Abstract
Summary
The role of dairy foods for hip fracture prevention remains controversial. In this study, among US men and women, a glass of milk per day was associated with an 8% lower risk of hip fracture. This contrasts with a reported increased risk with higher milk intake in Swedish women.
Introduction
The purpose of this study was to examine whether higher milk and dairy food consumption are associated with risk of hip fracture in older adults following a report of an increased risk for milk in Swedish women.
Methods
In two US cohorts, 80,600 postmenopausal women and 43,306 men over 50 years of age were followed for up to 32 years. Cox proportional hazards models were used to calculate the relative risks (RR) of hip fracture per daily serving of milk (240 mL) and other dairy foods that were assessed every 4 years, controlling for other dietary intakes, BMI, height, smoking, activity, medications, and disease diagnoses.
Results
Two thousand one hundred thirty-eight incident hip fractures were identified in women and 694 in men. Each serving of milk per day was associated with a significant 8% lower risk of hip fracture in men and women combined (RR = 0.92, 95% confidence interval (CI) 0.87 to 0.97). A suggestive inverse association was found for cheese in women only (RR = 0.91, CI 0.81 to 1.02). Yogurt consumption was low and not associated with risk. Total dairy food intake, of which milk contributed about half, was associated with a significant 6% lower risk of hip fracture per daily serving in men and women (RR = 0.94, CI 0.90 to 0.98). Calcium, vitamin D, and protein from non-dairy sources did not modify the association between milk and hip fracture, nor was it explained by contributions of these nutrients from milk.
Conclusions
In this group of older US adults, higher milk consumption was associated with a lower risk of hip fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures are a serious consequence of low bone density as they require costly surgery and long stays in a rehabilitation facility and subsequently increase risk of death, particularly for men [1]. The number of adults in the USA with low bone density at the femoral neck was estimated to be about 39 million in 2010 [2] and the count will climb as the elderly population grows. To protect aging bone, the 2015 Dietary Guidelines for Americans recommends that adults consume 2 to 3 cups of milk or equivalent dairy foods per day [3], whereas actual consumption among adults 50–71 years of age is 1.4 per day in women and 1.7 in men [3].
Milk is a likely food for maintaining bone health as it is a significant source of calcium and protein and also supplies vitamin D due to fortification in the US. However, the benefit of milk consumption for the prevention of hip fractures has not been established and it is unclear to what extent other dairy foods may or may not lower fracture risk. In 2005, a meta-analysis of data from six cohorts found a non-significant 17% increase in risk of hip fracture for men and women consuming less than one glass of milk per day compared with all others [4], whereas a 2010 meta-analysis of data with six additional cohort studies reported no overall association between milk and hip fractures [5]. In both analyses, a benefit from milk appeared to be stronger for men, though the results were too imprecise to draw a conclusion due to the much smaller number of male participants and fractures. More recently, a non-significant 40% lower risk of hip fracture was reported in elderly men and women in the Framingham Original Cohort who consumed more than one serving of milk per week compared with those with lower intakes [6]. On the other hand, in two large Swedish cohorts, women had a significant 9% greater risk of hip fracture for every glass of milk consumed per day, whereas no association was observed men [7].
To compare with these results from the Swedish study and to address the relative lack of data in men, we examined long-term consumption of milk and other dairy foods and risk of hip fracture in two large US cohorts, the Nurses’ Health Study (NHS) of women and the Health Professionals Follow-up Study (HPFS) of men. We previously reported no significant associations between milk consumption and hip fractures in these cohorts [8,9,10], though statistical power was low. In this investigation with additional years of follow-up and hip fracture cases, we expanded analyses to explore whether a benefit from dairy foods may vary by sex, age, timing of dairy food consumption in relation to fracture occurrence, or other dietary intakes in order to determine whether differences in these factors between previous studies could help to explain differences in results. Our hypothesis was that milk would be protective against hip fracture when assessed as a long-term measure and may be limited to those with lower intakes of calcium, vitamin D, and protein from non-dairy sources if these nutrient contributions from milk were responsible for the protective effect.
Methods
Study population
The NHS began in June of 1976 when 121,700 female registered nurses, 30 to 55 years of age, responded to a mailed questionnaire. The HPFS was formed 10 years later in January of 1986 with 51,529 male health professionals who were 40 to 75 years of age. On the initial questionnaires, participants provided a medical history and information on lifestyle and disease risk factors. Follow-up questionnaires have been mailed every 2 years to update individual characteristics and to identify incident diagnoses. Dietary intake was first assessed in 1980 in NHS and at 1986 baseline in HPFS. Deaths were ascertained from family members and the postal service and confirmed through the National Death Index [11, 12].
