Abstract
Summary
In the present meta-analysis, reductions in the risk of hip fracture with milk consumption were only observed among American adults, but not among Scandinavian adults, possibly because milk products are more commonly fortified with vitamin D in the former population than in Scandinavian countries. The reduction in the risk of hip fracture was also observed with yogurt consumption, which is often associated with healthy lifestyles and dietary patterns that contribute to improved bone health.
Introduction
Although dairy products contain bone-beneficial nutrients, the association between dairy consumption and the risk of hip fracture remains equivocal. Fueling this uncertainty, the elevated risk of hip fracture in association with milk consumption was observed in a cohort of Swedish women. A systematic review and meta-analysis of prospective cohort studies was performed to critically evaluate the association, or lack thereof, between dairy consumption (milk, yogurt, and cheese) and the risk of hip fracture.
Methods
A random effects model was used to generate the summary relative risks (RRs) with their 95% confidence intervals (CIs) for the associations of interest.
Results
In the meta-analysis of the highest versus lowest category of consumption, higher consumption of yogurt (RR 0.78, 95% CI 0.68, 0.90), but not milk (RR 0.86, 95% CI 0.73, 1.02) or cheese (RR 0.85, 95% CI 0.66, 1.08), was associated with a lower risk of hip fracture. For milk, the reduced risk of fracture with higher milk consumption was observed in the USA (RR 0.75, 95% CI 0.65, 0.87), but not in Scandinavian countries (RR 1.00, 95% CI 0.85, 1.17). These findings were further supported by the fact that American studies (RR 0.93, 95% CI 0.88, 0.98; per 1 glass/day), but not Scandinavian studies (RR 1.01, 95% CI 0.95, 1.07; per 1 glass/day), demonstrated a linear association between milk consumption and the risk of hip fracture.
Conclusions
The cumulative evidence from prospective cohort studies reassuringly suggests that the risk of hip fracture may not be elevated among people who consume milk, yogurt, and cheese, and that a greater consumption of milk or yogurt may even be associated with a lower risk of hip fracture depending on the factors that may differ across the population of interest.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dairy products, including milk and other dairy foods, contain a unique package of nutrients that are essential for bone health. Following the scientific review, the European Food Safety Authority has authorized the beneficial claims, in terms of bone health, associated with several nutrients, including protein, calcium, phosphorus, magnesium, manganese, zinc, vitamin D, and vitamin K [1]. All these nutrients, except vitamin D, are naturally present in considerable amounts in dairy products [2, 3]. In certain countries, vitamin D is either mandatorily or voluntarily added to dairy products, particularly milk, which contributes to the dietary intake of this vitamin [4, 5]. Given that dairy products are excellent sources of bone-beneficial nutrients, the role of dairy products in bone health has been extensively studied, with a special focus on the prevention of osteoporosis and bone fractures.
While accumulating evidence suggests that dairy consumption is inversely associated with bone turnover markers and positively associated with bone mineral content or bone mineral density (BMD) [6,7,8,9,10], the potential beneficial role of dairy products in the prevention of fracture is less convincing. No randomized controlled trials (RCTs) till date have investigated the effect of dairy consumption on fracture risk. Observational studies on the association between dairy consumption (mainly milk) and hip fracture risk have yielded inconsistent results [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. Fueling this uncertainty, an elevated risk of hip fracture associated with milk consumption has been reported among Swedish women [22]; this controversial finding has been inaccurately exaggerated in media coverage and fiercely debated among researchers and practitioners (https://www.bmj.com/content/349/bmj.g6015/rapid-responses). Several recent meta-analyses [27,28,29] on this topic observed that milk or dairy consumption was not significantly associated with the risk of hip fracture. Although pooled data are important for the establishment of a more robust estimate of the association, particularly when the findings of the individual studies are conflicting, the findings of previous meta-analyses [27,28,29] may have been biased by the considerable methodological issues in their analyses (Table S1). These methodological issues include the inclusion of studies [11, 12] that compared low versus high milk consumption and the risk of hip fracture in the meta-analysis of high versus low intake [27,28,29]; inclusion of studies [15, 17] with incorrect exposure [27, 29]; double-counting [29] of data from the same study cohort [17, 22]; and several important studies being either missed or not included. More importantly, those meta-analyses [27,28,29] did not critically evaluate the lack of an association between milk or dairy consumption and the risk of hip fracture. By failing to do so, people may question the nutritive value of dairy products on the basis of the findings of observational studies, when, in fact, they have been shown to have favorable effects on bone health in RCTs [6,7,8,9,10].
Although dairy products contain numerous bone-beneficial nutrients, the main rationale behind the recommendation of dairy products for the optimization of bone health is largely driven by the fact that they provide considerable amounts of high bioavailable calcium, the mineral most important for bone health. The ability of the body to properly absorb dietary calcium is determined by the presence of vitamin D. The vitamin D metabolite—1,25-dihydroxycholecalciferol—acts as a hormone in the regulation of calcium and phosphorus metabolism for the maintenance of normal serum calcium and phosphorus concentrations that ensure normal bone mineralization [3, 4]. In humans, vitamin D can be naturally synthesized through the action of sunlight to the skin [4]. However, owing to the current modern lifestyle, which is characterized by daily activities that take place indoors, the degree of sun exposure is often insufficient for optimal vitamin D synthesis [4]. Moreover, sun-induced vitamin D synthesis is greatly influenced by several factors, such as season, latitude, altitude, skin pigmentation, and sunscreen use [4]. In this case, the dietary intake of vitamin D is also important to ensure the adequate intake of this vitamin. Since only a few foods in nature contain vitamin D, the fortification of widely consumed foods with vitamin D offers a solution to this issue. The majority of studies on the association between milk consumption and the hip fracture risk were conducted either in the USA [18, 21, 23, 25], in which various fluid milk products are voluntarily fortified with vitamin D [5]; or Scandinavian countries, including Norway [20, 26] and Sweden [22], in which low-fat milk is mandatorily fortified with vitamin D [5]; and Denmark [24], in which vitamin D fortification has not been widely implemented and accepted [30]. Hypothetically, dairy fats may enhance the absorption of fat-soluble vitamin D; the addition of vitamin D in milk and its derived products may promote the intestinal absorption of their calcium and phosphorus content, leading to a greater degree of bone mineralization. Given this consideration, we hypothesized that vitamin D fortification, to some extent, may modify the association between milk consumption and the risk of hip fracture and that the lack of an overall association between milk consumption and the risk of hip fracture may have been driven by studies conducted in Scandinavian countries, in which vitamin D fortification is less prevalent than in the USA. The potential role of vitamin D fortification as a potential modifying factor in the association between milk consumption and hip fracture risk has not been considered in previous meta-analyses [27,28,29]. Further investigation of this possibility is warranted to refine the evidence on this topic.
To facilitate a better interpretation and expand upon the current knowledge of the influence of dairy consumption on hip fracture risk, we performed a systematic review and meta-analysis of prospective cohort studies to critically evaluate the association, or lack thereof, between dairy consumption (milk, yogurt, and cheese) and the risk of hip fracture, with a special focus on disentangling the controversy surrounding milk.
Methods
The present meta-analysis was prepared and reported according to the Meta-analysis of Observational Studies in Epidemiology (MOOSE) checklist [31]. Two investigators (K.H. and X.D.) independently performed the literature search, study selection, data extraction, and quality assessment. Discrepancies or disagreements between the two reviewers were resolved by a team meeting.
