo, Brazil). After amplification for 40 cycles (45 seg at 94°C, 45 seg at 56°C and 1 min at 72°C, respectively), PCR products were electrophoresed in 2% agarose gels and viewed by ethidium bromide staining. Band fluorescence images were acquired and digitalized using a ChemiImager 5500 system (Alpha Innotech Corporation, San Leandro, CA, USA). For each sample, the rations between the densitometry value for each specific gene and the corresponding GAPDH were expressed relative to those for β-actin in the same sample.
Western blot analysis for 3-nitrotyrosine (3-NT)-containing proteins
A sample of 50 μg of total proteins contained in the main bronchus homogenate was electrophoresed on SDS-polyacrylamide gels (SDS-PAGE; 10% polyacrylamide) and further transferred to a nitrocellulose membrane (Laemmli 1970). After blocking non-specific sites with casein (0.2%), blots were sequentially overlaid overnight (12 h, at 4°C) with 500 ng/ml of the primary mouse monoclonal anti-NT (Upstate; New York, USA). An alkaline phosphatase-labelled rabbit anti-mouse antibody was employed as secondary antibody, and the immunoreactive bands were detected using a chemiluminescent assay kit (Lumi-Phos; Pierce; Rockford, IL, USA). The Bands intensities were estimated by densitometric analysis.
Capsaicin desensitization
All experiments were carried in accordance with the guidelines for animal care at the Institute of Biomedical Sciences (University of São Paulo, Brazil). The rostral part of the back of neonate rats (second day of life; 7–8 g) was cleaned, and approximately 50 mg of lidocaine gel (2%) was applied to the skin. After 10 min, rats received a single subcutaneous (s.c.) injection of capsaicin to deplete sensory neuropeptides (Jancso et al. 1977; Costa et al. 1997) or its corresponding volume of vehicle (100 μl/mouse; 10% ethanol and 10% Tween 80, in 0.9% w/v NaCl solution). Both male and female rats were used 60–70 days later.
Statistical analysis
Data are presented as mean ± SEM unless otherwise stated. Differences among data groups were assessed by ANOVA followed by Bonferroni’s modified t test or when requested by unpaired Student’s t tests as indicated. A P value of less than 0.05 was considered to indicate significance.
Results
Effect of simultaneous injection of DEP and 1,2-NQ on microvascular permeability in the rat airways
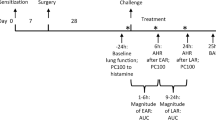
Intratracheal injection of DEP (1 and 5 mg/kg, n = 4–8) induced an increase in microvascular permeability (plasma extravasation) as measured by 125I-BSA in the isolated trachea and main bronchus, but with a lack of effect in the lung after 15 min (Fig. 1a). At 1 mg/kg, DEP was unable to evoke a significant plasma extravasation, whereas at 5 mg/kg, this substance caused a marked response in these structures as compared to vehicle-treated animals (Fig. 1a). Likewise, the i.tr. injection of the reactive compound 1,2-NQ, at 35 and 100 nmol/kg (n = 5–8), produced a significant and dose-dependent plasma extravasation in the trachea and main bronchus, but not in the lung (Fig. 1b).
The effect of intratracheal (i.tr.) injection of DEP (1 and 5 mg/kg, (a) and 1,2-NQ (35 and 100 nmol/kg, (b) in the rat trachea, main bronchus and lung. Either pollutants or its vehicle were itr. injected and plasma extravasation was measured by the extravascular accumulation of i.v. injected 125I-BSA in the rat airways. The results are expressed as microlitres of plasma extravasated/g of wet tissue. The columns represent the mean ± SEM of seven to nine rats. * P < 0.05; *** P < 0.001 compared to vehicle-treated group
Figure 2a and b shows that the non-significant plasma extravasation evoked by DEP (1 mg/kg) in the rat trachea and main bronchus was greatly increased by co-injection with 35 nmol/kg of 1,2-NQ (110 ± 18% and 350 ± 10.2% for trachea and bronchus, respectively, n = 9) in comparison to DEP alone.