This longitudinal analysis included follow-up from the initial cohort dietary assessment through 2012. Women did not enter into analysis until they reached menopause, and for consistency, men did not enter until they reached 50 years of age. Participants were excluded at entry if they reported a prior hip fracture (144 women; 15 men) or a diagnosis of osteoporosis (2933 women; 186 men) or were African-American or Asian (3630 women; 1405 men). In our primary analyses using long-term dietary measures, participants were also excluded if they did not respond to the dietary questionnaire at entry (27,315 women; 4831 men). A total of 80,600 women and 43,306 men contributed to this analysis. Follow-up rates for these study populations were more than 90% over the time period of this analysis. This investigation was approved by the Institutional Review Board at Brigham and Women’s Hospital in Boston, MA.
Hip fractures
On every biennial questionnaire, participants were asked to report any hip fracture with the date of occurrence and a description of the circumstances. As health professionals, cohort members were capable of accurately reporting these event, as demonstrated in a small validation study in which all 30 self-reports were confirmed by medical records [13]. Fractures due to malignancy or major traumatic events (e.g., motor vehicle accidents, skiing, horseback riding) were not included as outcomes in this study. The majority of the fracture cases occurred when slipping, tripping, falling from the height of a chair, or similar low trauma event (96% in women, 91% in men). Hip fractures were also identified from death records in both cohorts.
Diet and supplement use
Diet was assessed with a semiquantitative food frequency questionnaire (FFQ) in 1980 and 1984 in the NHS and in1986 and every 4 years thereafter in both cohorts, totaling nine FFQs in the NHS and seven in the HPFS over follow-up. Participants reported their frequency of consumption over the previous year for specified serving sizes of more than 130 foods by selecting from among nine categories: never or ˂ 1/month, 1–3/month, 1/week, 2–4/week, 5–6/week, 1/day, 2–3/day, 4–5/day, ≥ 6/day. Skim, low fat, and whole fat varieties of milk were assessed separately and reported per 1 cup (240 mL) serving. Yogurt was assessed as plain, regularly sweetened, or artificially sweetened and each was reported per 1 cup serving. Hard cheese and cream cheese were reported per 1 oz. (28 g) and cottage or ricotta cheese per 0.5 cup serving. Other dairy foods on the FFQ included regular ice cream per 0.5 cup, frozen yogurt or low fat ice cream per 0.5 cup, and cream or sour cream per 1 tablespoon (15 mL). Daily energy and nutrient intakes, including calcium, vitamin D, protein, vitamin K, caffeine, and alcohol, were calculated from all reported frequencies of food consumption and the nutrient contents of these foods, which were derived primarily from U.S. Department of Agriculture sources and supplemented with data from food manufacturers and published research.
Current use of nutrient supplements, including calcium, vitamin D, retinol, and multivitamins, was ascertained on every biennial questionnaire. Participants provided the brand name and number of tablets per week for multivitamins and dosage per day for calcium, vitamin D, and retinol supplements so that an accurate daily intake of could be calculated.
In validation studies, the FFQ was shown to be a suitable instrument for discriminating between levels of dietary intakes. In a comparison of the FFQ with diet records collected seasonally over the previous year, the correlation for skim and low fat milk consumption was 0.88 among 127 HPFS men [14] and 0.81 among 173 NHS women [15].
Non-dietary measures
Non-dietary measures, including weight, smoking status and number of cigarettes smoked per day, menopausal status and use of postmenopausal hormones (women), diagnoses of cancer, cardiovascular disease, diabetes and osteoporosis, hours per week spent in recreational activities, and use of thiazide diuretics, furosemide-like diuretics (e.g., Lasix®, Bumex®), and oral steroids were assessed on biennial questionnaires. Total metabolic energy expenditure (MET-hours/week) was calculated from the reported recreational activities [16]. Body mass index (kg/m2) was calculated from the current biennial weight and the height reported on the initial cohort questionnaire. In 1986, participants were asked to recall their frequency of milk consumption during teenage years and they also reported their waist circumference to the nearest 0.25 in. using the tape measure provided with this questionnaire. Waist assessments were repeated in 1996 and 2000 in women and 1996 and 2008 in men.