Search strategy
The PubMed and Web of Science databases were searched for relevant articles published in any language from their inception to October 31, 2019. The following search terms were used for the identification of the relevant articles: (milk OR dairy OR cheese OR yogurt) AND fracture. We also manually reviewed the references cited in the retrieved articles and previous meta-analyses [27,28,29] to minimize the likelihood of missing studies.
Study selection
The Participants, Interventions, Comparisons, Outcomes, and Study design (PICOS) criteria are presented in Table 1. In brief, the prospective cohort studies were considered relevant only if they reported risk estimates (relative risks [RRs] or hazard ratios [HRs]) with their 95% confidence intervals (CIs) for the association between higher versus lower (reference) consumption of milk, yogurt, or cheese in adulthood and the risk of hip fracture. Therefore, prospective cohort studies that compared the association between lower versus higher (reference) consumption of milk, yogurt, or cheese in adulthood and the risk of hip fracture were excluded. Studies with a cross-sectional or case-control design were also excluded because the quality of the evidence of these studies is generally lower than that of prospective cohort studies. If multiple articles reported data from the same study population, we included only the one with the longest follow-up period to avoid double-counting. Given that the nutritional contents of different dairy products vary [6, 7], it may not be appropriate to consider them as a single exposure. Therefore, total dairy consumption was not investigated in the present meta-analysis.
Data extraction and quality assessment
A standardized form was used to extract the following information from the included studies: first author name, year of publication, setting, mean of follow-up, mean age, proportion of men, dietary and fracture ascertainments, exposure comparison, variables adjusted for in the maximally adjusted models, and the risk estimates with their 95% CIs from the maximally adjusted models. The Newcastle-Ottawa Scale (NOS) [32] was used to judge the quality of the included studies.
Statistical analysis
The RRs were chosen as measures of the association between milk, yogurt, and cheese consumption and the risk of hip fracture. A DerSimonian and Laird random effects model [33] was used to generate the summary RRs with their 95% CIs for the associations of interest. If the studies separately reported risk estimates according to sex, these sex-specific risk estimates were first pooled together before being included in the overall meta-analysis to simplify the presentation of the data displayed in the forest plot. However, sex-specific risk estimates were used in their current form in the subgroup analyses by sex. In the main analysis, the risk of hip fracture associated with the highest versus lowest category of milk, yogurt, and cheese consumption was estimated. In addition, the risk of hip fracture associated with each additional glass-per-day of milk consumption was estimated using the method proposed by Greenland and Longnecker [34] and Orsini et al. [35]; this method requires studies to report at least three quantitative exposure categories of milk consumption. The risk of hip fracture associated with each increment in the level of yogurt or cheese consumption was not estimated because the limited number of studies on these associations precludes meaningful analysis. Where possible, subgroup and meta-regression analyses were performed according to sex, vitamin D fortification hypothesis (USA versus Scandinavian countries; see “Introduction”), and adjustment for certain variables (age, body mass index (BMI), height, physical activity, alcohol, smoking, energy intake, or vitamin D or calcium supplementation) to investigate the potential source of heterogeneity and effect modifiers. The Q and I2 statistics were used to assess the heterogeneity across studies. For the Q statistic, P < 0.1 was considered statistically significant; for the I2 statistic, the following cut-off values were assigned to define the degree of heterogeneity: < 25% (low heterogeneity), 25–50% (moderate heterogeneity), and > 50% (high heterogeneity) [36]. Begg’s rank correlation test and Egger’s linear regression test were used to assess potential publication bias [37]. If publication bias was evident, the trim and fill method was performed to adjust for it [38]. All statistical analyses were performed using STATA software, version 11.0 (STATA Corp., College Station, TX, USA). All P values were two-sided, and the level of significance was set at < 0.05.
Results
Literature review and study characteristics
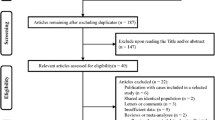
The study selection process is presented in Figure S1. The initial database searches resulted in a total of 1834 articles (602 from PubMed and 1232 from Web of Science). Twenty-eight articles were eligible for full-text evaluation following duplicate article removal and title/abstract screening. Of these 28 articles, 19 were excluded for various reasons, as presented in Appendix S1. Finally, nine articles [18,19,20,21,22,23,24,25,26] with a total of 14 study cohorts were included in the present meta-analysis. The articles were published between 1997 and 2019. The characteristics of the included studies are summarized in Table S2. One study [18] enrolled only women, while the remaining investigated men and women. One study [19] was conducted in Japan, while the remaining were conducted in either the USA [18, 21, 23, 25] or Scandinavian countries (Norway [20, 26], Sweden [22], and Denmark [24]). Dietary information was collected using a food frequency questionnaire (FFQ) in all studies. In most studies, data on fracture events were obtained through a self-reported questionnaire, and the findings were further confirmed by medical records and radiographic and operative reports. All studies reported adjusted risk estimates; however, there were considerable differences in the selection and number of variables accounted for in the maximally adjusted models. All studies were considered to have good quality (NOS ≥ 7).
Meta-analysis
Milk consumption and the risk of hip fracture
Fourteen prospective cohort studies, with a total of 9564 hip fracture events among 363,383 participants, reported in nine articles [18,19,20,21,22,23,24,25,26], were included in the meta-analysis of the association between the highest versus lowest category of milk consumption and the risk of hip fracture. Higher milk consumption was not associated with the risk of hip fracture (RR 0.86, 95% CI 0.73, 1.02; Fig. 1), with a high heterogeneity across the studies (I2 = 60.1%; P heterogeneity = 0.01). There was no evidence of publication bias (P Begg’s = 0.10; P Egger’s = 0.21). The results of the subgroup analyses and meta-regression analyses are presented in Table 2. Vitamin D fortification policy, sex, and adjustment for certain variables appeared to be sources of heterogeneity across the studies. Meta-regression analyses revealed that vitamin D fortification policy could be a potential effect modifier (P meta-regression = 0.04) for the association between milk consumption and the risk of hip fracture, showing that a reduced risk of hip fracture was only evident in the USA (RR 0.75, 95% CI 0.65, 0.87), but not in Scandinavian countries (RR 1.00, 95% CI 0.85, 1.17). Seven articles [17,18,20, 22, 23, 25, 26] provided sufficient data for the investigation of the potential linear association between milk consumption and the risk of hip fracture. There was no linear association between milk consumption and the risk of hip fracture (RR 0.97, 95% CI 0.92, 1.03; per 1 glass/day). However, a reduction in the risk with increased milk consumption was observed in the USA (RR 0.93, 95% CI 0.88, 0.98; per 1 glass/day), but not in Scandinavian countries (RR 1.01, 95% CI 0.95, 1.07; per 1 glass/day), confirming the results of the main analysis.