Combination of DEP and 1,2-NQ on rat airway. Low doses of DEP (1 mg/kg) and 1,2-NQ (35 nmol/kg) resulted in additive effect of the increased vascular permeability (plasma extravasation) on the rat trachea (a) and main bronchus (b). The results are expressed as microlitres of plasma extravasated/g of wet tissue. The columns represent the mean ± SEM of five to eight rats. * P < 0.05; *** P < 0.001 compared to vehicle group and # P < 0.05; ### P < 0.01 compared to DEP or 1,2-NQ alone
Effect of the tachykinin NK1 and NK2 receptor antagonists and capsaicin depletion on the pollutant-induced plasma extravasation
The pretreatment of rats with the NK1 receptor antagonist L-732,138 (5 mg/kg, i.p.) acted in a potent manner to inhibit the plasma protein extravasation evoked by the mixture of DEP and 1,2-NQ in the trachea and main bronchus (Fig. 3, n = 4). Similarly, the NK2 receptor antagonist SR48968 (1.6 μmol/kg, i.v.) significantly inhibited the responses evoked by these pollutants in the trachea and main bronchus (n = 4, Fig. 3). The inhibitory response evoked by SR48968 in the rat trachea and main bronchus was smaller.
Effect of the tachykinin NK1 receptor antagonist L-732,138 and the NK2 receptor antagonist SR48968 on the changes in vascular permeability caused by DEP and 1,2-NQ on rat airway. The open columns represent the responses to pollutants in control rats, whereas the closed and striped columns show the response to pollutants in the presence of L-732,138 (5 mg/kg, 30 min, i.p.) and SR48968 (1.6 μmol/kg, 5 min, i.v.), respectively, in the trachea and main bronchus. The results are expressed as microlitres of plasma extravasated/g of wet tissue and are the mean ± SEM of three to four rats. * P < 0.05; ** P < 0.01 compared to control group
In order to investigate the direct involvement of C-fibres in DEP and 1,2-NQ-induced plasma extravasation in the rat trachea and main bronchus, experiments were conducted in rats treated with capsaicin as neonates. The ability of these pollutants to elicit plasma protein extravasation in the airways of capsaicin-treated rats was markedly reduced (P < 0.05, P < 0.01) when compared with healthy rats treated only with the pollutants (n = 10; Fig. 4). The i.tr. injection of the pollutants vehicle in healthy or capsaicin-treated animals did not evoke a significant plasma extravasation in the trachea and main bronchus (Fig. 4; n = 4).
Effect of the neonatal treatment with capsaicin on the changes in vascular permeability caused by DEP and 1,2-NQ. The open columns represent the responses to pollutants or their vehicle in healthy rats and the closed columns show the response to pollutants or their vehicle in capsaicin-treated rats. The results are expressed as microlitres of plasma extravasated/g of wet tissue and are the mean ± SEM of four to ten rats. * P < 0.05; *** P < 0.001 compared to healthy rats
To ascertain if the neonatal capsaicin treatment was effective, either healthy or capsaicin-treated rats were submitted to i.tr. injection of capsaicin (160 nmol/kg, n = 4) as previously described (Ricciardolo et al. 1994). Rats depleted of neuropeptides by neonatal treatment with capsaicin exhibited a marked reduction of plasma extravasation in the airways in response to i.tr. injection of capsaicin (79 ± 7.6 and 75 ± 26 μl/g for trachea and main bronchus, respectively; n = 4) when compared with values in healthy rats (165 ± 10.5 and 197.4 ± 11 μl/g for trachea and main bronchus, respectively; n = 4). The i.tr. injection of capsaicin vehicle in rats depleted of neuropeptides did not evoke a significant change in the increase of microvascular permeability in the trachea and main bronchus as compared to healthy animals that received the same treatment intratracheally (not shown; n = 4).
Pollutants-induced up-regulation of TRPV1 and the tachykinin NK1 and NK2 receptors expression in rat main bronchus
Following 3 h of treatment with DEP (1 mg/kg) or 1,2-NQ (35 nmolkg), the main bronchus cells of healthy rats did not exhibit a significant change in the gene expression of NK1, NK2 and TRPV1 receptors as compared to healthy rats treated with the pollutant–vehicle (Fig. 5a, c). However, the RT-PCR analysis in the main bronchus of healthy rats showed a marked induction of mRNA expression for these receptors by the mixture of DEP and 1,2-NQ (Fig. 5a, c). In capsaicin-treated rats exposed to DEP and 1,2-NQ, there was a significant inhibition in the mRNA expression levels of NK1, NK2 and TRPV1 receptors in the main bronchus as compared to healthy rats exposed to DEP and 1,2-NQ (Fig. 5a, c).