Statistical analysis
NHS participants contributed person-time from the return date of their 1980 questionnaire if they were postmenopausal, either natural or through surgery, or at the first questionnaire after reaching menopause. HPFS participants contributed person-time from the return date of their 1986 questionnaire if they were at least 50 years of age or at the first questionnaire after age 50. Participants were censored at the date of hip fracture or death from hip fracture, last questionnaire response, or the end of follow-up in 2012. In the primary analyses, we used food and nutrient intakes that were cumulatively averaged over follow-up, i.e., at every dietary assessment, intakes were updated with the mean of all reports up to that time. Participants who did not respond to the baseline FFQ were not included in this analysis and those who were included did not contribute person-time in cycles in which they failed to report their dietary intake on the two most recent FFQs.
In alternate analyses, we used current dairy food intake and baseline intake at study entry as the exposure variables to examine how time between diet assessment and hip fracture might affect the results. The number of hip fracture cases and person-time in these analyses differed from our primary analysis. Current diet was calculated as the mean from the two most recent FFQs and participants did not contribute person-time in cycles in which they were missing both assessments. The baseline analysis included all participants who responded to the FFQ at study entry.
We used Cox proportional hazards models to compute relative risks (RR) for hip fracture within categories of consumption of specific dairy foods, using the same categories as the reports from the FFQ and collapsing the categories to accommodate the distribution of intakes. We also analyzed total dairy foods as the sum of the servings consumed from all dairy foods on the FFQ in pre-determined categories of ˂ 1, 1, 2, 3, ≥ 4 servings/day. All models were conditioned on months of age and questionnaire cycle to account for age and calendar time and controlled for total energy intake (continuous). Multivariable RRs were calculated from models adjusted simultaneously for all dietary and non-dietary covariates, which included all assessed factors associated or thought to be associated with risk of hip fracture and/or consumption of dairy foods: intakes of calcium, vitamin D, and protein from non-dairy foods and supplements (quintiles), retinol from supplements (zero, ˂ 400, 400–999, 100–1599, ≥ 1600 μg/day), intakes of vitamin K and caffeine (quintiles), alcohol (˂ 0.5, 0.5–4.9, 5–9.9, 10–19.9, ≥ 20 g/day), milk intake during teenage years (˂ 1, 1, 2, ≥ 3 glasses/day, missing), body mass index ˂ 21, 21–22, 23–24, 25–26, 27–28, ≥ 29 kg/m2, missing), attained height (continuous), physical activity (quintiles, missing), smoking (never smoker, past smoker with ˂ 5, 5–9, ≥ 10 years since quitting, current smoker with ˂ 15, 15–24, ≥ 25 cigarettes/day, missing), use of postmenopausal hormones (never, past, current, missing), use of thiazide diuretics, furosemide-type diuretics, and oral steroids (no, yes, missing), and diagnoses of cancer, diabetes, and cardiovascular disease (no, yes). The dairy food and covariate data at the beginning of every 2-year questionnaire cycle were used to allocate person-time to the appropriate category for each variable. To assess a dose-response effect, a linear trend was determined by putting dairy food consumption into the model as a continuous value for an increase of one serving per day or per week. There was no evidence that the proportional hazards assumption was violated as the interactions terms between each dairy food (continuous) and age (continuous) were non-significant. We examined the possibility of nonlinear relations between dairy foods and risk of hip fracture non-parametrically using restricted cubic splines with three knots [17]. Significant curvature was assessed using the likelihood ratio test, comparing the model with only the linear term to the model with the linear and cubic spline terms (P curvature). The results from the two cohorts were pooled using a fixed effects model for the log of the relative risks [18]. Heterogeneity between the cohorts was assessed using the Q statistic (P heterogeneity).
To determine whether the associations between dairy food consumption and hip fracture varied within the populations, we stratified analyses by age, intakes of non-dairy calcium, vitamin D and protein, and other risk factors. Multiplicative interactions between the dairy food and the stratifying variables were assessed using the Wald test for continuous data or the likelihood ratio test for categorical data (P interaction). Statistical significance was set at p ˂ 0.05 for tests of interaction and curvature and p ˂ 0.10 for tests of heterogeneity.
Results
Mean age at study entry was 53.6 years (range 34–60) in the women and 57.7 years (range 50–75) in the men and mean follow-up times were 20.8 years among 80,600 women and 17.5 years among 43,306 men. Over follow-up in our primary analyses, 2138 low to moderate trauma hip fractures were identified in the women (median age 74 years, range 39–91) and 694 in the men (median age 78 years, range 51 to 96). Mean milk consumption dropped from 6.3 to 5.3 servings per week between 1986 and 2010 in both cohorts and 89% of the milk consumed was skim or low fat.