Consumption of cheese or yogurt and the risk of hip fracture
Six prospective cohort studies, with a total of 8217 hip fracture events among 234,654 participants, reported in four articles [21,22,23, 25], were included in the meta-analysis of the association between the highest versus lowest category of yogurt consumption and the risk of hip fracture. Furthermore, eight prospective cohort studies, with a total of 8860 hip fracture events among 305,157 participants, reported in four articles [22,23,24,25], were included in the meta-analysis of the association between the highest versus lowest category of cheese consumption and the risk of hip fracture. Higher yogurt (RR 0.78, 95% CI 0.68, 0.90; Fig. 2), but not cheese (RR 0.85, 95% CI 0.66, 1.08; Fig. 2), consumption was associated with a lower risk of hip fracture. The heterogeneity was high in the analysis of cheese (I2 = 76.9%; P heterogeneity < 0.01) and low in the analysis of yogurt (I2 = 14.3%; P heterogeneity = 0.32). There was no evidence of publication bias (all P Begg’s > 0.36; all P Egger’s > 0.45). Higher yogurt consumption was inversely associated with the risk of hip fracture in both men (RR 0.80, 95% CI 0.66, 0.96) and women (RR 0.72, 95% CI 0.60, 0.86), whereas higher cheese consumption was not associated with the risk of hip fracture in either men (RR 0.88, 95% CI 0.65, 1.01) or women (RR 0.77, 95% CI 0.53, 1.12).
Discussion
Summary of the primary findings
In the highest versus lowest category meta-analysis, higher consumption of yogurt, but not milk or cheese, was associated with a lower risk of hip fracture. For milk, a reduced risk of hip fracture with higher milk consumption was observed in the USA, but not in Scandinavian countries; these findings were further supported by the fact that American studies, but not Scandinavian studies, demonstrated a linear association between milk consumption and the risk of hip fracture.
Milk consumption and the risk of hip fracture
The best available evidence on the association between milk consumption and the risk of hip fracture was predominantly derived from prospective cohort studies conducted in the USA [18, 21, 23, 25] and Scandinavian countries (Norway [20, 26], Sweden [22], and Denmark [24]), all countries in which the levels of milk consumption [39], hip fracture probability [40], and hip fracture incidence [41] are relatively high. The results of individual studies generally showed a tendency towards an inverse association between higher milk consumption and the risk of hip fracture, except for the dose-dependent increase in the risk of hip fracture with milk consumption among Swedish women in the Swedish Mammography Cohort [22]. In this cohort, however, yogurt or cheese consumption was associated with a lower risk of hip fracture. The authors hypothesized that milk may have an undesirable effect because it is the major dietary source of D-galactose, which has been shown to cause premature aging in animal models via oxidative stress and chronic inflammation, factors that contribute to bone and muscle loss in humans. In contrast, fermented dairy products, such as yogurt and cheese, have lower or untraceable levels of galactose and distinct functional properties compared to milk due to the presence of probiotics and/or prebiotics that may confer additional bone benefits beyond the effects of their nutrients (e.g., protein, calcium, phosphorus). The potential influence of fermented dairy products on the risk of hip fracture will be discussed in detail in the section below (see “Fermented dairy products and the risk of hip fracture”).
Instead of interpreting the aforementioned results with caution, the media has exaggerated and improperly interpreted the findings of the Swedish Mammography Cohort [22], and this may create public skepticism and confusion that may cause people to unnecessarily stop or avoid consuming milk, when in fact they contain bone-beneficial nutrients [2, 3, 6,7,8]. Observational studies cannot prove or disprove the presence of a direct cause and effect between milk consumption and fracture incidence owing to the influence of genetic and lifestyle factors, and it is almost impossible to control all these factors. Although currently no RCT have focused on this association, accumulating evidence from RCTs does not support the potentially detrimental effect of milk on bone health, showing that milk consumption generally has favorable effects on BMD [42,43,44] and bone turnover markers [45,46,47,48,49] in adults.
The average age at the baseline of the women enrolled in the Swedish Mammography Cohort [22] was approximately 53 years, and after approximately 20 years of follow-up, they will be in their 70s. It is known that the prevalence of osteoporosis increases progressively with age [50]. In Sweden, osteoporosis is prevalent among older women, with one in three women aged between ages 70 and 79 years having osteoporosis [51]. Since milk contains nutrients that are essential for the maintenance of bone health, older women at a high risk of fracture or with osteoporosis may have been consuming more milk than those without this condition. Osteoporosis per se confers a greater risk of fracture development. Scandinavian countries have the highest incidences of hip fracture, worldwide [40, 41]. The incidence of hip fracture among Swedish women is among the highest, globally [40, 41]. Thus, the increased risk of hip fracture observed in association with higher milk consumption may have been driven by osteoporosis. Notably, a history of osteoporosis or BMD was not considered in the maximally adjusted model.
Milk fortification is utilized to improve the dietary intake of certain nutrients, particularly vitamin D. Thus, the nutrient concentration in milk may differ across countries depending on the fortification policy. It has been suggested that the increased risk of fracture among the women in the Swedish Mammography Cohort [22] may be because milk in Sweden was fortified with high amounts of vitamin A at the time the dietary questionnaires were administered [7]; a high intake of vitamin A and retinol has been linked with a higher risk of hip fracture [52]. However, the increased risk of hip fracture was corroborated after adjustment for several nutrients related to milk consumption, including retinol. In the USA, fluid milk (also includes acidified milk and cultured milk) and yogurt are voluntarily fortified with vitamin D (1.05 μg/100 g for milk and 2.225 μg/100 g for yogurt) [5]. In Sweden, milk with a maximum fat content of 1.5% must be fortified with 0.38–0.50 μg/100 g vitamin D; in 2015, this mandatory fortification policy was proposed to include all fluid milk products with a maximum fat content of 3% (0.95–1.10 μg/100 g for milk and 0.75–1.10 μg/100 g for fermented milk) [5]. In Norway, only extra low-fat milk was fortified with vitamin D (0.40 μg/100 g) [5]. In Denmark, vitamin D fortification has not yet been widely implemented and accepted [30].
It is particularly important to acknowledge that adequate vitamin D is necessary for optimal calcium absorption [3, 4]. A recent meta-analysis [53] of RCTs suggested that calcium in combination with vitamin D, but not vitamin D alone, is associated with a reduced risk of hip fracture among postmenopausal women compared to a placebo. In a 1-year clinical trial, calcium and vitamin D-fortified milk intake was associated with significantly reduced bone turnover marker levels among Chinese postmenopausal women in Malaysia compared to regular milk [42]. Higher consumption levels of total dairy, fluid dairy, and milk were associated with a higher BMD among Puerto Rican adults aged 46–79, particularly in those with vitamin D sufficiency [54]. The Framingham Study [55] found that, among vitamin D supplement users, but not nonusers, higher intakes of milk, fluid dairy, and milk + yogurt + cheese were associated with a higher lumbar spine BMD, while higher intakes of milk + yogurt + cheese were associated with a higher trochanter BMD. The inconsistency or heterogeneity across studies investigating the association between milk consumption and hip fracture risk could, to some extent, be explained by the presence of different vitamin D fortification policies across these countries. In the present meta-analysis, the reduced risk of hip fracture with higher consumption of milk was only observed in the USA, but not in Scandinavian countries, possibly because the vitamin D fortification of milk products is more commonly performed in the USA than Scandinavian countries. Alternately, the lack of an association between milk consumption and hip fracture risk in Scandinavian countries could be attributed due to the very high consumption of dairy products in these countries [39]. Therefore, it would be more difficult to detect a statistically significant association because even those in the lower categories of milk consumption are likely to consume high amounts of other dairy products that may potentially influence the association between milk consumption and the risk of hip fracture. Only one [19] prospective cohort study focusing on the association between milk consumption and the risk of hip fracture has been performed in a country other than the USA and Scandinavian countries. A study in Japan [19], in which the vitamin D fortification of milk products is not commonly performed [56], found that higher milk consumption was not associated with hip fracture risk. However, a study [56] in female Japanese college students showed that consumption of vitamin D-fortified milk for 8 weeks was associated with increased serum levels of calcium and fibroblast growth factor-23 and reduced serum levels of bone-specific alkaline phosphatase and N-terminal telopeptide of type I collagen. While most studies focusing on the association between milk consumption and the risk of hip fracture adjusted for the intake of calcium or vitamin D from supplements [18, 21,22,23, 26] or other non-dairy sources [25], this does not account for the vitamin D synthesized in the skin following sun exposure. Thus, information on the vitamin D status of the participants may provide valuable insights into the association between milk consumption and the risk of hip fracture. Furthermore, if vitamin D is truly among the nutrients in milk that influences the risk of hip fracture, comparisons should take into account not only fortification status (fortified versus regular) but also the amounts of vitamin D added in milk.