mRNA expression for TRPVR1 and NK1 and NK2 receptors in the main bronchus of rats after 3 h exposure to i.tr. injection of DEP and 1,2-NQ alone or co-injected. a The RT-PCR amplification of mRNA for TRPVR1 and b, c the mRNA for NK1 and NK2 receptors, respectively. d GAPDH that was used as the internal standard. The mRNA levels were estimated by densitometry of the bands. The open columns represent the responses to pollutants vehicle in healthy rats and both light and dark grey columns show the response to DEP or 1,2-NQ alone in healthy rats. The closed and striped columns illustrates the responses to the pollutants mixture (DEP and 1,2-NQ) in healthy and capsaicin-treated rats, respectively. The results are expressed as mean ± SEM of three to five rats. * P < 0.05 compared to control group that received the pollutants vehicle and # P < 0.05 compared to healthy rats exposed to DEP and 1,2-NQ
Nitration of protein tyrosine residues (3-NT) containing proteins in the rat main bronchus
We investigated whether acute exposure to both DEP and 1,2-NQ could increase protein tyrosine nitration (3-NT) in the main bronchus cells. The Western blot analysis did not reveal a significant difference in 3-NT contents in the main bronchus of rats exposed to these pollutants when compared to rats exposed to vehicle pollutants only (data not shown).
Discussion
Epidemiological studies have associated different levels of ambient pollutants with and adverse birth outcomes. However, the interaction between two environmental pollutants such as DEP and 1,2-NQ and pulmonary inflammation is poorly studied. We have used inflammatory parameters such as increased vascular permeability (plasma extravasation), an oxidative stress marker and assessment of gene expression for neurogenic modulators (e.g. tachykinins and TRPV1, the capsaicin receptor, a sensory neuronal TRP (transient receptor potential) ion channel, in airway chemosensation and inflammation, to test the hypothesis that the adverse pro-inflammatory effects of exposure to DEP can be exacerbated by organic chemical compounds such as 1,2-NQ via direct actions on capsaicin-sensitive sensory fibres. We have used the i.tr. instillation of substances as bolus amounts since this method of delivery has been shown to be a convenient and valid mode of administration of precise doses of foreign compounds, including PM, into the airways of mice and rats, as well as it allows the administration of precise doses into the airways of animals within a short period of time (Wallenborn et al. 2007; see review Driscoll et al. 2000). Here, using a low dose of DEP (1 mg/kg), which did not produce a significant plasma protein extravasation in the rat airways, we could observe that the co-administration of 1,2-NQ produced a clear increase in DEP-induced response in the rat trachea and main bronchus, but not in the lung. Responses to DEP and 1,2-NQ were additive rather than synergistic, i.e. the responses did not occlude each other. Taken together, these data suggest that 1,2-NQ might represent a crucial component by which DEP perpetuates and amplify the deleterious response capable to evoke clinical inflammatory signs.
Evidence shows that the sensory fibres and non-neuronal cells such as human nasal mucosa and bronchial epithelial cells contain TRPV1 receptors (Reilly et al. 2005; Seki et al. 2006). Moreover, the trachea and main bronchus are densely innervated by sensory nerves immunoreactive to substance P (Lundberg et al. 1984; Baluk et al. 1992) and the vasodilator CGRP (for review, see Dakhama et al. 2004). Herein, the involvement of TRPV1 and the tachykinin receptors gene expression in the mediation of DEP and 1,2-NQ-induced plasma extravasation was investigated as previous data indicated a possible involvement of TRPV1 receptors in 1,2-NQ-induced tracheal contraction in vitro (Kikuno et al. 2006) and substance P in DEP-induced pulmonary inflammation in rats in vivo (Wong et al. 2003). We found that the exposure of rats for more than 3 h to DEP and 1,2-NQ produced TRPV1 and both NK1 and NK2 receptors over-expression in the cells of rat main bronchus. This effect was not observed with a single dose of DEP, whilst the treatment with 1,2-NQ alone produced a significant increase in the tachykinin NK1 receptor gene expression, but failed to affect the gene expression of TRPV1 and NK2 receptors. This confirms our data that DEP-induced adverse effects on the airways (e.g. additive plasma protein extravasation) are greatly mediated by the organic contaminant 1,2-NQ, thus suggesting also that the additive oedema in response to simultaneous i.tr. injection of DEP and 1,2-NQ depend on up-regulation of TRPV1 and tachykinin receptors.