Age-standardized characteristics of the study populations are shown by frequency of milk consumption at baseline (Table 1). In both cohorts, more frequent consumption was associated with lower alcohol intake, higher total energy intake, and more frequent milk consumption during teenage years. Women with less frequent consumption were more likely to smoke, whereas smoking rates were low among the men overall. On average, women consumed more calcium from supplements than men.
In the primary analysis in which dairy food intakes were cumulatively averaged over follow-up, each additional serving of milk per day was associated with a significant 8% lower risk of hip fracture in women (RR = 0.92, 95% CI 0.86–0.98), a non-significant 9% lower risk in men (RR = 0.91, 95% CI 0.82–1.02), and a significant 8% lower risk for the pooled results (RR = 0.92, 95% CI 0.87–0.97) after adjusting for yogurt and cheese intakes and all assessed covariates in the multivariable models (Table 2). In the categorical analyses for milk in which ˂ 1/week was the reference group, those consuming 1/day had a 17% lower risk of hip fracture (RR = 0.83, 95% CI 0.73–0.96) and those consuming ≥ 2/day had a 23% lower risk (RR = 0.77, 95% CI 0.65–0.91) when results from the two cohorts were pooled. In women, results for milk from the basic model adjusted only for age, follow-up cycle, and total energy intake were somewhat attenuated in the multivariable model primarily due to confounding by physical activity, BMI, and smoking; in men, the basic model results were strengthened after adding height, alcohol, non-dairy protein, and milk consumption during teenage years, which we previously found to be associated with a higher risk of hip fracture in men [19]. For cheese, a lower risk associated with higher intake was observed in women only and was not significant (RR = 0.91, 95% CI 0.81–1.02 per 1 a day). Yogurt was not associated with a lower risk of hip fracture, though consumption was infrequent in both cohorts. Consumption was also low for cream and ice cream and neither one was associated with hip fracture in either cohort (data now shown). Higher total dairy food consumption (comprised of milk, cheese, yogurt, cream, and ice cream) was associated with a significant 7% lower risk of hip fracture in women (RR = 0.93, 95% CI 0.88–0.98 per 1 a day), largely due to the fact that milk contributed approximately half to the total, whereas the association exhibited significant curvature in men. When the cohort results were pooled, risk of hip fracture declined by a significant 6% per daily serving of dairy foods (RR = 0.94, 95% CI 0.90–0.98). Spline curves for hip fracture risk by the cumulative averaged food intakes are in Supplemental Fig. 1.
In the multivariable analyses, all covariates for diet, disease diagnoses, and height had no missing data. In both cohorts, less than 4% of the observations were missing data for physical activity, BMI, smoking, and use of medications, whereas 16% were missing data for milk consumption during teenage years as it was asked on only one questionnaire. In alternate analyses, we excluded all observations with any missing data rather than including them in separate categories, leaving 1621 hip fractures in the women and 541 in the men. The results were essentially the same as those from the models that included missing covariate data, e.g., the RR for each additional serving of milk per day was 0.89 (95% CI 0.82–0.96) in women and 0.90 (95% CI 0.79–1.02) in men. Results also remained unchanged when covariates were entered into the models as continuous rather than categorical data (data now shown).
We conducted several secondary analyses. In one, we included total intakes of calcium, vitamin D, and protein in our multivariable models instead of the non-dairy sources of these nutrients, expecting the results to be attenuated if the benefit from milk could be attributed to one or more of these nutrient components, but we did not observe this. For example, the RR for hip fracture per daily serving of milk was 0.90 (95% CI 0.83–0.98) in women and 0.89 (95% CI 0.77–1.02) in men. In another analysis, women were censored (n = 18,325) upon reported use of any osteoporosis drug, specifically bisphosphonates, raloxifene, calcitonin, and tamoxifen, which were added to the biennial questionnaires in 1998 and later. All results were essentially the same as the primary results (data not shown). Finally, we controlled for whether participants reported difficulty with their balance or limited ability to walk several blocks or climb a flight of stairs, which were initially assessed in 1990. Again, results remained unchanged (data not shown).
We examined whether current diet or an early diet assessment would show different associations between dairy foods and hip fracture compared with our cumulative average measure (Table 2). For both men and women, results for current and cumulative average dairy food intakes were very similar. For example, for the pooled cohort results for milk, both measures were associated with a significant 8% lower risk per daily serving. In contrast, we observed only a non-significant 4% lower risk when the baseline diet assessment was used in relation to hip fracture over the full follow-up period. Results for baseline cheese and total dairy food intakes were similarly attenuated in comparison with the cumulative average and current measures in women. Pooled cohort results from the categorical food intake models in Table 2 are in Supplemental Table 1.