In the present meta-analysis, the inverse association between higher milk consumption and hip fracture risk was somewhat stronger in studies that did not adjust for BMI than in those that adjusted for it, although the difference between the groups was not significant (P meta-regression = 0.24; Table 2). BMI and waist circumference have been shown to influence the association between milk consumption and the risk of hip fracture [25]. The Nurses’ Health Study and the Health Professionals Follow-up Study [25] showed that milk consumption was associated with a lower risk of hip fracture among men and women with a BMI of at least 30 kg/m2. The joint association of BMI and milk consumption with the risk of hip fracture may be complicated by mechanical loading, bone strength, and soft tissue padding. Cumulative evidence [57, 58] from observational studies indicates that a low BMI is associated with a higher risk of hip fracture, independent of BMD, whereas a high BMI is associated with a reduced risk of hip fracture, conditional on BMD. BMD tends to increase with increasing BMI as a consequence of greater skeletal loading from excess weight. While excess weight may increase the fracture risk as a consequence of an increased impact forces in a fall, the increased impact forces are likely to be offset by a greater absorption of impact forces by extra soft tissue padding [59], leading to a reduction in the risk of fracture at certain sites among individuals with a high BMI [57,58,59]. The Norwegian Counties Study and Five Counties Study demonstrated a tendency towards an increased risk of hip fracture with a consumption of four or more glasses of milk per day among women with a BMI lower than 24 kg/m2 [26]. As the authors acknowledged, this positive association could be due to the high prevalence of cigarette smoking, physical inactivity, and poor self-rated health among women with a BMI lower than 24 kg/m2 [26]. Nonetheless, the reduced soft tissue padding around the hip region may not provide sufficient protection during falls in those with a low BMI, resulting in an increased hip fracture risk.
Unlike high BMI, high waist circumference—a marker of abdominal adiposity—has been linked to an increased risk of hip fracture [60]. It has been suggested that the inflammatory cytokines released by visceral adipocytes may stimulate bone resorption and suppress bone formation [61]. The low-grade inflammation associated with excess visceral adipose tissue may be counterbalanced by positive factors associated with body fatness, such as estrogen [62]. As the production of estrogen by the ovaries ceases after menopause, the adipose tissue becomes the primary site of endogenous estrogen in postmenopausal women. Thus, the higher the degree of adiposity after menopause, the higher the levels of adipose tissue-derived estrogens [63]. Moreover, higher serum estradiol concentrations have been shown to be associated with a lower risk of hip fracture [64]. Indeed, the reduction in the risk of hip fracture associated with milk consumption was only observed in fracture cases among women, but not men, with a higher waist circumference [25].
Fermented dairy products and the risk of hip fracture
Lactic acid fermentation has been long used to prolong the shelf life of dairy products. Fermented dairy products, similar to the milk from which they are made, also contain important nutrients that are essential for bone health [65], while at the same time the presence of probiotics and/or prebiotics provide distinct functional properties that may confer additional bone-related benefits [8, 65, 66]. For this reason, fermented dairy products may have greater effects on bone health than milk, which neither contains probiotics nor prebiotics [8].
Prebiotics and probiotics have been proposed to be involved in the regulation of bone health via the modulation of gut microbiome, increased intestinal barrier function, and reduced intestinal inflammation, leading to several local and systemic responses [8, 65, 67, 68], as follows: reduced inflammation degree in the gut, blood, and bone; increased levels of metabolite such as short-chain fatty acids that can enhance calcium absorption and signal locally in the gut and bone; and increased levels of bacterial secreted factors and intestinal hormones such as incretins and serotonin that are known to regulate bone density [8, 65, 67, 68]. The aforementioned local and systemic responses may result in reduced osteoclast activity and/or increased osteoblast activity, leading to increased bone density, structure, and strength. Indeed, emerging evidence from RCTs indicates that probiotics and prebiotics may contribute to improved bone health in humans [8, 65]. In this case, probiotic supplementation has been shown to prevent bone loss [69, 70], reduce the bone resorption degree [71], and increase BMD [72] in postmenopausal women. Furthermore, prebiotic supplementation has been shown to consistently result in improved calcium absorption in adolescents [73,74,75] and postmenopausal women [76, 77].
Accumulating evidence from RCTs suggests that fermented dairy products may improve bone health through the maintenance of calcium balance and prevention of secondary hyperparathyroidism, as well as an age-related increase in the rate of bone resorption and age-related bone loss [65]. The association between the consumption of fermented dairy products, cheese and yogurt, and the risk of hip fracture has been investigated in several prospective cohort studies [21,22,23,24,25]. Although both yogurt and cheese are fermented dairy products, our findings indicate that higher intakes of yogurt, but not cheese, are associated with a lower risk of hip fracture in both men and women. The inverse association between higher yogurt, but not cheese, consumption and the risk of hip fracture could, to some extent, be explained by several factors. First, the lack of an association between cheese and hip fracture risk could be attributed to the limited statistical power for the detection of weak association, as a consequence of the small number of studies that investigated this association. Second, the association between cheese consumption and hip fracture risk may differ according to the type of cheese. Unfortunately, we could not test this possibility because all studies on this association did not stratify their analyses according to cheese type. The findings of longitudinal analyses of bone microstructure in postmenopausal women indicated that age-related cortical bone loss was attenuated at non-bearing bone sites among those who consumed fermented dairy products (including yogurts, fresh cheese, “petit-suisse” cheese, quark, and kefir), but not among those who consumed milk or ripened cheese [78]. Future studies on the association between cheese consumption and hip fracture risk must focus on the different cheese types (e.g., ripened cheese, fresh cheese) consumed by participants. Third, the stronger inverse association observed between yogurt consumption and hip fracture risk could be due to the fact that yogurt consumption is often associated with healthy lifestyles and dietary patterns [79] that may contribute to improved bone health [80]. Evidence from observational studies suggests that people who consume yogurt are more likely to be more physically active, smoke less frequently, consume lower amounts of alcohol, and have higher education levels and better nutrition-related knowledge than non-consumers [79].
Dairy consumption and the risk of fracture other than hip fracture
There is a lack of sufficient data from prospective cohort studies focusing on the association between dairy consumption and the risk of fractures other than hip fracture [12, 18, 81,82,83,83]. The association between milk consumption and the risk of vertebral fracture has been investigated in several studies [12, 18, 81,82,83,83], none of which found an association. Similarly, milk consumption was not associated with the risks of ankle fracture [18], proximal humeral fracture [18], and wrist fracture [12, 18]. A study [12] in elderly French people indicated the absence of an association between low cheese consumption and the risks of vertebral fracture and wrist fracture, whereas low yogurt consumption was associated with an increased risk of wrist fracture only. All the above-mentioned studies were hampered by the limited number of fracture events at each site and relatively short follow-up period. Further data on the association between dairy consumption and the risk of fractures other than hip fracture are warranted.