A variety of stimuli, such as LPS, cytokines and pollutants generates reactive oxygen species in the airway cells such as epithelial cells and macrophages (Imrich et al. 2007; Auger et al. 2006; Dagher et al. 2007), and this in turn leads to a worsening of airway inflammatory diseases, including asthma and bronchitis. Interestingly, the occurrence of 3-NT-containing proteins, a post-translational modification that may occur under oxidative stress conditions (mediated in some cases by nitric oxide and/or superoxide anion overproduction) has been shown in RAW 264.7 cell line treated with DEP (Xiao et al. 2005) as well as in the lung cells of rats exposed to fine PM (Laskin et al. 2003). However, we found no evidence of increased nitration of protein tyrosine residues in the main bronchus cells of rats treated acutely with DEP and 1,2-NQ, but it is necessary to examine the involvement of other oxidative stress markers to explain the oxidative reaction in the rat main bronchus.
In order to facilitate the better understanding of the adverse healthy effects of DEP with its contaminant 1,2-NQ, we investigated the possible underlying mechanisms involved in the rat airways. On the basis that if the final mechanism involved in DEP and 1,2-NQ-induced oedema in the rat airways is modulated by up regulation of TRPV1 and tachykinins (NK1 and NK2) receptors it would be expected that responses to these pollutants, like responses to capsaicin, would be modulated by a direct neurogenic-mediated component and, therefore, could be blocked by pretreatment of rats with capsaicin; a well-known tool used to deplete stock of neuropeptides (Jancso et al. 1977). We show clearly that the plasma extravasation evoked by these pollutants in the rat airways was significantly reduced, but not abolished, by this treatment. Thus, even though they partially act on the same population of capsaicin-sensitive fibres it is unlikely that this is the unique underlying mechanism.
The data obtained from the capsaicin-treated rats predict that DEP and 1,2-NQ-induced plasma extravasation in rat airways should be mediated by the endogenous release of the pro-inflammatory neuropeptide substance P. This peptide is most usually found in the peripheral sensory C-fibers and its main receptor (NK1) is widely distributed in the cells body, mainly on endothelial cells of post-capillaries venules, where increasing vascular permeability (oedema) and leukocyte transmigration take place (Rawlingson et al. 2004). We found this to be the case, as the tachykinin NK1 receptor antagonist markedly reduced the plasma extravasation evoked by DEP and 1,2-NQ in the rat trachea and main bronchus. To a lesser extent, although significantly, the plasma extravasation in response to these pollutants was also inhibited by the NK2 receptor antagonist, thus indicating that in addition to the NK1 receptor (and its endogenous agonist substance P), the NK2 receptor (and its endogenous agonist neurokinin A; NKA) plays a role in the inflammatory response evoked by DEP and 1,2-NQ. To our knowledge to date, this is the first time that the concomitant involvement of the NK2 receptor has been shown in the increased vascular permeability of the airways induced by acute exposure to DEP and 1,2-NQ. Nevertheless, this receptor has been involved in the deleterious effect of cigarette smoke (Tagawa et al. 2005) and ozone in the airways of guinea pigs (Fu et al. 2002). The current findings are supported by the RT-PCR results which showed that capsaicin treatment reduced the gene over-expression of both NK1 and NK2 receptors in the rat main bronchus in response to DEP and 1,2-NQ.
In conclusion, our results are consistent with the hypothesis that airway inflammation in response to acute exposure of DEP is highly influenced by increased ambient levels of 1,2-NQ, and that takes place by up regulation of TRPV1 and tachykinins (NK1 and NK2) receptors. These findings further contribute to growing evidences that implicates the up regulation of neurogenic components as one of the critical neurotoxicological mechanisms responsible for the increased adverse effects of PM in respiratory diseases.