Associations between milk and hip fracture did not differ significantly by age (P interaction = 0.54 in women and 0.29 in men) (Table 3). Nevertheless, there was a significant linear trend in lower risk with increasing milk consumption in men under 75 years of age (RR = 0.82, 95% CI 0.69–0.98 per 1 a day) but not in older men. We also did not find clear support for our hypothesis that a benefit from higher milk consumption may be limited to adults with a lower intake of calcium, vitamin D, or protein from non-dairy sources (all P interaction ˃ 0.05). Spline curves for the models in Table 3 are in Supplemental Fig. 2. Results for cheese and total dairy intake also showed no significant differences between strata of non-dairy calcium, vitamin D, and protein (data now shown).
In an exploratory analysis, we observed a strong interaction between milk and BMI in men (P interaction ˂ 0.001) (Table 4). Risk of hip fracture was 53% lower per daily serving in obese men with BMI ≥ 30 kg/m2 (RR = 0.47, 95% CI 0.25–0.87) but showed no benefit in the lower BMI categories. A similar pattern was seen for cheese (P interaction = 0.02) and total dairy foods (P interaction ˂ 0.001) in men. In women, a significant interaction with BMI was only observed for cheese (P interaction = 0.002), with lower risks in the BMI categories ≥ 25 but no benefit and significant curvature in the lower BMI categories. Risk of hip fracture was also a significant 21% lower among the obese women per daily serving of both milk and total dairy foods. We also examined associations between dairy foods and hip fracture stratified by waist circumference, which was available for 63% of the follow-up in women and 80% in men. In men, we observed some similarity to the BMI stratified results in that risk per daily serving was lower for cheese (P interaction = 0.05), total dairy foods (P interaction = 0.01), and somewhat for milk (P interaction = 0.19) in those with a larger waist circumference. However, this was not observed for any of the dairy food and hip fracture associations in women. In other exploratory analyses, we did not find any evidence that associations between dairy intakes and risk of hip fracture were modified by physical activity, alcohol, smoking, postmenopausal hormone use, height, or milk consumption during teenage years.
Discussion
In this investigation among Caucasian men 50 years of age and older and women past menopause, each additional serving of milk per day was associated with a significant 8% lower risk of hip fracture when milk was assessed as a long-term cumulative average that was updated every 4 years. In women, the data suggested that higher cheese intake may also contribute to a lower hip fracture risk but the result was not statistically significant. Yogurt, cream, and ice cream were not associated with risk of hip fracture in either cohort, though consumption was low and did not provide adequate distribution of intakes for analyses. For total dairy food consumption, risk of hip fracture was a significant 6% lower per daily serving in men and women. Analyses based on current dairy food intakes yielded similar results to those based on the cumulative average measures, whereas results were attenuated if only a baseline measure was used, indicating the importance of current diet for assessing hip fracture risk.
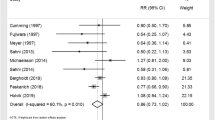
No clinical trials have been conducted to investigate milk or dairy food consumption and hip fractures and previous cohort studies do not generally support an inverse association. In a meta-analysis by Bischoff-Ferrari et al. [5], which included a previous meta-analysis [4], our earlier reports from HPFS [8] and NHS [10], and four additional studies, there was no association between milk and hip fracture in women, whereas each glass of milk per day was associated with a marginally significant 9% lower risk in men (RR = 0.91, 95% CI 0.81–1.01). The result for men was imprecise as the data included only 195 hip fractures. Nevertheless, it supports the similar inverse association that we observed in HPFS. The results for women were heavily influenced by the large Swedish Mammography Cohort [20], which was the only study with a positive association between milk and hip fracture risk. After excluding this study, the meta-analysis resulted in a marginally significant 5% lower risk per glass of milk per day in women (RR = 0.95, 95% CI 0.90–1.00). A subsequent study among men and women in the US Framingham cohort reported a threshold association between milk and hip fracture, with a marginally significant 40% lower risk for those consuming ˃ 1 versus ≤ 1 serving/week (RR = 0.60, 95% CI 0.36–1.02) that was partially attributed to increased bone mineral density [6].