Limitations
Several caveats need to be taken into account in the interpretation of the results of the present meta-analysis. First, observational studies are subject to residual confounders that may influence the observed associations. Residual confounders may remain unadjusted due to either the lack of information or confounders that were not considered. Although age, sex, physical activity, BMI, height, alcohol consumption, and smoking were considered in the majority of the included studies, nearly all of them lacked information on potentially important confounders, such as vitamin D status; the use of certain medications; a history of osteoporosis, frailty, falls, and certain medical conditions; hormone levels; and bone markers, all of which have been shown to influence fracture risk [85,87,87,87]. Second, dairy consumption was assessed using a FFQ. FFQ data are subject to bias related to memory and sincerity, which may lead to the imprecise estimation of the true association. For example, people tend to overestimate the intake of foods perceived as healthy and underreport the intake of foods perceived as less healthy [88]. To address this limitation associated with FFQs, several fatty acids (C14:0, C15:0, C17:0, and trans-C16:1n-7) were used as biomarkers of dairy intake [89,89,91]. It would be of interest to investigate the associations between these fatty acids and the risk of fracture. Third, the meta-analyses of cheese and yogurt were based on a limited number of studies. Therefore, subgroup analyses could not be performed, preventing robust conclusions from being drawn. Fourth, the high heterogeneity observed in the analysis of milk or cheese consumption and hip fracture risk suggests that the results should be interpreted with caution. For milk, the subgroup analyses revealed that the heterogeneity across studies was driven by the Scandinavian studies, as we found no heterogeneity among the American studies. For cheese, we were unable to perform subgroup analyses for the identification of the source of heterogeneity owing to the limited number of studies on this association. Finally, the generalizability of our findings may be limited as the included studies were predominantly conducted in America and Scandinavian countries, in which the level of dairy consumption [39] and hip fracture probability [40, 41] are high. More studies must be conducted in other countries/continents.
Implications
While some people avoid dairy product intake for a variety of reasons, many others cherish the flavor of milk, cheese, and yogurt and the potential health benefits derived from the nutrients present in them. Individual judgment may play an important part in the decision of whether the health benefits of the intake of milk and other dairy foods outweigh the potential health risks, often influenced by various sources of information. Given the high importance of dairy products as major sources of important dietary nutrients, worldwide, any information based on weak science or cherry-picking evidence may cause confusion and skepticism among consumers. Our findings, together with a substantial proportion of the current scientific evidence [7, 93,94,95,92,96] on this field, demonstrate the scientifically unsound and misleading nature of claims that state that dairy products cause many diseases, such as bone fractures. The commonly observed misconceptions and facts [98,99,100,101,102,103,104,105,106,107,108,109,110,97,116] regarding dairy products and bone health are compiled in Table 3. It is safe to say that dairy products neither guarantee healthy and strong bones, nor are they deleterious to bone health. Having a healthy lifestyle, including participation in physical activity, maintenance of a healthy weight, limited alcohol consumption, avoidance of smoking, and intake of a healthy, balanced diet that provides an adequate supply of bone health-beneficial nutrients, is essential for the maintenance of bone health [80, 109]. In this case, dairy products can be incorporated into a healthy, balanced diet as they contain a unique package of valuable nutrients that are important for bone health [2, 3, 6,7,8]. Altogether, there is no compelling reason to discourage moderate milk and dairy consumption in individuals without a contraindicating condition (e.g., lactose intolerance, milk allergy).
Conclusions and future directions
The cumulative evidence from prospective cohort studies reassuringly suggests that the risk of hip fracture may not be elevated among people who consume milk, yogurt, and cheese, and that higher consumption levels of milk or yogurt may even be associated with a lower risk of hip fracture depending on factors that differ across populations of interest. Additional data from prospective cohort studies focusing on the associations between the consumption of different types of dairy products, preferably stratified by fat content and fortification status, during different periods in life and the risks of fracture at different sites across different subpopulations and genetic variations, may refine the current knowledge on this topic. It is also of interest to investigate the associations between the biomarkers of dairy product intake and fracture risk. Owing to the fact that observational studies cannot establish causal relationships, long-term, large-scale RCTs are warranted to establish the causal relationship between dairy consumption and the risk of fracture.
References
Commission Regulation (EU) No 432/2012 of 16 May 2012 establishing a list of permitted health claims made on foods, other than those referring to the reduction of disease risk and to children’s development and health. https://eurlex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2012:136:0001:0040:EN:PDF. Accessed 20 Dec 2019
Burrow K, Young W, McConnell M, Carne A, Bekhit AE (2018) Do dairy minerals have a positive effect on bone health? Compr Rev Food Sci F 17:989–1005
Hess JM, Jonnalagadda SS, Slavin JL (2018) Dairy foods: current evidence of their effects on bone, cardiometabolic, cognitive, and digestive health. Compr Rev Food Sci F 17:251–268
Schmid A, Walther B (2013) Natural vitamin D content in animal products. Adv Nutr 4:453–462
Itkonen ST, Erkkola M, Lamberg-Allardt CJE (2018) Vitamin D fortification of fluid milk products and their contribution to vitamin D intake and vitamin D status in observational studies-a review. Nutrients 10:E1054
Rizzoli R (2014) Dairy products, yogurts, and bone health. Am J Clin Nutr 99:1256S–1262S
Rozenberg S, Body JJ, Bruyère O, Bergmann P, Brandi ML, Cooper C, Devogelaer JP, Gielen E, Goemaere S, Kaufman JM, Rizzoli R, Reginster JY (2016) Effects of dairy products consumption on health: benefits and beliefs--a commentary from the Belgian Bone Club and the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases. Calcif Tissue Int 98:1–17
Geiker NRW, Mølgaard C, Iuliano S et al (2019) Impact of whole dairy matrix on musculoskeletal health and aging-current knowledge and research gaps. Osteoporos Int 31(4):601-615