References
Auger F, Gendron MC, Chamot C, Marano F, Dazy AC (2006) Responses of well-differentiated nasal epithelial cells exposed to particles: role of the epithelium in airway inflammation. Toxicol Appl Pharmacol 215:285–294
Baluk P, Nadel JA, McDonald DM (1992) Substance P-immunoreactive sensory axons in the rat respiratory tract: a quantitative study of their distribution and role in neurogenic inflammation. J Comp Neurol 319:586–598
Bang R, Biburger M, Neuhuber WL, Tiegs G (2004) Neurokinin-1 receptor antagonists protect mice from CD95- and tumor necrosis factor-alpha-mediated apoptotic liver damage. J Pharmacol Exp Ther 308:1174–1180
Brain SD (1997) Sensory neuropeptides: their role in inflammation and wound healing. Immunopharmacology 37:133–152
Cho AK, Schmitz DA, You Y, Rodriquez CE, Distefano E, Kumagai Y, Miguel AH, Eiguren A, Kobayashi T, Avol EL, Froines JR (2004) Determination of four quinones in Diesel exhaust particles, SRM1649A and athmosferic 2.5. Aerosol Sci Technol 38:1–14
Coleridge JC, Coleridge HM (1984) Afferent vagal C fibre innervation of the lungs and airways and its functional significance. Rev Physiol Biochem Pharmacol 99:1–110
Costa SK, de Nucci G, Antunes E, Brain SD (1997) Phoneutria nigriventer spider venom induces oedema in rat skin by activation of capsaicin sensitive sensory nerves. Eur J Pharmacol 339:223–226
Dagher Z, Garcon G, Billet S, Verdin A, Ledoux F, Courcot D, Aboukais A, Shirali P (2007) Role of nuclear factor-kappa B activation in the adverse effects induced by air pollution particulate matter (PM(2.5)) in human epithelial lung cells (L132) in culture. J Appl Toxicol 27:284–290
Dakhama A, Larsen GL, Gelfand EW (2004) Calcitonin gene-related peptide: role in airway homeostasis. Curr Opin Pharmacol 4:215–220 Review
Driscoll KE, Costa DL, Hatch G, Henderson R, Oberdorster G, Salem H, Schlesinger RB (2000) Intratracheal instillation as an exposure technique for the evaluation of respiratory tract toxicity: uses and limitations. Toxicol Sci 55:24–35 Review
Frampton MW, Utell MJ, Zareba W, Oberdorster G, Cox C, Huang LS, Morrow PE, Lee FE, Chalupa D, Frasier LM, Speers DM, Stewart J (2004) Effects of exposure to ultrafine carbon particles in healthy subjects and subjects with asthma. Res Rep Health Eff Inst 126:49–63
Franco Lino, dos Santos A, Damazo AS, Beraldo de Souza HR, Domingos HV, Oliveira-Filho RM, Oliani SM, Costa SK, Tavares de Lima W (2006) Pulmonary neutrophil recruitment and bronchial reactivity in formaldehyde-exposed rats are modulated by mast cells and differentially by neuropeptides and nitric oxide. Toxicol Appl Pharmacol 214:35–42
Franco-Penteado CF, De Souza IA, Lima CS, Teixeira SA, Muscara MN, De Nucci G, Antunes E (2006) Effects of neonatal capsaicin treatment in the neutrophil production, and expression of preprotachykinin-I and tachykinin receptors in the rat bone marrow. Neurosci Lett 407:70–73
Fu L, Kaneko T, Ikeda H, Nishiyama H, Suzuki S, Okubo T, Trevisani M, Geppetti P, Ishigatsubo Y (2002) Tachykinins via Tachykinin NK(2) receptor activation mediate ozone-induced increase in the permeability of the tracheal mucosa in guinea-pigs. Br J Pharmacol 135:1331–1335
Goldberg MS, Burnett RT, Yale JF, Valois MF, Brook JR (2006) Associations between ambient air pollution and daily mortality among persons with diabetes and cardiovascular disease. Environ Res 100:255–267
Groneberg DA, Niimi A, Dinh QT, Cosio B, Hew M, Fischer A, Chung KF (2004) Increased expression of transient receptor potential vanilloid-1 in airway nerves of chronic cough. Am J Respir Crit Care Med 170(12):1276–1280
Harrod KS, Jaramillo RJ, Rosenberger CL, Wang SZ, Berger JA, McDonald JD, Reed MD (2003) Increased susceptibility to RSV infection by exposure to inhaled diesel engine emissions. Am J Respir Cell Mol Biol 28:451–463