A more recent analysis of the Swedish Mammography Cohort with the addition of the Cohort of Swedish Men [7] reported a significant 9% increase in risk of hip fracture per glass of milk per day in women, although after controlling for the intake of other dairy foods as we did, the result was attenuated to a 6% increase in risk but remained significant. The authors suggested that milk may indeed have an undesirable effect because it is the main dietary source of d-galactose, which causes premature aging in animal models through oxidative stress and chronic inflammation [21], factors that contribute to bone and muscle loss in humans [22,23,24]. In contrast to milk, fermented milk, and yogurt were associated with a significant 11% lower risk of hip fracture per daily serving in women, despite the galactose content of these foods [25]. Cheese, which is typically low in galactose, was associated with a 14% lower risk. None of these dairy foods were associated with hip fracture in the men. It is difficult to know why the results from this Swedish study should contrast with what we observed in our US cohorts, though some differences are worth noting. The prevalence of obesity in adults is much higher in the USA than in Sweden (36 and 17%, respectively) [26, 27], and we found some evidence that milk and dairy foods may be more likely to reduce risk of for hip fracture among those with higher BMI. In addition, Scandinavia has the highest reported incidence of hip fracture worldwide [28], and particular factors contributing to this high incidence may influence the risk associated with dairy consumption. Fortification of milk with vitamin D also differs, with levels in Sweden about half that in the USA and does not include all milk types. In terms of study design, the follow-up period for the Swedish women was over 20 years and diet was updated only once and only for a portion of the population. In our cohort, we found that current milk and dairy food intakes were most important, with the inverse association with hip fracture attenuating as the diet assessment became more distant in time, albeit never showing a positive association as seen in the Swedish study.
We anticipated that the relationship between dairy and hip fractures would change with age. We found some support for this in men, as milk was associated with a lower risk of hip fracture in those younger than 75 years but not at older ages. However, the evidence was weak and not confirmed in the women. We also expected that a benefit from dairy foods could be at least partially attributed to its calcium, vitamin D, and/or protein content. The data did not support this hypothesis, as non-dairy sources of these nutrients did not significantly modify the association between milk intake and hip fracture and the association was not attenuated when controlled for total intakes, including dairy sources, of these three nutrients. For vitamin D, it may be that the amount provided by milk (2.5 μg/glass) is too low to contribute to hip fracture reduction [29, 30]. For protein, it may be that in these US cohorts where protein consumption is high, an additional 8 g per glass of milk does not further improve fracture risk.
The inverse associations between dairy food consumption and risk of hip fracture may be stronger or even limited to those with a larger body size, as measured by BMI and waist circumference. Body fat can have a negative impact on bone as it induces a chronic inflammatory state [31] that can both accelerate bone resorption and inhibit bone formation [32] and may also negatively influence bone microarchitecture [33]. Indeed, although risk of hip fracture decreases with higher BMI, no additional benefit may occur with obesity [34,35,36]. Abdominal obesity-related inflammation may be particularly detrimental for bone, as we previously reported that risk of hip fracture in women increased with increasing waist circumference, independent of BMI [37]. Dairy food consumption might help to protect against hip fractures in the obese by reducing inflammation [38]. However, although some studies have shown that adding milk proteins to the diet can reduce markers of inflammation and oxidative stress, others have reported no effect [39]. It has also been suggested that an increase in dietary calcium and dairy foods may promote loss of body fat [40], although the preponderance of research indicates that this only occurs in energy-restricted weight loss diets [41, 42].
The major strength of the present study is the multiple measures of milk and dairy food intakes for up to 32 years of follow-up, which allowed us to calculate long-term average intakes and to reduce measurement error. We also assessed most major risk factors for hip fractures to control for confounding. Another strength is the large number of hip fractures for analysis that provided statistical power to observe associations. One limitation of the study was that we were unable to assess the influence of yogurt on risk of hip fractures due to low consumption. Another limitation was that hip fractures were mostly self-reported, and elderly participants in particular may have failed to respond to questionnaires to report their fracture. However, we also identified hip fractures that were a contributing cause of death on a death certificate. Misclassification of hip fractures could have attenuated our results. As the study populations were Caucasian, results may not be applicable to other races.
In conclusion, we found that higher long-term milk consumption in older adults was associated with a lower risk of hip fracture. The benefit was not explained by the calcium, vitamin D, or protein content of milk. The impact of other specific dairy foods in hip fracture prevention and the role of obesity require more detailed study.