van den Heuvel EGHM, Steijns JMJM (2018) Dairy products and bone health: how strong is the scientific evidence? Nutr Res Rev 31:164–178
Kouvelioti R, Josse AR, Klentrou P (2017) Effects of dairy consumption on body composition and bone properties in youth: a systematic review. Curr Dev Nutr 1:e001214
Kanis JA, Johansson H, Oden A, de Laet C, Johnell O, Eisman JA, Mc Closkey E, Mellstrom D, Pols H, Reeve J, Silman A, Tenenhouse A (2005) A meta-analysis of milk intake and fracture risk: low utility for case finding. Osteoporos Int 16:799–804
Feart C, Lorrain S, Ginder Coupez V et al. (2013) Adherence to a Mediterranean diet and risk of fractures in French older persons. Osteoporos Int 24:3031–3041
Owusu W, Willett WC, Feskanich D et al. (1997) Calcium intake and the incidence of forearm and hip fractures among men. J Nutr 127:1782–1787
Feskanich D, Willett WC, Colditz GA (2003) Calcium, vitamin D, milk consumption, and hip fractures: a prospective study among postmenopausal women. Am J Clin Nutr 77:504–511
Feskanich D, Bischoff-Ferrari HA, Frazier AL, Willett WC (2014) Milk consumption during teenage years and risk of hip fractures in older adults. JAMA Pediatr 168:54–60
Michaëlsson K, Melhus H, Bellocco R, Wolk A (2003) Dietary calcium and vitamin D intake in relation to osteoporotic fracture risk. Bone 32:694–703
Michaëlsson K, Wolk A, Lemming EW, Melhus H, Byberg L (2018) Intake of milk or fermented milk combined with fruit and vegetable consumption in relation to hip fracture rates: a cohort study of Swedish women. J Bone Miner Res 33:449–457
Cumming RG, Cummings SR, Nevitt MC, Scott J, Ensrud KE, Vogt TM, Fox K (1997) Calcium intake and fracture risk: results from the study of osteoporotic fractures. Am J Epidemiol 145:926–934
Fujiwara S, Kasagi F, Yamada M, Kodama K (1997) Risk factors for hip fracture in a Japanese cohort. J Bone Miner Res 12:998–1004
Meyer HE, Pedersen JI, Løken EB, Tverdal A (1997) Dietary factors and the incidence of hip fracture in middle-aged Norwegians. A prospective study. Am J Epidemiol 145:117–123
Sahni S, Tucker KL, Kiel DP, Quach L, Casey VA, Hannan MT (2013) Milk and yogurt consumption are linked with higher bone mineral density but not with hip fracture: the Framingham offspring study. Arch Osteoporos 8:119
Michaëlsson K, Wolk A, Langenskiöld S et al (2014) Milk intake and risk of mortality and fractures in women and men: cohort studies. BMJ 349:g6015
Sahni S, Mangano KM, Tucker KL, Kiel DP, Casey VA, Hannan MT (2014) Protective association of milk intake on the risk of hip fracture: results from the Framingham original cohort. J Bone Miner Res 29:1756–1762
Bergholdt HKM, Larsen MK, Varbo A, Nordestgaard BG, Ellervik C (2018) Lactase persistence, milk intake, hip fracture and bone mineral density: a study of 97 811 Danish individuals and a meta-analysis. J Intern Med 284:254–269
Feskanich D, Meyer HE, Fung TT, Bischoff-Ferrari HA, Willett WC (2018) Milk and other dairy foods and risk of hip fracture in men and women. Osteoporos Int 29:385–396
Holvik K, Meyer HE, Laake I, Feskanich D, Omsland TK, Søgaard AJ (2019) Milk drinking and risk of hip fracture. The Norwegian epidemiologic osteoporosis studies (NOREPOS). Br J Nutr 121:709–718
Bian S, Hu J, Zhang K, Wang Y, Yu M, Ma J (2018) Dairy product consumption and risk of hip fracture: a systematic review and meta-analysis. BMC Public Health 18:165
Matía-Martín P, Torrego-Ellacuría M, Larrad-Sainz A, Fernández-Pérez C, Cuesta-Triana F, Rubio-Herrera MÁ (2019) Effects of milk and dairy products on the prevention of osteoporosis and osteoporotic fractures in Europeans and non-Hispanic whites from North America: a systematic review and updated meta-analysis. Adv Nutr 10(suppl_2):S120–S143
Malmir H, Larijani B, Esmaillzadeh A (2019) Consumption of milk and dairy products and risk of osteoporosis and hip fracture: a systematic review and meta-analysis. Crit Rev Food Sci Nutr:1–16
Grønborg IM, Tetens I, Ege M, Christensen T, Andersen EW, Andersen R (2019) Modelling of adequate and safe vitamin D intake in Danish women using different fortification and supplementation scenarios to inform fortification policies. Eur J Nutr 58:227–232
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283:2008–2012
Wells GA, Shea B, O’connell D et al. (2000) The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 20 Dec 2019
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135:1301–1309
Orsini N, Bellocco R, Greenland S (2006) Generalized least squares for trend estimation of summarized dose-response data. Stata J 6:40–57
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56:455–463
Canadian Dairy Information Centre. DC007 World dairy products consumption. https://www.dairyinfo.gc.ca/index_e.php?s1=dff-fcil&s2=cons&s3=conscdn. Accessed 20 Dec 2019
Kanis JA, Johnell O, De Laet C, Jonsson B, Oden A, Ogelsby AK (2002) International variations in hip fracture probabilities: implications for risk assessment. J Bone Miner Res 17:1237–1244
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C, IOF Working Group on Epidemiology and Quality of Life (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256
Kruger MC, Chan YM, Lau LT, Lau CC, Chin YS, Kuhn-Sherlock B, Todd JM, Schollum LM (2018) Calcium and vitamin D fortified milk reduces bone turnover and improves bone density in postmenopausal women over 1 year. Eur J Nutr 57:2785–2794
Daly RM, Bass S, Nowson C (2006) Long-term effects of calcium-vitamin-D3-fortified milk on bone geometry and strength in older men. Bone 39:946–953
Reyes-Garcia R, Mendoza N, Palacios S et al (2018) Effects of daily intake of calcium and vitamin D-enriched milk in healthy postmenopausal women: a randomized, controlled, double-blind nutritional study. J Women's Health (Larchmt) 27:561–568
Josse AR, Tang JE, Tarnopolsky MA, Phillips SM (2010) Body composition and strength changes in women with milk and resistance exercise. Med Sci Sports Exerc 42:1122–1130
Bonjour JP, Brandolini-Bunlon M, Boirie Y, Morel-Laporte F, Braesco V, Bertière MC, Souberbielle JC (2008) Inhibition of bone turnover by milk intake in postmenopausal women. Br J Nutr 100:866–874
Kruger MC, Booth CL, Coad J, Schollum LM, Kuhn-Sherlock B, Shearer MJ (2006) Effect of calcium fortified milk supplementation with or without vitamin K on biochemical markers of bone turnover in premenopausal women. Nutrition 22:1120–1128
Kruger MC, Schollum LM, Kuhn-Sherlock B, Hestiantoro A, Wijanto P, Li-Yu J, Agdeppa I, Todd JM, Eastell R (2010) The effect of a fortified milk drink on vitamin D status and bone turnover in post-menopausal women from South East Asia. Bone 46:759–767
Kruger MC, Ha PC, Todd JM, Kuhn-Sherlock B, Schollum LM, Ma J, Qin G, Lau E (2012) High-calcium, vitamin D fortified milk is effective in improving bone turnover markers and vitamin D status in healthy postmenopausal Chinese women. Eur J Clin Nutr 66:856–861