Imrich A, Ning Y, Lawrence J, Coull B, Gitin E, Knutson M, Kobzik L (2007) Alveolar macrophage cytokine response to air pollution particles: oxidant mechanisms. Toxicol Appl Pharmacol 218:256–264
Jalaludin BB, O′Toole BI, Leeder SR (2004) Acute effects of urban ambient air pollution on respiratory symptoms, asthma medication use, and doctor visits for asthma in a cohort of Australian children. Environ Res 95:32–42
Jancso G, Kiraly E, Jancso-Gabor A (1977) Pharmacologically induced selective degeneration of chemosensitive primary sensory neurones. Nature 270:741–743
Jia Y, Lee LY (2007) Role of TRPV receptors in respiratory diseases. Biochim Biophys Acta 1772(10):1182 Review
Kikuno S, Taguchi K, Iwamoto N, Yamano S, Cho AK, Froines JR, Kumagai Y (2006) 1, 2-Naphthoquinone activates vanilloid receptor 1 through increased protein tyrosine phosphorylation, leading to contraction of guinea pig trachea. Toxicol Appl Pharmacol 210:47–54
Kim JY, Chen JC, Boyce PD, Christiani DC (2005) Exposure to welding fumes is associated with acute systemic inflammatory responses. Occup Environ Med 62:157–163
Laemmli UK (1970) Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227:680–685
Laskin DL, Morio L, Hooper K, Li TH, Buckley B, Turpin B (2003) Peroxides and macrophages in the toxicity of fine particulate matter in rats. Res Rep Health Eff Inst 117:53–63
Lundberg JM, Hokfelt T, Martling CR, Saria A, Cuello C (1984) Substance P-immunoreactive sensory nerves in the lower respiratory tract of various mammals including man. Cell Tissue Res 235:251–261
Macedo SM, Lourenço EL, Borelli P, Fock RA, Ferreira JMJ, Farsky SH (2006) Effect of in vivo phenol or hydroquinone exposure on events related to neutrophil delivery during an inflammatory response. Toxicology 220:126–135
Monks TJ, Jones DC (2002) The metabolism and toxicity of quinones, quinonimines, quinone methides, and quinone-thioethers. Curr Drug Metab 3:425–438 Review
Naess O, Nafstad P, Aamodt G, Claussen B, Rosland P (2007) Relation between concentration of air pollution and cause-specific mortality: four-year exposures to nitrogen dioxide and particulate matter pollutants in 470 neighborhoods in Oslo. Norway Am J Epidemiol 165:435–443
Nemmar A, Hoylaerts MF, Hoet PH, Nemery B (2004) Possible mechanisms of the cardiovascular effects of inhaled particles: systemic translocation and prothrombotic effects. Toxicol Lett 149:243–253
Nemmar A, Al-Maskari S, Ali BH, Al-Amri IS (2007) Cardiovascular and lung inflammatory effects induced by systemically administered diesel exhaust particles in rats. Am J Physiol Lung Cell Mol Physiol 292(3):L664–L670
Ni D, Gu Q, Hu HZ, Gao N, Zhu MX, Lee LY (2006) Thermal sensitivity of isolated vagal pulmonary sensory neurons: role of transient receptor potential vanilloid receptors. Am J Physiol Regul Integr Comp Physiol 291:R541–R550
Pereira FL, Silva DA, Sopelete MC, Sung SS, Taketomi EA (2004) Mite and cat allergen exposure in Brazilian public transport vehicles. Ann Allergy Asthma Immunol 93:179–184
Peters A, Dockery DW, Muller JE, Mittleman MA (2001) Increased particulate air pollution and the triggering of myocardial infarction. Circulation 103(23):2810–2815
Pope CA 3rd, Burnett RT, Thurston GD, Thun MJ, Calle EE, Krewski D, Godleski JJ (2004) Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation 109:71–77
Rawlingson A, Costa SKP, Brain SD (2004) Role of tachykinins in neurogenic inflammation of the skin and other external surfaces. In: Holzer P (ed) Tachykinins, handbook of experimental pharmacology, vol 164. Springer, Swiss, pp 1–569