References
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152(6):380–390
Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, Dawson-Hughes B (2014) The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 29(11):2520–2526
U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans, 8th Edition. December 2015. Available at http://health.gov/dietaryguidelines/2015/guidelines/
Kanis JA, Johansson H, Oden A, De Laet C, Johnell O, Eisman JA, Mc Closkey E, Mellstrom D, Pols H, Reeve J, Silman A, Tenenhouse AA (2005) Meta-analysis of milk intake and fracture risk: low utility for case finding. Osteoporos Int 16:799–804
Bischoff-Ferrari HA, Dawson-Hughes B, Baron JA, Kanis JA, Orav EJ, Staehelin HB, Kiel DP, Burckhardt P, Henschkowski J, Spiegelman D, Li R, Wong JB, Feskanich D, Willett WC (2011) Milk intake and risk of hip fracture in men and women; a meta-analysis of prospective cohort studies. J Bone Miner Res 26(4):833–839
Sahni S, Mangano KM, Tucker KL, Kiel DP, Casey VA, Hannan MT (2014) Protective association of milk intake on the risk of hip fracture: results from the Framingham original cohort. J Bone Miner Res 29(8):1756–1762
Michaëlsson K, Wolk A, Langenskiöld S, Basu S, Eva Lemming W, Melhus H, Byberg L Milk intake and risk of mortality and fractures in women and men: cohort studies. BMJ 2014;Oct 28 349:g6015
Owusu W, Willett WC, Feskanich D, Ascherio A, Spiegelman D, Colditz GA (1997) Calcium intake and the incidence of forearm and hip fractures among men. J Nutr 127(9):1782–1787
Feskanich D, Willett WC, Stampfer MJ, Colditz GA (1997) Milk, dietary calcium, and bone fractures in women: a 12-year prospective study. Am J Public Health 87(6):992–997
Feskanich D, Willett WC, Colditz GA (2003) Calcium, vitamin D, milk consumption, and hip fractures: a prospective study among postmenopausal women. Am J Clin Nutr 77(2):504
Stampfer MJ, Willett WC, Speizer FE, Dyserrt DC, Lipnick R, Rosner B, Hennekens CH (1984) Test of the National Death Index. Am J Epidemiol 119(5):837–839
Rich-Edwards JW, Corsano KA, Stampfer MJ (1994) Test of the National Death Index and Equifax Nationwide Death Search. Am J Epidemiol 140(11):10016–10019
Colditz GA, Martin P, Stampfer MJ, Willett WC, Sampson L, Rosner B, Hennekens CH, Speizer FE (1986) Validation of questionnaire information on risk factors and disease outcomes in a prospective cohort study of women. Am J Epidemiol 123(5):894–900
Feskanich D, Rimm EB, Giovannucci EL, Colditz GA, Stampfer MJ, Litin LB, Willett WC (1993) Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J Am Diet Assoc 93(7):790–796
Salvini S, Hunter DJ, Sampson L, Stampfer MJ, Colditz GA, Rosner B, Willett WC (1989) Food-based validation of a dietary questionnaire: the effects of week-to-week variation in food consumption. Int J Epidemiol 18(4):858–867
Ainsworth BE, Haskell WL, Leon AS, Jacobs DR, Montoye HJ, Sallis JF, Paffenbarger RS (1993) Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc 25(1):71–80
Durrleman S, Simon R (1989) Flexible regression models with cubic splines. Stat Med 8:551–561
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Feskanich D, Bischoff-Ferrari HA, Frazier AL, Willett WC (2014) Milk consumption during teenage years and risk of hip fracture in older adults. JAMA Pediatr 168(1):54–60
Michaelsson K, Melhus H, Bellocco R, Wolk A (2003) Dietary calcium and vitamin D intake in relation to osteoporotic fracture risk. Bone 32(6):694–703
Cui X, Zuo P, Zhang Q, Li X, Hu Y, Long J, Packer L, Liu J (2006) Chronic systemic D-galactose exposure induces memory loss, neurodegeneration, and oxidative damage in mice: protective effects of R-alpha-lipoic acid. J Neurosci Res 83(8):1584–1590
Hardy R, Cooper MS (2009) Bone loss in inflammatory disorders. J Endocrinol 201(3):309–320
Berglundh S, Malmgren L, Luthman H, McGuigan F, Akesson K (2015) C-reactive protein, bone loss, fracture, and mortality in elderly women: a longitudinal study in the OPRA cohort. Osteoporos Int 26(2):727–735
Roubenoff R (2007) Physical activity, inflammation and muscle loss. Nutr Rev 65(12 suppl 3):S208–S212