Hernlund E, Svedbom A, Ivergård M et al (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136
The Swedish Council on Technology Assessment in Health Care. Osteoporosis - Prevention, Diagnosis and Treatment. A Systematic Review. Stockholm, Sweden: 2003. 2 Volumes, 165/1+2
Wu AM, Huang CQ, Lin ZK, Tian NF, Ni WF, Wang XY, Xu HZ, Chi YL (2014) The relationship between vitamin a and risk of fracture: meta-analysis of prospective studies. J Bone Miner Res 29:2032–2039
Barrionuevo P, Kapoor E, Asi N, Alahdab F, Mohammed K, Benkhadra K, Almasri J, Farah W, Sarigianni M, Muthusamy K, al Nofal A, Haydour Q, Wang Z, Murad MH (2019) Efficacy of pharmacological therapies for the prevention of fractures in postmenopausal women: a network meta-analysis. J Clin Endocrinol Metab 104:1623–1630
Mangano KM, Noel SE, Sahni S, Tucker KL (2019) Higher dairy intakes are associated with higher bone mineral density among adults with sufficient vitamin D status: results from the Boston Puerto Rican osteoporosis study. J Nutr 149:139–148
Sahni S, Mangano KM, Kiel DP, Tucker KL, Hannan MT (2017) Dairy intake is protective against bone loss in older vitamin D supplement users: the Framingham study. J Nutr 147:645–652
Suzuki Y, Maruyama-Nagao A, Sakuraba K, Kawai S (2014) Milk fortified with vitamin D could reduce the prevalence of vitamin D deficiency among Japanese female college students. Arch Osteoporos 9:188
Johansson H, Kanis JA, Odén A, McCloskey E, Chapurlat RD, Christiansen C, Cummings SR, Diez-Perez A, Eisman JA, Fujiwara S, Glüer CC, Goltzman D, Hans D, Khaw KT, Krieg MA, Kröger H, LaCroix A, Lau E, Leslie WD, Mellström D, Melton LJ 3rd, O'Neill TW, Pasco JA, Prior JC, Reid DM, Rivadeneira F, van Staa T, Yoshimura N, Zillikens MC (2014) A meta-analysis of the association of fracture risk and body mass index in women. J Bone Miner Res 29:223–233
De Laet C, Kanis JA, Odén A et al (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16:1330–1338
Ishii S, Cauley JA, Greendale GA, Nielsen C, Karvonen-Gutierrez C, Ruppert K, Karlamangla AS (2014) Pleiotropic effects of obesity on fracture risk: the study of women’s health across the nation. J Bone Miner Res 29:2561–2570
Li X, Gong X, Jiang W (2017) Abdominal obesity and risk of hip fracture: a meta-analysis of prospective studies. Osteoporos Int 28:2747–2757
Kawai M, de Paula FJ, Rosen CJ (2012) New insights into osteoporosis: the bone-fat connection. J Intern Med 272:317–329
Shapses SA, Sukumar D (2012) Bone metabolism in obesity and weight loss. Annu Rev Nutr 32:287–309
Hidayat K, Yang CM, Shi BM (2018) Body fatness at a young age, body fatness gain and risk of breast cancer: systematic review and meta-analysis of cohort studies. Obes Rev 19:254–268
Cauley JA, Danielson ME, Jammy GR, Bauer DC, Jackson R, Wactawski-Wende J, Chlebowski RT, Ensrud KE, Boudreau R (2017) Sex steroid hormones and fracture in a multiethnic cohort of women: the Women’s Health Initiative study (WHI). J Clin Endocrinol Metab 102:1538–1547
Rizzoli R, Biver E (2018) Effects of fermented milk products on bone. Calcif Tissue Int 102:489–500
Heller KJ (2001) Probiotic bacteria in fermented foods: product characteristics and starter organisms. Am J Clin Nutr 73(2 Suppl):374S–379S
McCabe L, Britton RA, Parameswaran N (2015) Prebiotic and probiotic regulation of bone health: role of the intestine and its microbiome. Curr Osteoporos Rep 13:363–371
Whisner CM, Castillo LF (2018) Prebiotics, bone and mineral metabolism. Calcif Tissue Int 102:443–479
Jansson PA, Curiac D, Ahrén IL et al (2019) Probiotic treatment using a mix of three Lactobacillus strains for lumbar spine bone loss in postmenopausal women: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet Rheumatol 1:e154–e162
Nilsson AG, Sundh D, Bäckhed F, Lorentzon M et al (2018) Lactobacillus reuteri reduces bone loss in older women with low bone mineral density: a randomized, placebo-controlled, double-blind, clinical trial. J Intern Med 284:307–317
Jafarnejad S, Djafarian K, Fazeli MR, Yekaninejad MS, Rostamian A, Keshavarz SA (2017) Effects of a multispecies probiotic supplement on bone health in osteopenic postmenopausal women: a randomized, double-blind, controlled trial. J Am Coll Nutr 36:497–506
Takimoto T, Hatanaka M, Hoshino T, Takara T, Tanaka K, Shimizu A, Morita H, Nakamura T (2018) Effect of Bacillus subtilis C-3102 on bone mineral density in healthy postmenopausal Japanese women: a randomized, placebo-controlled, double-blind clinical trial. Biosci Microbiota Food Health 37:87–96
van den Heuvel EG, Muys T, van Dokkum W, Schaafsma G (1999) Oligofructose stimulates calcium absorption in adolescents. Am J Clin Nutr 69:544–548
Griffin IJ, Davila PM, Abrams SA (2002) Non-digestible oligosaccharides and calcium absorption in girls with adequate calcium intakes. Br J Nutr 87:S187–S191
Abrams SA, Griffin IJ, Hawthorne KM, Liang L, Gunn SK, Darlington G, Ellis KJ (2005) A combination of prebiotic short and long-chain inulin-type fructans enhances calcium absorption and bone mineralization in young adolescents. Am J Clin Nutr 82:471–476
Holloway L, Moynihan S, Abrams SA, Kent K, Hsu AR, Friedlander AL (2007) Effects of oligofructose-enriched inulin on intestinal absorption of calcium and magnesium and bone turnover markers in postmenopausal women. Br J Nutr 97:365–372
van den Heuvel EG, Schoterman MH, Muijs T (2000) Transgalactooligosaccharides stimulate calcium absorption in postmenopausal women. J Nutr 130:2938–2942
Biver E, Durosier-Izart C, Merminod F, Chevalley T, van Rietbergen B, Ferrari SL, Rizzoli R (2018) Fermented dairy products consumption is associated with attenuated cortical bone loss independently of total calcium, protein, and energy intakes in healthy postmenopausal women. Osteoporos Int 2018; 29: 1771–1782
Panahi S, Fernandez MA, Marette A, Tremblay A (2016) Yogurt, diet quality and lifestyle factors. Eur J Clin Nutr 71:573
Zhu K, Prince RL (2015) Lifestyle and osteoporosis. Curr Osteoporos Rep 13:52–59
Roy DK, O'Neill TW, Finn JD et al (2003) Determinants of incident vertebral fracture in men and women: results from the European prospective osteoporosis study (EPOS). Osteoporos Int 14:19–26
Nevitt MC, Cummings SR, Stone KL, Palermo L, Black DM, Bauer DC, Genant HK, Hochberg MC, Ensrud KE, Hillier TA, Cauley JA (2005) Risk factors for a first-incident radiographic vertebral fracture in women > or = 65 years of age: the study of osteoporotic fractures. J Bone Miner Res 20:131–140
Nakamura K, Kurahashi N, Ishihara J, Inoue M, Tsugane S, Japan Public Health Centre-based Prospective Study Group (2009) Calcium intake and the 10-year incidence of self-reported vertebral fractures in women and men: the Japan public health centre-based prospective study. Br J Nutr 101:285–294
Leslie WD, Lix LM (2014) Comparison between various fracture risk assessment tools. Osteoporos Int 25:1–21
Hidayat K, Du X, Shi BM (2018) Sex hormone-binding globulin and risk of fracture in older adults: systematic review and meta-analysis of observational studies. Osteoporos Int 29:2171–2180