Reilly CA, Johansen ME, Lanza DL, Lee J, Lim JO, Yost GS (2005) Calcium-dependent and independent mechanisms of capsaicin receptor (TRPV1)-mediated cytokine production and cell death in human bronchial epithelial cells. J Biochem Mol Toxicol 19:266–275
Ricciardolo FL, Nadel JA, Bertrand C, Yamawaki I, Chan B, Geppetti P (1994) Tachykinins and kinins in antigen-evoked plasma extravasation in guinea-pig nasal mucosa. Eur J Pharmacol 261:127–132
Richardson PS, Webber SE (1987) The control of mucous secretion in the airways by peptidergic mechanisms. Am Rev Respir Dis 136:S72–S76
Seki N, Shirasaki H, Kikuchi M, Sakamoto T, Watanabe N, Himi T (2006) Expression and localization of TRPV1 in human nasal mucosa. Rhinology 44:128–134
Spina D, Page CP (2002) Pharmacology of airway irritability. Curr Opin Pharmacol 2:264–272 Review
Sun Y, Taguchi K, Sumi D, Yamano S, Kumagai Y (2006) Inhibition of endothelial nitric oxide synthase activity and suppression of endothelium-dependent vasorelaxation by 1,2-naphthoquinone, a component of diesel exhaust particles. Arch Toxicol 80(5):280–285
Tagawa A, Kaneko T, Nishiyama H, Shinohara T, Sato T, Geppetti P, Ishigatsubo Y (2005) Cigarette smoke increases mucosal permeability in guinea pig trachea via tachykinin NK2 receptor activation. Eur J Pharmacol 507:223–228
Trevisani M, Patacchini R, Nicoletti P, Gatti R, Gazzieri D, Lissi N, Zagli G, Creminon C, Geppetti P, Harrison S (2005) Hydrogen sulfide causes vanilloid receptor 1-mediated neurogenic inflammation in the airways. Br J Pharmacol 145:1123–1131
Wallenborn JG, McGee JK, Schladweiler MC, Ledbetter AD, Kodavanti UP (2007) Systemic translocation of particulate matter-associated metals following a single intratracheal instillation in rats. Toxicol Sci 98(1):231–239
Wichmann HE, Spix C, Tuch T, Wolke G, Peters A, Heinrich J, Kreyling WG, Heyder J (2000) Daily mortality and fine and ultrafine particles in Erfurt, Germany part I: role of particle number and particle mass. Res Rep Health Eff Inst 98:87–94
Widdicombe J, Lee LY (2001) Airway reflexes, autonomic function, and cardiovascular responses. Environ Health Perspect Suppl 4:579–584 Review
Wong SS, Sun NN, Keith I, Kweon CB, Foster DE, Schauer JJ, Witten ML (2003) Tachykinin substance P signaling involved in diesel exhaust-induced bronchopulmonary neurogenic inflammation in rats. Arch Toxicol 77:638–650
Xia T, Korge P, Weiss JN, Li N, Venkatesen MI, Sioutas C, Nel A (2004) Quinones and aromatic chemical compounds in particulate matter induce mitochondrial dysfunction: implications for ultrafine particle toxicity. Environ Health Perspect 112:1347–1358
Xiao GG, Nel AE, Loo JA (2005) Nitrotyrosine-modified proteins and oxidative stress induced by diesel exhaust particles. Electrophoresis 26:280–292
Xin H, Tanaka H, Yamaguchi M, Takemori S, Nakamura A, Kohama K (2005) Vanilloid receptor expressed in the sarcoplasmic reticulum of rat skeletal muscle. Biochem Biophys Res Commun 332:756–762
Acknowledgments
We thank Dra Simone A. Teixeira, Dra. Ana A. Varriano, Maria A. Barreto, Dr Enilton A. Camargo for technical support. This work was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP). TELES A.M. and S.K.P.C. are supported by research fellowships from CNPq.
Conflicts of interest statement
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00204-009-0506-z
Rights and permissions
About this article
Cite this article
Teles, A.M., Kumagai, Y., Brain, S.D. et al. Involvement of sensory nerves and TRPV1 receptors in the rat airway inflammatory response to two environment pollutants: diesel exhaust particles (DEP) and 1,2-naphthoquinone (1,2-NQ). Arch Toxicol 84, 109–117 (2010). https://doi.org/10.1007/s00204-009-0427-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-009-0427-x