Abrahamson A. Galactose in dairy products. Available at http://stud.epsilon.slu.se/7718/1/abrahamson_a_150317.pdf
Ogden, CL, Carroll MD, Fryar CD, Flegal KM (2015) Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS data brief, no. 219. Hyattsville, MD: National Center for Health Statistics
Molarius A, Lindén-Boström M, Granström F, Jan Karlsson J (2016) Obesity continues to increase in the majority of the population in mid-Sweden—a 12-year follow-up. Eur J Pub Health 26(4):622–627
Kanis JA, Johnell O, De Laet C, Jonsson B, Oden A, Ogelsby AK (2002) International variations in hip fracture probabilities: implications for risk assessment. J Bone Miner Res 17(7):1237
Bischoff-Ferrari HA, Willett WC, Wong JB, Stuck AE, Staehelin HB, Orav EJ, Thoma A, Kiel DP, Henschkowski J (2009) Prevention of nonvertebral fractures with oral vitamin D and dose dependency: a meta-analysis of randomized controlled trials. Arch Intern Med 169(6):551
Bischoff-Ferrari HA, Willett WC, Orav EJ, Lips P, Meunier PJ, Lyons RA, Flicker L, Wark J, Jackson RD, Cauley JA, Meyer HE, Pfeifer M, Sanders KM, Stähelin HB, Theiler R, Dawson-Hughes BA (2012) Pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med 367(1):40–49
Das UN (2001) Is obesity an inflammatory condition? Nutrition 17(11–12):953–966
Baker-LePain JC, Nakamurab MC, Lane NE (2011) Effects of inflammation on bone: an update. Curr Opin Rheumatol 23(4):389–395
Rolland T, Boutroy S, Vilayphiou N, Blaizot S, Chapurlat R, Szulc P (2012) Poor trabecular microarchitecture at the distal radius in older men with increased concentration of high-sensitivity C-reactive protein—the STRAMBO study. Calcif Tissue Int 90(6):496–506
De Laet C, Kanis JA, Odén A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, McCloskey EV, Mellstrom D, Melton LJ 3rd, Meunier PJ, Pols HAP, Reeve J, Silman A, Tenenhouse A (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16(11):1330–1338
Armstrong ME, Spencer EA, Cairns BJ, Banks E, Pirie K, Green J, Wright FL, Reeves GK, Beral V (2011 Jun) Body mass index and physical activity in relation to the incidence of hip fracture in postmenopausal women. J Bone Miner Res 26(6):1330–1338
Nielson CM, Marshall LM, Adams AL, LeBlanc ES, Cawthon PM, Ensrud K, Stefanick ML, Barrett-Connor E, Orwoll ES (2011) BMI and fracture risk in older men: the osteoporotic fractures in men study (MrOS). J Bone Miner Res 26(3):496–502
Meyer HE, Willett WC, Flint AJ, Feskanich D (2016) Abdominal obesity and hip fracture: results from the Nurses’ Health Study and the Health Professionals Follow-up Study. Osteoporos Int 27(6):2127–2136
Sharples AP, Hughes DC, Deane CS, Saini A, Selman C, Stewart CE (2015) Longevity and skeletal muscle mass: the role of IGF signalling, the sirtuins, dietary restriction and protein intake. Aging Cell 14(4):511–523
Fekete ÁA, Givens DI, Lovegrove JA (2016) Can milk proteins be a useful tool in the management of cardiometabolic health? An updated review of human intervention trials. Proc Nutr Soc 75(3):328–341
Barba G, Russo P (2006) Dairy foods, dietary calcium and obesity: a short review of the evidence. Nutr Metab Cardiovasc Dis 16(6):445–451
Abargouei AS, Janghorbani M, Salehi-Marzijarani M, Esmaillzadeh A (2012) Effect of dairy consumption on weight and body composition in adults: a systematic review and meta-analysis of randomized controlled clinical trials. Int J Obes 36(12):1485–1493
Booth AO, Huggins CE, Wattanapenpaiboon N, Nowson CA (2015) Effect of increasing dietary calcium through supplements and dairy food on body weight and body composition: a meta-analysis of randomized controlled trials. Brit J Nutr 114(7):1013–1025
Funding
This study is funded by US National Institutes of Health grants CA186107, CA167552, and AG030521.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Feskanich, D., Meyer, H.E., Fung, T.T. et al. Milk and other dairy foods and risk of hip fracture in men and women. Osteoporos Int 29, 385–396 (2018). https://doi.org/10.1007/s00198-017-4285-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4285-8