Hidayat K, Du X, Wu MJ, Shi BM (2019) The use of metformin, insulin, sulphonylureas, and thiazolidinediones and the risk of fracture: systematic review and meta-analysis of observational studies. Obes Rev 20:1494–1503
Hidayat K, Du X, Shi BM (2019) Risk of fracture with dipeptidyl peptidase-4 inhibitors, glucagon-like peptide-1 receptor agonists, or sodium-glucose cotransporter-2 inhibitors in real-world use: systematic review and meta-analysis of observational studies. Osteoporos Int 30:1923–1940
Institute of Medicine (US) Committee on Dietary Risk Assessment in the WIC Program. Dietary Risk Assessment in the WIC Program. Washington (DC): National Academies Press (US); 2002. 5, Food-Based Assessment of Dietary Intake. Available from: https://www.ncbi.nlm.nih.gov/books/NBK220560/
Pranger IG, Joustra ML, Corpeleijn E, Muskiet FAJ, Kema IP, Oude Elferink SJWH, Singh-Povel C, Bakker SJL (2019) Fatty acids as biomarkers of total dairy and dairy fat intakes: a systematic review and meta-analysis. Nutr Rev 77:46–63
de Oliveira Otto MC, Lemaitre RN, Song X, King IB, Siscovick DS, Mozaffarian D (2018) Serial measures of circulating biomarkers of dairy fat and total and cause-specific mortality in older adults: the cardiovascular health study. Am J Clin Nutr 108:476–484
Imamura F, Fretts A, Marklund M et al (2018) Fatty acid biomarkers of dairy fat consumption and incidence of type 2 diabetes: a pooled analysis of prospective cohort studies. PLoS Med 15:e1002670
Hidayat K, Yu LG, Yang JR et al (2020) The association between milk consumption and metabolic syndrome: a cross-sectional study of the residents of Suzhou, China and a meta-analysis. Br J Nutr. https://doi.org/10.1017/S0007114520000227 Ahead of print
Thorning TK, Raben A, Tholstrup T, Soedamah-Muthu SS, Givens I, Astrup A (2016) Milk and dairy products: good or bad for human health? An assessment of the totality of scientific evidence. Food Nutr Res 60:32527
Hidayat K, Du X, Shi BM (2019) Milk in the prevention and management of type 2 diabetes: the potential role of milk proteins. Diabetes Metab Res Rev: e3187
Lamarche B, Givens DI, Soedamah-Muthu S, Krauss RM, Jakobsen MU, Bischoff-Ferrari HA, Pan A, Després JP (2016) Does milk consumption contribute to cardiometabolic health and overall diet quality? Can J Cardiol 32:1026–1032
Fenton TR, Lyon AW (2011) Milk and acid-base balance: proposed hypothesis versus scientific evidence. J Am Coll Nutr 30:471S–475S
Fenton TR, Lyon AW, Eliasziw M, Tough SC, Hanley DA (2009) Meta-analysis of the effect of the acid-ash hypothesis of osteoporosis on calcium balance. J Bone Miner Res 24:1835–1840
Fenton TR, Eliasziw M, Tough SC, Lyon AW, Brown JP, Hanley DA (2010) Low urine pH and acid excretion do not predict bone fractures or the loss of bone mineral density: a prospective cohort study. BMC Musculoskelet Disord 11:88
Fenton TR, Lyon AW, Eliasziw M, Tough SC, Hanley DA (2009) Phosphate decreases urine calcium and increases calcium balance: a meta-analysis of the osteoporosis acid-ash diet hypothesis. Nutr J 8:41
Calvez J, Poupin N, Chesneau C, Lassale C, Tomé D (2012) Protein intake, calcium balance and health consequences. Eur J Clin Nutr 66:281–295
Cao JJ, Johnson LK, Hunt JR (2011) A diet high in meat protein and potential renal acid load increases fractional calcium absorption and urinary calcium excretion without affecting markers of bone resorption or formation in postmenopausal women. J Nutr 141:391–397
Hunt JR, Johnson LK, Fariba Roughead ZK (2009) Dietary protein and calcium interact to influence calcium retention: a controlled feeding study. Am J Clin Nutr 89:1357–1365
Kerstetter JE, O'Brien KO, Caseria DM, Wall DE, Insogna KL (2005) The impact of dietary protein on calcium absorption and kinetic measures of bone turnover in women. J Clin Endocrinol Metab 90:26–31
Rizzoli R, Biver E, Bonjour JP, Coxam V, Goltzman D, Kanis JA, Lappe J, Rejnmark L, Sahni S, Weaver C, Weiler H, Reginster JY (2018) Benefits and safety of dietary protein for bone health-an expert consensus paper endorsed by the European Society for Clinical and Economical Aspects of Osteopororosis, Osteoarthritis, and Musculoskeletal Diseases and by the International Osteoporosis Foundation. Osteoporos Int 29:1933–1948
Darling AL, Manders RJF, Sahni S, Zhu K, Hewitt CE, Prince RL, Millward DJ, Lanham-New SA (2019) Dietary protein and bone health across the life-course: an updated systematic review and meta-analysis over 40 years. Osteoporos Int 30:741–761
Sahni S, Cupples LA, McLean RR, Tucker KL, Broe KE, Kiel DP, Hannan MT (2010) Protective effect of high protein and calcium intake on the risk of hip fracture in the Framingham offspring cohort. J Bone Miner Res 25:2770–2776
Mangano KM, Walsh SJ, Kenny AM, Insogna KL, Kerstetter JE (2014) Dietary acid load is associated with lower bone mineral density in men with low intake of dietary calcium. J Bone Miner Res 29:500–506
Dargent-Molina P, Sabia S, Touvier M, Kesse E, Bréart G, Clavel-Chapelon F, Boutron-Ruault MC (2008) Proteins, dietary acid load, and calcium and risk of postmenopausal fractures in the E3N French women prospective study. J Bone Miner Res 23:1915–1922
Weaver CM, Gordon CM, Janz KF, Kalkwarf HJ, Lappe JM, Lewis R, O'Karma M, Wallace TC, Zemel BS (2016) The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporos Int 27:1281–1386
Gowing LR, Ali RL, Allsop S et al (2015) Global statistics on addictive behaviours: 2014 status report. Addiction 110:904–919
Guthold R, Stevens GA, Riley LM, Bull FC (2018) Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health 6:e1077–e1086
GBD 2016 Alcohol Collaborators (2018) Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet 392:1015–1035
NCD Risk Factor Collaboration (NCD-RisC) (2016) A century of trends in adult human height. Elife 5:e13410
Salomon JA, Wang H, Freeman MK, Vos T, Flaxman AD, Lopez AD, Murray CJ (2012) Healthy life expectancy for 187 countries, 1990-2010: a systematic analysis for the global burden disease study 2010. Lancet 380:2144–2162
Weaver CM, Proulx WR, Heaney R (1999) Choices for achieving adequate dietary calcium with a vegetarian diet. Am J Clin Nutr 70:543S–548S
The Dietary Guidelines for Americans 2015-2020. Appendix 11. Food Sources of Calcium. https://health.gov/dietaryguidelines/2015/guidelines/appendix-11/. Accessed 20 Dec 2019
Funding
The study was supported by grants from the National Key R&D Program of China (No. 2017YFC1310700, No. 2017YFC1310701) and the Suzhou Science and Technology Bureau (No. SYS201741).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hidayat, K., Du, X., Shi, BM. et al. Systematic review and meta-analysis of the association between dairy consumption and the risk of hip fracture: critical interpretation of the currently available evidence. Osteoporos Int 31, 1411–1425 (2020). https://doi.org/10.1007/s00198-020-05383-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05383-3